Abstract
Background
Patients after heart transplantation (HTX) present with sinus tachycardia due to graft denervation. As elevated heart rates negatively affect survival, the aim of this study was to analyze the effects of ivabradine vs metoprolol succinate on heart rate, left ventricular (LV) mass and survival following HTX.
Methods
This observational retrospective single-center study assessed 84 patients continuously receiving either ivabradine (n = 40) or metoprolol succinate (n = 44) within 2 years after HTX. Patients with dual therapy (ivabradine and metoprolol succinate), other beta blockers, amiodarone, or digitalis were excluded. Patient characteristics, post-transplant medication, heart rates, LV mass, and survival were investigated.
Results
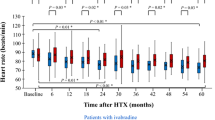
Analysis of patient characteristics, immunosuppressive drug regimen, and post-transplant medication showed no significant differences between groups except for ivabradine and metoprolol succinate. Baseline heart rates differed not significantly between patients treated with ivabradine [87.0 beats per minute (bpm)] and metoprolol succinate (86.2 bpm; P = 0.6395). At 2-year follow-up, patients with ivabradine (76.7 bpm) had a significantly lower heart rate compared to baseline (P < 0.0001) and to metoprolol succinate (82.0 bpm; P = 0.0283). LV mass in patients receiving ivabradine was lower at 2-year follow-up compared to baseline (P = 0.0067) and patients receiving metoprolol succinate (P = 0.0179). Patients with ivabradine had a superior 2-year survival after HTX (P = 0.0049).
Conclusion
Treatment with ivabradine in patients within 2 years after HTX significantly reduced post-transplant heart rate and LV mass and was associated with a superior survival in comparison with patients receiving metoprolol succinate.


Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Swedberg K, Komajda M, Böhm M et al (2010) Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet 376(9744):875–885
Böhm M, Swedberg K, Komajda M et al (2010) Heart rate as a risk factor in chronic heart failure (SHIFT): the association between heart rate and outcomes in a randomised placebo-controlled trial. Lancet 376(9744):886–894
Custodis F, Roggenbuck U, Lehmann N et al (2016) Resting heart rate is an independent predictor of all-cause mortality in the middle aged general population. Clin Res Cardiol 105(7):601–612
Schaeffer BN, Rybczynski M, Sheikhzadeh S et al (2015) Heart rate turbulence and deceleration capacity for risk prediction of serious arrhythmic events in Marfan syndrome. Clin Res Cardiol 104(12):1054–1063
Eick C, Duckheim M, Groga-Bada P et al (2017) Point-of-care testing of cardiac autonomic function for risk assessment in patients with suspected acute coronary syndromes. Clin Res Cardiol 106(9):686–694
Zhang R, Haverich A, Strüber M, Simon A, Pichlmaier M, Bara C (2008) Effects of ivabradine on allograft function and exercise performance in heart transplant recipients with permanent sinus tachycardia. Clin Res Cardiol 97(11):811–819
Zhang R, Bobylev D, Stiefel P, Haverich A, Bara C (2012) Lasting reduction of heart transplant tachycardia with ivabradine is effective and well tolerated: results of 48-month study. Clin Res Cardiol 101(8):631–636
Doesch AO, Celik S, Ehlermann P et al (2007) Heart rate reduction after heart transplantation with beta-blocker versus the selective If channel antagonist ivabradine. Transplantation 84(8):988–996
Doesch AO, Ammon K, Konstandin M et al (2009) Heart rate reduction for 12 months with ivabradine reduces left ventricular mass in cardiac allograft recipients. Transplantation 88(6):835–841
Doesch AO, Mueller S, Erbel C et al (2013) Heart rate reduction for 36 months with ivabradine reduces left ventricular mass in cardiac allograft recipients: a long-term follow-up study. Drug Des Dev Ther 7:1323–1328
Schüler S, Thomas D, Thebken M, Frei U, Wagner T, Warnecke H, Hetzer R (1987) Endocrine response to exercise in cardiac transplant patients. Transplant Proc 19(1 Pt 3):2506–2509
Beckers F, Ramaekers D, Speijer G et al (2004) Different evolutions in heart rate variability after heart transplantation: 10-year follow-up. Transplantation 78(10):1523–1531
Halpert I, Goldberg AD, Levine AB, Levine TB, Kornberg R, Kelly C, Lesch M (1996) Reinnervation of the transplanted human heart as evidenced from heart rate variability studies. Am J Cardiol 77(2):180–183
Koglin J, Gross T, Uberfuhr P, von Scheidt W (1997) Time-dependent decrease of presynaptic inotropic supersensitivity: physiological evidence of sympathetic reinnervation after heart transplantation. J Heart Lung Transplant 16(6):621–628
Schwaiblmair M, von Scheidt W, Uberfuhr P, Ziegler S, Schwaiger M, Reichart B, Vogelmeier C (1999) Functional significance of cardiac reinnervation in heart transplant recipients. J Heart Lung Transplant 18(9):838–845
Bengel FM, Ueberfuhr P, Schiepel N, Nekolla SG, Reichart B, Schwaiger M (2001) Effect of sympathetic reinnervation on cardiac performance after heart transplantation. N Engl J Med 345(10):731–738
Scott CD, McComb JM, Dark JH (1993) Heart rate and late mortality in cardiac transplant recipients. Eur Heart J 14(4):530–533
Dobre D, Borer JS, Fox K et al (2014) Heart rate: a prognostic factor and therapeutic target in chronic heart failure. The distinct roles of drugs with heart rate-lowering properties. Eur J Heart Fail 16(1):76–85
Li J, Franke J, Pribe-Wolferts R et al (2015) Effects of β-blocker therapy on electrocardiographic and echocardiographic characteristics of left ventricular noncompaction. Clin Res Cardiol 104(3):241–249
Tardif JC, Ford I, Tendera M, Bourassa MG, Fox K, INITIATIVE Investigators (2005) Efficacy of ivabradine, a new selective I(f) inhibitor, compared with atenolol in patients with chronic stable angina. Eur Heart J 26(23):2529–2536
Miró Ò, Müller C, Martín-Sánchez FJ et al (2016) BETAWIN-AHF study: effect of beta-blocker withdrawal during acute decompensation in patients with chronic heart failure. Clin Res Cardiol 105(12):1021–1029
DiFrancesco D (1986) Characterization of single pacemaker channels in cardiac sino-atrial node cells. Nature 324(6096):470–473
DiFrancesco D (1991) The contribution of the ‘pacemaker’ current (if) to generation of spontaneous activity in rabbit sino-atrial node myocytes. J Physiol 434:23–40
DiFrancesco D, Camm JA (2004) Heart rate lowering by specific and selective I(f) current inhibition with ivabradine: a new therapeutic perspective in cardiovascular disease. Drugs 64(16):1757–1765
Thollon C, Bedut S, Villeneuve N et al (2007) Use-dependent inhibition of hHCN4 by ivabradine and relationship with reduction in pacemaker activity. Br J Pharmacol 150(1):37–46
Fischer-Rasokat U, Honold J, Lochmann D et al (2016) β-Blockers and ivabradine differentially affect cardiopulmonary function and left ventricular filling index. Clin Res Cardiol 105(6):527–534
Mulder P, Barbier S, Chagraoui A et al (2004) Long-term heart rate reduction induced by the selective I(f) current inhibitor ivabradine improves left ventricular function and intrinsic myocardial structure in congestive heart failure. Circulation 109(13):1674–1679
Monnet X, Colin P, Ghaleh B, Hittinger L, Giudicelli JF, Berdeaux A (2004) Heart rate reduction during exercise-induced myocardial ischaemia and stunning. Eur Heart J 25(7):579–586
Rivinius R, Helmschrott M, Ruhparwar A et al (2017) Comparison of post-transplant outcomes in patients with no, acute or chronic amiodarone use before heart transplantation. Drug Des Dev Ther 11:1827–1837
Rivinius R, Helmschrott M, Ruhparwar A et al (2017) The influence of surgical technique on early posttransplant atrial fibrillation—comparison of biatrial, bicaval, and total orthotopic heart transplantation. Ther Clin Risk Manag 13:287–297
Rivinius R, Helmschrott M, Ruhparwar A et al (2016) Long-term use of amiodarone before heart transplantation reduces significantly early post-transplant atrial fibrillation and is not associated with increased mortality after heart transplantation. Drug Des Dev Ther 10:677–686
Rivinius R, Helmschrott M, Ruhparwar A et al (2014) Analysis of malignancies in patients after heart transplantation with subsequent immunosuppressive therapy. Drug Des Dev Ther 9:93–102
Helmschrott M, Rivinius R, Bruckner T, Katus HA, Doesch AO (2017) Renal function in heart transplant patients after switch to combined mammalian target of rapamycin inhibitor and calcineurin inhibitor therapy. Drug Des Dev Ther 11:1673–1680
Helmschrott M, Rivinius R, Ruhparwar A et al (2015) Advantageous effects of immunosuppression with tacrolimus in comparison with cyclosporine A regarding renal function in patients after heart transplantation. Drug Des Dev Ther 9:1217–1224
Doenst T, Strüning C, Moschovas A et al (2016) Cardiac surgery 2015 reviewed. Clin Res Cardiol 105(10):801–814
Doenst T, Essa Y, Jacoub K et al (2017) Cardiac surgery 2016 reviewed. Clin Res Cardiol 106(11):851–867
Reed RM, Netzer G, Hunsicker L, Mitchell BD, Rajagopal K, Scharf S, Eberlein M (2014) Cardiac size and sex-matching in heart transplantation: size matters in matters of sex and the heart. JACC Heart Fail 2(1):73–83
Boudoulas H, Rittgers SE, Lewis RP, Leier CV, Weissler AM (1979) Changes in diastolic time with various pharmacologic agents: implication for myocardial perfusion. Circulation 60(1):164–169
Guth BD, Heusch G, Seitelberger R, Ross J Jr (1987) Elimination of exercise-induced regional myocardial dysfunction by a bradycardiac agent in dogs with chronic coronary stenosis. Circulation 75(3):661–669
Kjekshus J (1987) Heart rate reduction—a mechanism of benefit? Eur Heart J 8(Suppl L):115–122
Kapadia SR (1999) Cytokines and heart failure. Cardiol Rev 7(4):196–206
Ide T, Tsutsui H, Kinugawa S et al (2000) Direct evidence for increased hydroxyl radicals originating from superoxide in the failing myocardium. Circ Res 86(2):152–157
Schnoor M, Schäfer T, Lühmann D, Sievers HH (2007) Bicaval versus standard technique in orthotopic heart transplantation: a systematic review and meta-analysis. J Thorac Cardiovasc Surg 134(5):1322–1331
Locali RF, Matsuoka PK, Cherbo T, Gabriel EA, Buffolo E (2010) Should biatrial heart transplantation still be performed?: a meta-analysis. Arq Bras Cardiol 94(6):829–840
Grande AM, Rinaldi M, D’Armini AM et al (2000) Orthotopic heart transplantation: standard versus bicaval technique. Am J Cardiol 85(11):1329–1333
Weiss ES, Nwakanma LU, Russell SB, Conte JV, Shah AS (2008) Outcomes in bicaval versus biatrial techniques in heart transplantation: an analysis of the UNOS database. J Heart Lung Transplant 27(2):178–183
Dell’Aquila AM, Mastrobuoni S, Bastarrika G et al (2012) Bicaval versus standard technique in orthotopic heart transplant: assessment of atrial performance at magnetic resonance and transthoracic echocardiography. Interact Cardiovasc Thorac Surg 14(4):457–462
Konertz W, Weyand M, Deiwick M, Scheld HH (1992) Is pretransplant antiarrhythmic drug therapy a risk factor? Transplant Proc 24(6):2677–2678
Blomberg PJ, Feingold AD, Denofrio D et al (2004) Comparison of survival and other complications after heart transplantation in patients taking amiodarone before surgery versus those not taking amiodarone. Am J Cardiol 93(3):379–381
Yerebakan H, Naka Y, Sorabella R et al (2014) Amiodarone treatment prior to heart transplantation is associated with acute graft dysfunction and early mortality: a propensity-matched comparison. J Heart Lung Transplant 33(4):S105
Macdonald P, Hackworthy R, Keogh A, Sivathasan C, Chang V, Spratt P (1991) The effect of chronic amiodarone therapy before transplantation on early cardiac allograft function. J Heart Lung Transplant 10:743–749
Chelimsky-Fallick C, Middlekauff HR, Stevenson WG et al (1992) Amiodarone therapy does not compromise subsequent heart transplantation. J Am Coll Cardiol 20(7):1556–1561
Sanchez-Lazaro IJ, Almenar L, Martinez-Dolz L et al (2006) Does amiodarone influence early mortality in heart transplantation? Transplant Proc 38(8):2537–2538
Kröller-Schön S, Schulz E, Wenzel P et al (2011) Differential effects of heart rate reduction with ivabradine in two models of endothelial dysfunction and oxidative stress. Basic Res Cardiol 106(6):1147–1158
Mangiacapra F, Colaiori I, Ricottini E et al (2017) Heart rate reduction by IVabradine for improvement of ENDothELial function in patients with coronary artery disease: the RIVENDEL study. Clin Res Cardiol 106(1):69–75
Sabbah HN, Gupta RC, Kohli S, Wang M, Zhang K, Sharad R (2014) Heart rate reduction with ivabradine improves left ventricular function and reverses multiple pathological maladaptations in dogs with chronic heart failure. ESC Heart Fail 1:94–102
Fröhlich H, Torres L, Täger T et al (2017) Bisoprolol compared with carvedilol and metoprolol succinate in the treatment of patients with chronic heart failure. Clin Res Cardiol 106(9):711–721
Acknowledgements
This study was supported in part by research grants from the Faculty of Medicine, University of Heidelberg (Physician Scientist Scholarship to Ann-Kathrin Rahm). We thank Viola Deneke and Berthold Klein for their assistance and advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest in this work.
Rights and permissions
About this article
Cite this article
Rivinius, R., Helmschrott, M., Ruhparwar, A. et al. Control of cardiac chronotropic function in patients after heart transplantation: effects of ivabradine and metoprolol succinate on resting heart rate in the denervated heart. Clin Res Cardiol 107, 138–147 (2018). https://doi.org/10.1007/s00392-017-1165-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-017-1165-3