Abstract
Purpose
Patients with inborn errors of immunity (IEI) have lifelong health complications including severe infections and physical impairments. Previous studies show that a patient’s perception of their health is an important predictor of health outcomes. The purpose of this study was to understand factors related to patient reported health status.
Methods
We used data from the Immune Deficiency Foundation (IDF) 2017 National Patient Survey and analyzed factors which correlated with the reported health status (RHS). Among a cohort of 1139 self-reported IEI patients, we identified age at the time of diagnosis, time gap between symptom onset and diagnosis, number of physicians seen, and whether the diagnosis was made in the first 5 years of life as significant. We used a two-tailed t-test, single-factor ANOVA, and Tukey-Kramer post-hoc test to assess statistical significance in the observed difference.
Results
Patients who received a diagnosis before the age of 12 had a significantly better mean RHS (n = 207 pre-12a vs. n = 900 post-12a; p < 0.0001). Patients who received a diagnosis within 10 years of symptom onset showed improved mean RHS (n = 413 pre-10 vs. n = 524 post-10; p < 0.0001). Among patients who had symptom onset within the first 5 years of life, those who received a diagnosis had a significantly improved RHS (3.5 ± 0.92, n = 275 undiagnosed vs. 2.8 ± 0.94, n = 108 diagnosed; p < 0.0001). Finally, RHS was significantly impacted by number of physicians(n ≥ 4) seen prior to diagnosis (3.1 ± 0.96 vs. 3.4 ± 0.80, p < 0.0001).
Conclusion
These findings shed light upon critical factors which impact IEI patient RHS. Specifically, we find that efficient, rapid and early-life IEI identification should improve patient reported health and relevant outcomes. These improvements appear to be independent of the clinician specialty ultimately making the IEI diagnosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Avoid common mistakes on your manuscript.
Introduction
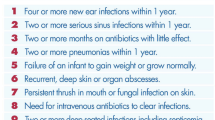
Inborn errors of immunity (IEI) are a group of chronic conditions characterized by a single gene mutation leading to a defective immune system of the affected individuals [1]. Although individually rare, as a group, IEI affects approximately 200,000 people across the United States [2]. Patients suffer from an extensive list of health conditions including an increased susceptibility to infections, autoimmune diseases, and malignancies [1]. However, each patient’s journey is unique, and surveys have shown a wide variance in how patients perceive their overall health [3]. Looking at perceived health allows us to analyze the importance of different variables and their distinct impact on health outcomes for IEI patients.
Perceived health (PH) is a subjective measure of individuals’ overall wellbeing and studies have shown it to be a reliable indicator of many objective health outcomes including morbidity and mortality [4]. Similarly, it has been observed that patients’ in better health have reported a higher satisfaction with their health status [4, 5]. Many factors have been shown to affect PH including education level, hospitalization, and access to specialist care [3]. When caring for patients with chronic conditions such as IEI, understanding all that affects their physical, mental, and overall health status allows providers to deliver a more personalized and more effective care to their patients.
Patients can communicate their PH through regular health surveys, which is common practice among Organization for Economic Co-operation and Development (OECD) countries. A standard question for assessing PH is “How is your health in general?” and patients can choose between Excellent, Very Good, Good, Fair, or Poor. This subjective reported health status (RHS) is correlated with healthcare utilization and mortality. Several studies have explored the relationship between RHS and variables such as socioeconomic, psychosocial, behavioral factors [6,7,8].
In this study we aimed to explore other factors that potentially affect the RHS of patients with IEI. These factors include age at the time of diagnosis, time gap between symptom onset and receiving a diagnosis (i.e. “diagnostic gap”), having a diagnosis in the first 5 years of life, the number of physicians seen, and the type of specialist that provided the diagnosis. A priori, these factors are expected contributors to impaired RHS; however, the degree of impact has not been evaluated. Previous studies on RHS in patients with IEI showed that earlier detection is vital and leads to less morbidity. These studies also stressed the importance of “vigilant care” which prevents further complications and serious healthcare interactions in the future [9]. Knowing important variables and understanding how they impact patients with IEI is vital for both quality patient care and health outcomes. Many studies reinforce this importance for patients with IEI [9,10,11].
Methods
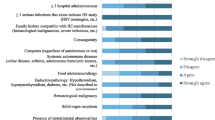
Data for this study was collected from the Immune Deficiency Foundation (IDF) 2017 National Patient Survey Data Dictionary. The survey coded the health status (RHS) of the patients on a 5-point scale, 1 for excellent health and 5 for poor health. We conducted analyses which addressed hypotheses related to patient age at diagnosis, diagnostic gap, impact of serious infections at the time of diagnosis and diagnostic odyssey burden impact upon patient reported RHS.
Age-Based Cohort Comparisons
We stratified the patients based on their age at the time of diagnosis into 6 groups: 0–12, 13–30, 31–45, 46–55, 56–65, > 65 years of age. Age groups were selected to ensure a similar number of subjects in each group. The mean RHS of the groups were compared using a single factor ANOVA. Pairwise group comparison was then conducted via a Tukey-Kramer post-hoc test to identify group by group differences.
Calculating the Diagnostic Delay Timespan(“Diagnostic Gap”)
To determine the diagnostic gap, we indexed age of first serious infection (indicator of symptom onset), age of IEI diagnosis and calculated the difference. We then split the patients into 5 diagnostic gap groups: <1, 1–10, 11–25, 26–40, and > 40 years elapsed. Mean RHS of the groups were compared using a single factor ANOVA. Pairwise group comparisons were then conducted via a Tukey-Kramer post-hoc test to identify group by group differences.
Quantifying the Diagnostic Odyssey Burden
We first assessed burden by impact of serious infection and lack of diagnosis. For this analysis, the patients were stratified by age of serious infection first reported at 5-year intervals, from 0 to 90. The proportion of subjects in each age bracket with serious infections were then calculated and the temporal association between health status measurement and timing of their IEI diagnosis was determined. From this, we focused our analysis on the 0–5-year age group, which had the largest number of patients experiencing serious infections (n = 383). However, within that group of 383 patients experiencing serious infections there were only 108 who had received a diagnosis. We then compared the group mean RHS of patients who experienced serious infections within that range (0–5 yrs) with a diagnosis (“Dx”; n = 108) to those without (“UDx”; n = 275).
Next, we evaluated burden by the number of physicians seen. As a group(n = 1145), the mean number of physicians seen per patient was calculated (n = 3) and the patients were divided into groups who had seen \(\:\le\:\:\)3 physicians and those who were seen by 4 or more physicians. A Student’s t-test was then used to compare mean RHS of patients across the two groups.
Results
Demographics of patients studied in this cohort is described in Table 1. Out of 1145 patients and parent proxies, 1139 reported their health status:38 patients reported excellent health (3%), 196 reported very good health (17%), 435 reported good health (38%), 372 reported their health as fair (33%), and 98 reported poor health (9%). The average RHS of the population was 3.259 ± 0.953.
Age-Based Cohort Comparisons
A total of 1107 patients reported age at diagnosis and were included in this analysis. The primary analysis (e.g. ANOVA) showed a significant difference between mean RHS across all age groups (p < 0.0001). Pairwise post testing revealed that significance stemmed from the 0–12 group which had a significantly better RHS compared to other groups individually (Table 2).
Calculating the Diagnostic Delay Timespan(“Diagnostic Gap”)
Of the 1107 patients who met the criteria for the first analysis, 937 reported the age of symptom onset and were studied in this analysis. There was a significant difference between the RHS across all groups (p < 0.0001). Group pairwise comparison demonstrated significant RHS differences between patients with a diagnostic gap \(\:\le\:10\) years (i.e. groups <1 and 1–10 yrs) compared to those with the longest diagnostic gap (i.e.>40 years elapsed) (Table 3).
Quantifying the Diagnostic Odyssey Burden
Of 383 patients who experienced serious infections in the 0–5 age range, 108 (28%) had received an IEI diagnosis while 275 (72%) had not. Between these two groups, we found a significant difference in reported health scores when comparing diagnosed (Dx) and undiagnosed (UDx) patients (Table 4). Here, we note that the 0–5 year-olds with serious infections having received a diagnosis had a significantly better RHS score than those who went undiagnosed.
Among the entire cohort (n = 1145) the mean and median number of physicians seen was 3(mean: 3±2.4; range: 0–11). Mean RHS among those who saw 3 (n = 617) or fewer physicians vs. those that saw 4 (n = 521) or more was significant (3.1 ± 0.96 vs. 3.4 ± 0.80, p < 0.0001). Here, RHS scores were improved among those seeing fewer physicians.
Discussion
This analysis used data derived from a nationally distributed mail/postal survey conducted by the IDF which captures a variety of first-person perspectives from IEI patients about their own health [12]. These surveys inquire about many different aspects of patients’ lives including their quality of life and how they perceive their general health. In our study, RHS was determined based on an answer to the question “ In general, how would you say the patient’s current health is?”. This question has been described as a reliable measure of health status as it pertains to both the objective wellbeing and subjective perceived health [12, 13]. Studies have shown a relationship between RHS and patient outcome and morbidity, supporting that a better RHS is indicative of better health [13, 14]. In this study we analyze and demonstrate, for the first time, the relationship between RHS and factors associated with a patients’ journey to receiving a diagnosis.
From our analysis, we wish to emphasize several key findings, First, time to diagnosis matters for IEI patients. Our analysis reveals that having a diagnosis sooner, and at a younger age led to better RHS scores further emphasizing a need for optimizing early IEI detection(Table 2). Even a diagnostic gap of ten years or less had significantly improved RHS compared to those diagnosed over longer intervals of time(Table 3). While a diagnostic gap of 10 years is still an interminable amount of time, we note the quantitative impacts of longer durations upon RHS here. In terms of age at diagnosis, patients with the lowest (i.e. better) RHS came from the youngest age bracket (Table 2; age 0-12yrs). Additionally, many patients in this cohort started experiencing infections at a young age which probably improved their likelihood of receiving an IEI diagnosis. However, within the 0–5 age group(n = 383), less than a third (n = 108; 28%) received an IEI diagnosis(Table 4). Among those, we found a significantly better RHS compared to those in the same age group without a diagnosis. These findings suggest that receiving a diagnosis at an earlier age and through a shorter diagnostic gap is associated with lower (i.e. better) RHS scores. Quantitatively, this analysis further underscores the association between worse RHS and suboptimal patient health outcomes such as being older at diagnosis, having greater comorbidities and taking more time to receive a diagnosis [5, 13].
Finally, patients in the IDF data set saw up to 11 different specialists throughout their diagnostic odyssey. Our analysis found that seeing fewer physicians correlated with an improved RHS score. Unsurprisingly, these findings suggest that reported health diminishes, and burden increases, as patients see more and more healthcare providers along their diagnostic journey. While economic factors were not assessed here, we also expect that worse RHS and higher health expenditures would go hand in hand, further diminishing the value of care. Interestingly, we did not note a significant difference in RHS scores between those diagnosed by an immunologist compared to other physician specialties. These findings suggest that the burden came from the number of physicians seen and not necessarily any one specialty. Thus, it may not matter who makes the diagnosis so long as one is precisely made at the earliest age, with less time in the healthcare system. This notion supports efforts to build awareness across any specialty, including primary care, for improving IEI patient reported health.
From our analysis, we find that each IEI patient has a unique diagnostic journey encompassing numerous factors such as lingering infections, seeing many specialists, and suffering extended periods of time without a diagnosis. Do these factors contribute to their overall health outcome? This study suggests that RHS scores are indeed influenced by discrete features of the clinical journey. Understanding these, and other, precise factors affecting health outcomes for patients with IEI could enable efforts to address drivers of impaired RHS. Systematically, decreasing the time to treatment, reducing the number of physicians seen prior to diagnosis, and identifying IEI earlier in life are all valuable for patients. Thus, efforts aimed at mitigating these drivers of burden are expected to improve RHS and lead to better health outcomes for patients.
While we believe that our findings quantitatively bolster previously held notions about diagnostic burden, we acknowledge some limitations of this study. First, our sample may not be representative of the general population given this largely white, female cohort suffering predominantly antibody deficiency syndromes (Table 1). Second, the IDF phone survey lends itself towards selection bias, recall bias, and other forms of response bias. Additionally, we chose parametric statistical tests to analyze ordinal Likert scores because of the size and largely normal distributions within our datasets. For these reasons, our results should be interpreted as exploratory rather than confirmatory. Finally, the 2017 survey was conducted before the COVID-19 pandemic; thus, impacts of a global pandemic could drastically change burden and result in different responses not captured in this analysis.
Ultimately, we believe that findings described here show a significant need for comprehensively educating generalists and subspecialists alike to expedite IEI patient diagnosis early in life and prior to onset of morbidity. Strategies like newborn screening and computational screening (e.g. artificial intelligence based methods) in addition to focused educational initiatives, are expected to impact this goal and improve RHS concomitantly with improved outcomes [15,16,17].
Data Availability
This is an observational study. Data from the IDF are available upon request.
Change history
06 January 2025
The original online version of this article was revised: The organization “Immune Deficiency Foundation (IDF)” was misnamed.
29 January 2025
A Correction to this paper has been published: https://doi.org/10.1007/s10875-025-01859-1
References
Seeborg FO, Seay R, Boyle M, et al. Perceived Health in patients with primary Immune Deficiency. J Clin Immunol. 2015. https://doi.org/10.1007/s10875-015-0196-7
Rider NL, Truxton A, Ohrt T, Margolin-Katz I, Horan M, Shin H, Davila R, Tenembaum V, Quinn J, Modell V, Modell F, Orange JS, Branner A, Senerchia C. Validating inborn error of immunity prevalence and risk with nationally representative electronic health record data. J Allergy Clin Immunol. 2024;153(6):1704–10. https://doi.org/10.1016/j.jaci.2024.01.011
Mutz J, Lewis CM. Cross-classification between self-rated health and health status: longitudinal analyses of all-cause mortality and leading causes of death tin the UK. Sci Rep. 2022. https://doi.org/10.1038/s41598-021-04016-x
Bayrhuber M, Tinsel I, Goldacker S, Kindle G, Warnatz K, Farin E, Nieters A. Perceived health of patients with common variable immunodeficiency–a cluster analysis. Clin Experimental Immunol. 2019;196(1):76–85.
Selina K, Berg CB, Thorup B, Borregaard AV, Christensen L, Thrysoee, Trine B, Rasmussen O, Ekholm K, Juel M, Vamosi. Patient-reported outcomes are independent predictors of one-year mortality and cardiac events across cardiac diagnoses: findings from the national DenHeart survey. Eur J Prev Cardiol. 2019. https://doi.org/10.1177/2047487318769766
Axon DR, Jang A, Son L, Pham T. Determining the association of perceived health status among United States older adults with self-reported pain. Aging Health Res. 2022. https://doi.org/10.1016/j.ahr.2021.100051
Palladino R, Lee T, Ashworth J, Triassi M, M., Millett C. Associations between multimorbidity, healthcare utilisation and health status: evidence from 16 European countries. Age Ageing. 2016. https://doi.org/10.1093/ageing/afw044
OECD. Perceived health status, in Health at a Glance 2017: OECD Indicators. 2017: https://doi.org/10.1787/health_glance-2017-13-en
Altman K, Zhou C, Hernandez-Trujillo V, et al. Health-Related Quality of Life in 91 patients with X-Linked agammaglobulinemia. J Clin Immunol. 2022. https://doi.org/10.1007/s10875-022-01222-8
Nicholson B, Goodman R, Day J, et al. Quality of Life and Social and Psychological outcomes in Adulthood following allogeneic HSCT in Childhood for Inborn errors of immunity. J Clin Immunol. 2022. https://doi.org/10.1007/s10875-022-01286-6
Zhang S, Kline M, Fuleihan RL, et al. PROMIS-29 survey confirms major impact of fatigue on health-related quality of life in common variable immunodeficiency. Immunol Res. 2020. https://doi.org/10.1007/s12026-020-09162-4
Immune Deficiency Foundation. (2024). URL:https://primaryimmune.org/.
Hunt SM, McKenna SP, McEwen J, Backett EM, Williams J, Papp E. A quantitative approach to perceived health status: a validation study. J Epidemiol Community Health. 1980. https://doi.org/10.1136/jech.34.4.281
Reinwarth AC, Wicke FS, Hettich N, Ernst M, Otten D, Brähler E, Wild PS, Münzel T, König J, Lackner KJ, Pfeiffer N, Beutel ME. Self-rated physical health predicts mortality in aging persons beyond objective health risks. Sci Rep. 2023;13:19531. https://doi.org/10.1038/s41598-023-46882-7
Kubala SA, Sandhu A, Palacios-Kibler T, Ward B, Harmon G, DeFelice M, et al. Natural history of infants with non-SCID T cell lymphopenia identified on newborn screen. Clin Immunol. 2022 Dec;245:109182. https://doi.org/10.1016/j.clim.2022.109182
Rider NL, Coffey M, Kurian A, Quinn J, Orange JS, Modell V, Modell F. A validated artificial intelligence-based pipeline for population-wide primary immunodeficiency screening. J Allg Clin Immunol. 2023;151(1):272–9. https://doi.org/10.1016/j.jaci.2002.10.005
Eldeniz FC, Gul Y, Yorulmaz A, Guner SN, Keles S, Reisli I. Evaluation of the 10 warning signs in primary and secondary immunodeficient patients. Front Immunol. 2022 May;13:900055. https://doi.org/10.3389/fimmu.2022.900055
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection was provided by Chrisopher Scalchunes at the Immune Deficiency Foundation and analyses were performed by Sarina Nikzad, Rebekah Johnson, and Nicholas Rider. The first draft of the manuscript was written by Sarina Nikzad and Rebekah Johnson. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nikzad, S., Johnson, R., Scalchunes, C. et al. Quantifying the Diagnostic Odyssey Burden Among Persons with Inborn Errors of Immunity. J Clin Immunol 45, 61 (2025). https://doi.org/10.1007/s10875-024-01855-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10875-024-01855-x