Abstract
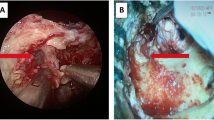
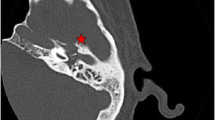
Skull base osteomyelitis is a vicious infection of temporal bone associated with very high morbidity and mortality. But few studies have been undertaken recently for eliciting its increasing incidence. Hence this study aims to describe the clinical profile of skull base osteomyelitis and changes noted in the post-covid period, and encourage a uniform treatment policy globally. This descriptive study was conducted among 140 patients diagnosed with skull base osteomyelitis. Data was collected using semi-structured proforma, HRCT temporal bone findings, microbiological reports, histopathology of granulation tissue, ESR and House-Brackmann grading. Male patients in 61–70 age group were most commonly affected and all patients had uncontrolled diabetes mellitus, usually presenting with nocturnal otalgia, ear canal granulation and cranial nerve palsy. Pseudomonas aeruginosa was the most common isolate followed by Staphylococcus aureus. Among fungal pathogens, candida albicans were the most common. 29.3% patients had extensive disease according to Thakar et al. staging and on follow up, 43.75% patients showed a satisfactory response. Coronary artery disease and cerebrovascular accidents were the leading cause of death. More atypical organisms, extensive disease and changes in antibiotic sensitivity were noted in the post-covid period. Prolonged treatment with culture sensitive antibiotic is the main stay of treatment. A uniform treatment guideline is needed for proper management of such patients.
Level of Evidence 4.





Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Cheng YF, Yang TH, Wu CS, Kao YW, Shia BC, Lin HC (2019) A population based time trend study in the incidence of malignant otitis externa. Clin Otolaryngol 44:851–855
Akhtar F, Iftikhar J, Azhar M, Raza A, Sultan F (2021) Skull base osteomyelitis: a single-center experience. Cureus 13(12):e20162. https://doi.org/10.7759/cureus.20162.PMID:35003991;PMCID:PMC8722461
Prasad KC, Prasad SC, Mouli N, Agarwal S (2007) Osteomyelitis in the head and neck. Acta Otolaryngol 127:194–205
Chang PC, Fischbein NJ, Holliday RA (2003) Central skull base osteomyelitis in patients without otitis externa: imaging findings. AJNR Am J Neuroradiol 24:1310–1316
Johnson AK, Batra PS (2014) Central skull base osteomyelitis: an emerging clinical entity. Laryngoscope 124:1083–1087
Rubin Grandis J, Branstetter BF 4th, Yu VL (2004) The changing face of malignant (necrotising) external otitis: clinical, radiological, and anatomic correlations. Lancet Infect Dis 4:34–39
Rinaldi MG (1983) Invasive aspergillosis. Rev Infect Dis 5:1061–1077
Carfrae MJ, Kesser BW (2008) Malignant otitis externa. Otolaryngol Clin North Am 41:537
Unnikrishnan R, Faizal BP, Pillai MG, Paul G (2013) Villaret’s syndrome: a rare presentation of skull base osteomyelitis. Case report Amrita J Med 9:1–44
Patmore H, Jebreel A, Uppal S, Raine CH, McWhinney P (2010) Skull base infection presenting with multiple lower cranial nerve palsies. Am J Otolaryngol 31:376–380
Khan MA, Quadri SAQ, Kazmi AS et al (2018) A comprehensive review of skull base osteomyelitis: diagnostic and therapeutic challenges among various presentations. Asian J Neurosurg 13(4):959–970. https://doi.org/10.4103/ajns.AJNS_90_17
Singh A, Al Khabori M, Hyder MJ (2005) Skull base osteomyelitis: Diagnostic and therapeutic challenges in atypical presentation. Otolaryngol Head Neck Surg 133:121–125
Adams A, Offiah C (2012) Central skull base osteomyelitis as a complication of necrotizing otitis externa: imaging findings, complications, and challenges of diagnosis. Clin Radiol 67:e7-16
Lee S, Hooper R, Fuller A, Turlakow A, Cousins V, Nouraei R et al (2008) Otogenic cranial base osteomyelitis: a proposed prognosis-based system for disease classification. Otol Neurotol 29:666–672
Acknowledgements
I would like to acknowledge all faculty of ENT Department for their guidance and support.
Funding
This paper has received no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors bear no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Krishnakumar, L., Vinayakumar, V., Suchit Roy, B.R. et al. Skull Base Osteomyelitis- Marauders of the Skull. Indian J Otolaryngol Head Neck Surg 76, 1770–1774 (2024). https://doi.org/10.1007/s12070-023-04405-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-04405-w