Abstract
Infantile antiphospholipid syndrome (APS) is a rare condition arising from either transplacental transfer of antiphospholipid antibodies (aPL) from the mother or de novo antibody production in the newborn. We present a unique case of cerebral artery thrombosis with persistently elevated anti-cardiolipin and anti-β2-glycoprotein-I antibodies, despite the absence of maternal aPL, suggesting primary de novo aPL synthesis. While the prevailing “second-hit” hypothesis suggests that additional thrombotic risk factors are required to trigger APS in infants, our case exhibited no prenatal, maternal, or thrombophilic risk factors. A literature review of 20 reported cases further confirmed that ours was the only case without additional thrombotic triggers among the 18 cases with complete data, challenging the necessity of a “second hit” in neonatal APS. Notably, aPL levels normalized over time without recurrence, raising questions about the need for long-term anticoagulation in select cases, including ours. These findings suggest a potential transient form of infantile APS and highlight the importance of sequential aPL testing to guide treatment. Further research is required to elucidate the mechanisms underlying de novo aPL synthesis and its clinical implications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antiphospholipid syndrome (APS) in adults is a well-established condition characterized by the occurrence of arterial, venous, or both, thrombosis, along with pregnancy morbidity, all accompanied by consistently positive antiphospholipid antibodies (aPL). These antibodies include lupus anticoagulant (LA), anti-cardiolipin (aCL), and/or anti-β2-glycoprotein I antibodies (aβ2GPI). Diagnosis typically requires the detection of these antibodies on a minimum of two consecutive occasions at least 12 weeks apart, in accordance with the international (Sydney) consensus statement criteria [1]. However, for research purposes, classification criteria were revised by the American College of Rheumatology (ACR) and the European League Against Rheumatism (EULAR) in 2023 which introduced a positive aPL test as an entry criterion and applied additive weighted criteria across clinical domains for APS classification [2].
Despite the comprehensive characterization of APS in adults, the literature currently lacks reliable data on the incidence and prevalence of pediatric APS due to the absence of validated clinical criteria [3]. Presently the diagnosis in the pediatric population relies on the application of adult criteria along with clinical assessment.
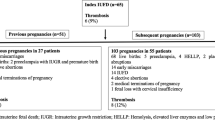
Infantile APS is a rare condition and only a few cases are reported in the literature [4,5,6,7]. The etiology of infantile APS can be classified into two primary factors: the transmission of maternal pathogenic antibodies through the placenta and the de novo synthesis of antibodies by the infant which is especially rare [8]. Evidence suggests that de novo infantile APS may necessitate the presence of additional thrombotic risk/trigger factors, often referred to as the “second-hit” mechanism as illustrated in Table 1 [4,5,6,7,8].
In the present paper, however, we report a case of atypical infantile de novo APS presented with a neonatal stroke, without the presence of additional risk/trigger factors, and discuss the treatment approach of this case. We further review the literature focusing on the additional risk factors related to reported cases with de novo infantile APS.
Materials and method
We performed a search of the literature for cases of infantile APS by using the keywords “neonatal” or “perinatal” or “infantile” together with “antiphospholipid antibody or syndrome.” in the electronic databases Medline/Pubmed, Embase, Scopus, and Directory of Open Access Journals through 9th of January 2025. The literature search was supplemented by a manual review of the references in the identified publications. We primarily reviewed English-language abstracts and articles, considering all study designs and article types, including case reports and letters to the editor, but excluding congress or meeting abstracts. Among this literature search, cases fulfilling the de novo occurrence of APS on the following criteria included this review: (a) neonatal, perinatal, and infantile presentation of thrombosis; (b) persistent positive aPL antibodies, including LA (analyzed on two different occasions); and (c) negative aPL antibodies, including LA in the mother or cord blood.
Study design, sex of the patients, clinical presentation, localization of thrombosis, infant and maternal aPL status, maternal, prenatal, thrombophilia risk factors, and anticoagulation treatment were extracted from the articles. The data are summarized in Table 2.
Information about our patient was retrieved from the electronic medical journal of the Thrombosis Clinic at the University Hospital of Southern Denmark, Esbjerg. Informed consent was obtained from the patient’s family to publish this paper.
LA was detected using a CS5100 coagulation analyzer (Sysmex Corporation, distributed by Siemens Healthcare) in accordance with ISTH guidelines [15] using two recommended assays with a CV of < 10%, the lupus-sensitive APTT, PTT-LA (Diagnostica Stago, Asnières-sur-Seine, France), and the dRVVT (Precision Biologic, Dartmouth, Canada). LA was considered positive if at least one of the two tests yielded a positive result.
The detection of aCL and aβ2GPI in the patient and patient’s mother was carried out using enzyme-labeled anti-isotype Assay (EliA) (Thermo Fisher Scientific), fully automated random access fluorescence enzyme immunoassays on the Phadia 250 instrument (Phadia GmbH) as previously described [16]. Both antibodies exhibited a CV of < 10%. A 99th percentile as the upper cutoff in the diagnosis of positive aPLs was utilized and determined through in-house validation in accordance with the approach suggested by the International Society on Thrombosis and Haemostasis (ISTH) [16].
Case presentation
Our patient, the first child of a 37-year-old healthy mother, was delivered at 41 + 3 weeks via a normal vaginal delivery following an uncomplicated gestational period. She had a normal birth weight (3540 g) and exhibited a full Apgar score. Upon discharge on the second post-delivery day, no abnormalities were noted. There was no maternal or family history of autoimmune disease, coagulation disorders, or cerebrovascular events. At 3.5 months of age, the parents observed reduced spontaneous movement in the left limbs. The patient was referred to a physiotherapist and a chiropractor for an initial evaluation, which confirmed reduced spontaneous movement in the left limbs. At 4.5 months of age physical examination revealed normative size for her age, but the neurological examination suggested a left-sided hemiparesis. A cerebral MRI performed at 5 months of age revealed encephalomalacia in the right frontal, temporal, and parietal lobes, consistent with an old right middle cerebral artery infarct (Fig. 1).
Thrombophilia screening performed at the age of 7.5 months showed normal blood count, prothrombin time, activated partial thromboplastin time, antithrombin III, protein C, protein S, and a normal genotype for factor V Leiden and factor II/prothrombin allele, as well as negative results for LA. However, high levels of IgG type aCL and aβ2GPI antibodies were detected (Table 3). The patient’s mother, who is entirely healthy with no prior history of fetal loss or thromboembolic events, tested negative for aPL antibodies 4 weeks after the initial positive aPL test in the patient (Table 3).
Follow-up testing of the patient 3 months later showed persistence of IgG aβ2GPI antibodies and IgG aCL antibodies though at reduced titers confirming infantile APS. The patient exhibited no other systemic manifestations of APS, except for neurological involvement. Both aCL and aβ2GPI antibodies were normalized 2 years after the initial assessment, also confirmed by consecutive negative tests for aPL almost 3 years apart (Table 3).
The patient received antiplatelet therapy with acetylsalicylic acid (ASA) at a dosage of 3 mg/kg, which was maintained until the normalization of high aPL levels, within 2.5 years.
Patient outcome
Throughout the 5.5-year follow-up period, the patient remained negative for aPL and LA and did not experience any recurrence of thrombotic events after discontinuation of ASA therapy. At the age of six, 8 months before the last normal aPL control, she however experienced focal seizures and was put on antiseizure medication. The follow-up MRI, conducted 6.5 years after the initial scan, revealed stable, extensive polycystic encephalomalacia in the right hemisphere, with no evidence of new infarcts. Additionally, two small hemosiderin deposits were noted at the frontal margin of the right frontal cyst.
Results
Including the present study, a total of 20 cases of infantile thrombosis associated with de novo synthesis of antiphospholipid antibodies (aPL) were identified across ten articles published as case reports or case series between 2010 and 2023 [5, 7, 8, 9,10,11,12,13,14] (Table 2).
Thrombotic manifestations of cases with de novo infantile APS
Among the 20 cases, 14 patients experienced ischemic stroke. One patient presented with small bowel infarction, renal vein thrombosis, and stroke associated with catastrophic APS. Another presented with a right atrial thrombus, while one developed sinus venous thrombosis. Additionally, one patient had deep vein thrombosis (DVT) in the left lower extremity, and another experienced multiple thrombosis in the central nervous system (CNS), affecting cerebral veins, sinuses, and arteries, including the left internal carotid. One further patient exhibited multiple thrombotic events in the context of catastrophic APS (Table 2).
Prenatal, maternal, and thrombophilic risk factors as “second-hit” mechanisms in infantile APS
Out of the 20 cases analyzed, only two cases (#7 and #11) and the present study (#20) reported no additional prenatal, maternal, or thrombophilic risk factors for thrombosis beyond APS. However, both cases (#7 and #11) were part of a case series with incomplete data. Specifically, case #7 lacked information on thrombophilia risk factors in the infant, while case #11 did not provide details on maternal risk factors (Table 2).
Among the 20 cases, prenatal risk factors for infantile thrombosis included infection or sepsis (7/20), the presence of a central venous catheter (2/20), dehydration (1/20), asphyxia (3/20), prematurity (5/20), respiratory distress syndrome (4/20), fetal inflammatory response syndrome (1/20), residual valvulopathies (1/20), chylothorax (1/20), hypoxic-ischemic encephalopathy 1/20), acute kidney injury (1/20), and macrosomia (1/20).
Maternal risk factors comprised diabetes or gestational diabetes (3/20), recurrent pregnancy losses or intrauterine fetal death (2/20), thrombus in the umbilical artery or vein (2/20), maternal infection (1/20), twin pregnancy (1/20), placental abruption (1/20), and protein S deficiency (1/20).
Thrombophilic risk factors identified in the infants included heterozygosity for the Factor V (FV) Leiden mutation (3/20), heterozygosity for the prothrombin (20210G/A) mutation (2/20), homozygosity for the methylenetetrahydrofolate reductase (MTHFR) mutation (either 677 T/T or 1298C/C) (3/20), homozygosity or compound homozygosity for plasminogen activator inhibitor-1 (PAI-1) mutations (either 844A/A and 675 4G/4G or 675G/A) (3/20), and elevated lipoprotein (a) levels (1/20) (Table 2).
Anticoagulation treatment of patients with de novo infantile APS
Data were missing for eight patients. Among the remaining cases, four patients were treated with ASA, one patient received both low-molecular-weight heparin (LMWH) and ASA, one patient was initially given unfractionated heparin, which was later switched to LMWH, three patients were treated with LMWH, and three patients did not receive any anticoagulation therapy (Table 2).
Discussion
In this paper, we present a case of infantile APS suffered from a neonatal thrombotic stroke, demonstrating persistent positivity for aPL antibodies, particularly high levels of aCL and aβ2GPI antibodies, leading to a diagnosis of primary APS with the absence of other APS manifestations. The mother showed no signs of aPL antibodies, suggesting primary de novo infantile aPL synthesis in the infant. Most notably the patient did not have additional risk factors beyond aPL to trigger de novo primary APS and exhibited a gradual disappearance of aPL over time. We also conducted a review of the existing literature on additional risk factors, termed the “second-hit” mechanism, in reported cases of de novo infantile APS. We identified 20 cases across 10 articles (Table 2). Among these, our case (#20) is the only one without additional prenatal, maternal, or thrombophilic risk factors, based on the 18 cases with complete data reporting all the aforementioned risk factors.
Despite the low incidence of clinical APS manifestations in infants, the brain is the most affected organ by thrombotic events, with the cerebral artery being the most affected site within the brain [6], as also highlighted in our current review. Of the 20 cases included in our review, 10 involved cerebral artery stroke, accounting for the majority of the 16 ischemic stroke cases. A meta-analysis identified the presence of aPL antibodies as a significant risk factor for arterial ischemic strokes in children, including neonates [17]. While there is strong evidence suggesting that aPLs can be pathogenic rather than merely a serological marker, it remains unclear whether aPLs alone are capable of triggering thrombosis.
Autoimmune diseases are uncommon in newborns due to immature immune systems, typically maturing by age 3 [18]. While most cases arise from transplacental transmission of maternal diseases, some pregnancies involve the transmission of aPL without resulting in clinical manifestations of APS. This is supported by a 5-year prospective study of 134 children born to mothers with APS found no instances of thrombosis despite the persistent presence of LA, aCL, or aβ2GPI antibodies) [19]. This further indicates that factors beyond aPL may be required to induce thrombotic events in neonates, supporting the notion of a “second-hit” model.
Given the rarity of infantile APS, only a limited number of cases have been reported, with the majority originating from the transplacental transmission of maternal antibodies. In the present paper, we expanded the previous review conducted by Gordon et al. [7], which included 11 cases of de novo neonatal APS. Our literature review identified 20 cases of de novo infantile APS, based on the criteria outlined in the Materials and Methods. Notably, in 18 of these cases, where complete data were provided by the authors, additional thrombotic risk or trigger factors were identified, with the exception of our case, where no supplementary risk factors were present.
According to a review by Gordon et al. [7] in de novo neonatal APS, the diagnosis was delayed compared to maternally transmitted APS, with an average diagnosis mean time of 4.7 months (range, 5 days to 13 months) after birth versus 2.2 months (range, immediately after birth–14 months). This delay is attributed to low clinician awareness or due to the absence of maternal or family history in de novo cases, whereas in maternally transmitted APS, nearly 40% of mothers had a diagnosis of APS before delivery, and others had a history of multiple miscarriages. In our case, the initial diagnosis of APS was made at 7.5 months after the birth, in a similar range to previously published de novo cases.
Contrary to the “second-hit” model, our case did not exhibit additional risk/trigger factors, typically associated with the onset of thrombotic events in neonatal APS, as recognized in the literature. These diverse risk factors encompass maternal, infant-specific conditions, and hereditary thrombophilia as presented in Table 1 [4, 5, 7,8,9,10,11,12,13,14]. Especially, hereditary thrombophilia, such as low levels of antithrombin, protein C, and protein S, as well as mutations in factors V and II (prothrombin) genes, are associated with thrombotic events in newborns, reflecting an imbalance between coagulants and anticoagulant activity. This is primarily attributed to the characteristics of the neonatal hemostasis system, which is marked by a prothrombotic state [8].
Remarkably, our case stands out as a rare instance of de novo APS without the presence of any other trigger factors, which is unprecedented in the literature. The question arises: what is the mechanism behind this? Berkun et al. [5] speculated that environmental factors, including vaccinations and drugs, might potentially trigger APS. They also proposed that the stress of delivery might induce the de novo aPL development in neonates.
Much of the information regarding the treatment of infantile APS is lacking in the reported cases in the literature [4,5,6,7] as also confirmed in our review (Table 2). The optimal therapy for infantile APS remains debated, with management primarily relying on observational studies and clinical expertise, leading to varied treatment approaches [20]. In our case, considering the patient’s age of 8 months and the absence of additional trigger risk factors, we chose antiplatelet therapy with a low dose of ASA (3 mg/kg/day) treatment which was continued until the normalization of aPL levels. Notably, Berkun et al. reported that high aPL levels normalized in 10 out of 12 neonatal APS cases with stroke, similar to our case, within 2.5 years [5]. Pines M et al. [14] described two de novo infantile APS cases—one with an atrial thrombus and another with multiple CNS thromboses—where LMWH was continued until aβ2GPI antibodies normalized at 37 and 59 weeks. During follow-up, no further thrombotic events were reported after 3 and 7 years following the cessation of anticoagulation. They suggested sequential aPL testing to guide treatment. These findings suggest that some patients meeting APS criteria may experience transient disease without recurrence, potentially eliminating the need for long-term anticoagulant therapy unless other risk factors are present. It is tempting to define these patients as having “pseudo infantile APS”. However, further longitudinal and larger cohort studies are necessary to gain a deeper understanding of this phenomenon.
A key strength of this study is its novelty, as it represents the first case report and review to specifically focus on infantile de novo APS and the identification of additional triggering risk factors, as a “second-hit mechanism” observed in affected patients. One limitation of our report is the timing of aPL testing in the mother, which was conducted one month after the patient’s APS diagnosis. This issue was also observed in most of the cases presented in Table 2, where aPL testing in the mother and infant was not performed simultaneously. Although transient aPL positivity during pregnancy cannot be completely excluded, it is considered unlikely in our case. The mother is healthy, with no history of fetal loss or thromboembolic events, and she experienced a normal vaginal delivery following an uncomplicated pregnancy. Another limitation of our study is the potential for incomplete patient data in our review, as outlined in Table 2, particularly when patients were reported within case series rather than as individual case reports.
In conclusion, this case presents a unique instance of de novo infantile APS characterized by the absence of additional trigger risk factors as a “second hit” among the 18 cases of de novo neonatal APS with complete data according to our review of cases reported in the literature. Moreover, the patient’s condition exhibited an atypical course, marked by the absence of other APS manifestations and a gradual disappearance of aPL. This unique case calls for further investigation into the mechanisms underlying infantile APS, particularly the potential role of environmental factors in initiating de novo antibody synthesis. Additionally, it raises questions about the necessity of long-term anticoagulation therapy in cases where no triggering risk factors are present.
Data availability
No datasets were generated or analysed during the current study.
References
Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost. 2006;4:295–306.
Barbhaiya M, Zuily S, Naden R, Hendry A, Manneville F, Amigo MC, et al. 2023 ACR/EULAR antiphospholipid syndrome classification criteria. Ann Rheum Dis. 2023;82:1258–70.
Madison JA, Zuo Y, Knight JS. Pediatric antiphospholipid syndrome. Eur. J Rheumatol. 2020;7:S3-s12.
Boffa MC, Lachassinne E. Infant perinatal thrombosis and antiphospholipid antibodies: a review. Lupus. 2007;16:634–41.
Berkun Y, Simchen MJ, Strauss T, Menashcu S, Padeh S, Kenet G. Antiphospholipid antibodies in neonates with stroke–a unique entity or variant of antiphospholipid syndrome? Lupus. 2014;23:986–93.
Peixoto MV, de Carvalho JF, Rodrigues CE. Clinical, laboratory, and therapeutic analyses of 21 patients with neonatal thrombosis and antiphospholipid antibodies: a literature review. J Immunol Res. 2014. https://doi.org/10.1155/2014/672603.
Gordon O, Almagor Y, Fridler D, Mandel A, Qutteineh H, Yanir A, et al. De novo neonatal antiphospholipid syndrome: a case report and review of the literature. Semin Arthritis Rheum. 2014;44:241–5.
Bitsadze V, Nalli C, Khizroeva J, Lini D, Andreoli L, Lojacono A, et al. APS pregnancy - the offspring. Lupus. 2020;29:1336–45.
Alshekaili J, Reynolds G, Cook MC. De novo infantile primary antiphospholipid antibody syndrome. Lupus. 2010;19:1565–8.
Cabral M, Abadesso C, Conde M, Almeida H, Carreiro H. Catastrophic antiphospholipid syndrome: first signs in the neonatal period. Eur J Pediatr. 2011;170:1577–83.
Merlin E, Dore E, Chabrier S, Biard M, Marques-Verdier A, Stephan JL. A case of infantile de novo primary antiphospholipid syndrome revealed by a neonatal arterial ischemic stroke. J Child Neurol. 2012;27:1340–2.
SoaresRolim AM, Castro M, Santiago MB. Neonatal antiphospholipid syndrome. Lupus. 2006;15:301–3.
Giani T, Mauro A, Ferrara G, Cimaz R. Case report: infantile ischemic stroke and antiphospholipid antibodies, description of four cases. Front Pediatr. 2020. https://doi.org/10.3389/fped.2020.596386.
Pines M, Meyer R, Grabowski EF, Flynn P, Kucine N. De novo antiphospholipid antibody syndrome in two infants. Pediatr Blood Cancer. 2023;70:e30129. https://doi.org/10.1002/pbc.30129.
Pengo V, Tripodi A, Reber G, Rand JH, Ortel TL, Galli M, de Groot PG. Update of the guidelines for lupus anticoagulant detection. J Thromb Haemost. 2009;7:1737–40.
Bor MV, Jacobsen IS, Gram JB, Sidelmann JJ. Revisiting the Phadia/EliA cut-off values for anticardiolipin and anti-β2-glycoprotein I antibodies: a systematic evaluation according to the guidelines. Lupus. 2018;27:1446–54.
Kenet G, Lütkhoff LK, Albisetti M, Bernard T, Bonduel M, Brandao L, et al. Impact of thrombophilia on risk of arterial ischemic stroke or cerebral sinovenous thrombosis in neonates and children: a systematic review and meta-analysis of observational studies. Circulation. 2010;121:1838–47.
Chang C. Neonatal autoimmune diseases: a critical review. J Autoimmun. 2012;38:J223–38.
Mekinian A, Lachassinne E, Nicaise-Roland P, Carbillon L, Motta M, Vicaut E, et al. European registry of babies born to mothers with antiphospholipid syndrome. Ann Rheum Dis. 2013;72:217–22.
Groot N, de Graeff N, Avcin T, Bader-Meunier B, Brogan P, Dolezalova P, et al. European evidence-based recommendations for diagnosis and treatment of childhood-onset systemic lupus erythematosus: the SHARE initiative. Ann Rheum Dis. 2017;76:1788–96.
Acknowledgements
We thank consultant neuroradiologist Ronald Antulov MD, PhD, for interpreting and preparation the patient’s MR images for use in the article.We also thank the patient's mother for granting permission to publish this article. Doruk Bor (DB) participated in this study while voluntarily undertaking a clinical clerkship in the Clinical Biochemistry department, University Hospital of Southern Denmark, Esbjerg.
Funding
Open access funding provided by University of Southern Denmark.
Author information
Authors and Affiliations
Contributions
DB performed the literature review, interpreted the data, and wrote the first draft of the manuscript and approved the final manuscript. MVB planned and designed the study, supervised for the recruitment of the patient, supervised the literature review, interpreted the data, and supervised the writing of the manuscript, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval is not required for this study in accordance with local or Danish national guidelines.
Consent to participate and for publication
Verbal informed consent, which was recorded in the patient’s electronic journal was obtained from the patient’s mother to participate in our study and for the publication of this case report.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bor, D., Bor, M.V. A case of atypical infantile de novo antiphospholipid syndrome presenting with neonatal ischemic stroke without any triggering risk factors as a “second hit” and review of the literature. Immunol Res 73, 53 (2025). https://doi.org/10.1007/s12026-025-09605-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12026-025-09605-w