Abstract
HSCT has been recognized as a successful treatment for various hematological disease. The 5-year survival rate for children and adolescents diagnosed with hematological disease has risen to over 90% in high-income countries. Nevertheless, it has been reported that between 65 and 84% of individuals who undergo HSCT suffer from premature ovarian failure(POF), with only 0.6% managing to conceive successfully. To report the 5-year experience and evaluate the fertility of young female survivors in HSCT at Peking University People’s Hospital, a total of 102 pediatric and female patients aged 8–35 years who underwent HSCT were included. The incidence of POF was 88.2%, 93.9% and 61.5% for young female AML, ALL and AA patients, respectively. The AA group (p = 0.028) had a significantly lower incidence of POF. In the POF group, 89% of patients underwent haploidentical related donor HSCT (p = 0.364) and the cyclophosphamide equivalent dose (CED) of these patients was 10,391 mg/m2 (4890, 10589) (p = 0.222). According to the univariate analysis, an age at HSCT ≥ 13 years (p = 0.007), a diagnosis of AA (p = 0.028), and menarche before and amenorrhea after HSCT (p = 0.016) were associated with POF occurrence. The patients diagnosed with AA had a lower incidence of POF(p = 0.028), while other factors were associated with a higher risk of POF. Multivariate analysis was performed that only age at HSCT was independently associated with POF post-HSCT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Avoid common mistakes on your manuscript.
Introduction
In 2022, the most recent cancer incidence in Chinese children and adolescents was comprehensively assessed. Leukemias (42·33 per million) were the most common cancer group among children, whereas leukemias (30·08 per million) were the second most common cancer group among adolescents [1]. However, leukemias were relatively rare in the adult population compared to other types of cancer. Hematopoietic stem cell transplantation (HSCT) is an established therapy for many malignant and nonmalignant hematologic diseases and other life-threatening diseases [2,3,4,5]. In 2021, 18,110 HSCT cases were reported from 174 transplant teams, 70% (12,744 cases) of which were allogeneic HSCTs [6]. Haploidentical related donor (HID) was the most important alternative donor, accounting for 63% (7977 cases) of allogeneic HSCTs in China in 2021 [6]. The BuCy-based regimen (57%) was the most popular conditioning regimen for allogeneic HSCT, followed by the BuFlu-based regimen (28%) and total body irradiation-based regimen (11%) [6]. Given that the probability of long-term survival reaching 80% in patients surviving 2 years post-allogeneic HSCT [7], the 5-year survival rate for children and adolescents with leukemias has improved to over 90% in high-income countries [8]. Concurrently, fertility following HSCT has garnered increasing attention. Reportedly, 65–84% of HSCT recipients experience ovarian failure [9], and only 0.6% achieve successful conception [10]. HSCT represents an independent risk factor for ovarian impairment, as conditioning regimens and graft vs. host disease (GVHD) exert synergistic gonadotoxic effects [11, 12]. Su et al.. investigated the impact of HSCT treatment on reproductive and ovarian functions in female survivors. The prevalence of premature ovarian insufficiency (POI) following HSCT was 72.7% (40/55), and POI was associated with age, conditioning regimen, and type of blood disease [13].
At present, there are no systematic reports on fertility assessment in long-term young female survivors with hematological disease after allogeneic HSCT in China. To our knowledge, this is the first systematic study to evaluate long-term fertility and related influencing factors in young blood patients after HSCT over the past 5 years, providing a basis for fertility evaluation for patients who have received HID allogeneic HSCT.
Materials and methods
Patients
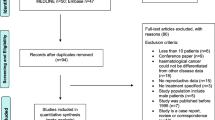
This study was conducted using the transplant database of Peking University, Institute of Hematology (PUIH), and included patients who met the following criteria: [1] were female surviving patients aged ≤ 35 years with hematological diseases; [2] received their first HSCT between 1 January 2017 and 31 December 2018; and [3] had tests for follicle-stimulating hormone (FSH), luteinizing hormone (LH), estradiol (E2), progesterone (P), prolactin (PRL) and testosterone (T) performed. (Fig. 1). The transplant indications were mainly based on the consensus of China [3, 14]. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Institutional Review Board of Peking University People’s Hospital.
Data collection
An independently designed questionnaire was used to gather the following information: general information (age, height, weight), information on blood disorders (type of hematologic disease, donor type, conditioning regimen), and information related to gynecology (menstrual status before and after HSCT, awareness of the protection of reproductive function, and hormone replacement therapy). The data were collected via telephone or network questionnaires and analyzed by gynecologists or hematologists approximately 5 years after transplantation.
Definitions
The following data were collected:
-
Demographic data;
-
Treatment data: underlying disease, age at HSCT, conditioning regimen, CED (cyclophosphamide equivalent dose) [15] (according to the formula: CED (mg/m2) = 1.0 (cumulative cyclophosphamide dose (mg/m2)) + 0.244 (cumulative ifosfamide dose (mg/m2)) + 0.857 (cumulative procarbazine dose (mg/m2)) + 14.286 (cumulative chlorambucil dose (mg/m2)) + 15.0 (cumulative carmustine dose (mg/m2)) + 16.0 (cumulative lomustine dose (mg/m2)) + 40 (cumulative melphalan dose (mg/m2)) + 50 (cumulative thiotepa dose (mg/m2)) + 100 (cumulative chlormethine dose (mg/m2)) + 8.823 (cumulative busulfan dose (mg/m2))), and exposure to abdominopelvic RT.
-
Clinical data: Posttreatment amenorrhea, uro-progestin therapy upon enrollment, other endocrinopathies.
-
Biochemical data collected between days 3 and 5 of the menstrual cycle among patients: FSH (IU/L), LH (IU/L), estradiol (pg/mL), P (ng/mL), PRL (ng/mL), and T (nmol/L).
-
The ovarian outcome was defined as follows:
Premature ovarian failure (POF) is classically defined as amenorrhea for 4–6 months in women under 40 years old, with elevated FSH > 40 IU/L) and low estradiol levels [16].
Statistical methods
The data were censored at the time of death or at the last available follow-up. The Mann–Whitney U test was used to compare continuous variables, and the χ2 test and Fisher’s exact test were used for categorical variables. Univariable and multivariable logistic regression were performed to determine the impact of potential prognostic factors on clinical outcomes. P < 0.05 was considered to indicate statistical significance. P values were based on two-sided hypothesis tests. Statistical analysis was performed using R software (version 4.2.0) (http://www.r-project.org) and SPSS 26.0 software (SPSS).
Results
Baseline and clinical characteristics of patients
A total of 102 patients were enrolled, and their characteristics are shown in Fig. 2. The average age at transplantation was 14 years (range 8–35), encompassing childhood, adolescent, and reproductive age groups (Tables 1 and 2). Malignant hematological diseases predominated, mainly acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML) (65%). Aplastic anemia (AA) accounted for 13%, with the remaining 10% having myelodysplastic syndrome (MDS), Fanconi anemia, rhabdomyosarcoma, chronic myelogenous leukemia (CML) and maternal plasma cell-like dendritic tumor lymphoma. Fifty-five patients received HID-HSCT (54%). Only 9/102 (9%) reported awareness of pretransplant reproductive/ovarian protection treatments, such as embryo, oocyte or ovarian tissue cryopreservation, ovarian shielding during total body irradiation (TBI), administration of gonadotropin-releasing hormone (GnRH) agonists to suppress ovarian function during treatment. No patient received fertility protection. The baseline characteristics of the cohort are shown in Table 1.
Correlations between the incidence of POF and different clinical factors
As shown in Table 2, the average age at transplantation in the POF group was 14 years (ranging from 8 to 35), which was significantly greater than that in the non-POF group (p = 0.014). The incidence of POF was 88.2% (30/34), 93.9% (31/33) and 61.5% (8/13) for young female patients with AML, ALL, and AA, respectively, following HSCT. Compared to the non-POF group, the AA group had a significantly lower incidence of POF (p = 0.028). In the POF group, 89% of patients underwent HID-HSCT (p = 0.364), and 10,391 mg/m2 (4890, 10589) had CED (p = 0.222); there was no statistically significant difference between the two groups. Moreover, 76% of patients with POF had menarche before HSCT (p = 0.099). On the other hand, 94% of patients experienced menarche before HSCT, but the rate of amenorrhea after HSCT was significantly different (p = 0.016).(Table 2).
Factors affecting POF in children and adolescent females
According to the univariate analysis, an age at HSCT ≥ 13 years (p = 0.007), a diagnosis of AA (p = 0.028), and menarche before and amenorrhea after HSCT (p = 0.016) were associated with POF occurrence. The patients diagnosed with AA had a lower incidence of POF(p = 0.028), while other factors were associated with a higher risk of POF. However, donor type of HSCT, CED, no menarche, and amenorrhea after HSCT did not affect the incidence of POF. According to the multivariate analysis, only age at HSCT was independently associated with POF after HSCT (Table 3).
Gonadal hormone levels, HRT usage and POF incidence in different age groups
The POF incidence was 74% in patients under 13 years of age and 94% in patients ≥ 13 years of age, which was a statistically significant difference (P = 0.007) (Table 4). The FSH level in the ≥ 13 years group (109.69 IU/L) was greater than that in the < 13 years group (85.29 IU/L). The HRT usage rate was 63% in the < 13 years group and 90% in the ≥ 13 years group (Fig. 1; Table 5). Further stratified statistics revealed that the POF incidence rates were 74%, 94% and 95% for the < 13 years, 13–18 years, and ≥ 18 years age groups, respectively. The 13- to 18-year-old group had a significantly greater incidence of POF than did the < 13-year-old group (P = 0.019) (Table 4). The HRT usage rates were 63%, 88% and 100%, respectively, in these three groups (Table 4).
Discussion
HSCT involves eliminating abnormal hematopoietic cells through conditioning regimens, such as radiotherapy and chemotherapy, followed by transplantating donor or autologous hematopoietic stem cells to replenish the hematopoietic and immune systems [13]. HSCT is the strongest predictor of POF, and further fertility investigations are needed [17]. With the increasing annual global frequency of HSCT and prolonged post-HSCT survival times, protection of reproductive and ovarian function has become increasingly vital [13]. In this study, the POF incidence rates were 88.2% (30/34), 93.9% (31/33) and 61.5% (8/13) for young female patients with AML, ALL, and AA, respectively, after HSCT. We also reported for the first time the incidence of POF in young female surviving patients with hematological disease and the impact of age on POF incidence. To the best of our knowledge, this was the first large cohort study on fertility assessment and the establishment of a predictive model for POF in young female surviving patients with hematological disease post-HSCT.
The high incidence of POF after HSCT
Among the 102 patients who underwent HSCT, the overall POF incidence was 86.3% (88/102). Previous studies have shown that women undergoing HSCT have 5.4-fold greater odds of needing fertility investigations [18]. In our study, the incidence of POF in AML and ALL patients with malignant hematological disorders was as high as 88.2% and 93.9%, respectively, while the incidence of POF in AA patients with benign hematological disorders was 61.5% (p = 0.028). Consistent with previous studies, POF incidence post-HSCT was found in 65% of patients with malignant disease and 33% with benign pathology (p = 0.07) [19]. Leukemia patients showed a lower spontaneous menarche incidence than did SAA patients post-HSCT. All 11 leukemia patients who underwent cranial irradiation (CRT) whose serum FSH was measured had a serum FSH above the normal reference range,10 with a serum FSH > 25 IU/l at the menopausal level [20]. A previous study confirmed that myeloablative chemotherapy is gonadotoxic [19]. Thus, gonadal failure is a common long-term endocrine consequence of HSCT and appears to be related mainly to the conditioning protocol applied [13]. When bone marrow transplantation (BMT) involves hemotherapy alone, busulfan appears to be the most gonadotoxic regimen, with reported ovarian failure rates of up to 100% [21,22,23,24]. In the study by Pascale et al.., all girls with ovarian failure in the chemotherapy group received busulfan, although 50% of those who maintained ovarian function also received this drug [19]. In our study, the incidence of POF in patients with malignant hematological diseases was significantly greater than that in AA patients. It is necessary to preserve fertility before HSCT in patients with malignant hematological diseases. Although there may be no statistically significant difference in POF occurrence among different diseases according to multivariate logistic analysis, due to the limited number of enrolled patients, malignant hematological diseases still have predictive value for POF in young hematological patients. Further large-scale data analysis is needed for verification.
POF occurs in patients of different ages
We observed that the incidence of POF was significantly greater when HSCT was performed in patients ≥ 13 years old, independent of the time elapsed since treatment. The POF incidence was 74% in the group of patients under 13 years old and 94% in the group of patients ≥ 13 years old, with a statistically significant difference (P = 0.007). Su et al.. reported that the incidence of POI among those aged 21–40 years was 100%, while it was 62.5% for those aged 11–20 years and 0% for those aged ≤ 10 years. Age is the most important factor influencing POF incidence: the younger the age at transplantation is, the lower the risk of POF [13]. Pascale et al.. suggested that the younger group showed clinical evidence of improved ovarian function after BMT significantly more often than did the older group (71% vs. 2%, P < 0.01). Moreover, logistic regression analysis confirmed the independent protective effect of young age at the time of BMT (p < 0.004). Interestingly, young age has a particularly protective effect [19]. The age cutoff for Pascale et al..‘s study was 10 years. Indeed, all girls > 10 years old at the time of BMT/TBI showed irreversible POF, whereas 40% of girls who underwent BMT/TBI before the age of 10 experienced spontaneous puberty [19]. Ovarian failure was more frequent among those who were older at HSCT and TBI conditioning [20]. Consistent with prior studies, our study showed that patients over age 10, especially those ≥ 13 years, had a greater probability of POF. At this age, the HPO axis is mature, and ovarian function is affected by gonadotoxic treatment, greatly increasing the likelihood of ovarian damage. However, age rather than pubertal status is critical. The protective effect of young age may be related to the greater number of nongrowing follicles (NGFs) in younger girls. Improved resistance of young ovarian follicles may thus result not only from increased NGF but also from particular anatomic or paracrine factors. Very recently, Kristensen et al.. identified follicles in the ovarian medulla [25], where the percentages of primordial and growing follicles decreased and increased, respectively, with age. Primordial follicles in the medulla might be more resistant to vascular phenomena and fibrosis, which are implicated in ovarian damage mechanisms [26] and account for the protective effect of young age. Alternatively, paracrine factors, such as AMH, may be less affected by gonadotoxic treatments in younger girls, leading to lower dormant follicle recruitment and a delayed ‘burn-out’ effect [26].
Our research showed that as age increased, the incidence of POF increased. Patients in prepuberty and early adolescence had stronger resistance to adeno-toxicity than adolescents and adults. Therefore, the HPO axis has yet to be established and has been shown to have a protective effect on female ovarian function. With increasing age, the HRT treatment also increased. Perhaps due to the appearance of corresponding symptoms, patients were more reminded to pay attention to endocrine and ovarian function decline, resulting in obvious adverse symptoms such as cardiovascular, cerebrovascular, and nervous system symptoms, requiring HRT treatment. However, improvements in symptoms, corresponding drug side effects, and compliance under long-term HRT treatment in these patients still require further long-term follow-up. The improvement effect of HRT treatment on long-term survival after POF was investigated. The long-term improvement of life therapy for patients with POF was evaluated by observing the effectiveness of HRT treatment.
Establishing a multifactor analysis model to predict the incidence of POF
Our study preliminarily established a predictive model for POF in young female patients with hematological diseases post-HSCT. Age at HSCT, diagnosis, donor of HSCT, cyclophosphamide equivalent dose (CED), whether menarche occurred before HSCT, and whether amenorrhea occurred after HSCT were used as predictive factors to establish the model. The results showed that age at HSCT was an independent predictor of POF occurrence in young female patients with hematological tumors after HSCT. The probability of developing POF in patients aged ≥ 13 years was 5.7 times greater than that in patients younger than 13 years. Our research innovation lies in calculating the CED levels of all enrolled patients and finding objective evidence by comparing the CED levels of patients with or without POF. As iatrogenic gonadotoxicity depends on the cumulative burden of the antineoplastic drugs administered [27–28], the dose of any alkylating agent can be normalized to the corresponding dose of cyclophosphamide via a dedicated algorithm. As a result, the CED can be regarded as a reliable tool for quantifying overall exposure to gonadotoxic treatments and comparing different antineoplastic protocols [29]. In our study, there was no statistically significant difference in CED between the two groups of patients. Our follow-up data are constantly increasing, and by expanding the data volume, we aim to find effective cutoff values for CED and provide guidance for clinical practice. Our data show that haploidentical HSCT does not increase the risk of POF compared to fully matched transplantation. In China, haploidentical HSCT is already the preferred HSCT regimen, but calling other HSCTs does not increase the risk of developing POF in patients, nor does it increase the risk of gonadal toxicity.
Low awareness rate of fertility protection
Among the 102 patients who were followed up, 9% (9/102) were aware of fertility protection, which is consistent with the findings of Su et al. [13]. The absence of fertility protection measures may have contributed to the observed incidence of POF in this study. Considering the follow-up period, the previous concept of fertility protection was not clear, especially in China. In recent years, fertility protection has also received attention from hematologists and reproductive doctors. Ovarian shielding, for instance, has been shown to reduce radiation exposure to the ovaries and preserve ovarian function in some patients undergoing TBI [30]. Similarly, cryopreservation of oocytes, embryos or ovarian tissue and prior to treatment could offer future fertility options for patients at risk of POF [31–32]. If there is enough time for ovarian stimulation before initiation of gonadotoxic therapy, cryopreservation of mature oocytes for menstruating adolescent girls is currently the clinical option for parenting their own child [33,34,35]. If treatment cannot be delayed, the cryopreservation of ovarian tissue offers a novel option for fertility preservation for young, sexually immature girls [35]. Leukemia patients constitute an important group of patients who could benefit from novel reimplantation techniques that have resulted in pregnancies and live births [34–35]. However, concern has been expressed that this method may carry a risk of leukemia relapse [17, 36]. The use of GnRH agonists to suppress ovarian function during chemotherapy or radiation remains controversial, with some studies suggesting a protective effect and others showing no significant benefit [37–38]. Therefore, with the maturity and promotion of fertility protection technology, it is recommended that more young female patients with hematological disease requiring fertility protection be referred to reproductive centers for consultation before HSCT.
Conclusion
The incidence of POF in long-term young female survivors with hematological disease after HSCT was high and correlated significantly with age at HSCT. A low awareness of fertility protection requires more attention and cooperation from hematologists and reproductive physicians to preserve fertility and improve the quality of life of these young patients.
Data availability
No datasets were generated or analysed during the current study.
References
Molinari S, Parissone F, Evasi V, De Lorenzo P, Valsecchi MG, Cesaro S et al (2021) Serum anti-Müllerian hormone as a marker of ovarian reserve after cancer treatment and/or hematopoietic stem cell transplantation in childhood: proposal for a systematic approach to gonadal assessment. Eur J Endocrinol 185:717–728
Alois Gratwohl MHB, Mahmoud Aljurf BMS, Marcelo MD, Pasquini C MD Luis Fernando Bouzas, MD Ayami Yoshimi, MD Jeff Szer, MD Jeff Lipton, MD. (2010)Hematopoietic Stem Cell Transplantation A Global Perspective. JAMA;303:1716– 624
Xu L, Chen H, Chen J, Han M, Huang H, Lai Y et al (2018) The consensus on indications, conditioning regimen, and donor selection of allogeneic hematopoietic cell transplantation for hematological diseases in China—recommendations from the Chinese society of hematology. Journal of Hematology & Oncology;11.
Duarte RF, Labopin M, Bader P, Basak GW, Bonini C, Chabannon C et al (2019) Indications for hematopoietic stem cell transplantation for hematological diseases, solid tumors and immune disorders: current practice in Europe, 2019. Bone Marrow Transplant 54:1525–1552
Edward A, Copelan MD (2006) Hematopoietic Stem-Cell transplantation. N Engl J Med 354:1813–1826
Xu L-P, Lu D-P, Wu D-P, Jiang E-L, Liu D-H, Huang H et al (2023) Hematopoietic Stem Cell Transplantation Activity in China 2020–2021 During the SARS-CoV-2 Pandemic: A Report From the Chinese Blood and Marrow Transplantation Registry Group. Transplantation and Cellular Therapy;29:136.e1-.e7
Bhatia S, Francisco L, Carter A, Sun C-L, Baker KS, Gurney JG et al (2007) Late mortality after allogeneic hematopoietic cell transplantation and functional status of long-term survivors: report from the Bone Marrow Transplant Survivor Study. Blood;110:3784-92
Inaba H, Pui C-H (2019) Immunotherapy in pediatric acute lymphoblastic leukemia. Cancer Metastasis Rev 38:595–610
Forgeard N, Jestin M, Vexiau D, Chevillon F, Ricadat E, Peffault de Latour R et al (2021) Sexuality- and Fertility-Related issues in women after allogeneic hematopoietic stem cell transplantation. Transplantation Cell Therapy 27:432.e1-.e6
Salooja N, Szydlo RM, Socie G, Rio B, Chatterjee R, Ljungman P et al (2001) Pregnancy outcomes after peripheral blood or bone marrow transplantation: a retrospective survey. Lancet 358:271–276
Chow EJ, Anderson L, Baker KS, Bhatia S, Guilcher GMT, Huang JT et al (2016) Late effects surveillance recommendations among survivors of childhood hematopoietic cell transplantation: A children’s oncology group report. Biol Blood Marrow Transplant 22:782–795)
Levine JM, Whitton JA, Ginsberg JP, Green DM, Leisenring WM, Stovall M et al (2018) Nonsurgical premature menopause and reproductive implications in survivors of childhood cancer: A report from the childhood Cancer survivor study. Cancer 124:1044–1052)
Su H, Zhou X, Zhao Y, Lu Y, Liu D, Zhang J et al (2022) Gynecological complications in long-term survivors after allogeneic hematopoietic cell transplantation—a single-center real-life cross-sectional study. Frontiers in Medicine;9.
Liu Kaiyan HX (2014) The consensus of allogeneic hematopoietic transplantation for hematological diseases in China(2014)——indication, conditioning regimen and donor selection. Chin J Hematol;35
Aurélie F, Agnès L, Nathalie R, Michael B, Anne-Laure B (2023) Impact of low- or moderate-risk gonadotoxic chemotherapy prior to testicular tissue freezing on spermatogonia quantity in human (pre)pubertal testicular tissue. Hum Reprod 38(11):2105–2118
Welt CK (2007) Primary ovarian insufficiency: a more accurate term for premature ovarian failure. Clin Endocrinol 68:499–509
Jahnukainen K, Tinkanen H, Wikström A, Dunkel L, Saarinen-Pihkala UM, Mäkinen S et al (2012) Bone marrow remission status predicts leukemia contamination in ovarian biopsies collected for fertility preservation. Leukemia 27:1183–1185
Haavisto A, Wettergren L, Lampic C, Lähteenmäki PM, Jahnukainen K (2023) Premature ovarian insufficiency and chance of pregnancy after childhood cancer: A population-based study (the Fex‐Can study). Int J Cancer 153:644–653
Jadoul P, Anckaert E, Dewandeleer A, Steffens M, Dolmans M-M, Vermylen C et al (2011) Clinical and biologic evaluation of ovarian function in women treated by bone marrow transplantation for various indications during childhood or adolescence. Fertil Steril;96:126– 33.e3.
Vatanen A, Wilhelmsson M, Borgström B, Gustafsson B, Taskinen M, Saarinen-Pihkala UM et al (2014) Ovarian function after allogeneic hematopoietic stem cell transplantation in childhood and adolescence. Eur J Endocrinol 170:211–218
By Raina J, Liesner ADL, lan, Hann M and Judith M. Chessells. (1994)Late Effects of Intensive Treatment for Acute Myeloid Leukemia and Myelodysplasia in Childhood. J Clin Oncol;12:916– 24
Teinturier C, Valteau-Couanet OHD, Benhamou E, PF Bougneres (1998) Ovarian function after autologous bone marrow transplantation in childhood: high-dose Busulfan is a major cause of ovarian failure. Bone Marrow Transplant 22:989–994
By G, Michel GS, Gebhard F, Bernaudin F, Thuret I, Vannier JP, Demeocq F, Leverger G, Pico JL, Rubie H, Mechinaud F, Reiffers J, Gratecos N, Troussard X, Jouet JP, Simonin G, Gluckman E, and D (1997) Maraninchi. Late effects of allogeneic bone marrow transplantation for children with acute myeloblastic leukemia in first complete remission: the impact of conditioning regimen without Total-Body Irradiation-A report from the Soci Te Fran Aise de greffe de Moelle. J Clin Oncol 15:2238–2246
E Thibaud KR-M, Trivin C, Espe´rou H, Michon J, Brauner R (1998) Ovarian function after bone marrow transplantation during childhood. Bone Marrow Transplant 21:287–290
Kristensen SG, Rasmussen A, Byskov AG, Andersen CY (2010) Isolation of preantral follicles from human ovarian medulla tissue. Hum Reprod 26:157–166
DROR MEIROW HB RICHARDA, ANDERSON and W. HAMISH B. WALLACE. (2010)Toxicity of chemotherapy and radiation on female reproduction. CLINICAL OBSTETRICS AND GYNECOLOGY;53:727–739
Chemaitilly W, Li Z, Krasin MJ, Brooke RJ, Wilson CL, Green DM et al (2017) Premature ovarian insufficiency in childhood Cancer survivors: A report from the St. Jude lifetime cohort. J Clin Endocrinol Metabolism 102:2242–2250
Charpentier A-M, Chong AL, Gingras-Hill G, Ahmed S, Cigsar C, Gupta AA et al (2014) Anti-Müllerian hormone screening to assess ovarian reserve among female survivors of childhood cancer. J Cancer Surviv 8:548–554
Green DM, Nolan VG, Goodman PJ, Whitton JA, Srivastava D, Leisenring WM et al (2013) The cyclophosphamide equivalent dose as an approach for quantifying alkylating agent exposure: A report from the childhood cancer survivor study. Pediatr Blood Cancer 61:53–67
.Wallace WH et al (2005) Ovarian shielding protects ovarian reserve during radiation therapy in young women with hematological malignancies. J Clin Oncol 23(12):2694–2700
Lambertini M et al (2020) Fertility preservation and post-treatment pregnancies in post-pubertal cancer patients: ESMO clinical practice guidelines. Ann Oncol 31(12):1664–1678
Hou Y, Tian L, Huai LF (2022) Fertility preservation for female patients with childhood and adolescent cancer. Gynecol Obstet Clin Med 2:161–163. https://doi.org/10.1016/j.gocm.2022.11.002
Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K et al (2006) American society of clinical oncology recommendations on fertility preservation in Cancer patients. J Clin Oncol 24:2917–2931)
Kim SS, Donnez J, Barri P, Pellicer A, Patrizio P, Rosenwaks Z et al (2012) Recommendations for fertility preservation in patients with lymphoma, leukemia, and breast cancer. J Assist Reprod Genet 29:465–468)
Jadoul P, Dolmans MM, Donnez J (2010) Fertility preservation in girls during childhood: is it feasible, efficient and safe and to whom should it be proposed? Hum Reprod Update 16:617–630
Dolmans M-M, Marinescu C, Saussoy P, Van Langendonckt A, Amorim C, Donnez J (2010) Reimplantation of cryopreserved ovarian tissue from patients with acute lymphoblastic leukemia is potentially unsafe. Blood 116:2908–2914
Blumenfeld Z et al (2012) GnRH-agonist for prevention of chemotherapy-induced ovarian damage in young women with breast cancer: a systematic review and meta-analysis. Hum Reprod Update 18(4):388–400
.Senra JC et al (2018) GnRH agonists for ovarian protection during cancer chemotherapy: systematic review and meta-analysis. Reprod Biomed Online 36(5):501–511
Acknowledgements
We thank all the staff of the Reproductive Medicine Center for their contributions.
Funding
This work was supported by Peking University People’s Hospital Research and Development Fund (RDL2022-27), Beijing Research Ward Excellence Program, BRWEP(BRWEP2024W1340801004), National Key R&D Program of China (Grant No.2022YFB3604703) and Peking University People’s Hospital Scientific Research Development Funds (RDJP2023-23).
Author information
Authors and Affiliations
Contributions
Yanru Hou: Project development, Data collection, Data analysis, Manuscript writing.Li Tian, Yifei Cheng and Jianliu Wang: Project development, Data analysis, Manuscript editing. Ziyu Li and Lu Bai: Data analysis. Shuting Li, Jiajia Ai and Cheng Cheng: Data collection.
Corresponding authors
Ethics declarations
Ethics statement
Ethics Committee of Peking University People’s Hospital that approved the study and the committee’s reference number was 2022PHB408-001. And all participants gave informed consent.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hou, Y., Li, Z., Bai, L. et al. Fertility assessment in long-term young female survivors with hematological disease after allogeneic hematopoietic cell transplantation: a single-center real-life cross-sectional study. Ann Hematol 104, 1897–1905 (2025). https://doi.org/10.1007/s00277-025-06275-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-025-06275-4