Abstract
Purpose
To evaluate the clinical outcomes and prognosis of patients undergoing laparoscopic surgery for tubo-ovarian abscess (TOA) and identify risk factors for pelvic inflammatory disease (PID) recurrence.
Methods
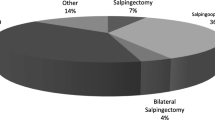
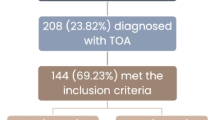
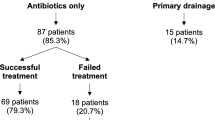
We conducted a retrospective cohort analysis including 98 women who underwent laparoscopic surgery for TOA at the Department of Obstetrics and Gynecology at the Bern University Hospital from January 2011 to May 2021. The primary outcome studied was the recurrence of PID after TOA surgery. Clinical, laboratory, imaging, and surgical outcomes were examined as possible risk factors for PID recurrence.
Results
Out of the 98 patients included in the study, 21 (21.4%) presented at least one PID recurrence after surgery. In the univariate regression analysis, the presence of endometriosis, ovarian endometrioma, and the isolation of E. coli in the microbiology cultures correlated with PID recurrence. However, only endometriosis was identified as an independent risk factor in the multivariate analysis (OR (95% CI): 9.62 (1.931, 47.924), p < 0.01). With regard to the time of recurrence after surgery, two distinct recurrence clusters were observed. All patients with early recurrence (≤ 45 days after TOA surgery) were cured after 1 or 2 additional interventions, whereas 40% of the patients with late recurrence (> 45 days after TOA surgery) required 3 or more additional interventions until cured.
Conclusion
Endometriosis is a significant risk factor for PID recurrence after TOA surgery. Optimized therapeutic strategies such as closer postsurgical follow-up as well as longer antibiotic and hormonal therapy should be assessed in further studies in this specific patient population.




Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Ford GW, Decker CF (2016) Pelvic inflammatory disease. Dis Mon 62(8):301–305. https://doi.org/10.1016/j.disamonth.2016.03.015
Trent M, Bass D, Ness RB, Haggerty C (2011) Recurrent PID, subsequent STI, and reproductive health outcomes: findings from the PID evaluation and clinical health (PEACH) study. Sex Transm Dis 38(9):879–881. https://doi.org/10.1097/olq.0b013e31821f918c
Weström L, Joesoef R, Reynolds G, Hagdu A, Thompson SE (1992) Pelvic inflammatory disease and fertility. A cohort study of 1,844 women with laparoscopically verified disease and 657 control women with normal laparoscopic results. Sex Transm Dis 19(4):185–92
Chappell CA, Wiesenfeld HC (2012) Pathogenesis, diagnosis, and management of severe pelvic inflammatory disease and tuboovarian abscess. Clin Obstet Gynecol 55(4):893–903. https://doi.org/10.1097/grf.0b013e3182714681
Siegenthaler F, Krause E, Mueller MD (2020) Management of pelvic inflammatory disease. Ther Umsch 77(4):164–170. https://doi.org/10.1024/0040-5930/a001171
Landers DV, Sweet RL (1985) Current trends in the diagnosis and treatment of tuboovarian abscess. Am J Obstet Gynecol 151(8):1098–1110. https://doi.org/10.1016/0002-9378(85)90392-8
Landers DV, Sweet RL (1983) Tubo-ovarian abscess: contemporary approach to management. Rev Infect Dis 5(5):876–884. https://doi.org/10.1093/clinids/5.5.876
Wiesenfeld HC, Sweet RL (1993) Progress in the management of tuboovarian abscesses. Clin Obstet Gynecol 36(2):433–444. https://doi.org/10.1097/00003081-199306000-00022
Hiller N, Sella T, Lev-Sagi A, Fields S, Lieberman S (2005) Computed tomographic features of tuboovarian abscess. J Reprod Med 50(3):203–208
Peterson HB, Galaid EI, Cates W Jr (1990) Pelvic inflammatory disease. Med Clin North Am 74(6):1603–1615. https://doi.org/10.1016/s0025-7125(16)30497-7
Workowski KA, Bolan GA (2015) Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 64(Rr-3):1–137
Workowski KA et al (2021) Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep 70(4):1–187. https://doi.org/10.15585/mmwr.rr7004a1
Jonathan Ross MC, Evans C, Lyons D, Dean G, Cousins D. PPI representative, 2018 United Kingdom National Guideline for the Management of Pelvic Inflammatory Disease. 2018, BASHH Guidelines.
Asadollahi K, Hastings IM, Beeching NJ, Gill GV, Asadollahi P (2011) Leukocytosis as an alarming sign for mortality in patients hospitalized in general wards. Iran J Med Sci 36(1):45–49
Shapiro MF, Greenfield S (1987) The complete blood count and leukocyte differential count. An approach to their rational application. Ann Intern Med 106(1):65–74. https://doi.org/10.7326/0003-4819-106-1-65
Miettinen AK, Heinonen PK, Laippala P, Paavonen J (1993) Test performance of erythrocyte sedimentation rate and C-reactive protein in assessing the severity of acute pelvic inflammatory disease. Am J Obstet Gynecol 169(5):1143–1149. https://doi.org/10.1016/0002-9378(93)90271-j
Keckstein J et al (2021) The #Enzian classification: a comprehensive non-invasive and surgical description system for endometriosis. Acta Obstet Gynecol Scand 100(7):1165–1175
Clarizia R et al (2021) Inflammation calls for more: severe pelvic inflammatory disease with or without endometriosis. Outcomes on 311 laparoscopically treated women. J Gynecol Obstet Hum Reprod 50(3):101811. https://doi.org/10.1016/j.jogoh.2020.101811
Tai FW et al (2018) Association of pelvic inflammatory disease with risk of endometriosis: a nationwide cohort study involving 141,460 individuals. J Clin Med 7(11):379
Elizur SE et al (2014) Pelvic inflammatory disease in women with endometriosis is more severe than in those without. Aust NZ J Obstet Gynaecol 54(2):162–165. https://doi.org/10.1111/ajo.12189
Chen MJ et al (2004) Increased occurrence of tubo-ovarian abscesses in women with stage III and IV endometriosis. Fertil Steril 82(2):498–499
Gao Y et al (2021) Risk factors for the development of tubo-ovarian abscesses in women with ovarian endometriosis: a retrospective matched case–control study. BMC Womens Health 21(1):43
Padilla SL (1993) Ovarian abscess following puncture of an endometrioma during ultrasound-guided oocyte retrieval. Hum Reprod 8(8):1282–1283
Yaron Y et al (1994) Infected endometriotic cysts secondary to oocyte aspiration for in-vitro fertilization. Hum Reprod 9(9):1759–1760
Younis JS et al (1997) Late manifestation of pelvic abscess following oocyte retrieval, for in vitro fertilization, in patients with severe endometriosis and ovarian endometriomata. J Assist Reprod Genet 14(6):343–346
Ho HN, Wu MY, Yang YS (1997) Peritoneal cellular immunity and endometriosis. Am J Reprod Immunol 38(6):400–412
Chen C et al (2017) The microbiota continuum along the female reproductive tract and its relation to uterine-related diseases. Nat Commun 8(1):875
Villette C et al (2016) Risks of tubo-ovarian abscess in cases of endometrioma and assisted reproductive technologies are both under—and overreported. Fertil Steril 106(2):410–415
Grimes DA (2000) Intrauterine device and upper-genital-tract infection. Lancet 356(9234):1013–1019. https://doi.org/10.1016/s0140-6736(00)02699-4
Kapustian V et al (2018) Is intrauterine device a risk factor for failure of conservative management in patients with tubo-ovarian abscess? An observational retrospective study. Arch Gynecol Obstet 297(5):1201–1204. https://doi.org/10.1007/s00404-018-4690-z
Granberg S, Gjelland K, Ekerhovd E (2009) The management of pelvic abscess. Best Pract Res Clin Obstet Gynaecol 23(5):667–678. https://doi.org/10.1016/j.bpobgyn.2009.01.010
Krivak TC, Cooksey C, Propst AM (2004) Tubo-ovarian abscess: diagnosis, medical and surgical management. Compr Ther 30(2):93–100. https://doi.org/10.1007/s12019-004-0003-5
Saini S, Gupta N, Aparna BG, Arora DR (2003) Role of anaerobes in acute pelvic inflammatory disease. Indian J Med Microbiol 21(3):189–92
Brook I (2008) Microbiology and management of abdominal infections. Dig Dis Sci 53(10):2585–2591. https://doi.org/10.1007/s10620-007-0194-6
Goharkhay N, Verma U, Maggiorotto F (2007) Comparison of CT- or ultrasound-guided drainage with concomitant intravenous antibiotics vs. intravenous antibiotics alone in the management of tubo-ovarian abscesses. Ultrasound Obstet Gynecol 29(1):65–9. https://doi.org/10.1002/uog.3890
McNeeley SG, Hendrix SL, Mazzoni MM, Kmak DC, Ransom SB (1998) Medically sound, cost-effective treatment for pelvic inflammatory disease and tuboovarian abscess. Am J Obstet Gynecol 178(6):1272–1278. https://doi.org/10.1016/s0002-9378(98)70333-3
Reed SD, Landers DV, Sweet RL (1991) Antibiotic treatment of tuboovarian abscess: comparison of broad-spectrum beta-lactam agents versus clindamycin-containing regimens. Am J Obstet Gynecol 164(6pt1):1556–61. https://doi.org/10.1016/0002-9378(91)91436-z
Topçu HO et al (2015) Risk factors for adverse clinical outcomes in patients with tubo-ovarian abscess. J Obstet Gynaecol 35(7):699–702. https://doi.org/10.3109/01443615.2014.991294
Jiang X et al (2019) Clinical value of early laparoscopic therapy in the management of tubo-ovarian or pelvic abscess. Exp Ther Med 18(2):1115–1122. https://doi.org/10.3892/etm.2019.7699
Chu L et al (2019) Effectiveness and adverse events of early laparoscopic therapy versus conservative treatment for tubo-ovarian or pelvic abscess: a single-center retrospective cohort study. Gynecol Obstet Invest 84(4):334–342. https://doi.org/10.1159/000493855
Kinay T et al (2016) The value of ultrasonographic tubo-ovarian abscess morphology in predicting whether patients will require surgical treatment. Int J Gynaecol Obstet 135(1):77–81. https://doi.org/10.1016/j.ijgo.2016.04.006
Silva F et al (2015) Minimally invasive approach of tubo-ovarian abscesses. Rev Bras Ginecol Obstet 37(3):115–118. https://doi.org/10.1590/so100-720320150005257
Brun JL et al (2016) Updated French guidelines for diagnosis and management of pelvic inflammatory disease. Int J Gynaecol Obstet 134(2):121–125. https://doi.org/10.1016/j.ijgo.2015.11.028
Nakayama K et al (2013) Surgical treatment outcomes of serious chronic tubo-ovarian abscess: a single-center series of 20 cases. Clin Exp Obstet Gynecol 40(3):377–380
Acknowledgements
We would like to thank all participants in our study.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
ZTM: protocol and project development, data collection and management, data analysis, manuscript writing and editing. NK: protocol and project development, manuscript writing and editing. NS: data collection and management. IS: manuscript writing and editing. MMD: protocol and project development, manuscript writing and editing.
Corresponding author
Ethics declarations
Conflict of interest
Authors A, B, and C declare they have no financial interests. Author D has received speaker honoraria from Company Bayer. Author E has received a research grant from Inno Suisse Foundation and speaker honoraria from Companies Bayer, Roche, and Storz.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. The ethical approval was granted by the Ethics Committee of Switzerland, the IRB (Institutional Review Board for research ethics, Bern) and was registered with the number 2021-01194.
Informed consent
Due to the retrospective design of the study no informed consent was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zografou Themeli, M., Nirgianakis, K., Neumann, S. et al. Endometriosis is a risk factor for recurrent pelvic inflammatory disease after tubo-ovarian abscess surgery. Arch Gynecol Obstet 307, 139–148 (2023). https://doi.org/10.1007/s00404-022-06743-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-022-06743-6