Abstract
Purpose
Transferring adult cancer patients from the hospital to the home environment for home parenteral nutrition (HPN) can be challenging. There is limited real-world data on how those affected perceive this situation. Our aim was to assess the quality of life (QoL) on HPN and the benefits and burdens from the cancer patient's perspective.
Methods
This observational study from Germany examined the QoL on HPN on the basis of the Functional Assessment of Cancer Therapy – G questionnaire (FACT-G). The benefits and burdens of HPN were assessed using predefined questions and answers tailored to the situation of this patient group.
Results
139 adults with advanced solid tumors in a palliative setting at 10 hospitals in Germany were eligible for the study. The follow-up was 12 weeks. At week 4, the Least-square (LS) mean (95% CI) change from baseline in the total FACT-G score was 0.9 (-2.4; 4.2) points, indicating QoL stability. HPN was associated with few complications, with a low rate of hospital readmission due to catheter-related issues (3.8%; n = 5). In the patient assessment of the benefits of HPN, the LS mean values at Week 4 ranged between 7.6 and 8.5 on a 10-point Likert scale. The most commonly perceived burden was "restricted mobility".
Conclusion
With thorough preparation for home parenteral nutrition, the transition from hospital to home care environment works well. QoL is largely maintained through HPN, and cancer patients perceive this situation as not or minimally burdensome alongside their underlying disease, although many patients found the limited mobility to be a burden.
Trial Registration number
NCT03425435 / Date of registration: February 01, 2018.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Avoid common mistakes on your manuscript.
Background
Many patients were discharged from hospital with HPN since the first patients were treated with this option in the 1960s, and the development of home delivery of these therapies has revolutionized the field of clinical nutrition [1]. Advances in delivery systems, formulations and services have permitted HPN to become a standard therapy for patients with intestinal failure. Although not all studies have demonstrated a benefit of parenteral nutrition (PN), there is a general consensus on the importance of supporting cancer patients to improve their QoL [2,3,4], even if the results of QoL assessments in studies have been inconclusive [5, 6]. Clinical studies demonstrate that PN can increase or stabilize body weight, preserve fat-free mass, and improve the Karnovsky index and overall body functions [7,8,9,10,11].
Most patients discharged from hospital with an indication for HPN suffer from cancer. Antitumor therapy itself and tumor-associated changes in metabolism may lead to alteration of a patient’s nutritional status. Mucositis, vomiting, nausea, diarrhea and obstruction often impair the uptake of food and nutrients. To combat malnutrition in cancer, HPN is indicated in patients who cannot fulfil their nutritional requirements by enteral absorption and who are able to continue this therapy outside of an acute care setting [12].
However, ensuring the provision of HPN to patients can be challenging, requiring complex teamwork among multiple participants to ensure optimal care and minimize burdens on the patients. To avoid major complications, such as infection of the central venous catheter, correct handling and strict hygiene is mandatory [13]. Many parties are involved in the management of HPN: the pharmacy supplies the PN, the physician is responsible for the indication and nutritional plan, the healthcare insurance covers the expenses, a supplier for medical devices (bandaging material etc.) and a care team to perform the therapy (connection/disconnection of PN) is needed. From the patient's point of view, long-term HPN may fundamentally change daily life, and this challenge is compounded by the constraints of the malignant disease, concomitant therapies and frequent medical visits.
Based on the authors' experience, it is common practice in the German healthcare system for hospital patients receiving parenteral nutrition to be discharged abruptly and with very short notice when transitioning from hospital care to home care. This often leaves only a few days to make the necessary preparations and adjustments. A good interlocking of all key participants is required to collect and distribute the relevant information, to secure proper training for those involved and to have all utilities and equipment at hand when the patient arrives. Although standards are available (especially for hygiene and the performance of HPN), experience of the players is pivotal for the successful establishment of PN at home and for the prevention of mistakes and problems later on [12].
The successful implementation of HPN involves managing the transition from the inpatient to the home-based care (discharge management), the organization of the HPN at home or in a care facility, possessing expertise in providing care to patients with HPN and maintaining consistent adherence to quality standards of care [12, 14]. However, there are few real-world data on how well discharge management and the establishment of HPN work, as well as how HPN is perceived from the patient's perspective. Therefore, the aim of this observational study was to examine these aspects more closely and to investigate the quality of life of patients on HPN.
Methods
Study design and participants
This is a prospective, single-arm, multisite, non-interventional study. Patients with advanced cancer were recruited by hospital physicians (internists) who routinely initiated PN during the inpatient stay and planned to continue to prescribe the PN in an outpatient setting following discharge. The decision regarding PN in the individual patient was made at the discretion of the treating doctors in the hospital.
Eligible patients were adult males and females with solid malignancy who received an initial prescription for PN during their hospital stay that included daily requirements for at least the macronutrients glucose and amino acids. In most patients, the PN also contained lipids. Study participants were expected to receive HPN for at least 28 days. Further inclusion criteria comprised an ECOG (Eastern Co-operative Oncology Group) performance status ≤ 3 and a signed informed consent. Patients could not participate if they lacked full legal capacity or a legal guardian, were not fluent in German language, had a PN contraindication, were pregnant or breastfeeding, or had a concurrent participation in other clinical studies that required deviations from the hospital’s routine PN procedures.
Outcome measures
The primary objective was to compare the patient's QoL before and four weeks after hospital discharge using the results from the FACT-G [15]. Key secondary objectives included assessment of discharge management by the patient and the attending hospital doctor, patient assessment of the benefits and burden of HPN, PN-associated complications (catheter infections) and hospital readmissions, the frequency of HPN interruptions or early discontinuations, and the course of the nutritional status (body weight (bw) and body mass index (BMI)) with HPN.
Clinical and nutritional parameters, including patient-reported parameters, were collected along the entire continuum of care of HPN patients. At each visit, participating patients were asked to complete the FACT-G and another questionnaire on HPN management and well-being. This HPN questionnaire assessed patient satisfaction with discharge management using a 10-point Likert scale (1 = worst possible satisfaction, 10 = highest possible satisfaction). In addition, four categorical (nominal) questions were asked about the quality of discharge and home-based care management, which patients could answer with “yes” or “no” (see Fig. 2). Hospital physicians were also asked to rate discharge management from their perspective. For this purpose, physicians answered two categorical (ordinal) questions with a predefined list of answer options to choose from (see Table 1). Patient perceptions of the benefits and burdens of HPN were assessed using 7 categorical (nominal) questions on mobility, nighttime disturbances, time consumption (expenditure of time for the implementation of HPN), environmental disturbances, disturbances from infusion pump noise, lack of independence, and other aspects, and were answered by patients with “yes” or “no” (see Table 2). In addition, outpatient or office-based general practitioners or oncologists were asked to document HPN-specific clinical parameters. The nutritional status had to be assessed at baseline with nutritional risk screening (NRS).
Data collection
The observation period was about 3 months and included a documentation before discharge (Visit 1), and at about 1 week (Visit 2), 4 weeks (Visit 3), and 12 weeks (Visit 4) after discharge. Clinical data were collected at Visit 1 by the participating hospital, and upon the subsequent visits by the treating general practitioner or oncologist (if possible). The physician transferred the data to the participating hospital with the patient’s consent. The data from the three sources (hospital, patient, primary care physician) were entered into an electronic case report form (eCRF) by hospital staff. The first set of patient questionnaires were filled out by the patients during their hospital stay. Patient questionnaires for Visit 2, 3 and 4 were handed out to patients at the hospital in advance of the regular visit times. Patients were encouraged to complete the questionnaires themselves whenever possible but were allowed to request assistance. To ensure that the questionnaires were returned, the patients were reminded at regular intervals by the participating site.
Data analysis
For the analysis of the collected data, we applied inferential and descriptive statistics. Continuous parameters were presented with the number of observations, arithmetic mean, standard deviation, minimum, lower quartile (Q25), median, upper quartile (Q75), and maximum. Categorical parameters were presented with absolute and relative frequencies within respective categories. Mean changes in total FACT-G scores between baseline (Visit 1) and Visits 2 through 4 were each presented with corresponding 95% confidence intervals (CI). Analysis of covariance (ANCOVA) were applied on the change in FACT-G from baseline to Visit 3 with baseline as covariate and study site as fixed effects in the model. LS mean of changes were presented including the corresponding 95% CI based on the t-distribution and the residual error from the model. Analyses were applied analogously for all continuous secondary endpoints.
Results
Patient profiles
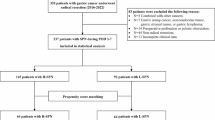
This health outcome study was conducted between April 19, 2019 (first patient in), and December 14, 2021 (last patient out), and enrolled 142 patients across 10 hospitals in Germany with advanced cancer in a palliative setting, of which 139 were eligible for home parenteral nutrition. Out of these, 133 patients started HPN. 60 patients had completed at least 21 days of HPN at Visit 3, and 41 patients had completed at least 70 days at Visit 4. During the study 31 out of 133 patients died, 31 were lost to follow-up, 24 patients ended HPN during the observational period, and 5 patients dropped out for other reasons.
The patient baseline characteristics are summarized in Table 3. The mean age was 64.4 (SD 11.7) years, with a range of 25 to 92 years. The main purposes of PN per patient stated by hospital physicians included "adequate intake of protein, energy, etc." in 72 (51.8%) patients and "improvement in nutritional status" in 37 (26.6%) patients. Less frequent purposes were "maintenance of nutritional status" in 18 (12.9%) patients, "improving QoL" in 7 (5.0%) patients, and "enabling physical activity" in 4 (2.9%) patients. For one patient (0.7%) all of the above purposes were selected. 74.8% (n = 104) received partial, and 25.2% (n = 35) full PN via a venous port in 90.6% (n = 126) of the cases. Further venous accesses included a peripherally inserted central catheter (PICC; 5.8%), a Hickman/Broviac catheter (1.4%), or others (2.2%). 108 patients (77.7%) had received chemotherapy in the last 3 months before hospital discharge (no data: n = 2). 44 patients continued chemotherapy after discharge, 27 patients received radiotherapy and 19 patients received immunotherapy post-discharge.
Discharge management and patient satisfaction with preparation for discharge
After hospital discharge, the vast majority (94.0%; n = 125) of patients who started HPN (n = 133) went home; 1.5% were admitted to a nursing home, 1.5% to a rehabilitation facility and 0.8% to a hospice (missing data: 2.3%).
To avoid an interruption in care, 33.8% (n = 45) of patients were prescribed HPN by the hospital for the first few days at home. The initial conversation about the upcoming discharge, involving participants such as patients, relatives, hospital doctors, the nutrition team, nursing services, or others, occurred a median of 3.0 days before discharge (mean ± SD: 6.1 ± 8.5 days). Additionally, 78.2% (n = 104) of patients received a repeated explanation of the discharge steps. A discharge notification from the hospital went out to the treating physician before discharge for 16.5% (n = 22) of the patients. Joint planning for post-discharge care was conducted for 92.5% (n = 123) of the patients (Fig. 1). 82.7% (n = 110) received nutritional counseling, during which the target amount and administration method of parenteral nutrition were discussed together with the patient and, if necessary, their relatives or the responsible nursing staff, with the goal of ensuring an adequate intake of energy as well as macro- and micronutrients while considering the patient’s daily routine.
When they were discharged, 90.6% (n = 126) of the patients felt that they had been well informed about the HPN and the next steps (Fig. 2). On a Likert scale of 1 (worst possible satisfaction) to 10 (highest possible satisfaction), they rated their satisfaction with the discharge management between 7.8 and 8.3 (LS means). The ratings were similar at each visit during the study (95% CI): 8.3 (8.0–8.6) at discharge (n = 132); 7.9 (7.5–8.2) at Week 1 (n = 93); 7.8 (7.3–8.3) at Week 4 (n = 69); 8.2 (7.8–8.6) at Week 12 (n = 48). The broadest 95% CI with 7.3 to 8.3 was observed at week 4. The attending hospital physicians rated the discharge management in 94.2% (n = 131) of the patient cases as very good or rather good, but mentioned the high time consumption that arises from the discharge management in planned HPN (n = 21; 15.1%) and sometimes found it difficult to identify and contact persons responsible for post-discharge and follow-up care (n = 9; 6.5%). In 51.1% (n = 71) of the cases, there were no concerning issues in discharge management from the hospital doctor’s (usually the ward doctor) perspective (Table 1).
Quality of life on HPN
The primary objective of this study was to evaluate the patient’s QoL before and four weeks after discharge from hospital. The mean changes in total scores of the FACT-G from Visit 1 to Visit 3 were evaluated to answer this question. At Visit 3, the LS mean (95% CI) change from baseline in total FACT-G score was 0.9 (-2.4; 4.2) points and remained stable among the 60 patients who had completed HPN for at least 21 days. Table 4 shows the results for the FACT-G subscores (physical, social, emotional, and functional wellbeing). At Visit 2 (Week 1; n = 45), the LS mean (95% CI) changes in total scores of the FACT-G from baseline were 0.8 (-1.8; 3.4) points, and 1.1 (-2.6; 4.8) points at Visit 4 (Week 12; n = 36). In addition, the influence of HPN on patient well-being was also recorded in the additional HPN questionnaire (“How significantly was your quality of life in the past 7 days influenced by the parenteral nutrition?”). Here, most patients reported that the HPN had rather little or no impact on their QoL: 62.4% (n = 83; missing data: 16.5%) at discharge, 54.1% (n = 72; missing data / no HPN anymore: 28.6%) at week 1, 33.9% (n = 45; missing data / no HPN anymore: 48.8%) at week 4, and 21.8% (n = 29; missing data / no HPN anymore: 68.4%) at week 12.
Patient perception of benefits and burdens of HPN
The mean (SD) duration of HPN was 7.1 (5.7) weeks, and the total duration of PN including the hospital and home periods comprised 8.5 (5.9) weeks. Patient’s perception of the benefits of HPN was rated on a Likert scale of 1 (worst possible satisfaction) to 10 (highest possible satisfaction). LS mean scores ranged from 7.6 to 8.5, with the widest 95% confidence interval (7.4 to 8.3) observed at Visit 3 (Week 4). Scores from Visit 1 showed a slight decline during the first four weeks (Week 1: -0.4; Week 4: -0.3) but improved in subsequent weeks (Week 12: 0.6). The most burdensome aspects of PN for patients were restricted mobility, followed by night-time disruptions and lack of independence (Table 2). Treatment gaps in HPN were reported by 14.4% (n = 19) of patients at Week 1, 13.5% (n = 18) at Week 4, and 11.3% (n = 15) at Week 12. Reasons given for deviating from the prescribed HPN amount included “the patient does not tolerate it well”, “it takes too long”, “disturbing influences” or “other”.
Complications and hospital readmission
At discharge, 61.7% (n = 82) of patients on HPN were free of bacterial infection. Among the remaining patients, 34.6% (n = 46) had no clinical symptoms but displayed laboratory values suggestive of systemic infection, 1.5% (n = 2) exhibited clinical symptoms of systemic infection and 2.3% (n = 3) had a local infection. Since discharge, 7.5% (n = 10) reported catheter infection, while 24.1% (n = 32) were unsure if they had catheter infection. Additionally, 23.3% (n = 29) reported nausea and 9.8% (n = 13) experienced edema during HPN. Most patients rated PN tolerability as very good (57.9% at Visit 1 and 26.3% at Visit 4) or satisfactory (27.8% and 9.8%). Hospital readmissions were documented for 51.1% (n = 68) of patients and were mostly due to the underlying disease in 40.6% (n = 54) of the cases. 3.8% (n = 5) of the patients had catheter related issues. PN was continued during the hospital stay in 36.8% (n = 49) of the cases.
Effect of HPN on nutritional status
To assess malnutrition in the enrolled patients, the NRS method (n = 120; 86.3%), NRS-BIA (n = 15; 10.8%), NRS-SGA (n = 1; 0.7%), NRS-SGA-BIA (n = 1; 0.7%), or NRS-Other (n = 1; 0.7%; “Other” was not further specified) were used; for one patient, no data were available. An NRS score ≥ 3 indicates a high risk of or clear malnutrition and is generally a prerequisite for receiving parenteral nutrition.
In most cases, HPN met the macro- and micronutrient and energy needs of patients: 31.7% (n = 19) at Week 1, 46.7% (n = 28) at Week 4, and 33.3% (n = 20) at Week 12 (missing data / not on HPN anymore: 35.5%, n = 21 at Week 4; 36.7%, n = 22 at Week 1 and Week 12, 18.3%, n = 11 at Week 12). At Week 12, an estimated body weight gain without edema of 1.6 (95% CI: 0.3; 2.8) kg and an increase in BMI of 0.5 (95% CI:0.1; 0.9) kg/m2 were observed (Table 5). Serum albumin increased by 1.0 g/L at Week 1, by 1.4 g/L at Week 4 and by 1.8 g/L at Week 12. CRP levels decreased by 8.1 mg/L at Week 1 and by 7.0 mg/L at Week 4, but increased by 4.4 mg/L from baseline at Week 12.
Discussion
This non-interventional healthcare study from Germany focused on QoL and patient-perceived challenges during HPN. It also examined patient satisfaction with the management of the transition from hospital discharge to HPN care in outpatient settings (i.e., at home, in a nursing home, or hospice). Additionally, we included hospital doctors to assess their satisfaction with discharge management. To the best of our knowledge, this is the first report on the transition from hospital discharge to outpatient HPN care in patients with advanced solid tumors in a palliative setting in Germany.
Other studies have estimated the prevalence of malnutrition in patients with advanced cancer to be over 70% [16, 17]. Malnutrition is becoming an increasingly prevalent indication for HPN [18], accounting for 25 to 60% of all HPN indications in European countries and the US [19]. A recent meta-analysis found that providing nutritional support to non-critically ill medical inpatients reduced the risk of both mortality and hospital readmission by approximately 25% [20]. To what extent this also applies to severely ill patients with advanced tumor disease remains unclear; however, HPN is becoming increasingly important in this patient group. Given the increasing number of patients requiring home parenteral nutrition, it is important to understand what HPN means from the patient and physician perspective, the transition challenges, and how these patients should be best managed [1, 21].
The transition of adult cancer patients from PN in the hospital to HPN in the home care environment spanning the sectorial boundaries between hospital and ambulatory care can be challenging due to the complexities of arrangements required [22, 23]. The lack of expertise in establishing HPN for cancer patients was reported as one of the main barriers to effective service provision for these patients in a recent multi-centered European survey [18]. Our study exemplifies how the establishment of HPN for adult cancer patients is approached in Germany. In this real-world study, discharge management worked well with sufficient preparation. Nutritional status (bw and BMI), based on clinical and anthropometric parameters, remained stable or improved in some parameters, and HPN was generally perceived as positive from the patient perspective. The strongest burden to the patients was restricted mobility. Physicians rated the discharge management for most patients as good, but noted that it required a significant amount of time.
Training of the patient and their caregiver is a further essential aspect. It has been shown that many potential complications can be minimized or prevented by providing patients with a comprehensive educational curriculum on HPN [1]. This is supported by a study from the UK which examined the transition of adult HPN services between two specialized centers. The transition model used was successful, with most patients being 'very satisfied' with the transition management and their ongoing care. Effective communication with patients and between the two centers was key to success [24]. In our study, all patients and caregivers had a first conversation about the upcoming HPN a few days before discharge from the hospital, and a second conversation in more than three quarters of the cases.
Another important step prior to discharge from the hospital is to ensure that the patient has follow-up care arranged with a physician, who will also take responsibility for monitoring the patient's laboratory values and clinical status and adjusting the PN formula if necessary. This doctor must work closely with a pharmacist, a nutritionist, and a home care worker when the patient finally goes home [1]. For hospital doctors in Germany, we were able to show that they had difficulties in identifying and contacting the persons responsible for post-discharge and follow-up care in more than three quarters of the patients.
Although HPN can be a life-saving therapy, it may also be associated with serious complications. For example, infections of the central venous catheter are among the most common reasons for hospital readmission in HPN patients [1]. Awareness of these complications and close monitoring are essential to prevent and identify such problems. In our study, HPN catheter infection rates and hospital readmissions for catheter-related problems were low. A UK study showed similar results with low HPN-related complications and low HPN-related readmission rates [19].
While nutritional benefits are expected from HPN, there are concerns that the physical and social limitations caused by HPN could negatively impact the recipients' QoL [25]. Maintaining a good QoL is crucial in patients with cancer, and it is important to acknowledge that these patients may significantly derive benefit from HPN. Our results suggest that HPN is not necessarily too burdensome or troublesome to be offered to patients with a primary cancer diagnosis, and that HPN was not associated with a decline in QoL. The patients’ nutritional status (bw and BMI) could be maintained during HPN, and the patients felt that HPN had a low impact on their current QoL. These results are supported by another study from UK that investigated cancer patients' and family caregivers' experiences of HPN. From patients’ experiences burden of treatment did not mitigate the benefits of HPN. Motivation to live outweighed the constraints imposed. Patients and family caregivers recognized the treatment as a lifeline and were grateful for it [26]. Additional research confirms that both patients and caregivers perceived the benefits of HPN outweighing the reported negative aspects [27, 28].
In summary, our data emphasize that HPN is largely not perceived as an additional burden by cancer patients. The primary concern from the patients' perspective was restricted mobility. These findings are supported by several other studies that show patients can benefit from HPN through reduced anxiety and depression, as well as improved quality of life [7, 8, 11, 29].
Limitations
When interpreting the results of this real-world study involving severely ill patients in a palliative care setting, several limitations must be considered. A significant aspect is the large amount of missing data and the high dropout rates. The willingness of severely ill cancer patients to consistently complete the questionnaires likely decreased as the study progressed. Additionally, the rapidly increasing mortality rates in such a population further complicate data collection. Given the substantial amount of missing data, particularly after Visit 3 (Week 4), the results are therefore only partially interpretable.
Another factor is the challenge that, given the severity of the patients' illnesses, completing more complex and extensive questionnaires was not feasible. Therefore, very simple questions were chosen, some of which could only be answered with "Yes" or "No." This means that other important information may not have been captured, potentially leading to a bias in the results and further limiting the interpretability of the data. Additionally, we have no data on dosages, adjustments of PN, or reasons for discontinuing HPN during the observation period.
We also had no control over which patients were included in the study, which introduces a selection bias. Since participation by the study centers was voluntary, it is possible that only sites with known high-quality care participated. Moreover, we lack information on which patients declined to participate in the study and for what reasons. Originally, a significantly larger sample size of 700 patients was planned. However, the study period largely coincided with the COVID-19 pandemic, which greatly hindered recruitment.
Further limitations are the observational design and the lack of a control group. Observational studies cannot identify cause-effect relationships.
Our results may not provide a representative view of HPN from the perspective of oncology patients in a palliative care setting, nor of discharge management in Germany. Additionally, the organization of HPN management procedures may vary from country to country, so the results may not necessarily be generalizable to other countries.
Conclusions
With sufficient preparation for HPN, discharge management from the hospital and the home delivery of PN works well. HPN has been associated with few complications (e.g., low rate of catheter infections), the nutritional status (bw and BMI) was stabilized and the current QoL of the patients could be maintained. Overall, from the patient's point of view, HPN was perceived as little or no burden in addition to the underlying disease. It would be important to collect more data on this topic in larger patient groups and in different countries.
Data availability
No datasets were generated or analysed during the current study.
References
Bering J, DiBaise JK (2022) Home Parenteral and Enteral Nutrition. Nutrients 14(13):2558. https://doi.org/10.3390/nu14132558
Muscaritoli M, Arends J, Bachmann P et al (2021) ESPEN practical guideline: Clinical Nutrition in cancer. Clin Nutr 40(5):2898–2913. https://doi.org/10.1016/j.clnu.2021.02.005
Roeland EJ, Bohlke K, Baracos VE et al (2020) Management of Cancer Cachexia: ASCO Guideline. J Clin Oncol 38:2438–2453. https://doi.org/10.1200/JCO.20.00611
Bischoff SC, Arends J, Decker-Baumann C et al (2024) S3 Guideline Home Enteral and Home Parenteral Nutrition of the German Society for Clinical Nutrition and Metabolism (DGEM). Aktuel Ernahrungsmed 49:73–155. https://doi.org/10.1055/a-2270-7667
Sowerbutts AM, Lal S, Sremanakova J et al (2018) Home parenteral nutrition for people with inoperable malignant bowel obstruction. Cochrane Database Syst Rev 8(8):CD012812. https://doi.org/10.1002/14651858.cd012812.pub2
Bouleuc C, Anota A, Cornet C et al (2020) Impact on health-related quality of life of parenteral nutrition for patients with advanced cancer cachexia: results from a randomized controlled trial. Oncologist 25(5):e843–e851. https://academic.oup.com/oncolo/article/25/5/e843/6444368
Senesse P, Tadmouri A, Culine S et al (2015) A prospective observational study assessing home parenteral nutrition in patients with gastrointestinal cancer: benefits for quality of life. J Pain Symptom Manage 49(2):183-191.e2. https://doi.org/10.1016/j.jpainsymman.2014.05.016
Seys P, Tadmouri A, Senesse P et al (2014) Home parenteral nutrition in elderly patients with cancer: an observational prospective study. Bull Cancer 101(3):243–249. https://doi.org/10.1684/bdc.2014.1903
Vashi PG, Dahlk S, Popiel B et al (2014) A longitudinal study investigating quality of life and nutritional outcomes in advanced cancer patients receiving home parenteral nutrition. BMC Cancer 14:593. https://doi.org/10.1186/1471-2407-14-593
Tobberup R, Thoresen L, Falkme UG et al (2019) Effects of current parenteral nutrition treatment on health-related quality of life, physical function, nutritional status, survival and adverse events exclusively in patients with advanced cancer: A systematic literature review. Crit Rev Oncol Hematol 139:96–107. https://doi.org/10.1016/j.critrevonc.2019.04.014
Culine S, Chambrier C, Tadmouri A et al (2014) Home parenteral nutrition improves quality of life and nutritional status in patients with cancer: a French observational multicentre study. Support Care Cancer 22(7):1867–1874. https://doi.org/10.1007/s00520-014-2164-9
Pironi L, Boeykens K, Bozzetti F et al (2023) ESPEN practical guideline: Home parenteral nutrition. Clin Nutr 42(3):411–430. https://doi.org/10.1016/j.clnu.2022.12.003
Reber E, Strahm R, Bally L et al (2019) Efficacy and Efficiency of Nutritional Support Teams. J Clin Med 8(9):1281. https://doi.org/10.3390/jcm8091281
Cederholm T, Barazzoni R, Austin P et al (2017) ESPEN guidelines on definitions and terminology of clinical nutrition. Clin Nutr 36(1):49–64. https://doi.org/10.1016/j.clnu.2016.09.004
Cella DF, Tulsky DS, Gray G et al (1993) The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. Clin Oncol 11(3):570–579. https://doi.org/10.1200/jco.1993.11.3.570
Arends J, Bachmann P, Baracos V et al (2017) ESPEN guidelines on nutrition in cancer patients. Clin Nutr 36(1):11–48. https://doi.org/10.1016/j.clnu.2016.07.015
Ruggeri E, Giannantonio M, Agostini F et al (2020) Home artificial nutrition in palliative care cancer patients: Impact on survival and performance status. Clin Nutr 39(11):3346–3353. https://doi.org/10.1016/j.clnu.2020.02.021
Naghibi M, Skinner C, Burden ST, etal, (2022) A multi-national survey of experience and attitudes towards commencing home parenteral nutrition for patients with advanced cancer. Clin Nutr ESPEN 47:246–251. https://doi.org/10.1016/j.clnesp.2021.12.002
Kopczynska M, Teubner A, Abraham A et al (2022) Home Parenteral Nutrition in Patients with Advanced Cancer: Quality Outcomes from a Centralized Model of Care Delivery. Nutrients 14(16):3379. https://doi.org/10.3390/nu14163379
Gomes F, Baumgartner A, Bounoure L et al (2019) Association of Nutritional Support With Clinical Outcomes Among Medical Inpatients Who Are Malnourished or at Nutritional Risk: An Updated Systematic Review and Meta-analysis. JAMA Netw Open 2(11):e1915138. https://doi.org/10.1001/jamanetworkopen.2019.15138
Dreesen M, Foulon V, Hiele M et al (2013) Quality of care for cancer patients on home parenteral nutrition: development of key interventions and outcome indicators using a two-round Delphi approach. Support Care Cancer 21(5):1373–1381. https://doi.org/10.1007/s00520-012-1679-1
Sowerbutts AM, Lal S, Sremanakova J et al (2020) Discharging Women with Advanced Ovarian Cancer on Home Parenteral Nutrition: Making and Implementing the Decision. Nutrients 12(1):166. https://doi.org/10.3390/nu12010166
Baker J, Smith PJ, White SJ et al (2023) Availability of palliative parenteral nutrition to patients with advanced cancer: A national survey of service provision. J Hum Nutr Diet 6(4):1225–1233. https://doi.org/10.1111/jhn.13174
Fletcher J, Mumtaz S, Dera M et al (2019) Patient Experience in the Transition of Home Parenteral Nutrition Services Between Centers: Evaluation of a Transition Model. J Patient Exp 6(3):224–230. https://doi.org/10.1177/2374373518795423
Schönenberger KA, Reber E, Huwiler VV et al (2023) Quality of Life in the Management of Home Parenteral Nutrition. Ann Nutr Metab 79(3):326–333. https://doi.org/10.1159/000530082
Sowerbutts AM, Lal S, Sremanakova J et al (2019) Palliative home parenteral nutrition in patients with ovarian cancer and malignant bowel obstruction: experiences of women and family caregivers. BMC Palliat Care 18(1):120. https://doi.org/10.1186/s12904-019-0507-5
McCracken J, Wheelwright S, Hon Y, Shaw C (2023) Experience, decision-making and information needs around parenteral nutrition among people with advanced cancer, and their carers: A scoping review. J Hum Nutr Diet 36(2):453–467. https://doi.org/10.1111/jhn.13104
Schuetz P, Fehr R, Baechli V et al (2019) Individualised nutritional support in medical inpatients at nutritional risk: a randomised clinical trial. Lancet 393(10188):2312–2321. https://doi.org/10.1016/s0140-6736(18)32776-4
Pinto-Sanchez MI, Gadowsky S, McKenzie S et al (2019) Anxiety, Depression and Quality of Life Improve After One Month and Three Months of Home Parenteral Nutrition: A Pilot Study in a Canadian Population. J Can Assoc Gastroenterol 2(4):178–185. https://doi.org/10.1093/jcag/gwy045
Acknowledgements
This study was supported by Fresenius Kabi Deutschland GmbH, Bad Homburg, Germany. The authors thank the following participating investigators: Kersten Borchert and Heide Weiss, Städt. Klinikum Magdeburg, Magdeburg/Germany (current address KB: Ameos Klinik Aschersleben, Aschersleben, Germany). The Pharmalog Institut für klinische Forschung GmbH Ismaning, Germany was responsible for project management, monitoring and data management. Editorial support for the manuscript (in the form of writing assistance under the direction and guidance of the authors) was provided by Dr. Anja Luetke (medinform, Ratekau, Germany).
Funding
The study was funded by Fresenius Kabi Deutschland GmbH, Bad Homburg/Germany.
Author information
Authors and Affiliations
Contributions
A.S. and J.B. contributed to the study conception and design and together with A.G. to the analysis of the data. A.S. was the coordinating investigator according to § 40 German Drug Law. The first draft of the manuscript was written by A.S. and J.B.. The authors A.S., C.B., Y.Z., H.T., C.S., C.P., H.M., A.M., S.M., I.R., C.S., A.G. and E.J. contributed to the acquisition and collection of data. All authors read and commented previous versions and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Involved ethics committees (reference number) were: Ethikkommission der Medizinischen Hochschule Hannover (7730_BO_S_2018), Ethikkommission der Friedrich-Alexander-Universität Erlangen-Nürnberg (129_18 Bc), Ethik-Kommission der Landesärztekammer Baden-Württemberg (B-F-2018–031), Ethik-Kommission bei der Landesärztekammer Hessen (MC 266/2018), Ethikkommission der Universität zu Lübeck (18–307), Ethikkommission Ärztekammer Sachsen-Anhalt (68/18), Ethik-Kommission II Medizinische Fakultät Mannheim der Ruprecht-Karls-Universität Heidelberg (2018-644N-MA), Ethikkommission bei der Medizinischen Fakultät der LMU München (18–884), Ethik-Kommission der Universität Witten/Herdecke (199/2018).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Competing interests
Elke Jäger and Ingeborg Rötzer report personal fees from Clinic for Oncology and Haematology, Nordwest Hospital, UCT University Center, 60488 Frankfurt, during the conduct of the study. Christian Sina held an endowed professorship from 2016 to 2018. Justinus Beer is an employee of Fresenius Kabi Deutschland GmbH, Bad Homburg/Germany. All other authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Schneider, A., Baur, C., Zopf, Y. et al. Quality of care of oncological patients with home parenteral nutrition. Support Care Cancer 32, 834 (2024). https://doi.org/10.1007/s00520-024-09011-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00520-024-09011-2