Abstract
Purpose
To investigate the factors associated with live births and the interaction between age and the number of embryos transferred after in vitro fertilisation (IVF) treatment.
Methods
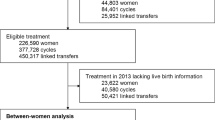
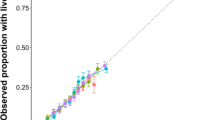
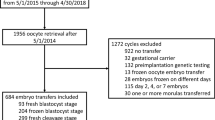
This study analyses data from a population-based-assisted reproductive database of all registered artificial reproduction institutions (n = 80) from 2010 to 2016 in Taiwan. The probability of a live birth in correlation with the treatment parameters was measured with multivariate logistic regression analyses using the generalised additive model (GAM) and Pearson’s chi-square exact test.
Results
A total of 104,015 IVF treatments performed between 2010 and 2016 were included in our analysis. From these treatments, 31,467 (30.3%) were successfully delivered, and 40,565 test-tube babies were born. Pearson’s chi-square exact test indicated that parents’ age, cause of infertility, type of ovarian stimulation, additional assisted reproductive technology techniques, donated egg or sperm, fresh or frozen embryo, presence or absence of ovarian hyperstimulation syndrome, and day of embryo transfer were significantly associated with live births after an IVF cycle (p < 0.05). Multiple logistic regression analysis with the GAM revealed that the odds of a live birth with IVF treatment in patients < 34 years of age were 2.55 times higher than that in patients ≥ 45 years of age (odds ratio = 2.55, 95% confidence interval = 1.69–2.90) for patients who underwent a single-embryo transfer (SET); a similar pattern was observed when two or more embryos were transferred. Egg donation, the assisted hatching technique, oral ovarian stimulation agents, and implantation of frozen embryos during SET were shown to improve the chance of a live birth by 29–90%. Implantation of the embryo after the 5th day of culture yielded the highest odds of a live birth. The interaction plot revealed that maternal age, especially < 40 years, was associated with the probability of a live birth. SET and double-embryo transfer showed similar associations with the probability of a live birth across age groups. Transferring more than two embryos might reduce the probability of a live birth during IVF treatment for women ≥ 40 years of age.
Conclusions
Implanting a greater number of embryos did not improve the age-related decrease in fertility for patients undergoing IVF. Therefore, we suggested that ≤ 2 blastocysts could be transferred during IVF treatments for women ≥ 40 years. Transferring a blastocyst on day 5 of culture was associated with a significant increase in the odds of a live birth resulting from IVF.



Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Data availability
All data are available upon request; however, the raw data is unavailable.
References
Vander Borght M, Wyns C. Fertility and infertility: definition and epidemiology. Clin Biochem. 2018;62:2–10.
Gurunath S, Pandian Z, Anderson RA, Bhattacharya S. Defining infertility-a systematic review of prevalence studies. Hum Reprod Update. 2011;17(5):575–88.
Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 2012;9(12):e1001356.
Shi Y, Sun Y, Hao C, Zhang H, Wei D, Zhang Y, et al. Transfer of fresh versus frozen embryos in ovulatory women. N Engl J Med. 2018;378(2):126–36.
Penzias A, Bendikson K, Butts S, Coutifaris C, Fossum G, Falcone T, et al. Guidance on the limits to the number of embryos to transfer: a committee opinion. Fertil Steril. 2017;107(4):901–3.
Vaegter KK, Lakic TG, Olovsson M, Berglund L, Brodin T, Holte J. Which factors are most predictive for live birth after in vitro fertilization and intracytoplasmic sperm injection (IVF/ICSI) treatments? Analysis of 100 prospectively recorded variables in 8,400 IVF/ICSI single-embryo transfers. Fertil Steril. 2017;107(3):641–8.
Dyer S, Chambers GM, de Mouzon J, Nygren KG, Zegers-Hochschild F, Mansour R, et al. International Committee for Monitoring Assisted Reproductive Technologies world report: assisted reproductive technology 2008, 2009 and 2010. Hum Reprod. 2016;31(7):1588–609.
Schieve LA, Meikle SF, Ferre C, Peterson HB, Jeng G, Wilcox LS. Low and very low birth weight in infants conceived with use of assisted reproductive technology. N Engl J Med. 2002;346(10):731–7.
Allen BD, Adashi EY, Jones HW. On the cost and prevention of iatrogenic multiple pregnancies. Reprod BioMed Online. 2014;29(3):281–5.
Keith L, Oleszczuk JJ. Iatrogenic multiple birth, multiple pregnancy and assisted reproductive technologies. Int J Gynecol Obstet. 1999;64(1):11–25.
Nyirati I, Orvos H, Bártfai G, Kovács L. Iatrogenic multiple pregnancy - Higher risk than a spontaneous one? J Reprod Med. 1997;42(11):695–8.
Verberg MFG, Macklon NS, Heijnen EMEW, Fauser BCJM. ART: iatrogenic multiple pregnancy? Best Pract Res Clin Obstet Gynaecol. 2007;21(1):129–43.
Reynolds MA, Schieve LA. Trends in embryo transfer practices and multiple gestation for IVF procedures in the USA, 1996-2002. Hum Reprod. 2006;21(3):694–700.
Wright VC, Schieve LA, Reynolds MA, Jeng G. Assisted reproductive technology surveillance--United States, 2002. MMWR Surveill Summ. 2005;54(2):1–24.
Pandian Z, Marjoribanks J, Ozturk O, Serour G, Bhattacharya S. Number of embryos for transfer following in vitro fertilisation or intra-cytoplasmic sperm injection: summary of a Cochrane review. Fertil Steril. 2014;102(2):345–7.
Fujimoto A, Morishima K, Harada M, Hirata T, Osuga Y, Fujii T. Elective single-embryo transfer improves cumulative pregnancy outcome in young patients but not in women of advanced reproductive age. J Assist Reprod Genet. 2015;32(12):1773–9.
Maheshwari A, Raja EA, Bhattacharya S. Obstetric and perinatal outcomes after either fresh or thawed frozen embryo transfer: an analysis of 112,432 singleton pregnancies recorded in the Human Fertilisation and Embryology Authority anonymized dataset. Fertil Steril. 2016;106(7):1703–8.
Maheshwari A, Pandey S, Amalraj Raja E, Shetty A, Hamilton M, Bhattacharya S. Is frozen embryo transfer better for mothers and babies? Can cumulative meta-analysis provide a definitive answer? Hum Reprod Update. 2018;24(1):35–58.
Rhenman A, Berglund L, Brodin T, Olovsson M, Milton K, Hadziosmanovic N, et al. Which set of embryo variables is most predictive for live birth? A prospective study in 6252 single embryo transfers to construct an embryo score for the ranking and selection of embryos. Hum Reprod. 2015;30(1):28–36.
Malizia BA, Hacker MR, Penzias SA. Cumulative live-birth rates after in vitro fertilization. N Engl J Med. 2009;360(3):236–43.
Fedorcsák P, Storeng R, Dale PO, Tanbo TOM, Åbyholm T. Obesity is a risk factor for early pregnancy loss after IVF or ICSI. Acta Obstet Gynecol Scand. 2000;79(1):43–8.
Kasius A, Smit JG, Torrance HL, Eijkemans MJ, Mol BW, Opmeer BC, et al. Endometrial thickness and pregnancy rates after IVF: a systematic review and meta-analysis. Hum Reprod Update. 2014;20(4):530–41.
Richter KS, Bugge KR, Bromer JG, Levy MJ. Relationship between endometrial thickness and embryo implantation, based on 1,294 cycles of in vitro fertilization with transfer of two blastocyst-stage embryos. Fertil Steril. 2007;87(1):53–9.
Steward RG, Lan L, Shah AA, Yeh JS, Price TM, Goldfarb JM, et al. Oocyte number as a predictor for ovarian hyperstimulation syndrome and live birth: an analysis of 256,381 in vitro fertilization cycles. Fertil Steril. 2014;101(4):967–73.
Tannus S, Cohen Y, Henderson S, Son WY, Tulandi T. The effect of assisted hatching on live birth rate following fresh embryo transfer in advanced maternal age. Reprod Sci. 2019;26(6):806–11.
Li Z, Wang AY, Bowman M, Hammarberg K, Farquhar C, Johnson L, et al. ICSI does not increase the cumulative live birth rate in non-male factor infertility. Hum Reprod. 2018;33(7):1322–30.
Health Promotion Administration, Ministry of Health and Welfare. 2013 National Report of the Assisted Reproductive Technology Summary in Taiwan. 2015. https://www.hpa.gov.tw/EngPages/Detail.aspx?nodeid=1063&pid=6083.
Cai J, Liu L, Jiang X, Li P, Sha A, Ren J. Low body mass index is associated with ectopic pregnancy following assisted reproductive techniques: a retrospective study. BJOG : an international journal of obstetrics and gynaecology. 2020. https://doi.org/10.1111/1471-0528.16378.
Venables WN, Dichmont CM. GLMs, GAMs and GLMMs: an overview of theory for applications in fisheries research. Fish Res. 2004;70(2-3):319–37.
Wang S, Zhang Y, Mensah V, Huber WJ, Huang YT, Alvero R. Discordant anti-müllerian hormone (AMH) and follicle stimulating hormone (FSH) among women undergoing in vitro fertilization (IVF): which one is the better predictor for live birth? J Ovarian Res. 2018;11(1):60.
Debón A, Molina I, Cabrera S, Pellicer A. Mathematical methodology to obtain and compare different embryo scores. Math Comput Model. 2013;57(5-6):1380–94.
Van Loendersloot LL, Van Wely M, Repping S, Bossuyt PMM, Van Der Veen F. Individualized decision-making in IVF: calculating the chances of pregnancy. Hum Reprod. 2013;28(11):2972–80.
Choi B, Bosch E, Lannon BM, Leveille MC, Wong WH, Leader A, et al. Personalized prediction of first-cycle in vitro fertilization success. Fertil Steril. 2013;99(7):1905–11.
Gleicher N, Orvieto R. Is the hypothesis of preimplantation genetic screening (PGS) still supportable? A review. J Ovarian Res. 2017;10(1):21.
Verlinsky Y, Kuliev A. Preimplantation diagnosis of common aneuploidies in infertile couples of advanced maternal age. Hum Reprod. 1996;11(10):2076–7.
Maxwell SM, Melzer-Ross K, McCulloh DH, Grifo JAA. Comparison of pregnancy outcomes between day 3 and day 5/6 embryo transfers: does day of embryo transfer really make a difference? J Assist Reprod Genet. 2015;32(2):249–54.
Margreiter M, Weghofer A, Kogosowski A, Mahmoud KZ, Feichtinger WA. Prospective randomized multicenter study to evaluate the best day for embryo transfer: does the outcome justify prolonged embryo culture? J Assist Reprod Genet. 2003;20(2):91–4.
Skorupski JC, Stein DE, Acholonu U, Field H, Keltz M. Successful pregnancy rates achieved with day 4 embryo transfers. Fertil Steril. 2007;87(4):788–91.
Pantos K, Makrakis E, Chronopoulou M, Biba M, Perdikaris A. &and Dafereras A. Day 4 versus day 3 embryo transfer: a prospective study of clinical outcomes. Fertil Steril. 2008;89(3):573–7.
Simopoulou M, Sfakianoudis K, Tsioulou P, Rapani A, Maziotis E, Giannelou P, et al. Should the flexibility enabled by performing a day-4 embryo transfer remain as a valid option in the IVF laboratory? A systematic review and network meta-analysis. J Assist Reprod Genet. 2019;36:1049–61.
Acknowledgements
We thank the Health and Welfare Data Science Centre, Ministry of Health and Welfare for permitting the use of the Taiwan ARD for this analysis. We appreciate the Elsevier Language Service that helped us edit and improve our language quality.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 93 kb).
Rights and permissions
About this article
Cite this article
Yu, HC., Rei, WM., Chiou, ST. et al. Multivariate analysis of the factors associated with live births during in vitro fertilisation in Southeast Asia: a cross-sectional study of 104,015 in vitro fertilisation records in Taiwan. J Assist Reprod Genet 38, 2415–2423 (2021). https://doi.org/10.1007/s10815-021-02086-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-021-02086-4