Abstract
The prognosis of adult T-cell leukemia/lymphoma (ATL) with primary central nervous system (CNS) involvement has been unclear since the advent of new therapies. Recently, we have shown that flow cytometric CD7/CADM1 analysis of CD4 + cells (HAS-Flow) is useful to detect ATL cells that are not morphologically diagnosed as ATL cells. We investigated the role of CNS involvement in ATL using cytology and HAS-Flow by analyzing cerebrospinal fluid (CSF) from 73 aggressive ATL cases. Based on the findings in CSF, the study subjects were classified into CNS + (cytologically malignant, n = 18), CNS- (cytologically non-malignant and ATL cell population negative in HAS-Flow, n = 44), and CNS-Micro (cytologically non-malignant and ATL cell population positive in HAS-Flow, n = 11) groups. As expected, the CNS + group had a shorter overall survival than the CNS- groups (P < 0.001). However, the CNS-Micro group showed no adverse impact on overall survival compared to the CNS- group (P = 0.506), even without additional CNS-targeted treatments. HAS-Flow also demonstrated clinical utility in the diagnosis of CSF lesions in ATL patients with cerebral white matter lesions and in the detection of ATL cells on post-treatment CSF examination in patients with CNS involvement. Our study demonstrates that ATL with CNS involvement have a poor prognosis and that CSF HAS-Flow is useful to assist in the diagnosis of suspected CNS involvement and to detect ATL cells with high sensitivity after treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adult T-cell leukemia/lymphoma (ATL) is a hematological malignancy with a poor prognosis that originates from human T-cell leukemia virus (HTLV)−1-infected T lymphocytes [1, 2]. Although primary central nervous system (CNS) lymphoma is known to have a poor prognosis [3], reports on the impact of CNS involvement on ATL outcomes are limited and show inconsistent results [4,5,6], leaving the prognostic significance of CNS involvement status at diagnosis undefined.
In addition to symptoms and imaging studies, cerebrospinal fluid (CSF) examination is important for diagnosing CNS involvement in lymphoma. Along with cell counts and cytology of CSF, the analysis of CSF cells for CADM1 and CD7 in CD4 + cells using flow cytometry (HAS-Flow) has been reported to be useful [7]. We recently reported that HAS-Flow analysis of peripheral blood is useful for prognostic estimation in aggressive ATL, demonstrating its ability to identify morphologically unidentified ATL cells in peripheral blood [8]. Therefore, we hypothesized that the effectiveness of HAS-Flow in detecting cryptic ATL cells could also be applied to CSF examinations for detecting CNS invasion. In addition, we explored the clinical impact of HAS-Flow-positive results.
Methods
Patients, Definitions, and Analyses
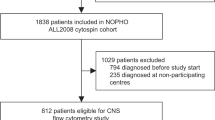
Aggressive ATL patients treated at the Research Hospital, Institute of Medical Science, University of Tokyo, who had at least one CSF analysis between September 2014 and February 2024, were included. Data used in this study, including flow cytometric data, were extracted from medical records. The details of this observational study were published online, and consent of participants was obtained by an opt-out method [9]. ATL disease subtypes were classified according to the Shimoyama classification [10]. Pathological evaluation of CSF cells was performed in accordance with the standard Papanicolaou classification system [11] as follows: class I, normal; class II, benign atypia; class III, suggestive of malignancy; class IV, strongly suggestive of malignancy; and class V, consistent with malignancy. Class IV and V were considered malignant and denoted as Cyto + , while Classes I–III were categorized as Cyto-. Peripheral blood contamination of the CSF was determined by skilled pathologists. CSF examinations, including flow cytometry, were performed as part of the clinical assessment. Flow cytometric analyses were performed on CSF samples as previously reported for peripheral blood using a FACS Canto II (BD Biosciences), and the data were analyzed using FlowJo software (Tree Star) [8, 12]. Representative flow cytometric plots of CSF cells from this study are shown in Fig. 1A. Among CD4 + cells, HTLV-1 non-infected cells are represented as the P fraction (CD7 + /CADM1-), and among the HTLV-1 infected cell fractions (CADM1 + : D + N fractions), the N fraction (CD7-/CADM1 +) is shown to increase with clonal evolution [8, 12]. Samples with ≥ 20% and < 20% N fractions were assumed as HAS-Flow + and HAS-Flow-, respectively. This study was performed in accordance with the Declaration of Helsinki. The Institutional Review Board of the Institute of Medical Science, University of Tokyo, approved this study (2019–72–0217).
Effects of CADM1 versus CD7 flow cytometric plots and prognosis of aggressive ATL based on CNS infiltration status. A Representative flow cytometric plots using CSF samples from this study. B, C Proportion of the N fraction (%) (B) and absolute number of log-transformed N fraction (C) compared according to cytology results. D Overall survival of aggressive ATL patients compared by CNS infiltration status
Statistical analysis
Continuous variables were compared using Student’s t-test or the Kruskal–Wallis test. Variables were log-transformed when necessary to ensure a normal distribution. Categorical variables were compared using a chi-square test. Overall survival (OS) was analyzed based on the time since the first CSF examination and compared between groups by log-rank test. All statistical analyses were performed using GraphPad Prism software (version 7.0d; GraphPad Software), or EZR (version 1.55; Saitama Medical Center, Jichi Medical University) [13].
Results
We analyzed 154 CSF samples from 73 patients with aggressive ATL. The median age at the time of the initial CSF examination was 65 years, with 58 patients (79%) having acute-type ATL (Table 1). CSF examination parameters by CSF cytology showed that the Class V group had significantly higher CSF cell counts, lactate dehydrogenase (LDH) values, and both the percentage and absolute number of ATL cell fractions (N fraction) by flow cytometry than the Class I–III group, which was not classified as malignant (Fig. 1B,C; S1A,B). We then evaluated 71 samples that underwent both CSF HAS-Flow and cytology analysis. CSF HAS-Flow was performed for screening at the time of initial CSF collection, to aid in the diagnosis of suspected CNS infiltration, and for follow-up of patients with CNS involvement. Of the 25 Cyto + samples, 24 were HAS-Flow + , whereas among the 46 Cyto- samples, 21 were HAS-Flow- (Fig. 1B,C). Thus, HAS-Flow had 96% sensitivity but only 46% specificity for cytological malignancy. This suggests the presence of CSF ATL cells that are not visually identified as well as cases with minimal CNS involvement among Cyto- patients. Based on the results of the initial CSF analysis, the patients were categorized into three groups: CSF + group (Cyto + without peripheral blood contamination), CNS-Micro group (Cyto- and HAS-Flow + without peripheral blood contamination), and CNS- group (all other cases). One patient, with an elevated CSF cell count (56/μL), a 94% N fraction on HAS-Flow, multiple cerebral white matter lesions on magnetic resonance imaging (MRI), and cytology classified as Class V on the second CSF examination was included in the CNS + group despite an initial CSF of Class III.
Eleven percent of the patients in this cohort had their first CNS examination before initiation of systemic chemotherapy, most of whom were in the CNS + group (Table 1). The CSF cell counts and LDH values were not significantly different between the CNS- and CNS-Micro groups, whereas the ratio and absolute number of N fractions showed a stepwise increase in the CNS-, CNS-Micro, and CNS + groups (Figure S1C–F). All patients in this cohort, including the CNS- group, received intrathecal injection of chemotherapy (IT), and no further treatment was given to the CNS-Micro group for the control of CNS lesions (Table 1). Two patients in the CNS- group (5%) and one in the CNS-Micro group (9%) showed definite CNS involvement at the later follow-up (Table 1). The CNS + group had a significantly shorter OS compared with the CNS- and CNS-Micro groups, whereas there was no difference between the CNS- and CNS-Micro groups (Fig. 1D). Similar results were obtained when the analysis was limited to the acute-type ATL patients (Figure S2A). This suggests that CNS-Micro groups need no further CNS-targeted treatment in addition to prophylactic IT.
Allogeneic hematopoietic cell transplantation (allo-HCT) is a crucial treatment that contributes to improved prognosis for eligible patients with aggressive ATL [14]. Forty patients (54%) in this cohort as a whole underwent allo-HCT, while only 5 (28%) in the CNS + group underwent (Table 1). In this cohort as a whole, patients with allo-HCT had a better prognosis than non-transplant patients (Figure S2B). When comparing prognosis by CNS involvement status, only the CNS + group had a significantly worse prognosis than the other two groups as did the cohort as a whole, when limited to non-transplant cases (Figure S2C). However, there was no significant difference among the 3 groups in OS when limited to cases with allo-HCT (Figure S2D).
We then reviewed three cases with CNS involvement that were evaluated for CSF by HAS-Flow repeatedly (Figs. 2A–C). Treatment for the CNS lesions reduced the cell counts to the normal range and changed malignant CSF cytology to the non-malignant category in all cases. However, the flow cytometric analyses showed that the N fraction disappeared in one case and remained in the other two cases. The two patients with a residual N fraction were subsequently treated with craniospinal irradiation followed by allo-HCT. One patient is alive without CNS lesion recurrence, while the other experienced CNS recurrence approximately 9 months after allo-HCT and died. These results suggest that HAS-Flow can detect ATL cells with high sensitivity and may be useful as a multifaceted evaluation of CNS lesions after treatment.
Discussion
This is the first report showing that aggressive ATL patients with CNS infiltration at diagnosis have a poor prognosis, while simultaneously demonstrating that flow cytometric analysis of CSF is useful in detecting ATL cells.
Due to the rarity of the disease, the prognosis of CNS involvement in ATL was unclear. A report published more than 20 years ago showed that CNS involvement conferred no significant impact on OS [4]. The prognosis for the CNS + group in that report was 5.2 months from the time of CNS involvement detection, which is almost identical to this report (median OS 6.3 months). The treatment strategy for CNS lesions in ATL has not changed significantly over these 20 years, with IT or radiation being the mainstay [4, 6]. In contrast, the prognosis for ATL as a whole has improved with the advent of novel modalities, better allo-HCT outcomes, and improved supportive care, including infectious disease management [15]. This discrepancy in treatment progress between overall ATL and CNS-involved ATL is assumed to highlight the impact of CNS involvement on outcomes.
There are reports that the cases of CNS involvement with uncontrolled CNS lesions prior to allo-HCT are associated with poor prognosis, whereas the cases who achieved complete remission of CNS lesions are not associated with subsequent poor prognosis [6]. In this cohort, only a small number of patients in the CNS + group underwent allo-HCT. This indicates that there are a large number of patients in the CNS + group who did not achieve transplantation-eligible status because of the extremely poor prognosis. Actually, CNS + was not a significant prognostic factor only in cases with allo-HCT (Figure S2D). Therefore, this report supports the previous findings that CNS involvement does not confer poor prognosis when it is well-controlled prior to transplantation.
This report suggests that there is a group of patients with micro-CNS infiltration of ATL cells detected by flow cytometry alone, who would have been classified as CNS-negative without HAS-Flow. Unexpectedly, patients in this group did not have a poor prognosis, and many did not subsequently develop explicit CNS lesions. All patients in this cohort received routine prophylactic IT, suggesting that micro-CNS infiltration can be controlled by IT.
Although our results suggested that CNS-Micro (HAS-Flow + alone) has no prognostic impact on outcomes and requires no additional treatment, HAS-Flow analysis might be useful for identifying increased morphologically non-malignant CSF cells. In fact, we encountered a case with elevated CSF cell counts (56/μL) and a cerebral lesion on MRI. Cytology was Class III, but HAS-Flow was 96% positive, leading us to classify this case as CNS + and successfully treat the CNS lesion with IT.
It should be emphasized that the negligible impact of CNS-Micro on outcomes applies only to initial CSF samples before receiving CNS treatment; the role of CNS-Micro after treatment has not yet been determined. We had two patients whose explicit CNS + findings downgraded to CNS-Micro after CNS treatment. Both cases underwent allo-HCT following additional CNS radiotherapy, and one developed CNS recurrence after allo-HCT and died. These cases suggest that transient CNS-Micro findings after CNS treatment do not indicate favorable outcomes and should be treated with caution.
This study had several limitations. Firstly, it was a small, single-center, retrospective study. Large-scale, prospective studies are desirable. Secondly, HAS-Flow data were available for only 58% of the cases. There were cases in both the CNS + and CNS- groups where HAS-Flow was not performed (Table 1). A cohort with a larger number of analyzed cases would be desirable for investigating the utility of HAS-Flow. Thirdly, the prognosis of cases transitioning from CNS + to CNS-Micro after treatment has not been clarified. The accumulation of cases tracking the course of HAS-Flow in CNS + patients is desirable.
In conclusion, this study revealed that ATL cases with CNS involvement at diagnosis have a poor prognosis. HAS-Flow may be a potentially useful qualitative assessment of CSF cells in addition to cytology, but further validation is needed.
Data availability
No datasets were generated or analysed during the current study.
References
Uchiyama T, Yo J, Sagawa K, Takatsuki K, Uchino H (1977) Adult T-cell leukemia: clinical and hematologic features of 16 cases. Blood 50(3):481–92
Yoshida M, Miyoshi I, Hinuma Y (1982) Isolation and characterization of retrovirus from cell lines of human adult T-cell leukemia and its implication in the disease. Proc Natl Acad Sci U S A 79(6):2031–2035. https://doi.org/10.1073/pnas.79.6.2031
Houillier C, Soussain C, Ghesquières H, Soubeyran P, Chinot O, Taillandier L et al (2020) Management and outcome of primary CNS lymphoma in the modern era: An LOC network study. Neurology 94(10):e1027–e1039. https://doi.org/10.1212/WNL.0000000000008900
Teshima T, Akashi K, Shibuya T, Taniguchi S, Okamura T, Harada M et al (1990) Central nervous system involvement in adult T-cell leukemia/lymphoma. Cancer 65(2):327–332. https://doi.org/10.1002/1097-0142(19900115)65:2%3c327::aid-cncr2820650224%3e3.0.co;2-w
Fukushima T, Taguchi J, Moriuchi Y, Yoshida S, Itonaga H, Ando K et al (2011) Allogeneic hematopoietic stem cell transplantation for ATL with central nervous system involvement: the Nagasaki Transplant Group experience. Int J Hematol 94(4):390–394. https://doi.org/10.1007/s12185-011-0935-3
Fuji S, Inoue Y, Utsunomiya A, Moriuchi Y, Choi I, Otsuka E et al (2019) Impact of pretransplant central nervous system invasion in patients with aggressive adult T-cell leukemia lymphoma. Bone Marrow Transplant 54(1):134–137. https://doi.org/10.1038/s41409-018-0248-8
Takeda R, Ishigaki T, Ohno N, Yokoyama K, Kawamata T, Fukuyama T et al (2020) Immunophenotypic analysis of cerebrospinal fluid reveals concurrent development of ATL in the CNS of a HAM/TSP patient. Int J Hematol 111(6):891–896. https://doi.org/10.1007/s12185-019-02815-7
Jimbo K, Kawamata T, Inamoto Y, Ito A, Yokoyama K, Sato A et al (2024) Flow cytometric profiles with CD7 and CADM1 in CD4+ T cells are promising indicators for prognosis of aggressive ATL. Blood Adv 8:3760–70. https://doi.org/10.1182/bloodadvances.2024013089
Vellinga A, Cormican M, Hanahoe B, Bennett K, Murphy AW (2011) Opt-out as an acceptable method of obtaining consent in medical research: a short report. BMC Med Res Methodol 11:40. https://doi.org/10.1186/1471-2288-11-40
Shimoyama M (1991) Diagnostic criteria and classification of clinical subtypes of adult T-cell leukaemia-lymphoma. A report from the Lymphoma Study Group (1984–87). Br J Haematol 79(3):428–37. https://doi.org/10.1111/j.1365-2141.1991.tb08051.x
Lieu D (1996) The Papanicolaou smear: its value and limitations. J Fam Pract 42:391–399
Kobayashi S, Nakano K, Watanabe E, Ishigaki T, Ohno N, Yuji K et al (2014) CADM1 expression and stepwise downregulation of CD7 are closely associated with clonal expansion of HTLV-I-infected cells in adult T-cell leukemia/lymphoma. Clin Cancer Res 20(11):2851–2861. https://doi.org/10.1158/1078-0432.ccr-13-3169
Kanda Y (2013) Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant 48(3):452–458. https://doi.org/10.1038/bmt.2012.244
Cook LB, Fuji S, Hermine O, Bazarbachi A, Ramos JC, Ratner L et al (2019) Revised adult T-cell leukemia-lymphoma international consensus meeting report. J Clin Oncol 37(8):677. https://doi.org/10.1200/jco.18.00501
Imaizumi Y, Iwanaga M, Nosaka K, Ishitsuka K, Ishizawa K, Ito S et al (2020) Prognosis of patients with adult T-cell leukemia/lymphoma in Japan: a nationwide hospital-based study. Cancer Sci 111(12):4567–4580. https://doi.org/10.1111/cas.14658
Acknowledgements
The authors thank the physicians and staff at the hospital in Department of Hematology/Oncology and Department of Laboratory Medicine for the treatment of patients and evaluation of the laboratory data, the lab members in Division of Hematopoietic Disease Control for advice on the study, and IMSUT Clinical Flow Cytometry Laboratory (The Institute of Medical Science, The University of Tokyo) for the analysis of flow cytometric data.
Funding
Open Access funding provided by The University of Tokyo. This work was supported by grants-in-aid from Japan Society for the Promotion of Science (JSPS) (22K16317) and Japan Agency for Medical Research and Development (AMED) (JP23fk0108672).
Author information
Authors and Affiliations
Contributions
K.J. treated the patients, planned the research, collected the clinical data, analyzed and interpreted the data, and wrote the paper. T.I. contributed to the development of the HAS-Flow method of CSF samples. M.S., S.A., H.I., A.I., K.Y., A.S., and T.F. treated the patients and contributed to collect the clinical data. K.U. treated the patients and guided the research. Y.N. treated the patients, guided the research, interpreted the data, and wrote the paper. All authors approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jimbo, K., Ishigaki, T., Sakashita, M. et al. Prognosis of aggressive adult T-cell leukemia/lymphoma with central nervous system infiltration and utility of CD7 versus CADM1 flowcytometric plots of cerebrospinal fluid. Ann Hematol 104, 635–640 (2025). https://doi.org/10.1007/s00277-025-06186-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-025-06186-4