Abstract
Background
Krüppel-like factor 5 (KLF5) is recognized as a tumor mediator in multiple types of tumors. Nevertheless, whether KLF5 plays a role in gallbladder cancer (GBC) remains to be elucidated. This study aims to clarify the role of KLF5 in the proliferation, migration and angiogenesis in GBC cells.
Methods
The expressions of KLF5 and platelet-derived growth factor subunit A (PDGFA) in GBC cell lines were analyzed by qRT-PCR and western blot assay. Cell proliferation was assessed utilizing the Cell Counting Kit-8 assay and EDU staining. Cell apoptosis was evaluated using flow cytometry, and apoptosis-related proteins was examined by western blotting. The migratory and invasive capabilities were evaluated utilizing wound healing and Transwell. Angiogenesis was assessed by ELISA, tube formation assay and western blot. The interaction between KLF5 and PDGFA was confirmed by ChIP assay, as well as luciferase reporter assay.
Results
In this study, we discovered that the levels of KLF5 and PDGFA were upregulated in GBC cells. Silencing of KLF5 reduced the viability and suppressed the proliferation of GBC cells, as well as promoting the apoptosis. In addition, KLF5 silencing restrained the invasion and migration and angiogenesis in NOZ and GBC-SD cells. KLF5 transcription activated PDGFA expression and KLF5 was proved to bind to PDGFA promoter in NOZ cells. Following the silencing of PDGFA, the proliferation, invasion, migration, angiogenesis and apoptosis exhibited similar changes to KLF5 silencing. Additionally, PDGFA overexpression reversed the effects of KLF5 silencing on NOZ cells.
Conclusion
Collectively, our results suggest that KLF5 regulates GBC cell proliferation, invasion, migration, angiogenesis, as well as apoptosis, via mediating PDGFA transcriptionally, which might provide a novel therapeutic strategy for treatment of human GBC.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Avoid common mistakes on your manuscript.
Introduction
Gallbladder cancer (GBC) is the most common and aggressive malignant tumor of the biliary tract, and a significantly higher incidence rate in women compared to men (Roa et al. 2022; Wernberg and Lucarelli 2014; Krell and Wei 2019). Although the overall incidence rate of GBC is not high, many patients are diagnosed at middle or late stages of the disease, resulting in a low rate of radical surgical resection and difficulties in achieving optimal therapeutic effects through radiotherapy (Schmidt et al. 2019; Hickman and Contreras 2019). In addition, GBC has a high degree of malignancy, and due to its anatomical characteristics, it is very easy to invade the liver, resulting in an extremely poor prognosis (Gallbladder cancer 2022). Recent studies suggest that the development of GBC is related to the mutation of many genes and environmental factors, with research primarily focusing on the genes and pathways involved in cancer biology (Javle et al. 2019). The external environmental factors lead to the mutation of the genes of key protein molecules in the signaling pathway, which affects the normal signaling, and ultimately leads to the formation of cancer (Cherkassky and D’Angelica 2019). Therefore, the development of novel therapeutic targets is of great significance for the treatment of GBC.
Krüppel-like factors (KLFs) belong to transcription factors that are involved in a variety of biological processes and diseases (Gao et al. 2015). Thirteen of these factors contain three highly conserved and tandemly linked zinc finger domains at the C-terminus, which bind to CACC-rich or GC-rich sequences in DNA to regulate the transcription of downstream target genes (Rane et al. 2019). Krüppel-like factor 5 (KLF5) is a member of the KLFs family, consisting of four exons and three introns (Li et al. 2021). KLF5 is transcribed into an mRNA of 1720 bp, which encodes a protein with a molecular weight of 55 kDa, consisting of 446 amino acids (Palioura et al. 2022). KLF5 has been reported to be involved in various biological functions, such as cellular stemness (Lee et al. 2023). It is specifically expressed in a variety of cells and plays an important role in development, metabolism and cellular pluripotency (Zeng et al. 2023). Although it is known that KLF5 participates in the malignant process of cancer through transcriptional activation of downstream genes, it’s role in GBC remains unexplored.
In this study, we analyzed the expression of KLF5 in a GBC database GSE139682 database and found that KLF5 was highly expressed in GBC. Thus, we investigated the biological role of KLF5 and its potential mechanism in GBC.
Materials and methods
Cell culture
Human gallbladder epithelium cell line H69, GBC cell lines SGC-996, GBC-SD and NOZ and the human umbilical vein endothelial cells (HUVECs) provided by Cellverse Co., Ltd. (Shanghai, China) were cultivated in high-glucose Dulbecco’s modified Eagle medium supplemented with 10% fetal bovine serum (FBS, Guangzhou Perseco Biotechnology Co., Ltd.) and 1% antibiotic at 37 °C in the presence of 5% CO2.
Cell transfection
The KLF5-specific pcDNA overexpression vector (Ov-KLF5), platelet-derived growth factor subunit A (PDGFA)-specific pcDNA overexpression vector (Ov-PDGFA), and the empty vector (Ov-NC), KLF5-specific siRNA (siRNA-KLF5-1/2), PDGFA-specific siRNA (siRNA- PDGFA-1/2) and corresponding control (siRNA-NC) were provided by GeneChem (Shanghai, China). Lipofectamine 3000 was applied for the transfection of NOZ cells and GBC-SD cells in light of recommended instructions.
CCK-8 assay
After the inoculation into 96-well plates, transfected NOZ cells or GBC-SD cells were cultivated in DMEM for 48 h. After removing the culture medium, 10 µL of WST-8 was added to each well to further cultivate the cells. The optical density (OD) at 450 nm was assessed using a microplate reader.
EDU staining
To detect cell proliferation following the transfection of NOZ cells and GBC-SD cells with siRNA-KLF5, with or without Ov-PDGFA, the BeyoClick™ EDU Cell Proliferation Kit with Alexa Fluor 488 was utilized. After labeling the cells with EDU, they were fixed in 4% paraformaldehyde and permeabilized with PBS containing 0.3% Triton X-100. Subsequently, Click Additive Solution was added to incubate the cells in darkness for 30 min, followed by observation with a fluorescence microscope.
Cell apoptosis analysis
Cell apoptosis was assessed using the FITC Annexin V/PI Apoptosis Detection Kit I. Cells in 6-well plates were stained with PI and Annexin V-fluorescein isothiocyanate (FITC) in the dark. Flowjo software (Tree Star, Ashland, OR, USA) was used for apoptosis analysis.
Wound healing assay
NOZ cells and GBC-SD cells, subjected to the indicated treatment, were inoculated into 6-well plates and cultured until 80–90% confluence was reached. Wounds in the cell monolayers were made with the help of white pipette tips. Then, the PBS-rinsed cells were cultured in serum-free medium for 24 h at 37 °C. The wounds were recorded at 0 and 24 h utilizing an inverted microscope.
Transwell assay
NOZ cells and GBC-SD cells subjected to the indicated treatment were inoculated into the serum-free medium in the upper chambers. DMEM medium supplemented with 10% FBS was added to in the lower chamber. After incubation for 24 h, invaded cells on the lower face were subjected to fixation with 100% methanol and staining with Crystal Violet Staining Solution. Images of cells that migrated through the membranes were captured utilizing an inverted microscope. Five random fields were selected for quantification.
Endothelial tube formation assay
HUVECs were seeded in 96-well plate that had been pre-coated with Matrigel. Conditioned medium (CM) was collected from different treatment groups after being cultured for 24 h in DMEM. HUVECs were incubated in 200 µL of CM for 12 h before image taking.
ELISA
ELISA kits were applied to determine the levels of VEGFA in cell supernatants in accordance with the suggested protocol. Finally, the OD value was measured using a microplate reader at a wavelength of 450 nm.
Chromatin immunoprecipitation (ChIP) assay
ChIP assays were performed using the EZ ChIP™ Kit. The cells were cross-linked with 1% formaldehyde for 10 min at 37 °C and quenched with 2.5 M glycine for 5 min at room temperature. To amplify the KLF5 binding site, DNA was immunoprecipitated from sonicated cell lysates using a KLF5 antibody and subjected to PCR.
Luciferase reporter assay
A luciferase reporter assay was performed to verify the combination between KLF5 and PDGFA. Fragments of the human PDGFA promoter containing the wildtype (WT) or mutant (MUT) target sites for KLF5 were cloned into a pGL3-Control Vector, generating the reporter vector PDGFA-wild-type (PDGFA-WT) or PDGFA-mutated-type (PDGFA-MUT), respectively. Then, NOZ cells were co-transfected with luciferase reporter vectors and either Ov-NC or Ov-KLF5 using lipofectamine 2000 (Invitrogen). After 48 h post-transfection, the relative luciferase activities were measured using the Dual-Luciferase Reporter Assay.
RT-qPCR
The cDNA was synthesized from total RNA isolated from sample cells using Trlzol® reagent and a commercial RevertAid™ cDNA Synthesis Kit. Subsequently, qRT-PCR was performed on the ABI PRISM 7900 Sequence Detection System using SYBR Green Master Mix (Applied Biosystems, Foster City, CA, USA). The comparative Ct method was employed to calculate relative gene expression levels (Smolarz et al. 2020).
Western blot assay
Proteins were isolated from cells utilizing RIPA lysis buffer and quantified using the BCA protein assay kit in light of standard protocol. After the separation with 8% SDS-PAGE, the proteins were transferred onto PVDF membranes. Then, the membranes were blocked with 5% non-fat milk, followed by incubation with primary antibodies specific to KLF5, PDGFA, BCL2, Bax, cleaved caspase3, MMP2, MMP9, VEGFA, VEGFR2 and GAPDH at 4 °C overnight. Subsequently, the membranes were incubated with HRP-labeled secondary antibody at room temperature. The protein bands were visualized by using an ECL detection system, and the density of the band was quantified by ImageJ software.
Statistical analysis
All data displayed in the format of mean ± SD were analyzed by GraphPad Prism 8 software. Significant differences between two groups were analyzed by Student’s t-test, while the comparisons among multiple groups were performed using one-way analysis of variance followed by Tukey’s post hoc test. The data were considered statistically significant when P is lower than 0.05.
Results
KLF5 silencing inhibits the proliferation and induces apoptosis of GBC cells
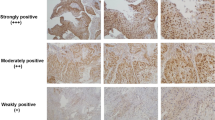
Firstly, we analyzed the expression of KLF5 in a GBC database GSE139682 and found that KLF5 was significantly highly expressed in GBC (Supplementary Material 1). To explore the role of KLF5 in the development of GBC, we then identified the expression of KLF5 in various GBC cell lines. As depicted in Fig. 1A, the protein levels of KLF5 and PDGFA were evidently upregulated in several GBC cell lines compared with the control cells. Among them, NOZ cells exhibited the highest expression levels of KLF5 and PDGFA, followed by GBC-SD cells. Therefore, NOZ and GBC-SD cells were selected for the subsequent experiments. Then, we transfected siRNA-KLF5-1/2 into both NOZ and GBC-SD cells to silence KLF5. The transfection efficiency was evaluated by western blot assay (Figs. 1B and 2A). Notably, siRNA-KLF5-1 showed a more effective knockdown effect in both NOZ and GBC-SD cells, and thus siRNA-KLF5-1 was selected for the following assays (named as siRNA-KLF5). Results from the CCK-8 and EDU assay revealed that KLF5 silencing remarkably suppressed the proliferation of NOZ cells (Fig. 1C-D) and GBC-SD cells (Fig. 2B-C) compared to the siRNA-NC. Furthermore, the apoptosis rates of NOZ cells (Fig. 1E) and GBC-SD cells (Fig. 2D) transfected with siRNA-KLF5 were noticeably elevated, as evidenced by increased levels of Bax and cleaved caspase3, alongside a decreased Bcl-2 level (Figs. 1F and 2E).
KLF5 silencing inhibits the proliferation and induces apoptosis of NOZ cells. A, The protein levels of KLF5 and PDGFA in GBC cells were detected by western blotting. B, The protein level of KLF5 in NOZ cells transfected with siRNA-KLF5 was detected by western blotting. CCK-8 (C) and EDU assay (D) were performed to assess NOZ cell proliferation. E, Cell apoptosis in NOZ cells transfected with siRNA-KLF5 was elucidated by TUNEL assay. F, Western bolt assay was utilized to determine apoptotic-related protein levels. Results are the mean ± SD. ***P < 0.001
KLF5 silencing inhibits the proliferation and induces apoptosis of GBC-SD cells. A, The protein level of KLF5 in GBC-SD cells transfected with siRNA-KLF5 was detected by western blotting. CCK-8 (B) and EDU assay (C) were performed to assess GBC-SD cell proliferation. D, Cell apoptosis in GBC-SD cells transfected with siRNA-KLF5 was elucidated by TUNEL assay. E, Western bolt assay was utilized to determine apoptotic-related protein levels. Results are the mean ± SD. ***P < 0.001
KLF5 knockdown represses the invasion, migration and angiogenesis of NOZ cells
Next, we investigated the impact of KLF5 interference on the malignant progression of GBC cells. The migratory and invasive capacities of NOZ cells (Fig. 3A-B) and GBC-SD cells (Fig. 4A-B) transfected with siRNA-KLF5 were significantly decreased in comparison with the NC group. Additionally, KLF5 interference resulted in reduced levels of MMP2 and MMP9 in both NOZ cells (Fig. 3C) and GBC-SD cells (Fig. 4C). Meanwhile, the results of the tube formation assay revealed that KLF5 knockdown reduced the ability of the tube-like structure formation of HUVECs stimulated with CM from NOZ cells (Fig. 3D) and GBC-SD cells (Fig. 4D) transfected with siRNA-KLF5. Moreover, KLF5 silencing resulted in decreased expression levels of VEGFA and VEGFR2 in both NOZ cells (Fig. 3E-F) and GBC-SD cells (Fig. 4E-F).
KLF5 knockdown represses the invasion, migration and angiogenesis of NOZ cells. A-B NOZ cell migration and invasion with or without siRNA-KLF5, detected by wound healing, as well as transwell assays. C, Protein expression of migration-related MMP2 and MMP9 in NOZ cells with or without siRNA-KLF5, detected by western blot. D, The formation of tube-like structures in NOZ cell supernatant, detected by HUVEC tube formation assay. E, Western bolt assay was used to assess VEGFA and VEGFR2 protein levels. Results are the mean ± SD. ***P < 0.001
KLF5 knockdown represses the invasion, migration and angiogenesis of GBC-SD cells. (A-B) GBC-SD cell migration and invasion with or without siRNA-KLF5, detected by wound healing, as well as transwell assays. C, Protein expression of migration-related MMP2 and MMP9 in GBC-SD cells with or without siRNA-KLF5, detected by western blot. D, The formation of tube-like structures in GBC-SD cell supernatant, detected by HUVEC tube formation assay. E, Western bolt assay was used to assess VEGFA and VEGFR2 protein levels. Results are the mean ± SD. ***P < 0.001
KLF5 activates PDGFA expression transcriptionally
Next, we further explored the mechanism involved in the function of KLF5 in GBC. Through the GSE139682 dataset, we found that the expression of PDGFA was increased in GBC (Supplementary Material 2). And both PDGFA mRNA and protein levels were specifically decreased in the KLF5-silenced NOZ cells (Fig. 5A-B). Then, we overexpressed KLF5 in NOZ cells and the results from RT-qPCR and western blot assay revealed that KLF5 overexpression remarkably elevated the mRNA and protein level of both KLF5 and PDGFA (Fig. 5C–E). ChIP assay detected markedly enriched PDGFA in the anti- KLF5 group compared to the IgG group (Fig. 5F). Additionally, the result of luciferase reporter assay showed a high level of luciferase activity in cells co-transfected with Ov-KLF5 and PDGFA-WT, and the PDGFA-MUT groups remains the unchanged luciferase activity (Fig. 5G).
KLF5 activates PDGFA expression transcriptionally. mRNA expression (A) and protein level (B) of PDGFA in NOZ cells transfected with siRNA-KLF5 were identified by qRT-PCR and western blotting. C, mRNA expression of KLF5 in NOZ cells transfected with Ov-KLF5 was identified by qRT-PCR. C–E, mRNA expression and protein level of KLF5 and PDGFA in NOZ cells transfected with Ov-KLF5 were assessed by qRT-PCR and western blotting. F, Relative PDGFA enrichment in cells incubated with IgG or anti-KLF5, assessed by ChIP assay. G, Relative luciferase activity of NOZ cells, illustrated by dual-luciferase reporter assay. Results are the mean ± SD. **P < 0.01, ***P < 0.001
PDGFA silencing attenuates proliferation and accelerates apoptosis of NOZ cells
To investigate the role of PDGFA in KLF5-regulated NOZ cells, we transfected NOZ cells with siRNA-PDGFA-1/2 to silence PDGFA expression (Fig. 6A). siRNA-PDGFA-1 demonstrated a more effective knockdown effect and was chosen for the following assays (named as siRNA-PDGFA). Silencing of PDGFA resulted in reduced the cell viability and decreased number of positive cells in NOZ cells (Fig. 6B-C). Moreover, siRNA-PDGFA treatment exacerbated cell apoptosis in NOZ cells compared with the negative control, with decreased levels of Bcl-2 and elevated levels of Bax and cleaved caspase 3 (Fig. 6D-E).
PDGFA silencing attenuates proliferation and accelerates apoptosis of NOZ cells. A, The protein level of PDGFA in NOZ cells transfected with siRNA-PDGFA was detected by western blotting. CCK-8 (B) and EDU assay (C) were performed to assess NOZ cell proliferation. D, Cell apoptosis was identified by TUNEL assay. E, Western bolt assay was used to assess apoptotic-related protein levels. Results are the mean ± SD. ***P < 0.001
PDGFA silencing restrains the invasion, migration and angiogenesis of NOZ cells
As illustrated in Fig. 7A–C, the invasive and migratory abilities of cells treated with siRNA-PDGFA were lower than those in the negative control cells, with decreased levels of MMP2 and MMP9. Additionally, the result of tube formation assay revealed the inhibitory effect of the cell supernatant silencing PDGFA on the tube-like structure formation of HUVECs (Fig. 7D). In addition, silencing PDGFA reduced the levels of VEGFA and VEGFR2 in NOZ cells (Fig. 7E-F).
PDGFA silencing restrains the invasion, migration and angiogenesis of NOZ cells. A-B NOZ cell migration and invasion in NOZ cells transfected with siRNA-PDGFA, measured by wound healing, as well as transwell assays. C, The protein expression of migration-related MMP2 and MMP9 in NOZ cells transfected with or without siRNA- PDGFA, identified by western blot. D, The formation of tube-like structures in NOZ cell supernatant, assessed by HUVEC tube formation assay. E, Western bolt assay was used to assess VEGFA and VEGFR2 protein levels. Results are the mean ± SD. **P < 0.01, ***P < 0.001
PDGFA overexpression reverses the effects of KLF5 silencing in NOZ cells
As shown in Fig. 8A, transfection with Ov-PDGFA resulted in an increase in the PDGFA levels in NOZ cells. Following PDGFA overexpression, the viability of NOZ cells was increased compared with the siRNA-KLF5 group (Fig. 8B). Furthermore, the result of EdU staining displayed that PDGFA overexpression increased the positive cell number in the absence of KLF5 (Fig. 8C). In addition, the apoptosis rate in cells co-transfected with siRNA-KLF5 and ov-PDGFA was obviously decreased compared with that in cells transfected with siRNA-KLF5 (Fig. 8D), which was in line with western blot results that Bcl-2 level was increased but the contents of Bax and cleaved caspase 3 were decreased by PDGFA overexpression (Fig. 8E). PDGFA overexpression reversed the migratory and invasive capacities of KLF5-silenced cells, as evidenced by elevated levels of MMP2 and MMP9 (Fig. 9A–C). Furthermore, PDGFA overexpression promoted the tube-like structure formation ability of HUVECs (Fig. 9D). The level of VEGFA and VEGFR2 in KLF5-silenced cells was also reversed by PDGFA overexpression (Fig. 9E-F).
PDGFA overexpression reverses the effects of KLF5 silencing on proliferation and apoptosis in NOZ cells. A, The protein level of PDGFA in NOZ cells transfected with Ov-PDGFA was detected by western blotting. CCK-8 (B) and EDU assay (C) were performed to assess NOZ cell proliferation. D, Cell apoptosis was detected by TUNEL assay. E, Western bolt assay was used to assess apoptotic-related protein levels. Results are the mean ± SD. ***P < 0.001 versus Control. ##P < 0.01, ###P < 0.001 versus siRNA-KLF5 + Ov−NC
Overexpression of PDGFA reverses the effects of KLF5 silencing on invasion, migration and angiogenesis in NOZ cells. A-B NOZ cell migration and invasion in NOZ cells transfected with siRNA-KLF5 with or without Ov-PDGFA, elucidated by wound healing, as well as transwell assays. C, The protein expression of MMP2 and MMP9 in NOZ cells that were transfected with siRNA-KLF5 with or without Ov-PDGFA, detected by western blot. D, The formation of tube-like structures in NOZ cell supernatant, detected by HUVEC tube formation assay. E, Western bolt assay was used to assess VEGFA and VEGFR2 protein levels. Results are the mean ± SD. ***P < 0.001 versus Control or Control(TCM) + HUVEC. ###P < 0.001 versus siRNA-KLF5 + Ov−NC or siRNA-KLF5 + Ov−NC(TCM) + HUVEC
Discussion
The incidence of GBC has been increasing annually, with most patients diagnosed at an advanced stage, thereby losing the opportunity of radical surgery and resulting in a poor overall prognosis (Baiu et al. 2018). As a representative therapeutic mode in the era of precision medicine, molecular targeted therapy offers high specificity and minimal toxicity and side effects (Abou-Alfa 2019). Therefore, there is a need to explore additional GBC targets and gene interactions, as well as to identify biomarkers suitable for targeted therapy, in order to implement individualized treatment strategies for GBC patients. This study demonstrated that the expressions of KLF5 and PDGFA were elevated in GBC cells. Silencing KLF5 inhibited the proliferation, invasion, migration and angiogenesis, while inducing apoptosis of NOZ cells and GBC-SD cells. Furthermore, KLF5 was found to transcriptionally regulate PDGFA expression in NOZ cells. Notably, silencing PDGFA produced effects analogous to KLF5 knockdown, while PDGFA overexpression reversed the effects of KLF5 silencing in NOZ cells.
The KLF family, especially KLF5, plays a key role in the progression of a variety of tumors, with aberrant expression of KLF5 linked to the development of renal, thyroid, and breast cancers (Jiang et al. 2022; Takagi et al. 2020; Zuo et al. 2023). KLF5 is a cytosolic transcription factor containing three tandem zinc-finger structures at the carboxyl terminus, primarily involved in regulating gene transcription by binding to target genes (Maehara et al. 2015). Numerous studies have confirmed the adverse effects of elevated KLF5 expression in various tumors, including breast (Qin et al. 2015), gastric (Chen et al. 2020), and prostate cancers (Ma et al. 2020). These findings suggest that abnormal upregulation of KLF5 may act as a pan-carcinogen. Bioinformatics analysis of the GSE139682 database revealed that KLF5 is highly expressed in GBC. However, the precise role of KLF5 in GBC remains unclear. We validated KLF5 expression in multiple GBC cell lines in vitro, confirming high expression levels consistent with our bioinformatics analysis. Furthermore, silencing KLF5 in NOZ and GBC-SD cells significantly inhibited their invasive and migratory capacities. Western blot analysis demonstrated increased expression of Bax and cleaved caspase-3, along with decreased levels of Bcl-2, MMP2, and MMP9 in the siRNA-KLF5 group. Angiogenesis, a critical process in tumor malignant progression, profoundly influences growth, invasion, and metastasis (Rotoli et al. 2017). VEGFA and its receptor VEGFR2 are essential molecules involved in tumor angiogenesis. In tube formation assays, we showed that KLF5 silencing significantly reduced the tube formation ability of HUVECs induced by NOZ and GBC-SD cells while downregulating VEGFA and VEGFR2 expression. These results indicate that, similar to other tumors, high KLF5 expression in GBC promotes malignant progression. This finding enhances our understanding of KLF5’s role in GBC and provides a comprehensive characterization of its involvement in cancer.
Wu et al. reported that KLF5 exacerbates tumor progression and contributes to PARP inhibitor resistance in ovarian cancer (Wu et al. 2023). Chen et al. revealed that KLF5 contributed to the proliferation of gastric cancer through the regulation of p21 and CDK4 (Chen et al. 2020). Another study demonstrated that KLF5 promotes esophageal squamous cell carcinoma via the activation of FGFBP1 transcriptionally (Wang et al. 2023), suggesting that KLF5 may be involved in the malignant progression of various cancers by activating downstream genes. To investigate potential downstream transcription factors of KLF5, this study utilized the JASPAR database to predict that KLF5 can transcriptionally activate PDGFA expression. PDGFA has been identified as a downstream target gene of miR-194-5p, and overexpression of miR-194-5p inhibits the proliferation invasion and migration of bladder cancer cells (Lu et al. 2022). Existing study showed that human UTP14a promoted angiogenesis by upregulating PDGFA expression in colorectal cancer (Ren et al. 2019). Also, high PDGFA expression has been associated with poor prognosis in esophageal squamous cell carcinoma (Han et al. 2021). In addition, silencing FOXE1 has been shown to promote proliferation, migration and invasion of PTC cells by regulating PDGFA expression (Ding et al. 2019). These findings suggest that PDGFA may function as an oncogene and contribute to the malignant progression of tumors. In the present study, we confirmed the binding of PDGFA and KLF5 through ChIP assay and luciferase reporter assay. Meanwhile, we found that silencing PDGFA significantly inhibited the proliferation, invasion and migration of NOZ cells as well as the angiogenesis capacity of HUVECs induced by NOZ. Importantly, PDGFA overexpression reversed the influences of KLF5 silencing on proliferation, metastasis and angiogenesis, as well as apoptosis in NOZ cells.
However, several limitations of the current study must be acknowledged. First, while the study observed high expression of KLF5 in GBC using a bioinformatics approach, and validated this finding in various GBC cell lines, it did not include a sufficient number of tumor and adjacent non-tumor tissues for further validation of KLF5 expression. This limitation should be addressed in future studies. Additionally, this study primarily employed cellular experiments, thus, to confirm the roles of KLF5 and PDGFA in GBC and elucidate their interactions, further validation through the tumor xenograft experiment is required. Moreover, previous research indicates that VEGFA binding to VEGFR2 activates the tyrosine kinase activity of VEGFR2, initiating a cascade of intracellular signaling pathways such as PI3K/Akt, PLCγ, and ERK1/2, which in turn promote angiogenesis (Wang et al. 2019). Therefore, further investigation into the mechanisms by which KLF5 inhibition affects GBC cell proliferation, invasion, migration, and angiogenesis is warranted.
Conclusion
In summary, we have demonstrated for the first time that silencing KLF5 exerts a suppressive effect on GBC progression, and the role of KLF5 in GBC cell proliferation, metastasis, angiogenesis and apoptosis may be related to it’s transcriptional regulation of PDGFA.
Data availability
No datasets were generated or analysed during the current study.
References
Abou-Alfa GK (2019) Gallbladder cancer, a forgotten global cancer problem. Chin Clin Oncol 8(4):30
Baiu I, Visser B (2018) Gallbladder Cancer. JAMA 320(12):1294
Chen P, Qian XK, Zhang YF et al (2020) KLF5 promotes proliferation in gastric cancer via regulating p21 and CDK4. Eur Rev Med Pharmacol Sci 24(8):4224–4231
Cherkassky L, D’Angelica M (2019) Gallbladder Cancer: managing the incidental diagnosis. Surg Oncol Clin N Am 28(4):619–630
Ding Z, Ke R, Zhang Y et al (2019) FOXE1 inhibits cell proliferation, migration and invasion of papillary thyroid cancer by regulating PDGFA. Mol Cell Endocrinol 493:110420
Gao Y, Ding Y, Chen H et al (2015) Targeting Krüppel-like factor 5 (KLF5) for cancer therapy. Curr Top Med Chem 15(8):699–713
Han N, Zhang YY, Zhang ZM et al (2021) High expression of PDGFA predicts poor prognosis of esophageal squamous cell carcinoma. Med (Baltim) 100(20):e25932
Hickman L, Contreras C (2019) Gallbladder Cancer: diagnosis, Surgical Management, and adjuvant therapies. Surg Clin North Am 99(2):337–355
Javle M, Zhao H, Abou-Alfa GK (2019) Systemic therapy for gallbladder cancer. Chin Clin Oncol 8(4):44
Jiang D, Qiu T, Peng J et al (2022) YB-1 is a positive regulator of KLF5 transcription factor in basal-like breast cancer. Cell Death Differ 29(6):1283–1295
Krell RW, Wei AC (2019) Gallbladder cancer: surgical management. Chin Clin Oncol 8(4):36
Lee E, Cheung J, Bialkowska AB (2023) Krüppel-like factors 4 and 5 in colorectal tumorigenesis. Cancers 15(9):24
Li J, Liu L, Zhou WQ et al (2021) Roles of Krüppel-like factor 5 in kidney disease. J Cell Mol Med 25(5):2342–2355
Lu X, Hu K, Tan Q et al (2022) Silencing SNHG1 suppresses viability, Proliferation and Invasion of Gallbladder Carcinoma Cells via Targeting miR-194-5p. Ann Clin Lab Sci 52(5):707–720
Ma JB, Bai JY, Zhang HB et al (2020) KLF5 inhibits STAT3 activity and tumor metastasis in prostate cancer by suppressing IGF1 transcription cooperatively with HDAC1. Cell Death Dis 11(6):466
Maehara O, Sato F, Natsuizaka M et al (2015) A pivotal role of Krüppel-like factor 5 in regulation of cancer stem-like cells in hepatocellular carcinoma. Cancer Biol Ther 16(10):1453–1461
Palioura D, Lazou A, Drosatos K (2022) Krüppel-like factor (KLF)5: an emerging foe of cardiovascular health. J Mol Cell Cardiol 163:56–66
Qin J, Zhou Z, Chen W et al (2015) BAP1 promotes breast cancer cell proliferation and metastasis by deubiquitinating KLF5. Nat Commun 6:8471
Rane MJ, Zhao Y, Cai L (2019) Krϋppel-like factors (KLFs) in renal physiology and disease. EBioMedicine 40:743–750
Ren P, Sun X, Zhang C et al (2019) Human UTP14a promotes angiogenesis through upregulating PDGFA expression in colorectal cancer. Biochem Biophys Res Commun 512(4):871–876
Roa JC, García P, Kapoor VK, Maithel SK, Javle M, Koshiol J (2022) Gallbladder cancer. Nat Rev Dis Primers 8(1):69. https://doi.org/10.1038/s41572-022-00398-y
Rotoli D, Pérez-Rodríguez ND, Morales M et al (2017) IQGAP1 in Podosomes/Invadosomes Is Involved in the Progression of Glioblastoma Multiforme Depending on the Tumor Status. Int J Mol Sci 18(1):13
Schmidt MA, Marcano-Bonilla L, Roberts LR (2019) Gallbladder cancer: epidemiology and genetic risk associations. Chin Clin Oncol 8(4):31
Smolarz B, Szyllo K, Romanowicz H (2020) The genetic background of endometriosis: can ESR2 and CYP19A1 genes be a potential risk factor for its development? Int J Mol Sci 21(21):1
Takagi Y, Sakai N, Yoshitomi H et al (2020) High expression of Krüppel-like factor 5 is associated with poor prognosis in patients with colorectal cancer. Cancer Sci 111(6):2078–2092
Wang L, Feng Y, Xie X et al (2019) Neuropilin-1 aggravates liver cirrhosis by promoting angiogenesis via VEGFR2-dependent PI3K/Akt pathway in hepatic sinusoidal endothelial cells. EBioMedicine 43:525–536
Wang F, Luo M, Cheng Y (2023) KLF5 promotes esophageal squamous cell cancer through the transcriptional activation of FGFBP1. Med Oncol 41(1):17
Wernberg JA, Lucarelli DD (2014) Gallbladder cancer. Surg Clin North Am 94(2):343–360
Wu Y, Chen S, Shao Y et al (2023) KLF5 promotes tumor progression and Parp Inhibitor Resistance in Ovarian Cancer Adv Sci 10(31):e2304638
Zeng L, Zhu Y, Moreno CS et al (2023) New insights into KLFs and SOXs in cancer pathogenesis, stemness, and therapy. Semin Cancer Biol 90:29–44
Zuo Q, Xu Q, Li Z et al (2023) Kruppel-like factor 5 enhances proliferation, lipid droplet formation and oxaliplatin resistance in colorectal cancer by promoting fatty acid binding protein 6 transcription. Anticancer Drugs 34(10):1171–1182
Funding
This study was supported by the Health Science and Technology Program of Zhejiang Province [2024KY1360].
Author information
Authors and Affiliations
Contributions
The authors confirm contribution to the paper as follows: study conception and design: Xiaowei Lu, Kai Zhao; data collection: Xiaowei Lu, Kui Hu; analysis and interpretation of results: Xiaowei Lu, Kui Hu, Dandan Zhangn, Xuefeng Yin, Jifeng Nie; draft manuscript preparation: Xiaowei Lu, Kai Zhao. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial interests.
Ethical approval
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lu, X., Hu, K., Zhang, D. et al. KLF5 silencing restrains proliferation, invasion, migration and angiogenesis of gallbladder carcinoma cells by transcriptional regulation of PDGFA. J Cancer Res Clin Oncol 151, 11 (2025). https://doi.org/10.1007/s00432-024-06059-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00432-024-06059-9