Abstract
The work is aimed to investigate whether midazolam functions in thyroid cancer and reveal the potential mechanism of action. Cell viability was detected by CCK-8 method when treated by varying doses of midazolam to detect the cytotoxicity of midazolam on human thyroid follicular epithelial cell line and thyroid cancer cell lines. In thyroid cancer cells, EDU staining, wound healing and transwell assays were respectively used to detect cell proliferation, migration and invasion. Western blot was used to detect the expressions of matrix metalloproteinases (MMPs). Flow cytometry assay, western blot and immunofluorescence staining were used to detect cell apoptosis. CB-Dock2 server predicted midazolam-tyrosine 3-monooxygenase/tryptophan 5-monooxygenase activation protein eta (YWHAH) interaction and western blot was also used to detect YWHAH expression. Midazolam dose-dependently decreased the viability of thyroid cancer cells and demonstrated no cytotoxicity on Nthy-ori-3-1 cells. In addition, increasing concentrations of midazolam or silencing of YWHAH significantly inhibited thyroid cancer cell proliferation, migration and invasion and induced cell apoptosis. Midazolam had a molecular binding with YWHAH and midazolam downregulated YWHAH expression. YWHAH partially reversed the impacts of midazolam on the cellular events in thyroid cancer. Collectively, midazolam may act as an anti-thyroid cancer agent via its interrelation with YWHAH.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Avoid common mistakes on your manuscript.
1 Introduction
Thyroid cancer originating from follicular or parafollicular thyroid cells approximately takes up 95% of all endocrine cancer cases, representing the most primary endocrine gland malignancy [1]. The new cases of thyroid cancer are reported to rise above half a million, leading to over 40,000 estimated deaths annually [2]. Importantly, the prevalence rate among females is predicted to be three- to four-fold higher that among males [1], suggesting that thyroid cancer is the only nonreproductive neoplasm with a marked female predominance. Most thyroid cancer types respond well to conventional treatment such as surgery and radioactive iodine therapy [3]. The therapy for thyroid cancer remains an issue since the tumor metastasizes more frequently to regional lymph nodes than to distant sites [4]. In this regard, novel therapeutic agents need to be exploited to develop effective treatment strategies of metastatic thyroid cancer.
As a γ-aminobutyric acid A (GABAA) receptor agonist of the benzodiazepine class, midazolam has potently hypnotic, sedative, anxiolytic, amnestic, anticonvulsant and muscle-relaxant effects through mediating benzodiazepine receptors in the central nervous system [5]. In clinical practice, midazolam is commonly applied as a sedative and an anesthetic adjuvant. Emerging literatures have demonstrated the anti-tumor activity of midazolam, such as lung cancer, breast cancer, hepatocellular carcinoma, head and neck squamous carcinoma and so on [6]. Nonetheless, the role of midazolam in thyroid cancer remains unclear to date.
The 14-3-3 family proteins are vital scaffold proteins that are ubiquitously expressed throughout the body with a regulatory role in numerous cellular processes [7]. As a member of the 14-3-3 protein family, tyrosine 3-monooxygenase/tryptophan 5-monooxygenase activation protein eta (YWHAH) has been widely involved in the biological events in human malignancies [8,9,10]. Noticeably, YWHAH has been widely considered as an oncogene in thyroid cancer [11, 12]. Further, recent evidence has demonstrated that YWHAH expression is down-regulated by midazolam during neurodevelopment [13].
Correspondingly, the work is committed to addressing the issue that whether midazolam functions in thyroid cancer and unraveling the interrelated response mechanism.
2 Materials and methods
2.1 Cell culture and treatment
Human thyroid follicular epithelial cell line Nthy-ori-3-1 provided by European Collection of Cell Cultures (ECACC) and thyroid cancer cell lines (TPC-1, BCPAP and KTC-1) purchased from BeNa Culture Collection (BNCC) were all incubated in Roswell Park Memorial Institute (RPMI)-1640 medium (VivaCell, Shanghai, China) with 10% fetal bovine serum (FBS; VivaCell, Shanghai, China) with 5% CO2 at 37 °C in a humidified incubator. The cells were passaged every three days, and log-phase cells were collected for experiments.
Additionally, all cells were treated by midazolam (Nhwa Pharmaceutical, Jiangsu, China) at varying doses (5, 10, 15, 20 and 40 μg/ml) for 24 h [14]. Subsequently, PTC-1 cells were treated by midazolam (15, 20 and 40 μg/ml) for 24 h and KTC-1 cells were treated by midazolam (35, 50 and 75 μg/ml) for 24 h.
2.2 Gene interference
The siRNAs targeting YWHAH (siRNA-YWHAH-1/2) and the scramble siRNA (siRNA-NC) were designed by Integrated DNA Technologies (San Diego, CA, USA). The synthetic YWHAH overexpression plasmid (Ov-YWHAH) and Ov-NC were purchased from Zoman (Beijing, China). Cells were seeded in 24-well plates at an optimized concentration of ~ 1 × 105 cells/well. When cell confluence had reached 60–70%, the aforementioned plasmids and siRNAs (100 nM) were then transfected into cells with Lipofectamine 2000 (Invitrogen, Carlsbad, CA, USA) at 37 °C for 48 h according to the manufacturer’s instructions. 48 h post transfection, the cells were collected for further assays. The following siRNA sequences were used: siRNA-YWHAH-1, 5′-CTCCAATGAAGATCGAAATCTCC-3′; siRNA-YWHAH-2, 5′-CACTAAACGAGGATTCCTATAAG-3′.
2.3 Cell counting kit-8 (CCK-8)
Nthy-ori-3-1 cells and thyroid cancer cells were seeded into the 96-well flat-bottomed plate (5 × 103 cells/well) and cultured at 37˚C, and treated by midazolam (5, 10, 15, 20 and 40 μg/ml) for 24 h. Additionally, TPC-1 cells were transfected with siRNA-YWHAH, siRNA-NC or Ov-YWHAH, Ov-NC in the presence or absence of midazolam (40 μg/ml). 10 μl CCK8 working liquid (ApexBio Technology, Houston, TX, United States) was added to each well. The plates were incubated for 2 h and the absorbance was measured with a microplate reader (Thermo MK3, Thermo Fisher Scientific, USA) at 450 nm.
2.4 5-Ethynyl-2′-deoxyuridine (EDU) staining
As per the protocol of the EdU Labeling Kit (Beyotime, Shanghai, China), TPC-1 and KTC-1 cells were seeded into 12-well plates (1.5 × 104 cells/well) were incubated with pre-warmed complete medium consisting of 10 µM EDU working solution for 1 h. Afterwards, cells were fixed with 3.7% paraformaldehyde for 15 min were then permeabilized by 0.5% Triton X-100 for 20 min. Following cultivation with 1 × ClickiT® reaction cocktail, the cell nuclei were stained with DAPI. The images were captured under a fluorescence microscope and the EDU-positive cells were counted with ImageJ software (version 1.8.0; National Institutes of Health).
2.5 Wound healing assay
TPC-1 and KTC-1 cells were plated in 6-well plates at 5 × 105 cells/well using serum-free RPMI-1640 medium at 37˚C for 24 h until cells reached 90% confluence. Linear wounds were created using a pipette tip, followed by PBS washing to remove the detached cells. Subsequently, the obtained cells were cultured in RPMI-1640 medium containing 2% FBS for 24 h at 37 °C. The wound healing rates were observed under an optical microscope at 0 and 24 h under a light microscope. The migration rate was calculated based on the formula: (Wound width at 0 h-wound width at 24 h)/wound width at 0 h × 100%.
2.6 Transwell assay
Transwell invasion assays were performed using 8-mm pore size Transwell® plates (Corning Inc.) that were coated with Matrigel (BD Biosciences) for 1 h at 37 °C. TPC-1 and KTC-1 cells (5 × 104 cells) were seeded into the upper chamber of the Transwell plate. The upper wells were filled with serum-free RPMI 1640 and the bottom wells were filled with RPMI-1640 containing 10% FBS. The cells were fixed with 10% methanol at room temperature for 10 min and stained with 0.5% crystal violet at room temperature for 10 min. The invaded cells were counted under a light microscope.
2.7 Flow cytometry assay
Cell apoptosis was appraised utilizing Annexin V-FITC/PI apoptosis detection kit (Qihai Biotec, Shanghai, China). TPC-1 and KTC-1 cells were seeded at a density of 2 × 105 cells per well in six-well plates. After being digested with trypsin, cells were centrifuged at 1000Xg for 5 min and re-suspended in 100 µl 1X binding buffer. Then the cells were double-stained with 5 μl Annexin V-FITC and propidium iodide (PI) for 15 min in the dark. The analysis was performed using a BD FACSAria™ II flow cytometer (Becton–Dickinson and Company), and the data were analyzed using CellQuest Pro software (version 5.1; Becton–Dickinson and Company).
2.8 Reverse transcription-quantitative PCR (RT-qPCR)
Total RNA was isolated from TPC-1 and KTC-1 cells using TRIzol reagent (TSINGKE, Shanghai, China). mRNA was reverse transcribed into cDNA using the cDNA synthesis Kit (TSINGKE, Shanghai, China) and the reaction was incubated at 25 °C for 5 min, 42 °C for 30 min, 85 °C for 5 min and then kept at 4 °C for 5 min. PCR reaction was implemented using 2 × TSINGKE® Master qPCR Mix (TSINGKE, Shanghai, China). The thermocycling conditions were as follows: Initial denaturation at 95 °C for 5 min, followed by 35 cycles of denaturation (45 s at 95 °C), annealing (45 s at 60 °C) and extension (8 min at 68 °C), before a final extension at 68 °C for 10 min. GAPDH was used for normalization, where gene expression was calculated using the 2−ΔΔCq method. The following primers were used: YWHAH forward, 5′-CCGCTACTTAGCAGAGGTCG-3′ and reverse, 5′-TGGCATCATCGAAGGCTTGT-3′ and β-actin forward, 5′-TGGAGTCCACTGGCGTCTTC-3′ and reverse, 5′-GCTTGACAAAGTGGTCGTTGAG-3′.
2.9 Western blot analysis
Total protein was extracted from TPC-1 and KTC-1 cells containing 1% protease and 1% phosphatase inhibitor cocktail (Sigma Aldrich; Merck KGaA) on ice using RIPA buffer (Abiowell, China). The concentration of protein samples was measured using a BCA kit (GENEray, Shanghai, China). Subsequently, equal amounts of proteins (40 µg) were separated by 10% SDS-PAGE and then transferred onto PVDF membranes. The membranes were blocked by 5% skim milk at 4 °C at room temperature for 1 h, and then incubated with primary antibodies against MMP2 (ab92536; 1/1000; Abcam), MMP9 (ab76003; 1/1000; Abcam), BCL2 (ab182858; 1/2000; Abcam), Bax (ab32503; 1/1000; Abcam), cleaved caspase3 (ab32042; 1/500; Abcam), YWHAH (ab206292; 1/1000; Abcam) and GAPDH (ab9485; 1/2500; Abcam) overnight at 4 °C at room temperature. The membranes were washed three times and incubated with horseradish peroxidase (HRP)-conjugated secondary antibodies (ab6721; 1/2000; Abcam) for 1 h at room temperature. The protein blots were visualized with the ECL solvent (Qihai Biotec, Shanghai, China) and quantified by ImageJ software (version 1.8.0; National Institutes of Health).
2.10 Immunofluorescence staining
TPC-1 and KTC-1 cells (2 × 105 cells/ml) were fixed with 4% paraformaldehyde at room temperature for 15 min and permeabilized with 0.5% Triton X-100 for 20 min at room temperature. After being sealed by 5% BSA, cells were incubated with primary antibodies against cleaved caspase3 overnight at 4 °C and secondary antibody conjugated with Alexa-Fluor 488 for 1 h at room temperature. The cell nuclei were stained with 1 mg/ml DAPI and the images were captured under a fluorescence microscope.
2.11 Statistics
All experiments were performed at least three times. All data were presented as mean ± standard deviation (SD). Statistical analyzes were performed using GraphPad 6 Software (GraphPad Software, Inc.). Multiple group comparisons were analyzed with one-way ANOVA along with Tukey’s post hoc test. P-value less than 0.05 was considered to indicate a statistically significant difference.
2.12 Bioinformatics tools
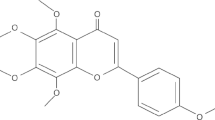
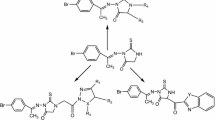
The midazolam structure and YWHAH protein crystal structure (PDB ID: 2c63) were obtained from PubChem (https://pubchem.ncbi.nlm.nih.gov/) and RCSB (http://www.rcsb.org/) databases, respectively. CB-Dock2 server (https://cadd.labshare.cn/cb-dock2), which is a molecular docking program based on AutoDock Vina [15], was applied to explore the docking of midazolam with YWHAH. All parameters were set to their default values.
3 Results
3.1 Midazolam concentration-dependently decreases thyroid cancer cell proliferation
To totally uncover the specific impacts of midazolam on the process of thyroid cancer, the aggressive phenotypes of thyroid cancer cells were evaluated when treated by varying concentrations of midazolam. As demonstrated by CCK-8 assay, increasing concentrations of midazolam (5, 10, 15, 20 and 40 μg/ml) exerted no significant influence on Nthy-ori-3-1 cell viability while significantly decreasing the viability of thyroid cancer cells including BCPAP (IC50 value: 38.28 μg/ml), TPC-1 (IC50 value: 30.75 μg/ml) and KTC-1 cells (IC50 value: 51.20 μg/ml) (Fig. 1A). Considering that midazolam demonstrated the most significant effect on TPC-1 and KTC-1 cells, TPC-1 and KTC-1 cells were utilized as representative cells in the following functional experiments to investigate the effects of midazolam on thyroid cancer cells. Considering the IC50 values of midazolam in TPC-1 and KTC-1 cells were respectively 30.75 μg/ml and 51.20 μg/ml, 15, 20 and 40 μg/ml of midazolam were selected for TPC-1 cells and 35, 50 and 75 μg/ml of midazolam were selected for KTC-1 cells. The experimental data from EDU staining also demonstrated that treatment with midazolam significantly reduced the number of EDU positive TPC-1 cells in a concentration-dependent manner (Fig. 1B).
Midazolam concentration-dependently decreases thyroid cancer cell proliferation. A CCK-8 method was used to detect the viability of Nthy-ori-3-1 cells and thyroid cancer cells. *P < 0.05 and ***P < 0.001 vs Nthy-ori-3-1. B EDU staining was used to detect TPC-1 cell proliferation. All experiments were performed at least three times
3.2 Midazolam concentration-dependently inhibits thyroid cancer cell migration and invasion
At the same time, through wound healing and transwell assays, it was discovered that the abilities of TPC-1 and KTC-1 cells to migrate and invade were significantly decreased by increasing concentrations of midazolam (Fig. 2A-B; Fig. S1A-B). To better convince these findings, the expressions of metastasis-associated MMP2 and MMP9 were detected and the results demonstrated that MMP2 and MMP9 protein expressions were both significantly downregulated when treated by increasing concentrations of midazolam (Fig. 2C; Fig. S1C).
Midazolam concentration-dependently inhibits TPC-1 cell migration and invasion. A Wound healing assay was used to detect TPC-1 cell migration. B Transwell assay was used to detect TPC-1 cell invasion. C Western blot was used to detect the expressions of MMPs in TPC-1 cells. All experiments were performed at least three times. *P < 0.05, **P < 0.01 and ***P < 0.001
3.3 Midazolam concentration-dependently induces thyroid cancer cell apoptosis
Meanwhile, from flow cytometry analysis, the enhanced apoptosis rate was observed in TPC-1 and KTC-1 cells treated by midazolam at varying concentrations (Fig. 3A; Fig. S2A). Upon exposure to increasing concentrations of midazolam, BCL2 expression was declined whereas Bax and cleaved caspase3 expressions were increased (Fig. 3B, C; Fig. S2B-C).
Midazolam concentration-dependently induces TPC-1 cell apoptosis. A Flow cytometry assay was used to detect TPC-1 cell apoptosis. B Western blot was used to detect the expressions of apoptotic proteins in TPC-1 cells. C Immunofluorescence staining was used to detect cleaved caspase3 expression in TPC-1 cells. All experiments were performed at least three times. *P < 0.05, **P < 0.01 and ***P < 0.001
3.4 Midazolam interacts with and downregulates YWHAH expression in TPC-1 cells
Herein, by CB-Dock2 server, the molecular binding of midazolam with YWHAH was confirmed (Fig. 4A). Western blot analysis also demonstrated that YWHAH protein expression was dose-dependently decreased in TPC-1 cells treated by midazolam (Fig. 4B). Consequently, midazolam at the concentration of 40 μg/ml which demonstrated the most significant effect was chosen for the following assays.
3.5 YWHAH knockdown suppresses thyroid cancer cell proliferation, migration, invasion while inducing cell apoptosis
Considering the down-regulated YWHAH expression in midazolam-treated TPC-1 cells, the specific influences of YWHAH on thyroid cancer cells also needed to be determined. Initially, YWHAH was dramatically cut down after transfection of siRNA-YWHAH-1/2 (Fig. 5A, B; Fig. S3A-B). YWHAH expression was lower in the siRNA-YWHAH-1 group than in the siRNA-YWHAH-2 group, demonstrating the significant interference efficacy of siRNA-YWHAH-1. Therefore, siRNA-YWHAH-1 was utilized and being briefly referred to as siRNA-YWHAH in the following assays. As expected, TPC-1 and KTC-1 cell activity and proliferation were significantly inhibited after YWHAH was silenced (Fig. 5C, D; Fig. S3C-D). Similarly, as demonstrated in Fig. 5E–G and Fig. S3E-G, interference with YWHAH decreased the capability of TPC-1 and KTC-1 cells to metastasize, validated by the declined migrated and invaded cells and the downregulated MMP2 and MMP9 expressions. Besides, the results from flow cytometry assay demonstrated that YWHAH knockdown increased the apoptotic rate, accompanied with the downregulated BCL2 expression, the enhanced Bax and cleaved caspase3 expressions in TPC-1 cells (Fig. 6A–C).
YWHAH knockdown suppresses TPC-1 cell proliferation, migration as well as invasion. A-B Examination of transfection efficacy of siRNA-YWHAH-1/2 in TPC-1 cells. C CCK-8 method was used to detect TPC-1 cell viability. D EDU staining was used to detect TPC-1 cell proliferation. E Wound healing assay was used to detect TPC-1 cell migration. F Transwell assay was used to detect TPC-1 cell invasion. G Western blot was used to detect the expressions of MMPs in TPC-1 cells. All experiments were performed at least three times. **P < 0.01 and ***P < 0.001
YWHAH knockdown induces TPC-1 cell apoptosis. A Flow cytometry assay was used to detect TPC-1 cell apoptosis. B Western blot was used to detect the expressions of apoptotic proteins in TPC-1 cells. C Immunofluorescence staining was used to detect cleaved caspase3 expression in TPC-1 cells. All experiments were performed at least three times. ***P < 0.001
3.6 Midazolam suppresses TPC-1 proliferation, migration, invasion and stimulates cell apoptosis via down-regulating YWHAH
With the goal of validating the suppressive mechanism of midazolam involving YWHAH, the aforementioned functional experiments were implemented again in YWHAH-overexpressing TPC-1 cells treated by midazolam. Following transfection of Ov-YWHAH, YWHAH expression was signifciantly elevated (Fig. 7A). The results of CCK-8 and EDU staining assays demonstrated that YWHAH elevation promoted the viability and proliferation which were both inhibited in midazolam-treated TPC-1 cells (Fig. 7B, C). Meanwhile, the declined abilities of TPC-1 cells to migrate and invade accompanied by the decreased MMP2 and MMP9 protein expressions imposed by midazolam treatment were both accelerated again when YWHAH was up-regulated (Fig. 7D–F). Upon exposure to midazolam, the number of apoptotic cells was enhanced, which was then reduced again after YWHAH was overexpressed (Fig. 8A). Consistently, the depleted BCL2 expression and the elevated Bax and cleaved caspase3 expressions in TPC-1 cells treated by midazolam were all partially reversed by YWHAH elevation (Fig. 8B, C).
Midazolam suppresses TPC-1 proliferation, migration, invasion and stimulates cell apoptosis via down-regulating YWHAH. A Examination of transfection efficacy of Ov-YWHAH in TPC-1 cells. B CCK-8 method was used to detect TPC-1 cell viability. C EDU staining was used to detect TPC-1 cell proliferation. D Wound healing assay was used to detect TPC-1 cell migration. E Transwell assay was used to detect TPC-1 cell invasion. F Western blot was used to detect the expressions of MMPs in TPC-1 cells. All experiments were performed at least three times. **P < 0.01 and ***P < 0.001
Midazolam induces TPC-1 cell apoptosis via down-regulating YWHAH. A Flow cytometry assay was used to detect TPC-1 cell apoptosis. B Western blot was used to detect the expressions of apoptotic proteins in TPC-1 cells. C Immunofluorescence staining was used to detect cleaved caspase3 expression in TPC-1 cells. All experiments were performed at least three times. ***P < 0.001
4 Discussion
A considerable body of evidence has revealed the tumor-suppressing or tumor-promoting role of anesthetics in cancers [16,17,18]. Midazolam, as an intravenous anesthetic agent, has been revealed to serve as a potent anti-tumor drug in diverse human malignancies [6, 19]. The information provided in the official labeling of [MIDAZOLAM HYDROCHLORIDE] by Pfizer has stated that midazolam may lead to a small but statistically significant increase in benign thyroid follicular cell tumors in high-dose male rats, suggesting the potential pro-tumorigenic role of midazolam in vivo. Interestingly, the current work conducted a comprehensive research on the role of midazolam in regulating the tumorigenesis and tumor metastasis in thyroid cancer in vitro. Functionally, midazolam decreased the abilities of thyroid cancer cells to proliferate, migrate, invade and induced cell apoptosis, which was distinctly different from the aforementioned information. Additionally, midazolam interacted with YWHAH mechanistically. To the best of our knowledge, it may be the first time to highlight the anticarcinogenic effect of midazolam in thyroid cancer and the potential mechanism of action.
Tumor cells are characterized by overproliferation, migration, invasion and the latter two phenotypes may increase the metastatic potential of tumors. Previous investigations have demonstrated that midazolam can inhibit the proliferation, migration and invasion of lung carcinoma cells [20], breast carcinoma cells [21] and hepatocellular carcinoma cells [14]. Initially, to ensure the safety of midazolam for normal cells, midazolam at varying concentrations (5, 10, 15, 20 and 40 μg/ml) were used in our study, which was far lower than the dosage used in mice in vivo [22]. Our investigation manifested that midazolam at varying concentrations significantly decreased the viability of thyroid cancer cells instead of human thyroid follicular epithelial cell line Nthy-ori-3-1, suggesting that midazolam at 5, 10, 15, 20 and 40 μg/ml was safe for Nthy-ori-3-1 cells. Subsequently, according to the IC50 values, the optimal concentrations of midazolam were respectively selected for TPC-1 and KTC-1 cells. Midazolam was also demonstrated to decrease the abilities of TPC-1 and KTC-1 cells to proliferate, migrate and invade in a dose-dependent manner. The basement membrane (BM), a specialized sort of extracellular matrix, is able to inhibit tumor progression through forming the major barrier to prevent cancer cells from metastasizing to surrounding tissues [23]. MMPs, that are believed to cleave BM components, are often found overexpressed during cancer progression [24]. Here, the experimental data demonstrated that midazolam downregulated MMP2 and MMP9 expressions in TPC-1 and KTC-1 cells as expected.
As the most renowned programmed cell death mode, apoptosis is pivotal in maintaining cell and tissue homeostasis and defective apoptosis is recognized to be responsible for cancers [25]. In the intrinsic (mitochondrial) pathway of apoptosis, Bax activation can initiate the caspase cascade, thus committing cells to the programmed death, which may be blocked by anti-apoptotic BCL2 [26]. Importantly, the pro-apoptotic role of midazolam has been also demonstrated in lung carcinoma [27], hepatocellular carcinoma [14] and pancreatic ductal adenocarcinoma [28]. Accordantly, treatment with midazolam increased the apoptotic rate of TPC-1 and KTC-1 cells, also proved by the decreased BCL2 expression and the enhanced Bax, cleaved caspase3 expressions.
Intriguingly, a literature published in 2023 has mentioned that long-term midazolam exposure can downregulate YWHAH expression during early neurodevelopment [13]. To further identify the intercorrelation of midazolam with YWHAH in thyroid cancer cells, CB-Dock2 server was applied and the results determined that midazolam had a potential molecular binding with YWHAH and also reduced YWHAH protein expression in thyroid cancer cells. Accumulative studies have well documented that YWHAH expression is increased in thyroid cancer cells and YWHAH acts as an oncogene through participating in thyroid cancer cell biology [11, 12]. Specifically, YWHAH contributes to thyroid cancer malignancy, including proliferation, migration, angiogenesis, along with invasion. As expected, our findings also proved that after YWHAH was silenced, TPC-1 and KTC-1 cell proliferation, migration and invasion were decreased and cell apoptosis was stimulated. Furthermore, the protection against TPC-1 cell proliferation, migration, invasion and the promotion on cell apoptosis imposed by treatment with midazolam were all partially countervailed by elevation of YWHAH, suggesting that midazolam might function in thyroid cancer via downregulating YWHAH.
5 Conclusion
To sum up, midazolam was preliminarily confirmed to exert anti-proliferation, anti-migration, anti-invasion and pro-apoptosis roles in thyroid cancer cells, which might be related to the downregulation of YWHAH. Overall, the paper suggested the inhibitory role of midazolam in the occurrence and progression of thyroid cancer, pointing to the potential of midazolam as an anti-thyroid cancer agent. However, there are some study limitations that need to be taken into account in our future studies. Considering the potential pro-tumorigenic role of midazolam in thyroid cancer in high-dose rats, animal models of thyroid cancer need to be established to further determine whether midazolam plays an anti-carcinogenic or pro-carcinogenic role in thyroid cancer. Besides, the impacts of midazolam on other aggressive phenotypes of thyroid cancer cells including stemness, angiogenesis also demand to be explored. Additionally, YWHAH has been reported to regulate PI3K/Akt signaling pathway in hepatocellular carcinoma [10] and gastric cancer (8). Therefore, whether YWHAH also regulates PI3K/Akt signaling pathway in thyroid cancer also needs to be investigated in further studies.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70(1):7–30.
Miranda-Filho A, Lortet-Tieulent J, Bray F, Cao B, Franceschi S, Vaccarella S, et al. Thyroid cancer incidence trends by histology in 25 countries: a population-based study. Lancet Diabetes Endocrinol. 2021;9(4):225–34.
Boucai L, Zafereo M, Cabanillas ME. Thyroid cancer: a review. JAMA. 2024;331(5):425–35.
Rajan N, Khanal T, Ringel MD. Progression and dormancy in metastatic thyroid cancer: concepts and clinical implications. Endocrine. 2020;70(1):24–35.
Reves JG, Fragen RJ, Vinik HR, Greenblatt DJ. Midazolam: pharmacology and uses. Anesthesiology. 1985;62(3):310–24.
Sethi A, Rezk A, Couban R, Chowdhury T. Role of midazolam on cancer progression/survival—an updated systematic review. Indian J Anaesth. 2023;67(11):951–61.
Aghazadeh Y, Papadopoulos V. The role of the 14-3-3 protein family in health, disease, and drug development. Drug Discov Today. 2016;21(2):278–87.
He J, Zeng F, Jin XI, Liang L, Gao M, Li W, et al. YWHAH activates the HMGA1/PI3K/AKT/mTOR signaling pathway by positively regulating Fra-1 to affect the proliferation of gastric cancer cells. Oncol Res. 2023;31(4):615–30.
Liu B, Li H, Zhou J, Wang L, Fang J, Pu Z, et al. LINC00943 regulates miR-1252-5p/YWHAH axis to promote tumor proliferation and metastasis in lung adenocarcinoma. Heliyon. 2023;9(6): e16736.
Wu Y, Zhang Y, Wang F, Ni Q, Li M. MiR-660-5p promotes the progression of hepatocellular carcinoma by interaction with YWHAH via PI3K/Akt signaling pathway. Biochem Biophys Res Commun. 2020;531(4):480–9.
Ma Y, Yang D, Guo P. Circ_0000144 acts as a miR-1178-3p decoy to promote cell malignancy and angiogenesis by increasing YWHAH expression in papillary thyroid cancer. J Otolaryngol Head Neck Surg. 2022;51(1):28.
Zhou Y, Liu S, Luo Y, Zhang M, Jiang X, Xiong Y. IncRNA MAPKAPK5-AS1 promotes proliferation and migration of thyroid cancer cell lines by targeting miR-519e-5p/YWHAH. Eur J Histochem. 2020. https://doi.org/10.4081/ejh.2020.3177.
Nguyen NM, Meyer D, Meyer L, Chand S, Jagadesan S, Miravite M, et al. Identification of YWHAH as a novel brain-derived extracellular vesicle marker post long-term midazolam exposure during early development. Cells. 2023. https://doi.org/10.3390/cells12060966.
Qi Y, Yao X, Du X. Midazolam inhibits proliferation and accelerates apoptosis of hepatocellular carcinoma cells by elevating microRNA-124-3p and suppressing PIM-1. IUBMB Life. 2020;72(3):452–64.
Liu Y, Yang X, Gan J, Chen S, Xiao ZX, Cao Y. CB-Dock2: improved protein-ligand blind docking by integrating cavity detection, docking and homologous template fitting. Nucleic Acids Res. 2022;50(W1):W159–64.
Jing Y, Zhang Y, Pan R, Ding K, Chen R, Meng Q. Effect of inhalation anesthetics on tumor metastasis. Technol Cancer Res Treat. 2022;21:15330338221121092.
Cata JP, Sood AK, Eltzschig HK. Anesthetic drugs and cancer progression. Anesthesiology. 2020;133(4):698–9.
Jiao B, Yang C, Huang NN, Yang N, Wei J, Xu H. Relationship between volatile anesthetics and tumor progression: unveiling the mystery. Curr Med Sci. 2018;38(6):962–7.
Jiao J, Wang Y, Sun X, Jiang X. Insights into the roles of midazolam in cancer therapy. Evid Based Complement Alternat Med. 2017;2017:3826506.
Zhang X, Han Z, Li Z, Wang T. Midazolam impedes lung carcinoma cell proliferation and migration via EGFR/MEK/ERK signaling pathway. Open Med (Wars). 2023;18(1):20230730.
Lu HL, Wu KC, Chen CW, Weng HK, Huang BM, Lin TY, et al. Anticancer effects of midazolam on lung and breast cancers by inhibiting cell proliferation and epithelial-mesenchymal transition. Life (Basel). 2021. https://doi.org/10.3390/life11121396.
Zhang Y, Zhu Y, Li Y, Ji F, Ge G, Xu H. Midazolam ameliorates acute liver injury induced by carbon tetrachloride via enhancing Nrf2 signaling pathway. Front Pharmacol. 2022;13: 940137.
Sekiguchi R, Yamada KM. Basement membranes in development and disease. Curr Top Dev Biol. 2018;130:143–91.
de Almeida LGN, Thode H, Eslambolchi Y, Chopra S, Young D, Gill S, et al. Matrix metalloproteinases: from molecular mechanisms to physiology, pathophysiology, and pharmacology. Pharmacol Rev. 2022;74(3):712–68.
Morana O, Wood W, Gregory CD. The apoptosis paradox in cancer. Int J Mol Sci. 2022. https://doi.org/10.3390/ijms23031328.
Edlich F. BCL-2 proteins and apoptosis: recent insights and unknowns. Biochem Biophys Res Commun. 2018;500(1):26–34.
Jiao J, Wang Y, Sun X, Jiang X. Midazolam induces A549 cell apoptosis in vitro via the miR-520d-5p/STAT3 pathway. Int J Clin Exp Pathol. 2018;11(3):1365–73.
Oshima Y, Sano M, Kajiwara I, Ichimaru Y, Itaya T, Kuramochi T, et al. Midazolam exhibits antitumour and anti-inflammatory effects in a mouse model of pancreatic ductal adenocarcinoma. Br J Anaesth. 2022;128(4):679–90.
Funding
None.
Author information
Authors and Affiliations
Contributions
Yang Li and Ai-Ping Tan performed the experiments, analyzed the data and wrote the main manuscript text. Yang Li revised the main manuscript text. Yu-Shan Zhong designed the study. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, Y., Tan, AP. & Zhong, YS. Anti-cancer effect of midazolam via downregulating YWHAH in papillary thyroid cancer cells. Discov Onc 16, 72 (2025). https://doi.org/10.1007/s12672-025-01807-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12672-025-01807-w