Abstract
Purpose
Postoperative peritoneal adhesion formation (PAF) is a distressing complication. Leptin, secreted by fat tissues, may be associated with PAF. However, the relationships between PAF and leptin are unclear. This study investigated the impact of leptin on PAF after colorectal tumor resection.
Methods
A cecum cauterization mouse model was used to investigate PAF and its association with leptin. Mice adhesion score (AS) was evaluated on day 7 after treatment. The clinical study included patients who underwent elective colorectal resection with temporary ileostomy between April 2021 and December 2024. The AS was evaluated at the time of ileostomy closure. Patients with the highest AS quartile were classified into the high-AS group; clinical factors associated with PAF were examined. An enzyme-linked immunosorbent assay was used to measure human and murine serum leptin concentrations.
Results
The animal experiment revealed that serum leptin levels on postoperative day 7 were negatively correlated with mice ASs (P = 0.0043, r = -0.6241). In a clinical study, eight patients had a high AS (27.6%). Visceral fat mass and preoperative serum leptin levels were higher in the high-AS group than in the low-AS group. The serum leptin ratio (postoperative value to preoperative value) on postoperative day 7 was lower in the high-AS group. In multivariate analysis, the serum leptin ratio was an independent factor for classifying into the high-AS group.
Conclusions
A decrease in postoperative serum leptin levels was associated with severe PAF. Leptin may be a novel key molecule in PAF.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Avoid common mistakes on your manuscript.
Introduction
Surgical resection of abdominal tumors is one of the most effective treatments for cancers without distant metastases. However, surgical intervention induces peritoneal adhesion formation (PAF), a distressing postoperative complication estimated to occur in 63─97% of patients after abdominal surgery [1,2,3]. PAF may significantly impair the quality of life in postoperative patients with chronic abdominal pain, female infertility, and small bowel obstruction [4,5,6]. Therefore, it is crucial to clarify PAF preventive methods and predictors.
Peritoneal adhesions form when fibrin clots containing immune cells, such as peritoneal macrophages and neutrophils, excessively accumulate in the peritoneal wall, which lacks mesothelial cells [7,8,9,10,11]. In normal peritoneal repair, these clots are fully fibrinolyzed within 72 h. However, if excessive clots accumulate, fibrinolysis becomes impossible, and fibrous structures form within the clots, resulting in PAF [12]. Currently, several materials are used clinically to suppress PAF by covering postoperative mesothelial cell defects [13,14,15], but these materials fail to completely prevent PAF [5, 16]. Regarding the predictors of PAF, clinical factors such as operative time [17, 18], surgical blood loss [17, 18], anastomosis leakage [17, 18], history of previous surgery [3, 17, 18], preoperative C–reactive protein levels [19, 20], and high body mass index (BMI) [19] have been reported as factors related to PAF. These findings suggest that severe surgical stress, acute perioperative inflammation, and chronic inflammation due to underlying diseases contribute to the initiation and development of PAF. However, clinically valuable predictors have yet to be identified. Therefore, the development of new preventive methods and predictors is needed.
Surgeons may encounter various cases and conduct translational research to explore the molecular mechanisms [21]. One hypothesis is that visceral fat is related to PAF, although the details of this mechanism remain unknown [22]. Adipocytes that constitute visceral fat affect various biochemical reactions via the secretion of adipokines, such as leptin and adiponectin [23]. In particular, leptin, which correlates with BMI and body fat [24], is associated with adipose tissue fibrosis [25] and wound healing [26,27,28]. The repair of peritoneal injuries may involve the skin repair system, which is structurally similar to the peritoneum. Therefore, leptin may be associated with that mechanism if visceral fat affects PAF.
Here, we revealed the relationship between leptin and PAF using preclinical data from a mouse model of cecum cauterization and clinical data from patients undergoing colorectal tumor resection. This study suggests that leptin may be a candidate for a novel key molecule in PAF.
Methods
Evaluation of anti-PAF effects by leptin in animal experiments
Eight-week-old female BALB/c mice were purchased from Japan SLC, Inc. (Shizuoka, Japan). All animals were maintained in a specific pathogen-free facility under a 12-h light/12-h dark cycle at 22 °C in the Research Center for Animal Life Science at Shiga University of Medical Science (SUMS). Cecum cauterization was performed on 10- to 12-week-old mice to evaluate the degree of PAF and serum leptin concentration. In brief, mice were anesthetized with 2% isoflurane. A 15 mm midline incision was made in the abdominal wall, and the cecum was removed from the body and cauterized immediately with an electric wire to avoid perforation (Online Resource Fig. 1). The peritoneum and skin were sutured using 6–0 vicryl (Ethicon, D5890). Mice were harvested for heart blood collection and sacrificed between 8 h and 14 days after treatment. An inverted U-shaped incision was made to evaluate the adhesion strength of the cecum and midline wound. In the leptin treatment experiment, mice were injected intraperitoneally with 500 μL of phosphate-buffered saline (PBS) or murine recombinant leptin diluted in PBS to 5 μg/g daily, from the day of surgery to 6 days post-surgery. On postoperative day 7, the mice were sacrificed to collect heart blood and evaluate the mouse adhesion score (AS).
Patient inclusion
This prospective study included 38 patients scheduled to undergo elective colorectal cancer resection with temporary ileostomy and two-stage ileostomy closure between April 2021 and December 2024. The protocol for this research project was approved by the Ethics Committee of SUMS (Approval No. R2020-202) and conformed to the provisions of the Declaration of Helsinki. The study included 29 patients, excluding those for whom ileostomy closure was not performed due to patient condition (n = 7) and those who underwent reoperation between colorectal resection and two-stage ileostomy closure (n = 2) (Fig. 1). Clinical data for all patients were collected, and AS were recorded when they underwent two-stage ileostomy closure. Venous blood samples were collected the day before and 1–7 days after surgery, centrifuged at 2000 g for 6 min, and the supernatant was collected and stored at −80 °C, and thawed immediately before use for measurements.
Clinical data collection
Patient characteristics, including perioperative laboratory data and postoperative findings, were also collected. Smoking history was defined as having smoked at least once in the past or currently, whereas drinking history was defined as drinking at least once per week. Computed tomography was performed using 64- and 320-slice devices (Aquilion™ CX Edition and Aquilion™ ONE, respectively; Canon Medical Systems Corporation, Tochigi, Japan). The slice thickness was set at 5 mm in all patients in accordance with our institutional protocol. Visceral and subcutaneous fat volumes were calculated using 3–dimensional computed tomography with SYNAPSE VINCENT (Fuji Film Co., Tokyo, Japan). These computed tomography data were obtained within 1 month before the primary surgery. The CONUT score, a key component of our research, was calculated based on the serum albumin concentration, total lymphocyte count, and total cholesterol concentration [29].
Definition of AS
Based on previous reports [7, 13, 30], the extent and strength of adhesion tissues were macroscopically evaluated on a 5-point scale (Table 1). In animal experiments, the mouse AS was defined as the sum of [points of the adhesion strength around the cecum] + [points of the adhesion strength around the midline wound]. In clinical research, the extent and strength of adhesion tissue around the ileostomy and at the midline wound were rated. For midline wound AS, severity could not be assessed because adhesions in this area are not typically dissected during actual surgery. Therefore, to balance the weighting between peristomal and midline wound AS, the score for the extent of midline wound adhesions was doubled to approximate the combined evaluation of extent and severity. AS was then defined as follows: [Points for the extent of adhesions around the ileostomy] + [points for the adhesion strength around the ileostomy] + 2 × [points for the extent of adhesions around the midline wound]. Finally, patients were divided into low- and high-AS groups, with high AS defined as the highest quartile.
Measurement of serum leptin levels
The serum leptin concentrations in each patient sample were measured using the Human Leptin DuoSet® ELISA (R&D, DY398-05) according to the manufacturer’s instructions. The serum leptin concentrations in murine samples were measured using the Mouse/Rat Leptin Quantikine® ELISA (R&D, MOB00B) according to the manufacturer’s instructions. Perioperative changes in serum leptin levels were calculated, and the serum leptin ratio was defined as [postoperative serum leptin levels] / [preoperative serum leptin levels].
Statistical analysis
Statistical analyses were performed using the GraphPad Prism 10 (GraphPad Software, San Diego, California, USA). For the mouse experimental data, the Mann–Whitney U test was used to compare two groups, and P < 0.05 was considered significant. In the clinical data, the measured parameter concentrations are shown as the median (interquartile range). Fisher’s exact (for categorical variables) and the Mann–Whitney U test (for continuous variables) were used to evaluate the significance of differences between the two groups, with P < 0.05 considered significant. The Spearman correlation coefficients were used to determine P values and r values in the correlation analysis. Multivariate logistic regression analyses were used to identify risk factors associated with classification into the high-AS group. Prior to regression analysis, continuous explanatory variables were standardized using Z-score transformation to allow for direct comparison of effect sizes. P < 0.05 was considered statistically significant.
Results
Impact of leptin on PAF in mice experiments
We hypothesized that perioperative serum leptin concentrations would change if leptin affects PAF as a circulating hormone. To investigate the perioperative dynamics of serum leptin concentrations, we sacrificed mice at multiple time points before and after cecum cauterization. This experiment revealed that serum leptin concentrations slightly increased 8 h after surgery and then decreased below baseline levels from the next day onward (Fig. 2A). Next, mice were administered exogenous leptin intraperitoneally to investigate whether leptin affected PAF in the cecum cauterization mouse model. The body weight of the mice was nearly identical (mean: 21.41 g, standard error: 1.47 g), with no significant differences before or after treatment between the PBS (n = 19) and leptin (n = 17) groups (Online resource Figs. 2A and B). Contrary to expectations, there were no significant differences in mouse AS and serum leptin levels on postoperative day 7 between the two groups (Online resource Figs. 2C and D). However, serum leptin levels on postoperative day 7 in the PBS group (P = 0.0021, r = −0.6598) and in all samples (P = 0.0112, r = −0.4177) were negatively correlated with mouse AS (Fig. 2B and Online resource Fig. 2E). Thus, these findings from the animal experiments suggested that low postoperative serum leptin levels may be associated with severe PAF.
Effect of serum leptin levels on peritoneal adhesion formation in the cecum cauterization mouse model. A The perioperative serum leptin levels of mice with cecum cauterization were characterized postoperatively on days 0 to 14 (n = 4–5). The serum leptin level on day 0 is the control level. B A scatter plot with a fitted linear regression line shows the relationship between the mouse serum leptin levels and adhesion score in the phosphate buffered saline group (n = 19). Values are presented as means ± standard error of the mean in (A). The Spearman correlation coefficient determined the P values and r in (B)
Clinical study population
To investigate whether serum leptin levels were associated with PAF, we conducted a prospective study. A total of 29 patients were enrolled. Among these, 19 were males (65.5%) and 10 were females (34.5%), with a median age of 67 years (interquartile range [IQR], 55─74). Twenty-six patients (89.7%) were diagnosed with colorectal cancer, two (6.9%) with neuroendocrine tumors, and one with gastrointestinal stromal tumors (3.4%). Colorectal resection was performed in all cases. Among these, 28 were performed laparoscopically (96.6%), including nine robotic surgeries (31.0%), 13 with transanal total mesorectal excisions (44.8%), and seven with lateral lymph node dissections (24.1%). Additionally, neoadjuvant chemotherapy was administered to 10 patients (34.5%), with radiation therapy to nine patients (31.0%). The median AS score was 2 (IQR, 0–5) (Fig. 3A).
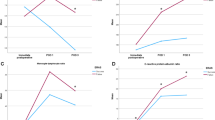
Effect of leptin on peritoneal adhesion formations in the clinical study. A Adhesion scores are evaluated for each assessment item and in total. B A scatter plot with a fitted linear regression line shows the relationship between serum leptin levels and visceral fat mass before colorectal resection. C The characteristics of serum leptin levels preoperatively and on days 1–7 postoperatively in all patients are shown. Day 0 is the preoperative day. (D) Each group’s perioperative serum leptin ratios are characterized postoperatively from day 0 to 7. The reference values are from day 0, the preoperative levels. E Quantification of the relative serum leptin levels on postoperative day 7 in low- (n = 21) and high- (n = 8) AS groups. Values are presented as the median with interquartile range in (A and E) or as means ± standard error of the mean in (C and D). The Spearman correlation coefficient determined the P values and r in (B). Statistical analyses were performed using the Mann–Whitney U test (E): **P < 0.01
Clinical features of the low- and high-AS groups
To study the relationship between PAF and clinical factors, including serum leptin levels, we compared patients in the low- and high-AS groups. Twenty-one patients were included in the low-AS group (72.4%) and eight in the high-AS group (27.6%). Table 2 shows the patients’ background and blood test data before colorectal resection. Body weight (57.0 kg vs. 68.6 kg, P = 0.0371), BMI (20.9 kg/m2 vs. 25.4 kg/m2, P = 0.0070), and visceral fat mass (1633 cm3 vs. 4754 cm3, P = 0.0134) were lower in the low-AS group than in the high-AS group. In addition, the proportion of patients with a drinking history was higher in the low-AS group than in the high-AS group (42.9% vs. 0%, P = 0.0332). Furthermore, in preoperative blood tests, the low-AS group had lower serum leptin levels than the high-AS group (1.77 ng/mL vs. 4.25 ng/mL, P = 0.0474). However, no significant differences were observed in age, sex, presence of diabetes mellitus, smoking history, previous surgery, previous antithrombotic therapy, tumor stage, or previous preoperative therapy. Moreover, no significant differences were observed in other blood test data before colorectal resection, such as white blood cell count, Creatinine, C-reactive protein, and albumin levels, or in preoperative nutritional status, such as the CONUT score.
Table 3 shows patients’ surgical factors and blood test data after colorectal resection in the two groups. The low-AS group had a higher platelet count on the first postoperative day than the high-AS group (17.0 μL × 104 vs. 12.3 μL × 104, P = 0.0398). However, there were no significant differences in other blood test items, such as white blood cell count, creatinine, C-reactive protein, hemoglobin, total bilirubin, prothrombin–activation, albumin, and leptin levels; surgical technique; use of anti-adhesive agents; operative time; blood loss; presence of surgical site infection; date of drain removal; or length of hospital stay.
Therefore, these results suggests that six clinical factors—high body weight, high BMI, high visceral fat mass, preoperative high serum leptin levels, no history of alcohol consumption, and low platelet count on the first postoperative day—are potential candidates that may be associated with severe PAF after colorectal tumor resection.
Clinical impact of the serum leptin ratio on PAF
It is well known that serum leptin concentrations are closely correlated with BMI and body fat [23]. Therefore, we suspected that differences in postoperative leptin levels between the two groups were obscured by differences in basal leptin levels. To validate this hypothesis, we investigated the associations between leptin and PAF using the serum leptin ratio. First, correlations between leptin and body fat were confirmed. As expected, preoperative leptin levels were correlated with visceral (P = 0.0002, r = 0.6446), subcutaneous (P < 0.0001, r = 0.8478), and total fat mass (P < 0.0001, r = 0.8253) (Fig. 3B, Online resource Fig. 3). Next, the dynamics of perioperative serum leptin levels were investigated, revealing that postoperative serum leptin levels transiently increased on postoperative day 1 compared with preoperative levels and decreased to near preoperative levels by postoperative day 7 (Fig. 3C). The serum leptin ratios were higher throughout the postoperative period in the low-AS group than in the high-AS group (Fig. 3D). In particular, the serum leptin ratio on postoperative day 7 was significantly higher in the low-AS group than in the high-AS group (1.18 vs. 0.67, P = 0.0079) (Fig. 3E). Additionally, the serum leptin ratio did not show a correlation with visceral fat (P = 0.4166, r = −0.1630), subcutaneous fat (P = 0.8489, r = −0.0385), and total fat (P = 0.6344, r = −0.0959). Finally, to identify risk factors associated with classification into the high-AS group, we performed multivariate analysis using the factors identified as significant in the univariate analysis. In this analysis, body weight, which overlaps with BMI, and alcohol consumption history, which showed complete separation from the outcome variable, were excluded. As a result, it was found that the serum leptin ratio on postoperative day 7 is an independent factor for classifying into the high-AS group (Odds ratio, 0.0559; 95% confidence interval 0.0020–0.4242; P = 0.0212) (Table 4). Therefore, this study suggested that a decreased postoperative serum leptin ratio is associated with severe PAF.
Discussion
In this study, based on the hypothesis that visceral fat may be associated with severe PAF, we focused on leptin, a hormone secreted by adipose tissue, and demonstrated that a postoperative decrease in serum leptin levels was associated with severe PAF. However, no significant differences were observed in well-known factors associated with PAF, such as operative time and blood loss, as reported in previous studies [17, 18]. Therefore, we will discuss two points: the effect of leptin on PAF and the differences in factors related to PAF from previous studies.
First, this study suggested that a postoperative decrease in serum leptin levels was associated with severe PAF. In the animal experiments, serum leptin levels on postoperative day 7 were negatively correlated with mouse AS. Moreover, in the clinical study, serum leptin ratios on postoperative day 7 were negatively correlated with AS and an independent factor for classifying into the high-AS group. Serum leptin levels are primarily influenced by body fat percentage, and when body fat percentage is equalized, no gender differences in serum leptin levels are observed [24]. Therefore, in animal experiments, inbred mice with the same genetic background, age, and sex were used to minimize experimental variability due to individual differences and to standardize preoperative body weight as much as possible. As a result, serum leptin levels before treatment were expected to be relatively similar across all mice. Thus, differences in postoperative serum leptin levels in mice were considered to have almost the same significance as the changes in serum leptin ratio observed in the clinical data. These findings in both animal and clinical studies suggest that low serum leptin ratios after surgery may promote PAF. Given that leptin can inhibit adipose tissue fibrosis [25], a postoperative decrease in serum leptin may promote PAF due to the formation of strong fibrotic structures, primarily involving adipose tissues, such as the omentum and mesentery. In addition, the low serum leptin ratios in the high-AS group may be due to prolonged postoperative sympathetic nerve stimulation associated with surgical invasion or postoperative infectious complications, which suppress leptin secretion [31, 32]. Therefore, preventing excessive postoperative inflammatory responses and maintaining adequate serum leptin levels may inhibit severe PAF. However, no significant difference was observed in mouse AS when administering exogenous recombinant murine leptin. Two possible reasons for this exist. First, the half-life of the circulating hormone leptin was tightly regulated at 47.3 min [33]; therefore, temporary administration, such as once daily, may not effectively reduce PAF because serum concentrations are not adequately maintained. Second, in the cecum cauterized mouse model used to create severe PAF, fluid resembling abscesses leaked from the PAF tissue during the AS evaluation in some samples from each group. Therefore, these inflammatory complications caused by cecum cauterization may affect the results. Complicating matters, it was difficult to accurately distinguish whether the fluid was due to fecal leakage from dissection or from abscess formation. Therefore, further investigation is needed to clarify how leptin affects PAF.
Second, we discuss the differences in factors related to PAF from previous studies. Although several researchers have shown that operative time and blood loss correlate with PAF [17, 18], these factors were not significantly associated with PAF in the present study. Additionally, we identified the serum leptin ratio on postoperative day 7 as a novel predictor of PAF. One possible reason for these differences is that this study included only patients who underwent surgery using an almost uniform technique for specific diseases, whereas previous studies included surgical techniques for various diseases. Another possible reason is that several previous reports evaluated the presence of PAF based on small bowel obstruction, whereas the present report directly assessed the presence of PAF. By comparing patients with similar surgical stress and including minor PAF that did not contribute to clinical symptoms, we hypothesized that factors related to the more detailed mechanism of PAF could be identified.
This study had a few limitations. First, it excluded patients who underwent reoperation due to anastomotic leakage or other factors between colorectal resection and two-stage ileostomy closure to detect factors associated with PAF accurately. Identifying how various factors affect PAF during regular postoperative intraperitoneal injury repair is important. Second, we could not rule out the influence of other factors on PAF because our study was limited to leptin. Finally, the number of enrolled patients was small, and only East Asian (Japanese) individuals from a single institution were enrolled.
Conclusions
The postoperative decrease in serum leptin after colorectal tumor resection was associated with severe PAF and may serve as a novel predictor of its severity. Thus, elucidating the molecular mechanisms by which leptin affects PAF may lead to the development of novel preventive strategies beyond anti-adhesive agents that cover the peritoneal injury area.
Data availability
The data supporting the results of this study will be available from the corresponding author upon reasonable request.
References
Kössi J, Salminen P, Rantala A, Laato M (2003) Population-based study of the surgical workload and economic impact of bowel obstruction caused by postoperative adhesions. Br J Surg 90:1441–1444. https://doi.org/10.1002/bjs.4272
Menzies D, Ellis H (1990) Intestinal obstruction from adhesions–how big is the problem? Ann R Coll Surg Engl 72:60–63
Strik C, Stommel MW, Ten Broek RP, van Goor H (2015) Adhesiolysis in patients undergoing a repeat median laparotomy. Dis Colon Rectum 58:792–798. https://doi.org/10.1097/DCR.0000000000000405
Okabayashi K, Ashrafian H, Zacharakis E et al (2014) Adhesions after abdominal surgery: a systematic review of the incidence, distribution and severity. Surg Today 44:405–420. https://doi.org/10.1007/s00595-013-0591-8
Chen J, Tang X, Wang Z et al (2023) Techniques for navigating postsurgical adhesions: insights into mechanisms and future directions. Bioeng Transl Med 8:e10565. https://doi.org/10.1002/btm2.10565
Liao J, Li X, Fan Y (2023) Prevention strategies of postoperative adhesion in soft tissues by applying biomaterials: based on the mechanisms of occurrence and development of adhesions. Bioact Mater 26:387–412. https://doi.org/10.1016/j.bioactmat.2023.02.026
Zindel J, Peiseler M, Hossain M et al (2021) Primordial GATA6 macrophages function as extravascular platelets in sterile injury. Science 371:eabe0595. https://doi.org/10.1126/science.abe0595
Wang J, Kubes P (2016) A reservoir of mature cavity macrophages that can rapidly invade visceral organs to affect tissue repair. Cell 165:668–678. https://doi.org/10.1016/j.cell.2016.03.009
Tsai JM, Shoham M, Fernhoff NB et al (2019) Neutrophil and monocyte kinetics play critical roles in mouse peritoneal adhesion formation. Blood Adv 3:2713–2721. https://doi.org/10.1182/bloodadvances.2018024026
Cheong YC, Laird SM, Li TC, Shelton JB, Ledger WL, Cooke ID (2001) Peritoneal healing and adhesion formation/reformation. Hum Reprod Update 7:556–566. https://doi.org/10.1093/humupd/7.6.556
Herrick SE, Wilm B (2021) Post–surgical peritoneal scarring and key molecular mechanisms. Biomolecules 11:692. https://doi.org/10.3390/biom11050692
Arung W, Meurisse M, Detry O (2011) Pathophysiology and prevention of postoperative peritoneal adhesions. World J Gastroenterol 17:4545–4553. https://doi.org/10.3748/wjg.v17.i41.4545
Suto T, Watanabe M, Endo T et al (2017) The primary result of prospective randomized multicenter trial of new spray-type bio-absorbable adhesion barrier system (TCD-11091) against postoperative adhesion formation. J Gastrointest Surg 21:1683–1691. https://doi.org/10.1007/s11605-017-3503-1
Dupré A, Lefranc A, Buc E et al (2013) Use of bioresorbable membranes to reduce abdominal and perihepatic adhesions in 2-stage hepatectomy of liver metastases from colorectal cancer: results of a prospective, randomized controlled phase II trial. Ann Surg 258:30–36. https://doi.org/10.1097/SLA.0b013e3182854949
Watanabe J, Ishida F, Ishida H et al (2019) A prospective multi-center registry concerning the clinical performance of laparoscopic colorectal surgery using an absorbable adhesion barrier (INTERCEED®) made of oxidized regenerated cellulose. Surg Today 49:877–884. https://doi.org/10.1007/s00595-019-01816-7
Ten Broek RPG, Stommel MWJ, Strik C, van Laarhoven CJHM, Keus F, van Goor H (2014) Benefits and harms of adhesion barriers for abdominal surgery: a systematic review and meta-analysis. Lancet 383:48–59. https://doi.org/10.1016/S0140-6736(13)61687-6
Honjo K, Kawai M, Tsuchiya Y et al (2023) Risk factors for small–bowel obstruction after colectomy for colorectal cancer: a retrospective study. Surg Today 53:1038–1046. https://doi.org/10.1007/s00595-023-02674-0
Fu WJ, Xiao X, Gao YH, Hu S, Yang Q (2023) Analysis of risk factors for recurrence and prognosis of adhesive small bowel obstruction. Asian J Surg 46:3491–3495. https://doi.org/10.1016/j.asjsur.2022.09.133
Li G, Zeng Y, Zeng J et al (2023) Analysis of abdominal adhesion using the ileostomy model. Med (Baltim) 102:e35350. https://doi.org/10.1097/MD.0000000000035350
Hellebrekers BWJ, Trimbos-Kemper TCM, Boesten L et al (2009) Preoperative predictors of postsurgical adhesion formation and the Prevention of Adhesions with plasminogen activator (PAPA-study): results of a clinical pilot study. Fertil Steril 91:1204–1214. https://doi.org/10.1016/j.fertnstert.2008.01.052
Noh DY (2021) Translational research in surgical oncology: introduction and my own experience as a surgeon-scientist. Adv Exp Med Biol 1187:3–20. https://doi.org/10.1007/978-981-32-9620-6_1
Arjmand MH (2022) The association between visceral adiposity with systemic inflammation, oxidative stress, and risk of post-surgical adhesion. Arch Physiol Biochem 128:869–874. https://doi.org/10.1080/13813455.2020.1733617
de Medeiros SF, Rodgers RJ, Norman RJ (2021) Adipocyte and steroidogenic cell cross-talk in polycystic ovary syndrome. Hum Reprod Update 27:771–796. https://doi.org/10.1093/humupd/dmab004
Considine RV, Sinha MK, Heiman ML et al (1996) Serum immunoreactive–leptin concentrations in normal-weight and obese humans. N Engl J Med 334:292–295. https://doi.org/10.1056/NEJM199602013340503
Liu Y, Li Y, Liang J et al (2021) The mechanism of leptin on inhibiting fibrosis and promoting browning of white fat by reducing ITGA5 in mice. Int J Mol Sci 22:12353. https://doi.org/10.3390/ijms222212353
Frank S, Stallmeyer B, Kämpfer H, Kolb N, Pfeilschifter J (2000) Leptin enhances wound re-epithelialization and constitutes a direct function of leptin in skin repair. J Clin Inves 106:501–509. https://doi.org/10.1172/JCI9148
Tadokoro S, Ide S, Tokuyama R et al (2015) Leptin promotes wound healing in the skin. PLoS ONE 10:e0121242. https://doi.org/10.1371/journal.pone.0121242
Shibata S, Tada Y, Asano Y et al (2012) Adiponectin regulates cutaneous wound healing by promoting keratinocyte proliferation and migration via the ERK signaling pathway. J Immunol 189:3231–3241. https://doi.org/10.4049/jimmunol.1101739
Ignacio de Ulíbarri J, González-Madroño A, de Villar NG et al (2005) CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp 20:38–45
Uyama N, Tsutsui H, Wu S et al (2019) Anti-interleukin-6 receptor antibody treatment ameliorates postoperative adhesion formation. Sci Rep 9:17558. https://doi.org/10.1038/s41598-019-54175-1
Caron A, Lee S, Elmquist JK, Gautron L (2018) Leptin and brain–adipose crosstalks. Nat Rev Neurosci 19:153–165. https://doi.org/10.1038/nrn.2018.7
Huang TS, Wang YH, Chen SY (2000) The relation of serum leptin to body mass index and to serum cortisol in men with spinal cord injury. Arch Phys Med Rehabil 81:1582–1586. https://doi.org/10.1053/apmr.2000.9173
Hart RA, Dobos RC, Agnew LL, Tellam RL, McFarlane JR (2016) Pharmacokinetics of leptin in female mice. Physiol Res 65:311–320. https://doi.org/10.33549/physiolres.933053
Acknowledgements
The authors thank Ikuko Arikawa, Yumiko Ito, and Sachiko Sawada for their technical assistance with the experiments. We thank Editage (www.editage.jp) for the English language editing.
Funding
The authors have no relevant financial or non-financial interests to disclose. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Study conception and design: T. Maekawa, T. Miyake and M. Tani. Acquisition, analysis, and interpretation of clinical data: T. Maekawa and T. Miyake. Surgery and clinical management: T. Miyake, M. Kojima, S. Tani, T. Matsunaga, Y. Nishina, S. Kaida, H. Maehira, and T. Shimizu. Animal experiments, analysis, and interpretation: T. Maekawa and T. Miyake. Manuscript drafting: T. Maekawa and T. Miyake. Critical revision of the manuscript: M. Kojima, S. Tani, T. Matsunaga, Y. Nishina, S. Kaida, H. Maehira, T. Shimizu, and M. Tani. All authors have approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
Animal studies: All animal experiments were carried out in strict accordance with the Guidelines for the Husbandry and Management of Laboratory Animals of the Research Center for Animal Life Science at SUMS, the guidelines of the Institutional Animal Care and Use Committee, and the Standards Relating to the Care and Fundamental Guidelines for Proper Conduct of Animal Experiment and Related Activities in Academic Research Institutions under the jurisdiction of the Ministry of Education, Culture, Sports, Science and Technology, Japan. All protocols for the animal experiments were approved by the Shiga University of Medical Science Animal Experiment Committee (approval numbers. 2021–9-3, 2021–9-3H1, 2021–9-3H2, and 2021–9-3H3).
Informed consent
Informed consent was obtained from the patients and/or guardians.
Competing interests
The authors declare no competing interests.
Clinical studies
The protocol for this research project was approved by a suitably constituted Ethics Committee of the institution (Committee of SUMS; approval No. R2020-202). and conformed to the provisions of the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
ESM 1
(PDF 152 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Maekawa, T., Miyake, T., Kojima, M. et al. Impact of leptin on postoperative peritoneal adhesion formations in colorectal resection. Int J Colorectal Dis 40, 67 (2025). https://doi.org/10.1007/s00384-025-04851-8
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-025-04851-8