Abstract
Objective
Constrictive pericarditis (CP) is a rare disease, and the diagnosis and surgical treatment of CP remain challenging. The aim of this study was to evaluate our Japanese single-center experience with isolated pericardiectomy for CP to elucidate the factors associated with improved outcomes.
Methods
Over a 20-year period, 44 consecutive patients underwent isolated pericardiectomy at our institution. The cause of CP was: idiopathic (59%), postsurgical (32%), tuberculosis (7%), and postradiation (2%) of the patients. All patients were diagnosed with CP using multiple modalities, including echocardiography, cardiac catheterization, computed tomography, or magnetic resonance imaging (MRI). Median sternotomy was performed in 42 (95%) patients. Twenty-eight (68%) patients underwent radical pericardiectomy.
Results
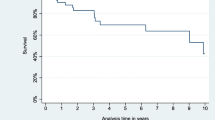
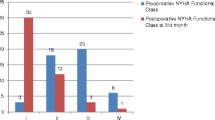
The postoperative diagnosis in all patients was CP. Among the multiple modalities, cardiac MRI had the greatest diagnostic sensitivity (97.2%). There were no operative or hospital deaths; late mortality occurred in seven (15.9%) patients in the series. Multivariable analysis showed that preoperative low LVEF was a risk factor for long-term mortality. Seven patients were readmitted for heart failure postoperatively. Multivariable analysis showed incomplete pericardiectomy and use of a preoperative inotrope were risk factors for readmission for heart failure.
Conclusions
The diagnosis using multimodality imaging for CP was effective in our institution and tagged cine MRI had the greatest sensitivity in diagnosing CP. Preoperative condition, including preoperative low LVEF or inotrope use, was correlated with long-term outcome after pericardiectomy. Pericardiectomy should be performed early and as radically as possible to prevent recurrent heart failure.


Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Myers RB, Spodick DH. Constrictive pericarditis: clinical and pathophysiologic characteristics. Am Heart J. 1999;138(2 Pt 1):219–32.
Syed FF, Schaff HV, Oh JK. Constrictive pericarditis—a curable diastolic heart failure. Nat Rev Cardiol. 2014;11:530–44.
Nataf P, Cacoub P, Dorent R, Jault F, Bors V, Pavie A, et al. Results of subtotal pericardiectomy for constrictive pericarditis. Eur J Cardiothorac Surg. 1993;7:252–6.
Kojima S, Yamada N, Goto Y. Diagnosis of constrictive pericarditis by tagged cine magnetic resonance imaging. N Engl J Med. 1999;341:373–4.
Power JA, Thompson DV, Rayarao G, Doyle M, Biederman RWW. Cardiac magnetic resonance radiofrequency tissue tagging for diagnosis of constrictive pericarditis: A proof of concept study. J Thorac Cardiovasc Surg. 2016;151:1348–55.
Amaki M, Savino J, Ain DL, Sanz J, Pedrizzetti GP, Kulkarni H, Narula J, Sengupta PP. Diagnostic Concordance of Echocardiography and Cardiac Magnetic Resonance–Based Tissue Tracking for Differentiating Constrictive Pericarditis From Restrictive Cardiomyopathy. Circulation: Cardiovascular Imag 2014; 7: 819–27.
McCaughan BC, Schaff HV, Piehler JM, Danielson GK, Orszulak TA, Puga FJ, et al. Early and late results of pericardiectomy for constrictive pericarditis. J Thorac Cardiovasc Surg. 1985;89:340–50.
Cameron J, Oesterle SN, Baldwin JC, Hancock EW. The etiologic spectrum of constrictive pericarditis. Am Heart J. 1987;113(2 Pt 1):354–60.
DeValeria PA, Baumgartner WA, Casale AS, Greene PS, Cameron DE, Gardner TJ, et al. Current indications, risks, and outcome after pericardiectomy. Ann Thorac Surg. 1991;52:219–24.
Bertog SC, Thambidorai SK, Parakh K, Schoenhagen P, Ozduran V, Houghtaling PL, et al. Constrictive pericarditis: etiology and cause-specific survival after pericardiectomy. J Am Coll Cardiol. 2004;43:1445–52.
Arsan S, Mercan S, Sarigül A, Atasoy S, Demircin M, Dogan R, et al. Long-term experience with pericardiectomy: analysis of 105 consecutive patients. Thorac Cardiovasc Surg. 1994;42:340–4.
Chowdhury UK, Subramaniam GK, Kumar AS, Airan B, Singh R, Talwar S, et al. Pericardiectomy for constrictive pericarditis: a clinical, echocardiographic, and hemodynamic evaluation of two surgical techniques. Ann Thorac Surg. 2006;81:522–9.
Bozbuga N, Erentug V, Eren E, Erdogan HB, Kirali K, Antal A, et al. Pericardiectomy for chronic constrictive tuberculous pericarditis: risks and predictors of survival. Tex Heart Inst J. 2003;30:180–5.
Cho YH, Schaff HV. Surgery for pericardial disease. Heart Fail Rev. 2013;18:375–87.
Szabo G, Schmack B, Bulut C, Soós P, Weymann A, Stadtfeld S, et al. Constrictive pericarditis: risks, aetiologies and outcomes after total pericardiectomy: 24 years of experience. Eur J Cardiothorac Surg. 2013;44:1023–8.
Tokuda Y, Miyata H, Motomura N, Araki Y, Oshima H, Usui A, et al. Outcome of pericardiectomy for constrictive pericarditis in Japan: a nationwide outcome study. Ann Thorac Surg. 2013;96:571–6.
Ling LH, Oh JK, Schaff HV, Danielson GK, Mahoney DW, Seward JB, et al. Constrictive Pericarditis in the Modern Ara: Evolving Clinical Spectrum and Impact on Outcome After Pericardiectomy. Circulation. 1999;100:1380–6.
Vistarini N, Chen C, Mazine A, Bouchard D, Hebert Y, Carrier M, et al. Pericardiectomy for constrictive pericarditis: 20 years of experience at the Montreal Heart Institute. Ann Thorac Surg. 2015;100:107–13.
Komoda T, Frumkin A, Knosalla C, Hetzer R. Child-Pugh score predicts survival after radical pericardiectomy for constrictive pericarditis. Ann Thorac Surg. 2013;96:1679–85.
Avgerinos D, Rabitnokov Y, Worku B, Neragi-Miandoab S, Girardi LN. Fifteen-year experience and outcomes of pericardiectomy for constrictive pericarditis. J Card Surg. 2014;29:434–8.
Góngora E, Dearani JA, Orszulak TA, Schaff HV, Li Z, Sundt TM 3rd. Tricuspid regurgitation in patients undergoing pericardiectomy for constrictive pericarditis. Ann Thorac Surg. 2008;85:163–71.
Kuroda H, Sakaguchi M, Takano T, Tsunemoto H, Shinohara M, Fukaya Y, et al. Intraoperative monitoring of pressure-volume loops of the left ventricle in pericardectomy for constrictive pericarditis. J Thorac Cardiovasc Surg. 1996;112:198–9.
Imagawa H, Ishikawa K. Images in cardiovascular medicine. Fading out dip-and-plateau pattern of right ventricular pressure in constrictive pericarditis. Circulation. 2010;122:404–5.
Cho YH, Schaff HV, Dearani JA, Daly RC, Park SJ, Li Z, et al. Completion pericardiectomy for recurrent constrictive pericarditis: importance of timing of recurrence on late clinical outcome of operation. Ann Thorac Surg. 2012;93:1236–40.
Kang SH, Song J-M, Kim M, Choo SJ, Chung CH, Kang D-H, et al. Prognostic predictors in pericardiectomy for chronic constrictive pericarditis. J Thorac Cardiovasc Surg. 2014;147:598–605.
Ha J-W, Oh JK, Schaff HV, Ling LH, Higano ST, Mahoney DW, et al. Impact of left ventricular function on immediate and long-term outcomes after pericardiectomy in constrictive pericarditis. J Thorac Cardiovasc Surg. 2008;136:1136–41.
Acknowledgements
We thank Andrea Baird, MD, from Edanz Group (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Saito, T., Fukushima, S., Yamasaki, T. et al. Pericardiectomy for constrictive pericarditis at a single Japanese center: 20 years of experience. Gen Thorac Cardiovasc Surg 70, 430–438 (2022). https://doi.org/10.1007/s11748-021-01718-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11748-021-01718-x