Abstract
Astrocytes have transcended their role from mere structural scaffolds to pivotal regulators of neural circuitry and sleep–wake dynamics. The strategic proximity of their fine processes to blood vessels and synapses positions them as key players in neurobiology, contributing to the tripartite synapse concept. Gap-junction proteins also enable astrocytes to form an extensive network interacting with neuronal assemblies to influence sleep physiology. Recent advances in genetic engineering, neuroimaging and molecular biology have deepened our understanding of astrocytic functions. This review highlights the different mechanisms by which astrocytes regulate sleep, notably through transcriptomic and morphological changes, as well as gliotransmission, whereby intracellular calcium (Ca2+) dynamics plays a significant role in modulating the sleep–wake cycle. In vivo optogenetic stimulation of astrocytes indeed induces ATP release, which is subsequently degraded into adenosine, modulating neuronal excitability in sleep–wake regulatory brain regions. Astrocytes also participate in synaptic plasticity, potentially modulating sleep-associated downscaling, a process essential for memory consolidation and preventing synaptic saturation. Although astrocytic involvement in synaptic maintenance is well supported, the precise molecular mechanisms linking these processes to sleep regulation remain to be elucidated. By highlighting astrocytes' multiple roles in sleep physiology, these insights deepen our understanding of sleep mechanisms and pave the way for improving sleep quality.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Avoid common mistakes on your manuscript.
Introduction
Astrocytes are a type of glial cells first described in 1858 by the biologist Rudolf Virchow. The term "astrocyte" comes from the Greek astron, meaning “star”, and kytos for “cell”. This name, chosen in 1895 by Michael von Lenhossèk, to reflect their typical star-like morphology, is reminiscent of celestial bodies [1]. Their extensive processes enable them to establish close contact with blood vessels and neuronal synapses, giving them a highly strategic position. However, recognition of astrocyte functions took time due to several technical and conceptual challenges that hindered their study for decades. First, their highly branched and fine processes made it difficult to analyze their structure and functions using traditional microscopy. Moreover, their lack of electrical excitability led neuroscientists to focus primarily on neurons, which communicate via action potentials. Inadequate experimental tools further delayed progress as early electrophysiological methods were optimized for recording rapid neuronal activity, but were not suited for detecting astrocytic calcium-based signaling. Additionally, the absence of specific molecular markers made it difficult to distinguish astrocytes from other cells types and to manipulate them selectively. It was only with advances in genetic tools (astrocyte-specific transgenic models) and imaging techniques (two-photon microscopy and superresolution microscopy), that the intricate roles of astrocytes started to be uncovered. Historically viewed as passive structural elements, astrocytes are now recognized as active participants in neuronal communication. They express all the molecular machinery to sense synaptically-released neurotransmitters via the expression of a wide repertoire of receptors, transporters, and ion channels. They respond to synaptic activity via calcium (Ca2+) signaling [2] and can in turn release gliotransmitters or change their coverage of synapses, which can modulate the diffusion or reuptake of neurotransmitters and thereby regulate neurotransmission. Thus, astrocytes are not merely sensitive to neuronal activity, but can also initiate changes in synaptic activity, placing these cells at the heart of the fine regulation of various behaviors. Remarkably, over a century ago, the pioneering neuroscientist Santiago Ramón y Cajal was the first to propose a dynamic role for astrocytes in regulating sleep. He proposed that astrocytic processes extend into synapses during sleep, acting as a ‘circuit breaker’ to block synaptic transmission and retract during wakefulness to restore it [3]. However, Cajal’s hypothesis was not tied to a specific brain region, serving instead as a general conceptual model.
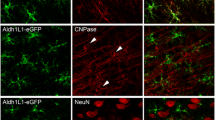
More recent studies, such as those by Bellesi et al. have provided experimental evidence focusing on the cortex. Using three-dimensional electron microscopy and immunohistochemistry, they demonstrated that astrocytic processes extend toward synapses during wakefulness, and retract during sleep, suggesting a dynamic role for astrocytes in synaptic regulation across the sleep–wake cycle [4]. Using translating ribosome affinity purification technology and microarrays, Bellesi et al. further demonstrated that arousal is accompanied by the upregulation of genes involved in extracellular matrix dynamics and cytoskeleton remodeling. This genetic activation facilitates the elongation of astrocytic processes toward synapses during wakefulness, in contrast to their retracted state observed state during sleep [4]. This reinforces the notion that astrocytes actively modulate synaptic interactions across the sleep–wake cycle.
Interestingly, these cortical-specific dynamics contrast Cajal’s prediction of astrocytic behavior during sleep and wake states. The close proximity of PAPs can enhance glutamate uptake, effectively reducing extracellular concentrations, while their withdrawal may increase glutamate spillover. Thus, the idea of a differential regulation of glutamate proposed by Cajal remains valid, albeit one that may vary across different brain regions and adapt to their specific functional demands.
The proximity of some astrocytic processes to synapses led to the concept of the tripartite synapse [5]. It is now clearly established that astrocytes play essential roles in brain functioning, not only in maintaining neuronal environment and survival, but also in modulating neural networks. They provide structural and metabolic support to neurons, and their proximity to blood vessels allows them to participate in the formation and maintenance of the blood–brain barrier, as well as in neurovascular coupling, adjusting blood flow in response to local neuronal activity [6,7,8] (Table 1). Astrocytes regulate ionic and aqueous homeostasis, particularly by regulating extracellular potassium levels [9, 10]. They can also trap and neutralize reactive oxygen species [11] and participate in the formation and maturation of synapses [12]. Following brain injury, astrocytes also contribute to the formation of the glial scar and the repair of the nervous tissue [13, 14]. Although not immune cells, astrocytes also play a role in the brain's inflammatory response [15] and phagocytose [16]. Finally, astrocytes communicate with each other via gap junctions, allowing them to form networks covering and modulating neuronal assemblies [17,18,19,20]. Thus, astrocytes regulate neuronal circuits underlying rhythmic behaviors such as locomotion, respiration, mastication, gastrointestinal motility, feeding, as well as sleep–wake cycles [21,22,23].
Advances in transgenic animals, brain imaging, and molecular biology have permitted to deepen our understanding of astrocytes in sleep regulation. This review will explore how astrocytes integrate metabolism, circadian rhythms, and synaptic activity to regulate sleep at the molecular, cellular and network levels.
Astrocytic gene expression: orchestrating circadian rhythms and sleep regulation
Astrocytes are key players in the regulation of circadian rhythms, a fundamental sleep regulatory process. In the suprachiasmatic nucleus (SCN), transcriptional regulation has been observed in astrocytes, enabling a negative feedback loop (transcription-translation feedback loop, TTFL), and constituting an astrocytic circadian molecular clock (Fig. 1). In this loop, the expression of transcription factors, circadian locomotor output cycles kaput (CLOCK), and Brain and Muscle ARNT-Like protein (BMAL1), form a heterodimer in the nucleus to promote the expression of numerous genes containing the cis-acting E-box promoter element, including the period (per) and cryptochrome (cry) genes [24]. Per and cry proteins inhibit the CLOCK-BMAL1 complex, but they are destabilized by post-transcriptional regulations, such as phosphorylation/dephosphorylation and ubiquitination, which play a crucial role in regulating their expression during the circadian cycle. While TTFLs are not exclusive to astrocytes, as neurons also maintain autonomous circadian oscillations, recent research has demonstrated that this astrocytic clock alone is sufficient to drive circadian oscillations within the SCN and influence circadian behaviors in mice [25], highlighting the essential role of astrocytes in coordinating circadian physiology.
Schematic overview of the various mechanisms by which astrocytes regulate sleep. Astrocytes modulate circadian behaviors through their molecular clock, via a transcription-translation negative feedback loop (TTFL). They regulate gene transcription, thereby modulating synaptic coverage and the size of the astrocytic network. Variations in aquaporin-4 expression facilitate cerebrospinal fluid circulation and brain clearing. Astroglial calcium activity changes dynamically across vigilance states and contributes to sleep homeostasis. Intracellular glycogen storage and degradation by astrocytes contribute to the regulation of wakefulness and sleep. Astrocytes also participate in the reuptake of neurotransmitters and the release of gliotransmitters, which regulate the neuronal network. Additionally, astrocytes contribute to synaptic homeostasis by modulating synaptic weights, which may decrease their downscaling during non-rapid eye movement (NREM) sleep. Yellow arrows indicate wakefulness-related changes, while blue arrows represent sleep-related changes
Moreover, the transcriptomic regulation of GABA transporters, specifically GAT3, facilitates the circadian rhythm of GABA uptake in the SCN. According to Patton et al. (2023), while GAT1 and GAT3 exhibit rhythmic expression, only GAT3 shows strong circadian regulation. GAT1 is expressed in both neurons and astrocytes, while GAT3 is predominantly astrocytic. Although both transporters contribute to GABA clearance, the authors demonstrated that this rhythmic GABA uptake is controlled by the cell autonomous circadian clock of astrocytes, with GAT3 playing a dominant role.
During the circadian day, the rhythmic upregulation of astrocytic GAT3 enhances GABA clearance, leading to lower extracellular GABA levels. This reduction in ambient GABA facilitates neuronal firing and promotes the release of neuropeptides essential for circadian signaling. In contrast, at night, the downregulation of GAT3 leads to an accumulation of extracellular GABA, which increases inhibitory tone and dampening neuronal excitability.
This circadian molecular clock within astrocytes orchestrates the day-night oscillation in GAT3 expression, driving its rhythmic transcription along with potentially other related genes. Through this time-of-day-dependent modulation of GABA uptake, astrocytes establish a dynamic environment that promotes neuronal activity during the day while exerting a more suppressive effect at night. This mechanism ensures the synchronization of GABAergic signaling with TTFL-driven circadian rhythms [26], emphasizing the integrative role of astrocytes in coordinating and sustaining circadian regulation, and the sleep–wake rhythm, at both the molecular and network levels (Fig. 1).
Transcriptional analysis of astrocytes from the cortex and striatum during the wake/sleep cycle has also revealed variations in gene expression throughout this cycle (Fig. 1). Using the technique of translating ribosome affinity purification (TRAP), which identifies mRNA undergoing translation, it has been shown that the astrocytic transcriptome changes between wakefulness and sleep, with 1.4% of astrocytic transcripts varying according to vigilance state [4]. Among these transcripts, 55 are overexpressed during sleep, such as Cirp and Uba1. Cirp encodes the cold-inducible RNA-binding protein, which binds to the untranslated regions of hundreds of transcripts to promote protein synthesis and cell proliferation and inhibits apoptosis [27], while Uba1 encodes a ubiquitination-activating enzyme involved in protein degradation and synaptic homeostasis, both essential for proper sleep regulation. However, many more transcripts are overexpressed during wakefulness, 396 in total, particularly those involved in extracellular matrix formation and cytoskeletal protein synthesis, which are implicated in the extension of astrocytic processes [4]. Among these transcripts is the gjb6 gene, which encodes connexin 30 (Cx30), a gap junction subunit controlling the morphological plasticity of astrocytes [28]. Astrocytes are indeed rapidly capable of modulating the extent of their peripheral astrocytic processes (PAPs), particularly in response to neuronal activity, which has been shown to directly influence synaptic glutamate levels in the hippocampus [28]. Thus, during wakefulness, astrocytic processes would be closer to synapses to facilitate glutamate clearance, whereas the reduction of astrocytic coverage during sleep could promote glutamate diffusion, to enhance neuronal synchronization, a hallmark of NREM sleep [4] (Fig. 1). Further experiments are required to determine whether these PAP movements effectively occur in relation to wakefulness and to explore whether such dynamics are consistent across distinct brain regions involved in regulating sleep and wakefulness.
Astrocytes also play a key role in sleep regulation through the circadian expression of mRNA encoding FABP7, a fatty acid-binding protein. As part of a large family of lipid chaperone proteins, FABP7 is essential in regulating intracellular fatty acid transport. Particularly enriched in astrocytes, FABP7 is involved in lipid signaling cascades that regulate changes in cellular growth, morphology and motility [29, 30]. The role of this protein in sleep regulation has been highlighted through the discovery of the T61M missense mutation in its gene, which leads to fragmented sleep in humans [30]. Similarly, its genetic deletion results in sleep fragmentation in mice [30].
Additionally, research into astrocytic gene expression during sleep has revealed an upregulation in the expression of the gene encoding the monocarboxylate transporter MCT1, which is essential for lactate transport between astrocytes and neurons [4]. This finding suggests an increased astrocyte-neuron lactate shuttle (ANLS) and restorative brain energy metabolism during sleep. Additionally, the increased glucose sensitivity observed in vitro, in astrocytes of the ventrolateral preoptic nucleus (VLPO), a key brain region involved in sleep regulation [7] further underscores the role of astrocytes in adjusting cerebral metabolism according to vigilance states. The influence of sleep deprivation on ANLS-related genes suggests that astrocytes dynamically adapt energy production and lactate transport to meet the fluctuating demands of wakefulness and sleep [31]. This ability of astrocytes to adapt metabolic processes is crucial for maintaining neuronal function and supporting sleep homeostasis, as the brain relies on these metabolic shifts for restoration and recovery during sleep.
Morphological modulations of astrocytes: from synaptic coverage to astrocytic network
Modulation of synaptic coverage
In the central nervous system, at least half of the synapses are enveloped by astrocytic processes known as perisynaptic astrocytic processes [12]. These fine processes are particularly enriched in ionic channels, neurotransmitter receptors, and transporters, allowing astrocytes to sense neuronal activity. Moreover, these extensions express proteins, such as ezrin, radixin, and connexin 30 (Cx30) [28, 32, 33], which contribute to the morphological plasticity of astrocytes. Through the non-channel functions of Cx30, changes in its expression levels can modulate intracellular cytoskeletal elements, leading to changes in astrocyte shape. Thus, the proximity of astroglial processes to the synapse permits the regulation of neurotransmission [28, 34]. Such changes in proximity to synapses have been observed by 3D electron microscopy during sleep regulation, as in the cortex, a few hours of sleep deprivation are sufficient to induce the extension of astrocytic processes closer to the synaptic cleft [4, 16] (Fig. 1).
Modulation of the astrocytic network size
Sleep regulation may also involve the modulation of astrocytic coupling. Astrocytes are indeed interconnected via gap junctions, composed of Cx30 and 43 (Cx43). These gap junctions enable the direct intercellular exchange of small molecules between astrocytes, creating a functional network. The size of the network refers to the number of astrocytes that are connected and able to communicate via these junctions. Variations in connexin expression can expand or shrink the size of this network, which in turn influences neuronal excitability [17] and consequently, sleep regulation [35].
The conditional Cx43 deficiency in astrocytes results in nocturnal hypersomnolence [36]. Modafinil, a potent wake-promoting psychostimulant, selectively upregulates Cx30 expression in the cortex without affecting Cx43 levels, potentially enhancing astrocytic coupling [37]. In contract, sleep-promoting agents such as gamma-hydroxybutyric acid or oleamide reduce astrocytic coupling, reinforcing the notion that astrocytic network connectivity is dynamically regulated across the sleep–wake cycle [38, 39]. These findings suggest that astrocytic coupling increases during wakefulness and decreases during sleep. Astrocytic networks play a pivotal role in regulating neuronal activity and sleep processes, dynamically adapting their size in response to physiological demands. This dynamic modulation may either mirror the activity levels of the underlying neuronal networks or exert direct influence over neuronal circuits. For example, when neuronal activity is suppressed using tetrodotoxin (TTX), astrocytic network size decreases significantly [20]. Conversely, heightened activity in the visual cortex, such as that induced by visual experience, induces a robust increase in Cx30 expression by approximately 70% [40].
Importantly, experimental manipulations of Cx30 expression further underscore its regulatory role. In Cx30-deficient mice, both astrocytic network size and neuronal activity are decreased [28, 41]. Conversely, viral overexpression of Cx30 expands the astrocytic network size but, paradoxically, also reduces neuronal activity [17]. These findings indicate that astrocytes finely tune neuronal excitability by modulating their network size, positioning them as dynamic regulators of excitability and sleep–wake transitions.
The evidence supports the idea that astrocytic networks are physiologically optimized to balance neuronal excitability and facilitate processes such as sleep regulation. A disruption in this optimization, either through reduced or excessive network size, can potentially impair neuronal function and sleep dynamics, underscoring the critical interplay between astrocytes and neurons in maintaining brain homeostasis.
Astrocytic roles in metabolite clearance and glycogen storage
Metabolite clearance in the brain
For over a decade, an interesting observation has been made regarding the importance of sleep for brain metabolite clearance. In vivo microdialysis experiments have shown that beta-amyloid peptide (Aβ) levels in the central nervous system’s interstitial fluid are higher during wakefulness than during sleep [42], with these variations decreasing as Alzheimer's disease progresses [43]. It has been proposed that the glymphatic drainage system may allow for the elimination of this Aβ peptide and that dysfunction of this drainage during sleep may contribute to the progression of the disease [44]. At the cortical level, sleep is associated with a ~ 60% increase in the interstitial space, which facilitates metabolite clearance [45, 46] (Table 1 and Fig. 1). However, these results remain debated [48], as Miao et al., suggest the opposite, showing that brain clearance may decrease during sleep due to limited bulk flow and diffusion dynamics [47]. These contrasting observations may stem from methodological differences among studies, particularly regarding the injection site of tracers, into the cerebrospinal fluid or directly into the brain parenchyma, as well as potential alterations in intracranial pressure, due to differences in infusion rates, injection volumes, or anesthesia protocols (e.g., isoflurane vs. ketamine-xylazine). These factors can differently influence cerebrospinal fluid dynamics and clearance efficiency by modulating cerebrovascular tone, glymphatic flow, and neuronal activity. Furthermore, the physicochemical properties of the injected molecules, including their molecular weight, charge, solubility, and affinity for specific transporters, may differentially affect their diffusion, uptake, and elimination across brain compartments. These different results highlight the need for standardized methodologies in tracer infusion and imaging techniques, methodology using non-invasive approaches and further investigations into the influence of regional heterogeneity on glymphatic clearance.
The primary mechanism responsible for this drainage involves aquaporin-4 (AQP4), a water-permeable channel essential for fluid transport. AQP4, one of the 13 members of the aquaporin family [48], is predominantly expressed by astrocytes at perivascular endfeet in contact with blood vessels [49]. Astrocytes may function as valves, actively promoting cerebrospinal fluid (CSF) flow through perivascular spaces, while preventing backflow [50, 51]. Deletion of AQP4 disrupts glymphatic clearance [52], underscoring the critical role of astrocytes in waste removal during sleep (Fig. 1).
Recent research provides further insights into the mechanisms driving glymphatic clearance. Nedergaard’s group demonstrated that in vivo, cerebrospinal fluid movement is facilitated by rhythmic blood vessel contractions regulated by norepinephrine oscillations, particularly during NREM sleep [53]. These oscillations create a pumping mechanism, propelling cerebrospinal fluid deeper into the brain, thereby enhancing waste clearance. Importantly, the study found that the widely used sleep aid zolpidem (Ambien) disrupts these blood vessel oscillations, potentially impairing glymphatic function and raising concerns about its impact on neurodegenerative diseases [53]. In addition to waste removal, astrocytes play a key role in brain metabolism by dynamically storing and utilizing glycogen to support neuronal function.
Glycogen storage for sleep and wakefulness consolidation
Glycogen is primarily stored in astrocytes and serves as an energy reservoir, breaking down into glucose and lactate in response to increased neuronal activity, thereby fueling neuronal metabolism [54]. While direct neuronal glucose uptake [55], mitochondrial function [56], and vascular supply [57] also play essential roles in sustaining energy homeostasis, astrocytes have been identified as key metabolic hubs. Heller and Benington (1995) were the first to hypothesize that the restoration of astrocytic glycogen during NREM sleep is a crucial function of this state [58], counteracting the depletion of cerebral glycogen stores that occurs during wakefulness [59, 60]. However, the observation of increased brain glycogen after sleep deprivation led to the "glycogenetic" hypothesis, which proposes that both glycogen synthesis and utilization increase during wakefulness. At the same time, reduced excitatory transmission during sleep creates an imbalance that causes glycogen accumulation [61]. This suggests that glycogen renewal primarily occurs during wakefulness [62]. Notably, overexpression of glycogen synthase kinase-3 β, a key enzyme in glycogen synthesis results in fragmented wake-sleep states, without affecting the total amount of sleep or wakefulness [63]. Therefore, rather than merely replenishing cellular energy stores, astrocytic glycogen storage and degradation appear to be crucial for maintaining both wakefulness and sleep cycles (Fig. 1). Beyond energy storage, astrocytes also exhibit intracellular dynamic calcium fluctuations, which are essential for modulating neuronal activity, gliotransmission, and sleep–wake transitions.
Calcium signaling in astrocytes and its influence on sleep–wake regulation
Physiological astrocytic Ca2+ fluctuations during the sleep–wake cycle
Growing evidence suggests that intracellular calcium (Ca2 +) signaling in astrocytes play a key role in sleep homeostasis. Recent in vivo imaging studies demonstrated that cortical astroglial Ca2⁺ levels fluctuate across vigilance states, reaching higher levels during wake and lower levels during NREM and REM sleep, with these changes predominantly occurring in astrocytic processes rather than somata [64]. These changes do not appear to simply reflect passive responses to surrounding neuronal activity, as cortical astrocytic Ca2+ displays distinct state-dependent patterns: synchronized activity that peaks during wakefulness [64], while cortical neurons reach peak synchronization during the slow-wave oscillations of deep sleep [65, 66]. Additionally, astrocytic Ca2+ activity exhibits dynamic shits that often precedes changes in neuronal firing patterns, suggesting a proactive role in driving transitions between sleep states [67, 68]. At the cortical level, the frequency of astrocytic Ca2+ events indeed increases just before the onset of slow-wave oscillations, characteristics of deep NREM sleep, a pattern that persists throughout sleep cycles [66]. Notably, further increases in astrocytic Ca2⁺ event frequency occur immediately before the transition into rapid eye movement (REM) sleep, and before awakening [70, 71]. Moreover, individual Ca2+ events in cortical astrocytes tend to be longer during wakefulness than sleep, with both the amplitude and duration of these events varying across wakes and sleep states [69]. Together, these findings suggest that astrocytes not only participate in, but also play an active role in modulating the neural processes underlying sleep–wake transitions and cortical synchrony (Table 1).
The essential role of astrocytic calcium signaling in sleep regulation has also been highlighted by the genetic ablation of the inositol 1,4,5-trisphosphate receptor 2 (IP3R2), a receptor almost exclusively expressed in astrocytes. IP3R2 activation leads to the release of Ca2+ from intracellular stores, particularly the endoplasmic reticulum and at the somatic level and major branches [70]. Its deletion selectively disrupts astrocytic Ca2+ signaling, leading to fragmented NREM sleep and a decrease in delta power during NREM sleep [67]. The involvement of astroglial Ca2+ has also been investigated by suppressing the transmembrane protein STIM1 (Stromal Interaction Molecule 1), which acts as a calcium sensor in the endoplasmic reticulum. When Ca2+ levels decrease in the endoplasmic reticulum, STIM1 is activated and initiates Ca2+ entry through the stores (Store-Operated Calcium Entry, SOCE). Thus, the specific suppression of STIM1 in astrocytes leads to a decrease in NREM sleep activity after sleep deprivation. These results suggest that cortical astrocytic Ca2+ contributes to sleep homeostasis [64].
All these findings underscore the crucial role of astrocytic Ca2+ signaling in sleep regulation (Fig. 1). However, it is noteworthy that these Ca2+ dynamics exhibit regional variability in the brain, particularly during NREM sleep [68, 71, 72]. During REM sleep, astrocyte Ca2+ levels consistently decrease across areas such as the cortex, hippocampus, hypothalamus, and brainstem. Upon waking, a rapid increase in Ca2+ levels occurs. In contrast, during NREM sleep, the changes in Ca2+ levels are more region-specific. In the cortex and hippocampus, Ca2+ levels significantly decrease, whereas in the hypothalamus and brainstem, these levels remain stable compared to wakefulness [68, 71, 72]. Therefore, the physiological role of astrocytes in sleep–wake regulation appears to be brain region-dependent.
Astrocytic Ca2+ variations induced by optogenetic or DREADD stimulations and effects on vigilance states
Recent studies using optogenetic or chemogenetic approaches provided further compelling evidence for the involvement of astrocytes in sleep regulation, revealing region-specific effects. However, while these findings are intriguing, they also raise significant methodological and interpretative challenges.
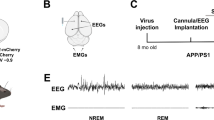
For instance, optogenetic stimulation of astrocytes in the posterior hypothalamus, a region involved in both wakefulness and sleep, transiently increases both NREM and REM sleep duration during circadian periods when rodents are typically awake [73]. Interestingly, this sleep induction did not enhance slow-wave activity, suggesting that astrocytes in this region primarily influence sleep timing and consolidation, rather than the intensity of slow-wave oscillations [73].
In contrast, chemogenetic activation of hippocampal astrocytes reduced the total time in wakefulness, while increasing the total sleep time, without affecting cortical oscillations across sleep–wakefulness states [74]. Conversely, astrocytic stimulation in the pons selectively impairs REM sleep, delaying REM onset and reducing the number of REM episodes. Interestingly, this regional modulation was accompanied by an enhancement of delta wave activity during NREM sleep [74].
Further supporting this regional specificity, targeted optogenetic stimulation of astrocytes in the VLPO, a key center for regulating NREM sleep, increases sleep duration during the active phase of mice [75]. Experiments in brain slices indicate that this astrocytic stimulation in the VLPO can inhibit local interneurons, while simultaneously depolarizing sleep-promoting neurons, suggesting that this astrocytic stimulation may induce the release of a signaling molecule with dual excitatory and inhibitory effects, such as adenosine, to promote sleep [76]. However, it remains unclear whether astrocytic adenosine release follows a physiologically relevant time course or is an artifact of artificial activation.
To further elucidate the role of astrocytic calcium activity, studies of astrocytic calcium dynamics in the cortex revealed that calcium transients in astrocytes precede spontaneous shifts to slow-oscillation states, characteristic of NREM sleep. Moreover, optogenetic activation of cortical astrocytes can trigger these states by altering extracellular glutamate levels [66]. Using two-photon glutamate imaging, studies have also demonstrated under anesthesia that astrocyte-evoked extracellular glutamate spikes coincide with neuronal circuit synchronization [66]. Remarkably, single electrophysiological stimulation of an astrocyte under anesthesia is sufficient to activate nearby astrocytes and induce membrane fluctuations in adjacent neurons, leading to network-driven "UP states", as visualized by two-photon imaging [77].
These findings collectively suggest that astrocytes play an active role in controlling cortical synchronizations, primarily through the modulation of extracellular glutamate, thereby stabilizing neuronal dynamics during sleep [66, 78]. Astrocytes appear capable of enhancing local synchrony without directly increasing cortical excitability to levels associated with wakefulness [77]. During NREM sleep, although cortical astrocytic Ca2⁺ levels are typically low [67], astrocytes nonetheless contribute meaningfully to the oscillatory and highly synchronized states that define this phase [66, 79]. Rather than driving activation, astrocytes support and reinforce the stability of these synchronized networks [77]. Conversely, during wakefulness, cortical astrocytes exhibit high Ca2⁺ levels [64] that are associated with increased extracellular glutamate [66], which promotes neuronal desynchronization, a hallmark of the awake state. This high astrocytic Ca2⁺ activity plays a pivotal role in the regulation of arousal, as it actively supports the dynamic and desynchronized neuronal environment needed for alertness and cognitive processing.
However, interpreting results from optogenetics and chemogenetics studies requires caution, as the frequencies, intensities, and stimulation patterns used in such experiments may exceed physiological levels. Moreover, astrocytes are highly polarized cells, and the abrupt, widespread opening of rhodopsin channels or activation of chemogenetic constructs can represent an artificial activation profile that might not accurately reflect astrocytic signaling.
Activation of cortical astrocytes, artificially and selectively expressing receptors solely activated by synthetic drugs (DREADD), has shown that different astroglial Ca2+ signaling pathways, although convergent, distinctly modulate sleep components. It has thus been demonstrated that cortical activation of Gi-DREADD, which increases the frequency of Ca2+ events, induces an increase in slow-wave activity (SWA) during slow-wave sleep without influencing its duration. Conversely, activation of Gq-DREADD in these astrocytes prolongs the duration of NREM sleep without influencing SWA [68]. Finally, Gq-DREADD activation of basal forebrain astrocytes induces prolonged and uninterrupted periods of wakefulness, without a homeostatic response (increase in sleep duration or intensity), typically observed following sleep deprivation [80].
Altogether, these results highlight the essential role of astrocytic Ca2 + signaling in sleep regulation, not merely as a passive reflection of neuronal activity. However, their precise role appears to be complex and context-dependent. While astrocytic Ca2⁺ activity appears to shape neuronal excitability and network dynamics, whether this occurs primarily through gliotransmission, metabolic support, or modulation of extracellular ionic balance remains an open question. Additionally, the interplay between Ca2⁺ transients and overall Ca2⁺ levels varies regionally, reinforcing the need for spatiotemporal specificity in future investigations. Moreover, the need for sleep may depend not only on how long an individual has been awake, but also on specific patterns of activity within both neuronal and glial circuits. Beyond their role in sleep–wake transitions, astrocytic Ca2⁺ dynamics influence gliotransmitter release, thereby modulating synaptic communication and network synchronization, further reinforcing their role in sleep homeostasis.
Astrocytic modulation of sleep through the release of gliotransmitters and sleep-regulating substances
Gliotransmission, described as the "active transfer of information from glia to neurons", is a complex phenomenon that encompasses various types of signaling and released molecules [81]. Many studies have reported that the release of gliotransmitters occurs via Ca2+-dependent exocytosis of vesicles [82,83,84] and lysosomes [85, 86]. Astrocytes indeed possess all the molecular machinery necessary for exocytosis, including proteins of the soluble N-ethylmaleimide-sensitive factor attachment protein receptor (SNARE) complex [87, 88], vesicular pumps and transporters [89, 90]. Furthermore, studies of astrocyte ultrastructure have revealed the presence of vesicles of various apparent sizes ranging from ~ 100 to 600 nm in diameter [91], as well as the localization of vesicles approximately thirty nanometers in diameter close to synaptic terminals [82]. Other modes of astroglial release not dependent on Ca2+ have also been described, involving the reversal of neurotransmitter transporters' polarity or the opening of hemichannels such as connexins [35] and pannexins [92]. However, the physiological and/or pathological conditions under which these different mechanisms occur remain unclear.
Adenosine
Astrocytes can release numerous molecules, some of which influence the regulation of sleep (Fig. 1). Adenosine release has certainly been the most studied, given the central role of this purine in the homeostatic regulation of sleep [93]. The accumulation of adenosine in the extracellular space is thought to result from the high ATP consumption during wakefulness [94, 95], particularly in brain regions such as the cortex and hippocampus [94, 95], as well as the hypothalamus [7]. This accumulation is believed to encode the need for sleep [58, 96].
Astrocytic exocytosis has long been widely recognized as a key mechanism involved in the release of adenosine by astrocytes, particularly in the regulation of sleep homeostasis. Early evidence supporting this hypothesis comes from studies using mutant mice expressing a dominant-negative form of the SNARE complex in astrocytes (dnSNARE), in which “astrocyte-specific” expression was shown to impair sleep homeostasis after sleep deprivation, of both NREM sleep and REM sleep duration, while control mice exhibited increased duration of sleep and episodes of deep NREM sleep following sleep deprivation [97]. However, subsequent studies have challenged the specificity of this model, based on the GFAP promoter used in these SNARE mice, which was found to leaky expression in neurons, that could confound interpretations of astrocyte-derived adenosine signaling [98]. Furthermore, direct measurements of extracellular adenosine levels using adenosine sensors of the G protein-coupled receptor activation-based type (GRAB-Ado), raised questions about whether astrocytes are the primary source of adenosine in sleep regulation. It has indeed been shown that in the basal forebrain, neurons, rather than astrocytes, represent an important source of adenosine [99]. Although the level of Ca2+ in astrocytes is positively correlated with the amount of extracellular adenosine, experimental suppression of astrocytic Ca2⁺ transients had no effect on adenosine levels in the basal forebrain [100]. This suggests that astrocytes may influence adenosine metabolism or transport, but their direct contribution to extracellular adenosine release remains unclear.
Additionally, adenosine production via ATP release from astrocytes may occur independently of Ca2-mediated exocytosis, as IP3R2-KO mice still exhibit Ca2+ transients in astrocytic processes, which may be crucial for adenosine production. Supporting this, optogenetic stimulation of VLPO astrocytes, known to increase sleep duration, has been shown to trigger ATP release by hemichannels and/or P2X7 receptors [75]. This ATP is subsequently degraded into adenosine by local interneurons through the activation of the Tissue-nonspecific Alkaline Phosphatase (TNAP) enzyme [76] (Table 1).
Taken together, these findings suggest that while astrocytes may play a role in adenosine homeostasis, their function as a primary source of adenosine release remains debated. The discrepancy between dnSNARE-based studies and direct adenosine measurements highlights the need for more refined transgenic models with improved cell-type specificity. Future research should aim to clarify the regional specificity of astrocytic ATP-to-adenosine conversion, particularly in sleep-regulating areas such as the VLPO and basal forebrain. It is also essential to distinguish between direct astrocytic adenosine release and the modulation of extracellular adenosine levels through ATP hydrolysis. Additionally, advancing high-resolution, real-time imaging techniques will be crucial for tracking adenosine dynamics in vivo across different sleep–wake states.
In vitro enzymatic measurements of adenosine levels further indicate that adenosine, once released into the extracellular space, also accumulates in the VLPO during wakefulness to exert sleep pressure [7]. Furthermore, astrocytes exhibit a time-depend regulation of their response to glucose and adenosine production, acting as temporal integrators. Thus, the same variation in glucose concentration in the VLPO induces a threefold increase in adenosine release at the beginning of the rest period compared to the end [7]. Adenosine promotes sleep by modulating neuronal excitability across multiple brain regions via A1 and A2A adenosine receptors (A1R and A2AR), which exert inhibitory and excitatory effects, respectively (for review, see [101]). In the VLPO, in vitro studies have shown that adenosine indirectly disinhibits sleep-promoting neurons by inhibiting local interneurons [7, 102], while also directly stimulating sleep-promoting neurons via A2A receptor activation [76, 103]. However, since sleep-promoting neurons also express A1 receptors, as local interneurons [7, 104], specific injection of adenosine A1R agonists into the VLPO increases wakefulness [105] (Fig. 2). Notably, the A2AR/A1R expression ratio on sleep-promoting neurons appears to be species-dependent. In rats, adenosine application inhibits sleep-promoting neurons [104], whereas in mice, it induces depolarization [7] (Table 1), emphasizing the need for species-specific investigation into adenosinergic regulation of sleep.
Schematic representation of adenosine origin and mode of action in the VLPO. Following astrocytic activation, intracellular Ca2 + levels increase, leading to the release of ATP via hemichannels or P2X7 receptors (1). This ATP is then cleaved into adenosine by tissue-nonspecific alkaline phosphatase (TNAP) enzymes (2) located on local interneurons. The adenosine (3) acts on A1R on these interneurons, reducing their inhibitory action on sleep-promoting neurons (4). Simultaneously, adenosine inhibits sleep-promoting neurons through A1R and activates them via A2AR, which are more highly expressed
Prostaglandin D2
Astrocytes play a key role in sleep regulation through the release of prostaglandins, notably prostaglandin D2 (PGD2) [106] and prostaglandin E2 [107]. These releases are regulated by Ca2+ oscillations within astrocytes [108]. Among these molecules, PGD2 is one of the most potent endogenous sleep-promoting molecules [103], with its concentration in the cerebrospinal fluid fluctuating according to the circadian rhythm of wakefulness and sleep [109, 110]. Astrocytes also express the DP1 receptor for PGD2, enabling them to respond to PGD2 activation. This interaction enhances extracellular adenosine concentrations, thereby simultaneously adjusting blood flow and neuronal activity within the VLPO [103]. Through these mechanisms, astrocytes effectively integrate metabolic and neuronal signals to regulate sleep–wake dynamics.
Lactate
Astrocytes can release lactate, the extracellular variations of which fluctuate during wake-sleep cycles [63, 108]. A mechanism known as the astrocyte-neuron lactate shuttle (ANLS) has been proposed to play a fundamental role in sleep regulation by linking neuronal activity to energy supply [31]. According to this mechanism, astrocytes take up glutamate released during neuronal activity and convert it into lactate for subsequent release, directly linking neuronal activity to lactate energy supply by astrocytes. Neurons are, however, directly sensitive to glucose [55] and may even prefer glucose over lactate as the primary energy source during periods of sustained activity [111]. Nevertheless, beyond the metabolic role of lactate, its release by astrocytes could directly contribute to the slowing of cortical neuron discharge while falling asleep [112]. Another effect of lactate on neurons has been reported by Yang and colleagues, who showed that genes related to neuronal plasticity such as Arc and Zif268 were stimulated in vitro and in vivo by lactate application [113]. This increase is thought to be mediated by NMDA receptor activation and the Erk1/2 signaling pathway [113]. Unlike the direct electrophysiological effects of lactate, lactate transport via monocarboxylate transporters (MCTs) is necessary to exert its effects [114]. These results indicate that, at the level of a single synapse, lactate could simultaneously support synaptic activity as an energy substrate and directly participate in activity-related plasticity mechanisms by triggering the transcription of plasticity-related genes. These lactate effects could contribute to memory mechanisms associated with sleep.
Neurotransmitters
Astrocytes can release glutamate via exocytosis, a process dependent on Ca2+ [3, 71], which involves a specific subpopulation of astrocytes expressing the vesicular glutamate transporter VGLUTs [115]. This release can also be modulated by changes in cell volume, thereby activating glutamate-permeable channels [116]. Moreover, exocytosis in astrocytes is stimulated by morphological changes induced by cyclic AMP, leading to increased glutamate release [117]. Ex-vivo experiments on brain slices demonstrated that this astrocyte-derived glutamate release promotes neuronal synchronization, a hallmark of NREM sleep [66].
Astrocytes also play a role in sleep physiology, particularly through the regulation of GABAergic signaling. They actively participate in the uptake of GABA, a neurotransmitter that plays a key role in sleep regulation [118]. In mammals, GABAergic neurons, within key sleep-regulating regions such as the median preoptic nucleus (MnPO), VLPO nuclei, suprachiasmatic nucleus (SCN), and parafacial zone [119], play a crucial role in the induction and maintenance of NREM sleep. The GABAergic nature of these neurons underscores the importance of astrocytic GABA uptake in fine-tuning sleep architecture. Astrocytes influence sleep onset and duration by modulating extracellular GABA levels. Pharmacological inhibition of the GABA transporter-1 (GAT-1), a key astrocytic transporter, shortens the latency to NREM sleep onset while simultaneously increasing the duration of NREM sleep and the number of sleep episodes [118]. These findings suggest that astrocytes regulate the availability of GABA at synapses, ensuring proper inhibitory tone necessary for sleep initiation and maintenance.
Similarly, in Drosophila, astrocytic regulation of extracellular GABA levels has emerged as a key mechanism in sleep regulation. The hypomorphic mutation gat (gat33-1) in the GAT-1 gene, encoding the astrocytic GABA transporter, leads to increased sleep duration and consolidation while reducing the latency to sleep onset [120]. These effects are attributed to an increase in extracellular GABA, which dampens the activity of wake-promoting circadian neurons, further reinforcing the conserved role of astrocytic GABAergic signaling in sleep regulation across species.
Together, these findings highlight the essential contribution of astrocytes to sleep homeostasis via GABAergic modulation. By controlling extracellular GABA levels, astrocytes not only regulate the balance between wakefulness and sleep, but also influence the stability and consolidation of sleep states. This underscores the need for further research into astrocytic GABA dynamics, particularly in different brain regions, to fully understand their region-specific contributions to sleep physiology.
Cytokines
Astrocytes play a significant role in regulating sleep, in part through the release of cytokines, such as interleukin 1 (IL-1). While astrocytes are a source of IL-1β, this cytokine is not exclusively produced by astrocytes; it is also expressed in microglia and, to a lesser extent, neurons [121]. Studies have shown that IL-1β mRNA levels exhibit diurnal fluctuations in sleep-regulatory brain regions. In the hypothalamus, hippocampus, and cortex, IL-1β mRNA levels peak shortly after the lights-on, decline during the reminder of the light period, and stay low during the dark phase [122]. In contrast, no significant changes in IL-1β mRNA levels were observed in the brainstem or cerebellum. These regional variations in IL-1β mRNA expression suggest a region-specific role for IL-1β in sleep–wake regulation. The cellular origin of these IL-1β mRNA fluctuations remains unclear, as both astrocytes and neurons express IL-1β mRNA in the brain. However, astrocytes are thought to be key contributors to IL-1β-mediated sleep regulation. Indeed, when IL-1β derived from cultured astrocytes are injected into the ventricles of rats, there is an increase in slow-wave sleep activity [123]. Similarly, the inhibition of IL-1 and TNF-α via antibodies or antagonists has been found to reduce slow-wave sleep, whereas their administration increases it [123, 124]. Recent in vivo research provides deeper insight into these processes. In transgenic mice that express IL-1 receptor 1 (IL1R1) selectively in the central nervous system and either on neurons or astrocytes, it was shown that in mice with IL-1 receptor 1 (IL1R1) expressed on astrocytes exhibit greater sleep fragmentation and delayed increases in NREM delta power compared to those with IL1R1 expressed on neurons [125]. Additionally, research in fruit flies demonstrates that calcium signaling in astrocytes can promote sleep by upregulating the expression of the monoamine receptor TyrRII and triggering the release of Spätzle, an IL-1 analog, which activates sleep-promoting neurons [126]. Together, these findings underscore a crucial, cell-specific role for astrocyte-derived IL-1 signaling in sleep regulation, further linking immune responses to sleep modulation in both mammals and invertebrates.
BDNF
The case of Brain-Derived Neurotrophic Factor (BDNF) is interesting because it is primarily synthesized by neurons, then internalized, matured, and finally released by astrocytes [127]. In addition to a role in cell growth and synaptic long-term potentiation (LTP), BDNF appears to be involved in sleep homeostasis. Studies have shown in mice that intracortical injection of BDNF at the beginning of the wake period increases the intensity of slow-wave sleep, measured by slow-wave activity (SWA) [128]. Conversely, in transgenic rats with a 50% reduction in BDNF levels, the duration of slow-wave sleep episodes is decreased [129]. Loss of BDNF expression dependent on the BDNF promoter IV has also been associated with decreased SWA during slow-wave sleep, suggesting altered sleep homeostasis [130].
BDNF exerts its effects via its receptor, tropomyosin-related kinase B (TrkB), which exists in two main isoforms: TrkB.FL, predominantly expressed by neurons, and TrkB.T1, the truncated isoform predominantly found in astrocytes [131]. TrkB.T1 lacks the intracellular tyrosine kinase domain. To explore the specific role of astrocytes and the TrkB.T1 receptor in sleep, researchers examined sleep patterns in mice genetically modified to lack TrkB.T1. These TrkB.T1-null mice exhibit normal NREM sleep time and NREM sleep homeostasis [132]. However, they display several alterations commonly observed in mood disorders. These include increased REM sleep time, reduced REM sleep latency, and sleep fragmentation, characterized by shorter bouts of both sleep and wakefulness episodes similar to those seen in major depressive disorders [132].
These results suggest that astrocytic TrkB.T1 plays a role in maintaining sleep integrity and may provide a molecular link between sleep abnormalities and psychiatric conditions. As astrocytes are also known to release a variety of other gliotransmitters in response to local brain activity [133], the full spectrum of their influence on sleep remains to be fully elucidated. This growing body of evidence underscores the importance of astrocyte-mediated BDNF signaling in sleep regulation and the broader context of brain health.
Synaptic regulation by astrocytes: pruning, plasticity, and sleep-associated downscaling
Astrocytes play a crucial role in maintaining synaptic homeostasis in the adult brain by regulating synaptic pruning through phagocytosis. In the hippocampus, astrocytes eliminate unnecessary excitatory synapses via the phagocytic receptor MEGF10, while inhibitory synapses are spared [134]. In the cerebellum, Bergmann glial cells utilize ABCA1, another phagocytic receptor, to regulate synapse size rather than reduce synapse numbers [135]. Additionally, in the cerebral cortex, astrocytes are involved in the elimination of presynaptic elements, especially under conditions like sleep deprivation, where increased astrocytic expression of the receptor MERTK is observed and increased lipid peroxidation in synaptoneurosomes [16]. These findings suggest that astrocytic phagocytosis may represent the brain’s adaptive response to the heightened synaptic activity during prolonged wakefulness. This process likely facilitates the maintenance of neural homeostasis by clearing worn-out components from heavily utilized synapses. Future research is needed to determine how astrocytic receptors MEGF10, ABCA1, and MERTK differentially recognize and control the pruning of different synapse types across various neural circuits [135,136,137].
The interactions between astrocytes and neurons also enable astrocytes to play a role in regulating long-term synaptic plasticity (LTP and LTD) [17, 138]. Their ability to form a more or less extensive astrocytic network, along with the regulation of the proximity of their processes to synapses, modulates the volume of the extracellular space and their capacity to regulate extracellular levels of glutamate and potassium. It has also been hypothesized that TNFα release by astrocytes could mediate the signaling pathways involved in sleep-associated synaptic weakening [139]. However, since the in vitro effects of TNFα on glutamatergic and GABAergic synapses are diverse [140, 141], it remains unclear whether glial-derived TNFα signaling provides a plausible molecular mechanism for synaptic weakening during sleep.
During deep slow-wave sleep, a crucial process of pruning and reducing synaptic connections in the brain has been hypothesized to be essential for cognitive health and memory. The Synaptic Homeostasis Hypothesis (SHY), primarily formulated by Giulio Tononi and Chiara Cirelli, suggests that deep slow-wave sleep plays a regulatory role in adjusting cerebral synaptic weights [142]. According to this hypothesis, during wakefulness, synapses are strengthened by learning and experiences, a fundamental process for memory formation. However, continuous increases in synaptic activity, without regulation, could lead to synaptic saturation and increased energy expenditure. Sleep, particularly during deep slow-wave sleep, may then serve as a "reset" for synapses, reducing their activity through a process of "downscaling" (Fig. 1). The SHY hypothesis predicts that this downscaling is not uniform for all synapses, but that some, those associated with "memories", are protected and remain stable during sleep [143]. This mechanism preserves essential information acquired throughout the day while eliminating excess connections, thus enabling new learning possibility every day. In a way, sleep is the price we pay for learning and memory formation. However, while it has been well established that astrocytes play a crucial role in modulating synaptic activity and plasticity, neurons also actively participate in this process through synaptic tagging, and activity-dependent modifications. Their coordinated interactions with astrocytes ensure appropriate synaptic downscaling and memory consolidation. However, the precise molecular interplay between astrocytic and neuronal contributions to synaptic weakening during sleep—essential for cognitive function, memory consolidation, and overall brain health—remains an open question that requires further investigation.
Conclusion
Long underestimated, the role of astrocytes in sleep regulation now appears to be undeniable. These cells are dynamic elements, fully equipped to integrate local information. Astrocytes act as integrators of energy metabolism, sleep pressure, and circadian timing to appropriately regulate and coordinate neuronal activities, neuronal networks, and sleep thanks to gene transcription, Ca2+ signaling pathways, their function as energy reservoirs, synaptic coverage plasticity, gliotransmission, and their ability to regulate long-term synaptic efficiency.
Developmental dynamics and astrocytic heterogeneity
The role of astrocytes evolves throughout life, encompassing various functions from development to senescence [144, 145]. During these extreme periods of life, both astrocytes function and sleep architecture undergo significant changes, highlighting the need for further research into how astrocytes contribute to sleep regulation over time. Moreover, astrocytes are not a uniform population. They exhibit marked heterogeneity across brain regions and subtypes, reflecting not only developmental origins, but also regional specialization and evolutionary influences [146]. This diversity likely translates into region-specific contributions to sleep regulation, as astrocytes in different brain areas express distinct receptors, as well as the brain regions where they are located.
For instance, cortical astrocytes have been shown to modulate slow-wave activity (SWA) during NREM sleep by regulating extracellular glutamate levels and promoting neuronal synchronization [66]. Conversely, astrocytes in the basal forebrain appear to be critical for wakefulness maintenance, as their stimulation leads to prolonged arousal without triggering compensatory sleep rebound [69]. Similarly, astrocytes in the VLPO, are thought to enhance NREM sleep through adenosine release, which exerts differential effects on wake-active and sleep-promoting neurons [76, 103].
Beyond these region-specific functions, astrocytes also play a role in sleep homeostasis, with their intracellular Ca2⁺ dynamics encoding sleep need. Studies have demonstrated that astrocytic Ca2⁺ activity is highest during wakefulness and decreases during sleep, particularly in response to prolonged wake states, suggesting a potential role in sleep pressure accumulation and discharge [64]. However, the extent to which astrocytes directly drive sleep–wake transitions versus supporting neuronal circuits in regulating these states remains an open question.
Ongoing research into the morphological, molecular and functional heterogeneity of astrocytes could further shed light on their specific implications for sleep regulation, which will be crucial for deciphering their precise roles in neural network dynamics and sleep homeostasis [147,148,149].
Technical and methodological challenges in astrocyte research
Despite the growing recognition of astrocytes in sleep regulation, significant methodological challenges persist in accurately dissecting their contributions. One major limitation is the difficulty in isolating astrocyte-specific functions due to their intricate interactions with neurons, microglia, and vascular cells. The use of genetic tools such as Cre-loxP systems, optogenetics, and chemogenetics has provided invaluable insights, but many of these approaches lack absolute specificity, as promoters commonly used in astrocytic transgenic models can also be active in neurons. This overlap complicates the interpretation of results and necessitates refined techniques to achieve selective astrocyte manipulation.
Additionally, the spatial and temporal resolution of current imaging technologies still presents challenges in capturing astrocytic dynamics in vivo. Genetically encoded calcium indicators and neurotransmitter sensors have improved our ability to visualize astrocytic activity, yet they remain limited in resolving fine-scale astrocyte-neuron interactions. The integration of advanced techniques such as single-cell transcriptomics, super-resolution microscopy, and spatial proteomics may offer deeper insights into astrocytic heterogeneity and their distinct functional roles in sleep.
Another key challenge is the interpretation of data from in vitro versus in vivo studies. While in vitro models enable precise manipulation of astrocytic pathways, they lack the complexity of intact neural networks, including interactions with neurons and the vascular system. Conversely, in vivo studies provide a physiologically relevant context but are constrained by the invasive nature of imaging and electrophysiological techniques. Given that astrocytes play regionally specific roles in synaptic and metabolic regulation, findings from one brain area may not be directly generalizable to others, emphasizing the need for context-specific experimental approaches.
Implications for sleep pathologies and future research
Finally, although the role of astrocytes in sleep-associated pathologies is not addressed in this review, it is important to highlight that astrocytes are also contributing to neuroinflammation, phagocytosis, and reactive gliosis, processes intimately linked to sleep disorders and neurodegenerative diseases [150]. Their ability to modulate inflammatory cascades suggests that they may play a pivotal role in pathological sleep disturbances, including insomnia, hypersomnia, and sleep fragmentation in neurodegenerative conditions [150, 151].
As sleep disorders affect over a third of the population and pose a significant societal and health burden, understanding astrocytic contributions to sleep regulation is essential. Future research should aim to refine experimental strategies that improve astrocyte specificity while considering their interactions with other glial cells and neuronal circuits. Advancements in imaging techniques, multi-omics approaches, and targeted pharmacological interventions may pave the way for novel therapeutic strategies aimed at restoring sleep homeostasis through astrocytic modulation.
Data availability
The datasets supporting this study are available from the website of PubMed (https://pubmed.ncbi.nlm.nih.gov/).
References
von Lenhossek M (1895) Der Feinere Bau des Nervensystems im Lichte neuester Forchungen. Fischer’s Medicinische Buchhandlung H Kornfiel, Berlin, pp 177–245
Cornell-Bell AH, Finkbeiner SM, Cooper MS (1979) Smith SJ (1990) Glutamate induces calcium waves in cultured astrocytes: long-range glial signaling. Science 247:470–473. https://doi.org/10.1126/science.1967852
Ramon y Cajal S (1899) Contribucion al conocimiento de la neuroglia del cerebro humano. Trabajos del Laboratorio de Investigaciones Biologicas de la Universidad de Madrid.
Bellesi M, de Vivo L, Tononi G, Cirelli C (2015) Effects of sleep and wake on astrocytes: clues from molecular and ultrastructural studies. BMC Biol 13:66. https://doi.org/10.1186/s12915-015-0176-7
Araque A, Parpura V, Sanzgiri RP, Haydon PG (1999) Tripartite synapses: glia, the unacknowledged partner. Trends Neurosci 22:208–215. https://doi.org/10.1016/S0166-2236(98)01349-6
Filosa JA, Iddings JA (2013) Astrocyte regulation of cerebral vascular tone. Am J Physiol Heart Circ Physiol 305:H609–H619. https://doi.org/10.1152/ajpheart.00359.2013
Scharbarg E, Daenens M, Lemaître F et al (2016) Astrocyte-derived adenosine is central to the hypnogenic effect of glucose. Sci Rep 6:19107. https://doi.org/10.1038/srep19107
Iadecola C (2017) The neurovascular unit coming of age: a journey through neurovascular coupling in health and disease. Neuron 96:17–42. https://doi.org/10.1016/j.neuron.2017.07.030
Simard M, Nedergaard M (2004) The neurobiology of glia in the context of water and ion homeostasis. Neuroscience 129:877–896. https://doi.org/10.1016/j.neuroscience.2004.09.053
Song Y, Gunnarson E (2012) Potassium dependent regulation of astrocyte water permeability is mediated by cAMP signaling. PLoS ONE 7:e34936. https://doi.org/10.1371/journal.pone.0034936
Dringen R, Gutterer JM, Hirrlinger J (2000) Glutathione metabolism in brain. Eur J Biochem 267:4912–4916. https://doi.org/10.1046/j.1432-1327.2000.01597.x
Augusto-Oliveira M, Arrifano GP, Takeda PY et al (2020) Astroglia-specific contributions to the regulation of synapses, cognition and behaviour. Neurosci Biobehav Rev 118:331–357
Schiweck J, Murk K, Ledderose J et al (2021) Drebrin controls scar formation and astrocyte reactivity upon traumatic brain injury by regulating membrane trafficking. Nat Commun 12:1490. https://doi.org/10.1038/s41467-021-21662-x
Fawcett JW, RichardA A (1999) The glial scar and central nervous system repair. Brain Res Bull 49:377–391. https://doi.org/10.1016/S0361-9230(99)00072-6
Giovannoni F, Quintana FJ (2020) The role of astrocytes in CNS inflammation. Trends Immunol 41:805–819. https://doi.org/10.1016/j.it.2020.07.007
Bellesi M, De VL, Chini M et al (2017) Sleep loss promotes astrocytic phagocytosis and microglial activation in mouse cerebral cortex. J Neurosci 37:5263–5273. https://doi.org/10.1523/JNEUROSCI.3981-16.2017
Hardy E, Moulard J, Walter A et al (2023) Upregulation of astroglial connexin 30 impairs hippocampal synaptic activity and recognition memory. PLoS Biol. https://doi.org/10.1371/journal.pbio.3002075
Dossi E, Zonca L, Pivonkova H et al (2024) Astroglial gap junctions strengthen hippocampal network activity by sustaining afterhyperpolarization via KCNQ channels. Cell Rep 43:114158. https://doi.org/10.1016/j.celrep.2024.114158
Chever O, Dossi E, Pannasch U et al (2016) Astroglial networks promote neuronal coordination. Sci Signal 9:1–9. https://doi.org/10.1126/scisignal.aad3066
Pannasch U, Vargová L, Reingruber J et al (2011) Astroglial networks scale synaptic activity and plasticity. Proc Natl Acad Sci U S A 108:8467–8472. https://doi.org/10.1073/pnas.1016650108
Broadhead MJ, Miles GB (2021) A common role for astrocytes in rhythmic behaviours? Prog Neurobiol. https://doi.org/10.1016/j.pneurobio.2021.102052
Montalant A, Carlsen EMM, Perrier J (2021) Role of astrocytes in rhythmic motor activity. Physiol Rep 9:15029
Morquette P, Verdier D, Kadala A et al (2015) An astrocyte-dependent mechanism for neuronal rhythmogenesis. Nat Neurosci. https://doi.org/10.1038/nn.4013
Bass J (1979) Takahashi JS (2010) Circadian integration of metabolism and energetics. Science 330:1349–1354. https://doi.org/10.1126/science.1195027
Brancaccio M, Patton AP, Chesham JE et al (2017) Astrocytes control circadian timekeeping in the suprachiasmatic nucleus via glutamatergic signaling. Neuron 93:1420-1435.e5. https://doi.org/10.1016/j.neuron.2017.02.030
Patton AP, Morris EL, McManus D et al (2023) Astrocytic control of extracellular GABA drives circadian timekeeping in the suprachiasmatic nucleus. Proc Natl Acad Sci. https://doi.org/10.1073/pnas.2301330120
Morf J, Rey G, Schneider K et al (1979) (2012) Cold-inducible RNA-binding protein modulates circadian gene expression posttranscriptionally. Science 338:379–383. https://doi.org/10.1126/science.1217726
Pannasch U, Freche D, Dallérac G et al (2014) Connexin 30 sets synaptic strength by controlling astroglial synapse invasion. Nat Neurosci 17:549–558. https://doi.org/10.1038/nn.3662
Arai Y, Funatsu N, Numayama-Tsuruta K et al (2005) Role of Fabp7, a downstream gene of Pax6, in the maintenance of neuroepithelial cells during early embryonic development of the rat cortex. J Neurosci 25:9752–9761. https://doi.org/10.1523/JNEUROSCI.2512-05.2005
Gerstner JR, Perron IJ, Riedy SM et al (2017) Normal sleep requires the astrocyte brain-type fatty acid binding protein FABP7. Sci Adv. https://doi.org/10.1126/sciadv.1602663
Petit J-M, Gyger J, Burlet-Godinot S et al (2013) Genes involved in the astrocyte-neuron lactate shuttle (ANLS) are specifically regulated in cortical astrocytes following sleep deprivation in mice. Sleep 36:1445–1458. https://doi.org/10.5665/sleep.3034
Heller JP, Rusakov DA (2015) Morphological plasticity of astroglia: Understanding synaptic microenvironment. Glia 63:2133–2151. https://doi.org/10.1002/glia.22821
Lavialle M, Aumann G, Anlauf E et al (2011) Structural plasticity of perisynaptic astrocyte processes involves ezrin and metabotropic glutamate receptors. Proc Natl Acad Sci U S A 108:12915–12919. https://doi.org/10.1073/pnas.1100957108
Mazaud D, Capano A, Rouach N (2021) The many ways astroglial connexins regulate neurotransmission and behavior. Glia 69:2527–2545. https://doi.org/10.1002/glia.24040
Yang S, Kong X-Y, Hu T et al (2022) Aquaporin-4, connexin-30, and connexin-43 as biomarkers for decreased objective sleep quality and/or cognition dysfunction in patients with chronic insomnia disorder. Front Psychiatry 13:1–9. https://doi.org/10.3389/fpsyt.2022.856867
Clasadonte J, Scemes E, Wang Z et al (2017) Connexin 43-mediated astroglial metabolic networks contribute to the regulation of the sleep-wake cycle. Neuron 95:1365-1380.e5. https://doi.org/10.1016/j.neuron.2017.08.022
Liu X, Petit J-M, Ezan P et al (2013) The psychostimulant modafinil enhances gap junctional communication in cortical astrocytes. Neuropharmacology 75:533–538. https://doi.org/10.1016/j.neuropharm.2013.04.019
Guan X, Cravatt BF, Ehring GR et al (1997) The sleep-inducing lipid oleamide deconvolutes gap junction communication and calcium wave transmission in glial cells. J Cell Biol 139:1785–1792. https://doi.org/10.1083/jcb.139.7.1785
Mayorquin LC, Rodriguez AV, Sutachan J-J, Albarracín SL (2018) Connexin-mediated functional and metabolic coupling between astrocytes and neurons. Front Mol Neurosci. https://doi.org/10.3389/fnmol.2018.00118
Ribot J, Breton R, Calvo C-F et al (1979) (2021) Astrocytes close the mouse critical period for visual plasticity. Science 373:77–81. https://doi.org/10.1126/science.abf5273
Hardy E, Cohen-Salmon M, Rouach N, Rancillac A (2021) Astroglial Cx30 differentially impacts synaptic activity from hippocampal principal cells and interneurons. Glia 69:2178–2198. https://doi.org/10.1002/glia.24017
Kang J-E, Lim MM, Bateman RJ et al (1979) (2009) Amyloid-β dynamics are regulated by orexin and the sleep-wake cycle. Science 326:1005–1007. https://doi.org/10.1126/science.1180962
Roh JH, Huang Y, Bero AW et al (2012) Disruption of the sleep-wake cycle and diurnal fluctuation of β-amyloid in mice with Alzheimer’s disease pathology. Sci Transl Med. https://doi.org/10.1126/scitranslmed.3004291
Astara K, Tsimpolis A, Kalafatakis K et al (2024) Sleep disorders and Alzheimer’s disease pathophysiology: the role of the Glymphatic System A scoping review. Mech Ageing Dev 217:111899. https://doi.org/10.1016/J.MAD.2023.111899
Xie L, Kang H, Xu Q et al (1979) (2013) Sleep drives metabolite clearance from the adult brain. Science 342:373–377. https://doi.org/10.1126/science.1241224
Sriram S, Carstens K, Dewing W, Fiacco TA (2024) Astrocyte regulation of extracellular space parameters across the sleep-wake cycle. Front Cell Neurosci. https://doi.org/10.3389/fncel.2024.1401698
Miao A, Luo T, Hsieh B et al (2024) Brain clearance is reduced during sleep and anesthesia. Nat Neurosci 27:1046–1050. https://doi.org/10.1038/s41593-024-01638-y
Dibas AI, Mia AJ, Yorio T (1998) Aquaporins (water channels): role in vasopressin-activated water transport. Exp Biol Med 219:183–199. https://doi.org/10.3181/00379727-219-44332
Verkman AS, Binder DK, Bloch O et al (2006) Three distinct roles of aquaporin-4 in brain function revealed by knockout mice. Biochimica et Biophysica Acta BBA Biomembranes 1758:1085–1093. https://doi.org/10.1016/j.bbamem.2006.02.018
Bork PAR, Ladrón-de-Guevara A, Christensen AH et al (2023) Astrocyte endfeet may theoretically act as valves to convert pressure oscillations to glymphatic flow. J R Soc Interface. https://doi.org/10.1098/rsif.2023.0050
Gan Y, Holstein-Rønsbo S, Nedergaard M et al (2023) Perivascular pumping of cerebrospinal fluid in the brain with a valve mechanism. J R Soc Interface. https://doi.org/10.1098/rsif.2023.0288
Iliff JJ, Wang M, Liao Y et al (2012) A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes including amyloid β. Sci Transl Med. https://doi.org/10.1126/scitranslmed.3003748
Hauglund NL, Andersen M, Tokarska K et al (2025) Norepinephrine-mediated slow vasomotion drives glymphatic clearance during sleep. Cell 188:606-622.e17. https://doi.org/10.1016/j.cell.2024.11.027
Brown AM, Ransom BR (2007) Astrocyte glycogen and brain energy metabolism. Glia 55:1263–1271. https://doi.org/10.1002/glia.20557
Varin C, Rancillac A, Geoffroy H et al (2015) Glucose induces slow-wave sleep by exciting the sleep-promoting neurons in the ventrolateral preoptic nucleus: a new link between sleep and metabolism. J Neurosci 35:9900–9911. https://doi.org/10.1523/JNEUROSCI.0609-15.2015
Melhuish Beaupre LM, Brown GM, Braganza NA et al (2022) Mitochondria’s role in sleep: novel insights from sleep deprivation and restriction studies. World J Biol Psychiatry 23:1–13. https://doi.org/10.1080/15622975.2021.1907723
Cherubini JM, Cheng JL, Williams JS, MacDonald MJ (2021) Sleep deprivation and endothelial function: reconciling seminal evidence with recent perspectives. Am J Physiol Heart Circ Physiol 320:H29–H35. https://doi.org/10.1152/ajpheart.00607.2020
Benington JH, Heller HC (1995) Restoration of brain energy metabolism as the function of sleep. Prog Neurobiol 45:347–360. https://doi.org/10.1016/0301-0082(94)00057-O
Kong J, Shepel PN, Holden CP et al (2002) Brain glycogen decreases with increased periods of wakefulness: implications for homeostatic drive to sleep. J Neurosci 22:5581–5587. https://doi.org/10.1523/JNEUROSCI.22-13-05581.2002
Karnovsky ML, Reich P, Anchors JM, Burrows BL (1983) Changes in brain glycogen during slow-wave sleep in the rat. J Neurochem 41:1498–1501. https://doi.org/10.1111/j.1471-4159.1983.tb00853.x
Petit J-M, Burlet-Godinot S, Magistretti PJ, Allaman I (2015) Glycogen metabolism and the homeostatic regulation of sleep. Metab Brain Dis 30:263–279. https://doi.org/10.1007/s11011-014-9629-x
Morgenthaler FD, Lanz BR, Petit J-M et al (2009) Alteration of brain glycogen turnover in the conscious rat after 5h of prolonged wakefulness. Neurochem Int 55:45–51. https://doi.org/10.1016/j.neuint.2009.02.023
Ahnaou A, Drinkenburg WHIM (2011) Disruption of glycogen synthase kinase-3-beta activity leads to abnormalities in physiological measures in mice. Behav Brain Res 221:246–252. https://doi.org/10.1016/j.bbr.2011.03.004
Ingiosi AM, Hayworth CR, Harvey DO et al (2020) A role for astroglial calcium in mammalian sleep and sleep regulation. Curr Biol 30:4373-4383.e7. https://doi.org/10.1016/j.cub.2020.08.052
Vyazovskiy VV, Olcese U, Lazimy YM et al (2009) Cortical firing and sleep homeostasis. Neuron 63:865–878. https://doi.org/10.1016/j.neuron.2009.08.024
Poskanzer KE, Yuste R (2016) Astrocytes regulate cortical state switching in vivo. Proc Natl Acad Sci 113:1–10. https://doi.org/10.1073/pnas.1520759113
Bojarskaite L, Bjørnstad DM, Pettersen KH et al (2020) Astrocytic Ca2+ signaling is reduced during sleep and is involved in the regulation of slow wave sleep. Nat Commun 11:3240. https://doi.org/10.1038/s41467-020-17062-2
Vaidyanathan TV, Collard M, Yokoyama S et al (2021) Cortical astrocytes independently regulate sleep depth and duration via separate GPCR pathways. Elife 10:1–55. https://doi.org/10.7554/eLife.63329
Ingiosi AM, Frank MG (2023) Goodnight, astrocyte: waking up to astroglial mechanisms in sleep. FEBS J 290:2553–2564. https://doi.org/10.1111/febs.16424
Srinivasan R, Huang BS, Venugopal S et al (2015) Ca2+ signaling in astrocytes from Ip3r2 -/- mice in brain slices and during startle responses in vivo. Nat Neurosci 18:708–717. https://doi.org/10.1038/nn.4001
Tsunematsu T, Sakata S, Sanagi T et al (2021) Region-specific and state-dependent astrocyte Ca 2+ dynamics during the sleep-wake cycle in mice. J Neurosci 41:5440–5452. https://doi.org/10.1523/JNEUROSCI.2912-20.2021
Steriade M (2000) Corticothalamic resonance, states of vigilance and mentation. Neuroscience 101:243–276. https://doi.org/10.1016/S0306-4522(00)00353-5
Pelluru D, Konadhode RR, Bhat NR, Shiromani PJ (2016) Optogenetic stimulation of astrocytes in the posterior hypothalamus increases sleep at night in C57BL/6J mice. Eur J Neurosci 43:1298–1306. https://doi.org/10.1111/ejn.13074
Kurogi Y, Sanagi T, Ono D, Tsunematsu T (2024) Chemogenetic activation of astrocytes modulates sleep–wakefulness states in a brain region-dependent manner. Sleep Adv. https://doi.org/10.1093/sleepadvances/zpae091
Kim J-H, Choi I-S, Jeong J-Y et al (2020) Astrocytes in the ventrolateral preoptic area promote sleep. J Neurosci 40:8994–9011. https://doi.org/10.1523/JNEUROSCI.1486-20.2020
Choi I, Kim J, Jeong J et al (2022) Astrocyte-derived adenosine excites sleep-promoting neurons in the ventrolateral preoptic nucleus: astrocyte-neuron interactions in the regulation of sleep. Glia 70:1864–1885. https://doi.org/10.1002/glia.24225
Poskanzer KE, Yuste R (2011) Astrocytic regulation of cortical UP states. Proc Natl Acad Sci 108:18453–18458. https://doi.org/10.1073/pnas.1112378108
Fellin T, Ellenbogen JM, De Pittà M et al (2012) Astrocyte regulation of sleep circuits: experimental and modeling perspectives. Front Comput Neurosci 6:65. https://doi.org/10.3389/fncom.2012.00065
Oliveira JF, Araque A (2022) Astrocyte regulation of neural circuit activity and network states. Glia 70:1455–1466. https://doi.org/10.1002/glia.24178
Ingiosi AM, Hayworth CR, Frank MG (2023) Activation of basal forebrain astrocytes induces wakefulness without compensatory changes in sleep drive. J Neurosci 43:5792–5809. https://doi.org/10.1523/JNEUROSCI.0163-23.2023
Savtchouk I, Volterra A (2018) Gliotransmission: beyond black-and-white. J Neurosci 38:14–25. https://doi.org/10.1523/JNEUROSCI.0017-17.2017
Jourdain P, Bergersen LH, Bhaukaurally K et al (2007) Glutamate exocytosis from astrocytes controls synaptic strength. Nat Neurosci 10:331–339. https://doi.org/10.1038/nn1849
Martineau M, Shi T, Puyal J et al (2013) Storage and uptake of D-serine into astrocytic synaptic-like vesicles specify gliotransmission. J Neurosci 33:3413–3423. https://doi.org/10.1523/JNEUROSCI.3497-12.2013
Jaiswal JK, Fix M, Takano T et al (2007) Resolving vesicle fusion from lysis to monitor calcium-triggered lysosomal exocytosis in astrocytes. Proc Natl Acad Sci 104:14151–14156. https://doi.org/10.1073/pnas.0704935104
Zhang H, Fan X, Bagshaw R et al (2008) Purification and proteomic analysis of lysosomal integral membrane proteins. Methods Mol Biol. https://doi.org/10.1007/978-1-59745-028-7_16
Montana V, Malarkey EB, Verderio C et al (2006) Vesicular transmitter release from astrocytes. Glia 54:700–715. https://doi.org/10.1002/glia.20367
Parpura V, Verkhratsky A (2012) Homeostatic function of astrocytes: Ca2+ and Na+ signalling. Transl Neurosci 3:334–344. https://doi.org/10.2478/s13380-012-0040-y
Sawada K, Echigo N, Juge N et al (2008) Identification of a vesicular nucleotide transporter. Proc Natl Acad Sci 105:5683–5686. https://doi.org/10.1073/pnas.0800141105
Parpura V, Zorec R (2010) Gliotransmission: exocytotic release from astrocytes. Brain Res Rev 63:83–92. https://doi.org/10.1016/j.brainresrev.2009.11.008
Sreedharan S, Shaik JH, Olszewski PK et al (2010) Glutamate, aspartate and nucleotide transporters in the SLC17 family form four main phylogenetic clusters: evolution and tissue expression. BMC Genomics 11:17. https://doi.org/10.1186/1471-2164-11-17
Prada I, Marchaland J, Podini P et al (2011) REST/NRSF governs the expression of dense-core vesicle gliosecretion in astrocytes. J Cell Biol 193:537–549. https://doi.org/10.1083/jcb.201010126
Shestopalov VI, Panchin Y, Tarasova OS et al (2017) Pannexins are potential new players in the regulation of cerebral homeostasis during sleep-wake cycle. Front Cell Neurosci 11:1–8. https://doi.org/10.3389/fncel.2017.00210
Greene RW, Bjorness TE, Suzuki A (2017) The adenosine-mediated, neuronal-glial, homeostatic sleep response. Curr Opin Neurobiol 44:236–242. https://doi.org/10.1016/j.conb.2017.05.015
Blutstein T, Haydon PG (2013) The Importance of astrocyte-derived purines in the modulation of sleep. Glia 61:129–139. https://doi.org/10.1002/glia.22422
Dunwiddie TV, Diao L, Proctor WR (1997) Adenine nucleotides undergo rapid, quantitative conversion to adenosine in the extracellular space in rat hippocampus. J Neurosci 17:7673–7682
Porkka-Heiskanen T, Strecker RE, Thakkar M et al (1979) (1997) Adenosine: a mediator of the sleep-inducing effects of prolonged wakefulness. Science 276:1265–1268
Halassa MM, Florian C, Fellin T et al (2009) Astrocytic modulation of sleep homeostasis and cognitive consequences of sleep loss. Neuron 61:213–219. https://doi.org/10.1016/j.neuron.2008.11.024
Fujita T, Chen MJ, Li B et al (2014) Neuronal transgene expression in dominant-negative SNARE mice. J Neurosci 34:16594–16604. https://doi.org/10.1523/JNEUROSCI.2585-14.2014
Peng W, Wu Z, Song K et al (1979) (2020) Regulation of sleep homeostasis mediator adenosine by basal forebrain glutamatergic neurons. Science. https://doi.org/10.1126/science.abb0556
Peng W, Liu X, Ma G et al (2023) Adenosine-independent regulation of the sleep–wake cycle by astrocyte activity. Cell Discov 9:16. https://doi.org/10.1038/s41421-022-00498-9
Garofalo S, Picard K, Limatola C, et al (2020) Role of glia in the regulation of sleep in health and disease. In: Comprehensive physiology. Wiley, pp 687–712
Morairty S, Rainnie D, McCarley R, Greene R (2004) Disinhibition of ventrolateral preoptic area sleep-active neurons by adenosine: a new mechanism for sleep promotion. Neuroscience 123:451–457
Scharbarg E, Walter A, Lecoin L et al (2023) Prostaglandin D2 controls local blood flow and sleep-promoting neurons in the VLPO via astrocyte-derived adenosine. ACS Chem Neurosci 14:1063–1070. https://doi.org/10.1021/acschemneuro.2c00660
Gallopin T, Luppi P-H, Cauli B et al (2005) The endogenous somnogen adenosine excites a subset of sleep-promoting neurons via A2A receptors in the ventrolateral preoptic nucleus. Neuroscience 134:1377–1390. https://doi.org/10.1016/j.neuroscience.2005.05.045
Zhang J, Yin D, Wu F et al (2013) Microinjection of adenosine into the hypothalamic ventrolateral preoptic area enhances wakefulness via the A1 receptor in rats. Neurochem Res 38:1616–1623. https://doi.org/10.1007/s11064-013-1063-7
Yamamoto K, Miwa T, Ueno R, Hayaishi O (1988) Muramyl dipeptide-elicited production of PGD2 from astrocytes in culture. Biochem Biophys Res Commun 156:882–888. https://doi.org/10.1016/S0006-291X(88)80926-4
Bezzi P, Carmignoto G, Pasti L et al (1998) Prostaglandins stimulate calcium-dependent glutamate release in astrocytes. Nature 391:281–285. https://doi.org/10.1038/34651
Zonta M, Angulo MC, Gobbo S et al (2003) Neuron-to-astrocyte signaling is central to the dynamic control of brain microcirculation. Nat Neurosci 6:43–50. https://doi.org/10.1038/nn980
Urade Y, Hayaishi O (2011) Prostaglandin D2 and sleep/wake regulation. Sleep Med Rev 15:411–418
Pandey HP, Ram A, Matsumura H, Hayaishi O (1995) Concentration of prostaglandin D2 in cerebrospinal fluid exhibits a circadian alteration in conscious rats. Biochem Mol Biol Int 37:431–437
Díaz-García CM, Mongeon R, Lahmann C et al (2017) Neuronal stimulation triggers neuronal glycolysis and not lactate uptake. Cell Metab 26:361-374.e4. https://doi.org/10.1016/j.cmet.2017.06.021
Bozzo L, Puyal J, Chatton J-Y (2013) Lactate modulates the activity of primary cortical neurons through a receptor-mediated pathway. PLoS ONE 8:e71721. https://doi.org/10.1371/journal.pone.0071721
Yang J, Ruchti E, Petit J-M et al (2014) Lactate promotes plasticity gene expression by potentiating NMDA signaling in neurons. Proc Natl Acad Sci 111:12228–12233. https://doi.org/10.1073/pnas.1322912111
Pierre K, Pellerin L (2005) Monocarboxylate transporters in the central nervous system: distribution, regulation and function. J Neurochem 94:1–14. https://doi.org/10.1111/j.1471-4159.2005.03168.x
de Ceglia R, Ledonne A, Litvin DG et al (2023) Specialized astrocytes mediate glutamatergic gliotransmission in the CNS. Nature 622:120–129. https://doi.org/10.1038/s41586-023-06502-w
Wang X, Lou N, Xu Q et al (2006) Astrocytic Ca2+ signaling evoked by sensory stimulation in vivo. Nat Neurosci 9:816–823. https://doi.org/10.1038/nn1703
Shiga H, Murakami J, Nagao T et al (2006) Glutamate release from astrocytes is stimulated via the appearance of exocytosis during cyclic AMP-induced morphologic changes. J Neurosci Res 84:338–347. https://doi.org/10.1002/jnr.20885
Xu X-H, Qiu M-H, Dong H et al (2014) GABA transporter-1 inhibitor NO-711 alters the EEG power spectra and enhances non-rapid eye movement sleep during the active phase in mice. Eur Neuropsychopharmacol 24:585–594. https://doi.org/10.1016/j.euroneuro.2013.09.002
Anaclet C, Ferrari L, Arrigoni E et al (2014) The GABAergic parafacial zone is a medullary slow wave sleep–promoting center. Nat Neurosci 17:1217–1224. https://doi.org/10.1038/nn.3789
Chaturvedi R, Stork T, Yuan C et al (2022) Astrocytic GABA transporter controls sleep by modulating GABAergic signaling in Drosophila circadian neurons. Curr Biol 32:1895-1908.e5. https://doi.org/10.1016/j.cub.2022.02.066
Srinivasan D, Yen J-H, Joseph DJ, Friedman W (2004) Cell Type-Specific Interleukin-1β Signaling in the CNS. J Neurosci 24:6482–6488. https://doi.org/10.1523/JNEUROSCI.5712-03.2004
Taishi P, Bredow S, Guha-Thakurta N et al (1997) Diurnal variations of interleukin-1β mRNA and β-actin mRNA in rat brain. J Neuroimmunol 75:69–74. https://doi.org/10.1016/S0165-5728(97)00002-7
Tobler I, Borbély AA, Schwyzer M, Fontana A (1984) Interleukin-1 derived from astrocytes enhances slow wave activity in sleep EEG of the rat. Eur J Pharmacol 104:191–192. https://doi.org/10.1016/0014-2999(84)90391-1
Hu S, Sheng WS, Peterson PK, Chao CC (1995) Differential regulation by cytokines of human astrocyte nitric oxide production. Glia 15:491–494. https://doi.org/10.1002/glia.440150412
Ingiosi AM, Opp MR (2016) Sleep and immunomodulatory responses to systemic lipopolysaccharide in mice selectively expressing interleukin-1 receptor 1 on neurons or astrocytes. Glia 64:780–791. https://doi.org/10.1002/glia.22961
Blum ID, Keleş MF, Baz E-S et al (2021) Astroglial calcium signaling encodes sleep need in Drosophila. Curr Biol 31:150-162.e7. https://doi.org/10.1016/j.cub.2020.10.012
Bergami M, Santi S, Formaggio E et al (2008) Uptake and recycling of pro-BDNF for transmitter-induced secretion by cortical astrocytes. J Cell Biol 183:213–221. https://doi.org/10.1083/jcb.200806137
Faraguna U, Vyazovskiy VV, Nelson AB et al (2008) A causal role for brain-derived neurotrophic factor in the homeostatic regulation of sleep. J Neurosci 28:4088–4095. https://doi.org/10.1523/JNEUROSCI.5510-07.2008
Garner JM, Chambers J, Barnes AK, Datta S (2018) Changes in brain-derived neurotrophic factor expression influence sleep-wake activity and homeostatic regulation of rapid eye movement sleep. Sleep 41:1–14. https://doi.org/10.1093/sleep/zsx194
Hill JL, Hardy NF, Jimenez DV et al (2016) Loss of promoter IV-driven BDNF expression impacts oscillatory activity during sleep, sensory information processing and fear regulation. Transl Psychiatry 6:e873. https://doi.org/10.1038/tp.2016.153
Niu C, Yue X, An JJ et al (2024) Genetic dissection of BDNF and TrkB expression in glial cells. Biomolecules 14:91. https://doi.org/10.3390/biom14010091
Watson AJ, Henson K, Dorsey SG, Frank MG (2015) The truncated TrkB receptor influences mammalian sleep. Am J Physiol Regul Integr Comp Physiol 308:R199–R207. https://doi.org/10.1152/ajpregu.00422.2014
Covelo A, Araque A (2018) Neuronal activity determines distinct gliotransmitter release from a single astrocyte. Elife. https://doi.org/10.7554/eLife.32237
Lee J-H, Kim J, Noh S et al (2021) Astrocytes phagocytose adult hippocampal synapses for circuit homeostasis. Nature 590:612–617. https://doi.org/10.1038/s41586-020-03060-3
Morizawa YM, Matsumoto M, Nakashima Y et al (2022) Synaptic pruning through glial synapse engulfment upon motor learning. Nat Neurosci 25:1458–1469. https://doi.org/10.1038/s41593-022-01184-5
Chung WS, Clarke LE, Wang GX et al (2013) Astrocytes mediate synapse elimination through MEGF10 and MERTK pathways. Nature 504:394–400. https://doi.org/10.1038/nature12776
Park J, Chung W-S (2023) Astrocyte-dependent circuit remodeling by synapse phagocytosis. Curr Opin Neurobiol 81:102732. https://doi.org/10.1016/j.conb.2023.102732
Cavaccini A, Durkee C, Kofuji P et al (2020) Astrocyte signaling gates long-term depression at corticostriatal synapses of the direct pathway. J Neurosci 40:5757–5768. https://doi.org/10.1523/JNEUROSCI.2369-19.2020
Puentes-Mestril C, Aton SJ (2017) Linking network activity to synaptic plasticity during sleep: hypotheses and recent data. Front Neural Circuits. https://doi.org/10.3389/fncir.2017.00061
Stellwagen D, Beattie EC, Seo JY, Malenka RC (2005) Differential regulation of AMPA receptor and GABA receptor trafficking by tumor necrosis factor-α. J Neurosci 25:3219–3228. https://doi.org/10.1523/JNEUROSCI.4486-04.2005
Olmos G, Lladó J (2014) Tumor necrosis factor alpha: a link between neuroinflammation and excitotoxicity. Mediators Inflamm 2014:1–12. https://doi.org/10.1155/2014/861231
Tononi G, Cirelli C (2014) Sleep and the price of plasticity: from synaptic and cellular homeostasis to memory consolidation and integration. Neuron 81:12–34. https://doi.org/10.1016/j.neuron.2013.12.025
Miyamoto D, Marshall W, Tononi G, Cirelli C (2021) Net decrease in spine-surface GluA1-containing AMPA receptors after post-learning sleep in the adult mouse cortex. Nat Commun 12:2881. https://doi.org/10.1038/s41467-021-23156-2
Clarke LE, Barres BA (2013) Emerging roles of astrocytes in neural circuit development. Nat Rev Neurosci 14:311–321. https://doi.org/10.1038/nrn3484
Shafqat A, Khan S, Omer MH et al (2023) Cellular senescence in brain aging and cognitive decline. Front Aging Neurosci. https://doi.org/10.3389/fnagi.2023.1281581
Oberheim NA, Goldman SA, Nedergaard M (2012) Heterogeneity of astrocytic form and function. Methods Mol Biol. https://doi.org/10.1007/978-1-61779-452-0_3
Karpf J, Unichenko P, Chalmers N et al (2022) Dentate gyrus astrocytes exhibit layer-specific molecular, morphological and physiological features. Nat Neurosci 25:1626–1638. https://doi.org/10.1038/s41593-022-01192-5
Westergard T, Rothstein JD (2020) Astrocyte diversity: current insights and future directions. Neurochem Res 45:1298–1305. https://doi.org/10.1007/s11064-020-02959-7
Schober AL, Wicki-Stordeur LE, Murai KK, Swayne LA (2022) Foundations and implications of astrocyte heterogeneity during brain development and disease. Trends Neurosci 45:692–703. https://doi.org/10.1016/j.tins.2022.06.009
Li Y, Que M, Wang X et al (2023) Exploring astrocyte-mediated mechanisms in sleep disorders and comorbidity. Biomedicines 11:2476. https://doi.org/10.3390/biomedicines11092476
Sofroniew MV (2014) Multiple roles for astrocytes as effectors of cytokines and inflammatory mediators. Neuroscientist 20:160–172. https://doi.org/10.1177/1073858413504466
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interests
Non-financial interests: none.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bellier, F., Walter, A., Lecoin, L. et al. Astrocytes at the heart of sleep: from genes to network dynamics. Cell. Mol. Life Sci. 82, 207 (2025). https://doi.org/10.1007/s00018-025-05671-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00018-025-05671-3