Abstract
Gout is the most common form of inflammatory arthritis that affects approximately 1% to 6.8% of the global population. Less than half of gout patients received urate-lowering therapy and compliance to the therapy, along with the climbing prevalence, adds a tight burden to public health, not to mention the potential tumor risk incurred by persistent inflammation in the patients. Thus, the study aimed to explore the links between gout, immune responses, and tumor development in terms of genetic alterations. Using RNA-seq data of peripheral blood mononuclear cells (PBMCs) from gout patients, we screened the differentially expressed genes (DEGs) of gout patients and found that they were closely involved in purine metabolism. We then focused on purine metabolism-related DEGs, and machine learning algorithms validated that these genes can help to discriminate gout from healthy conditions. ssGSEA revealed that these DEGs were significantly linked to immune reprogramming concerning fluctuation in the proportion and activity of various immunocytes. Most importantly, they were also partially dysregulated in a wide range of malignancies and exerted a notable influence on the survival of tumor patients, especially LIHC (Liver hepatocellular carcinoma). Therefore, our study made an urgent appeal to due attention to the underlying crosstalk among purine metabolism, immune responses, and tumor development in gout patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Gout, as a disease with a long history, has been associated with the extravagant life of the rich since ancient times. In modern times, with the in-depth study of gout genetics, researchers have gradually unveiled the mystery of this disease, revealing that gout is caused by hyperuricemia due to purine metabolism disorder, which triggers a series of inflammatory reactions and tissue damage [1]. The scientific essence behind the abnormal increase in serum uric acid levels is purine metabolism dysfunction [2]. As metabolic disorders, hyperuricemia and gout present important connections with genetic factors as well as the individual’s lifestyle, eating habits, and environmental factors [3,4,5]. Genomic analyses provide new biomarkers for the early diagnosis and risk assessment of gout and lay theoretical bases for the formulation of individualized treatment strategies [6,7,8,9]. Particularly, genome-wide association studies have revealed several susceptibility genes associated with the onset of gout, such as URAT1, ABCG2, etc. [10, 11]. These genes are executors of uric acid excretion, and their dysfunction denotes the roles of purine metabolism in hyperuricemia and gout pathology.
The crosstalk between purine metabolism and the immune system also draws investigators’ attention. Purines like ATP and NAD not only constitute the key components in cellular energy metabolism but also mediate signal transduction processes, thereby affecting the function of immune cells and the regulation of immune responses in many ways [12,13,14,15,16]. In addition, deficiency of FAMIN (fatty acid metabolism–immunity nexus), a purine metabolic enzyme associated with monogenic Still’s disease, signifies the links between purine metabolism and immune system disorder [17]. The interaction of multiple immune cells and inflammatory factors assembles the complex and varied immune landscape of gout [18,19,20]. In turn, the finely balanced immune regulation mechanism has a profound impact on both the acute onset and chronic progression of gout [6, 20,21,22,23]. Furthermore, purine metabolism reprogramming also fostered tumor immune escape and progression [24,25,26], and a cohort study has reported that gout patients demonstrated higher tumor prevalence and mortality [27,28,29,30]. At the same time, other metabolic diseases that often accompany gout patients, such as obesity, hypertension, and diabetes, may also be associated with an increased risk of tumors [31]. Therefore, delineating the pathophysiological triangle involving purine metabolism, the immune landscape, and the tumor risk of gout will provide new perspectives and strategies for gout flare alleviation and tumor prevention.
Previous documents have reported plenty of differentially expressed genes in gout. Still, the roles of purine metabolism-associated genes in the pathology, especially immune alteration, and the consequently elevated tumor risks remained unclear. Therefore, the study aims to screen the key genes associated with purine metabolism in gout and identify their correlation with immune infiltration and malignant potential in gout patients.
2 Methods
2.1 Data sources
Gene expression of gout patients was downloaded from Gene Expression Omnibus (GEO) (http://www.ncbi.nlm.nih.gov/geo/) with accession number GSE160170. The dataset contains the sequencing data of peripheral blood mononuclear cells (PBMCs) from 6 gout patients and 6 health controls. Gene expressions were detected by Agilent-079487 Arraystar Human LncRNA microarray V4 (Homo sapiens) on GPL21827 platform. Datasets were homogenized using preprocessCore packages in R language. This process aimed to diminish bias raised from oddity samples. R version 4.2.2 was used for all analyses of the article.
We inferred to MSigDB database (https://www.gsea-msigdb.org) for purine metabolism-related genes. Three genesets were obtained, including KEGG_PURINE_METABOLISM (https://www.gsea-msigdb.org/gsea/msigdb/human/geneset/KEGG_PURINE_METABOLISM), REACTOME_PURINE_CATABOLISM (https://www.gsea-msigdb.org/gsea/msigdb/human/geneset/REACTOME_PURINE_CATABOLISM), and WP_PURINE_METABOLISM (https://www.gsea-msigdb.org/gsea/msigdb/human/geneset/WP_PURINE_METABOLISM), and duplicate genes were removed before merging into one gene list. The purine metabolism gene list in the study contained 164 genes.
Expression and survival data of tumoral patients were acquired from the TCGA website (https://www.cancer.gov/ccg/research/genome-sequencing/tcga).
2.2 Screening of differentially expressed genes (DEGs)
DEGs were screened using the linear model for microarray data (LIMMA) package on R. Genes presenting the adjusted P < 0.05 and |logFC|> 0.25 compared between the control and gout cases were defined as significantly differential expressing.
2.3 Gene set enrichment analysis (GSEA)
GSEA was performed twice in the study to firstly investigate the biological functions of DEGs between gout patients and health control, and secondly explore the roles of purine metabolism-related core DEGs, ClusterProfiler package was utilized for functional analyses. The analyses incorporated Gene Ontology (GO) and the Kyoto Encyclopedia of Genes and Genomes (KEGG), and the GO analyses category delineated functional pathways into three aspects including biological processes (BP), molecular functions (MF), and cellular components (CC). The P-value was adjusted using the Benjamini–Hochberg approach or FDR for multiple testing corrections. The threshold was set at FDR < 0.05.
2.4 Selection of core DEGs
In order to screen DEGs involved in purine metabolism, DEGs between gout and control cases were intersected with the purine metabolism-related gene list containing 164 genes, which harvested 33 genes. These genes were again subjected to GSEA before machine learning selection. Next, LASSO (Least Absolute Shrinkage and Selection Operator) analyses were adopted to select key genes from the 33 candidates using the glmnet package on R. LASSO analysis is one of the machine learning methods that can illustrate the trajectories and distributions for each independent variable with respect to lambda. In our analyses, the optimal lambda value was identified to balance model complexity and predictive performance. Receiver operating characteristic (ROC) curves and the area under the curve (AUC) were used to calculate the discrimination efficacy, with the help of pROC package on R. Each gene prediction obtains distinct sensitivities and specificities, and their AUC reflects the strength of the gene in predicting occurrence of the given outcome.
2.5 Immune cell infiltration analysis
The study implemented single-sample gene set enrichment analysis (ssGSEA) to analyze the proportion of 23 types of immunocytes. The analyses were composed of reciprocal relevance between different types of immune cells, differences in immune infiltration between gout patients and healthy controls, and correlation of immune cells with core DEGs.
The ssGSEA (Single Sample Gene Set Enrichment Analysis) function in the GSVA (Gene Set Variation Analysis) package evaluates the degree of association between a single sample and a predefined gene set.
2.6 Construction of regulatory network
Regulator data concerning miRNA and transcriptional factors were obtained from the regnetwork database (https://regnetworkweb.org/) for upstream prediction of core DEGs. The regulatory network was constructed using Cytoscape software.
2.7 Pan-cancer survival analyses
The correlation of the core DEG expression with the overall survival of patients with various cancer types was analyzed using the TIMER2 database (https://cistrome.shinyapps.io/timer/). TIMER (Tumor Immune Estimation Resource) is a comprehensive web resource designed to systematically evaluate the clinical impact of various immune cells in different cancer types. The website provides several modules, including Gene, Survival, Mutation, SCNA (somatic CNA), Diff Exp(differential gene expression), Correlation, and Estimation. In the Survival module, the algorithm calculated the P-value of the log-rank test of groups assigned by users. Also, variables generated by the Cox model were calculated in the output.
2.8 Statistical analyses
All the statistical analyses were performed by R-4.2.2. Heat maps were plotted using the R package “pheatmap”. LASSO analysis was performed by R package “glmnet”. The box and volcano plots were plotted by R package “ggplot2”. For comparisons between the two groups, student’s t-test was performed.
3 Results
3.1 Differentially expressed genes in gout were enriched for purine metabolism
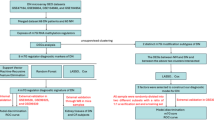
To screen the differentially expressed genes in gout, we obtained a dataset of PBMC from gout patients (GSE160170). The data were homogenous and remained similar before and after homogenization (Fig. 1A, B). We conducted differential analyses between healthy control and gout patients, which returned 1963 upregulated and 3054 downregulated genes (Fig. 1C, D, Supplementary Table 1). Gene Ontology (GO) analyses revealed that the differentially expressed genes (DEGs) intensively participated in purine metabolism as they were enriched for biological process (BP) including the purine nucleotide metabolic process and purine ribonucleotide metabolic process (Fig. 2A). The DEGs also presented strong associations with DNA/RNA biosynthesis-related cellular components (CC, Fig. 2B) and molecular function (MF, Fig. 2C) like nuclear DNA-directed RNA polymerase complex and nucleotidyltransferase activity. KEGG pathway analyses confirmed that components of purine metabolism accounted for a significant part of these DEGs (Fig. 2D). These results indicated that purine metabolism was dysregulated at the transcriptional level.
DEGs between gout patients and health controls. A, B Sample distribution before (A) and after (B) homogenization dataset. The data per se were homogenous as the distribution was identical before and after homogenization. C Volcano plot of DEGs between gout patients and healthy controls. Blue bubbles represented down-regulated genes and red represented up-regulated ones. D A heat map of the DEGs between patients and healthy controls, with red indicating higher expression and blue indicating lower expression. DEGs were ranked by their fold change and only the top 20 upregulated and downregulated candidates were displayed
Enrichment analyses of DEGs. A–C GO analyses of DEGs in aspects of (A) biological process (BP), (B) cellular components (CC), and (C) molecular function (MF). D Results of KEGG analyses concerning DEGs between gout patients and control cases. The color shades represented the P-value, and the size of the circle represented the number of enriched genes
3.2 Dysregulation of purine metabolism was associated with immune responses in gout patients
Therefore, we screened purine metabolism-related genes from the DEGs. We inferred established pathways (KEGG_PURINE_METABOLISM, REACTOME_PURINE_CATABOLISM, and WP_PURINE_METABOLISM) and achieved 164 purine metabolism-related genes. By intersecting these genes with the upregulated and downregulated DEGs, we found 7 upregulated (Fig. 3A) and 26 downregulated (Fig. 3B) purine metabolism-related genes. To explore the roles of these 33 candidates in gout pathology, we performed GO analyses and found their enrichment for mononuclear cell differentiation, lymphocyte differentiation, leukocyte migration, response to virus, and other immune response-related processes (Fig. 3C–E). Similarly, results of KEGG pathway analyses presented that the candidate genes are involved in infections of various pathogens, chemokine signaling, TNF signaling, and other innate and specific immune responses (Fig. 3F).
Screening of purine metabolism-related DEGs and pathway analyses. A Intersection of upregulated DEGs with purine metabolism genes list. B Intersection of downregulated DEGs with purine metabolism genes list. C–E GO annotation of genes from (A) and (B) in aspects of (C) biological process (BP), (D) cellular components (CC), and (E) molecular function (MF). F Results of KEGG analyses concerning intersected DEGs
3.3 Key purine metabolism DEGs discriminate gout from healthy conditions
Next, we sought to determine the key DEGs between health control and gout patients. As shown in Fig. 4A&B, 33 purine metabolism-related DEGs successfully distinguish gout patients from health controls. Most of these genes were downregulated in gout patients, except for ADCY4, NUDT18, NME5, PDE4B, PDE4D, ADK, and POLE3 (Fig. 4C), in accordance with the impaired purine metabolism of gout patients. LASSO regression selected 5 genes from the candidates to signify gout from health controls (Fig. 5A&B), including ADK, DCK, GMPS, NME5, and POLR3D. These crucial DEGs were pairwisely correlated and the downregulated two genes, ADK and NME5, were negatively associated with the other three (Fig. 5C). As validated by the ROC curve, their AUC values reached 1(Fig. 5D), indicating their potential for predicting gout development, which requires further validation in a separate, larger cohort.
DEGs participating in purine metabolism in gout patients. A The differences in expression of the 33 DEGs obtained from the intersection were shown in a volcano plot. B The differences in expression of the 33 DEGs obtained from the intersection were shown in a heatmap. C The differences in expression of the 33 DEGs obtained from the intersection were shown in a box plot. Ns, p > 0.05; *p < 0.05, **p < 0.01, ***p < 0.001
Selection of key DEGs using machine learning. A LASSO analysis of the 33 candidates. B Five key DGEs were selected by LASSO analysis. C The internal correlation of 5 key DEGs. Red bands represented a positive correlation and green bands represented a negative correlation. D ROC curve of 5 genes predicting disease occurrence. The X-axis depicted “1-specificity” and the Y-axis “sensitivity”
3.4 Dysregulated purine metabolism-related genes reflected the immune dysregulation in gout patients
Consequently, we wondered about their influence on gout patients. According to the results of GO functional and KEGG pathway analyses (Fig. 3C–F), dysregulated genes of purine metabolism in gout patients profoundly participated in immunocyte differentiation, pathogen infection, and immune response. We hypothesized that the crucial genes play certain roles in the immunity of gout patients and thus analyzed the immune signature of gout patients. As the effectors of adapted immunity, activated CD8 T cells, monocytes, natural killer T cells, and helper T cells were pairwisely and positively related; on the contrary, activated CD8 T cells were negatively associated with myeloid-derived suppressor cells (MDSC), the well-accepted immunosuppressive cells (Fig. 6A). We compared the proportion of 23 types of immunocytes between health control and gout patients. Activated CD8 T cells, MDSC, monocytes, CD56(bright) natural killer (NK) cells, and helper T cells decreased. In contrast, CD56(dim) NK cells, γδT cells, and TFH (follicular helper) cells increased in the PBMC from gout patients (Fig. 6B). Interestingly, ADK and NME5 were positively correlated with increased immunocytes and negatively with decreased cell types, and vice versa (Fig. 6C). These analyses suggested that purine metabolism dysfunction might influence gout patients’ immunity.
Immune proportion fluctuation of gout patients and its correlation with core DEGs. The internal correlation of immunocytes. Red bubbles presented a positive correlation, blue bubbles presented a negative correlation, and asterisks indicated the significance of the correlation. B Integrated box plots demonstrating differences in immune cell landscape between gout patients and healthy controls. Ns, p > 0.05; *p < 0.05, **p < 0.01, ***p < 0.001. C The correlations between the five core genes and immunocyte signature were shown respectively (immune cells with p < 0.05 were shown). The size of the circle presented a correlation coefficient, and the color represented the P value
In light of this, we examined the association of the crucial DEGs with other genes to inquire into the signaling pathways mediating their functions. As presented in Fig. 7, they were positively correlated to various genes respectively. The top 20 genes with positive correlation were subjected to GSEA. Genes co-expressed with ADK were enriched for expression and translocation of olfactory receptors, and the input genes of most analyses exhibited relevance with processes during DNA/RNA biosynthesis and cell meiosis (Fig. 8). Also, we constructed the regulatory network using the predicted upstream transcriptional factors and miRNAs of the crucial genes (Fig. 9). USF1(Upstream Transcription Factor 1), MYC (MYC Proto-Oncogene, BHLH Transcription Factor), MAX (MYC Associated Factor X), and MXI1 (MAX Interactor 1, Dimerization Protein) were predicted to be the transcriptional factors regulating at least three of them.
Enrichment analyses concerning satellite genes. Based on the results of the correlation analysis in Fig. 7, GSEA results of the top 20 genes related to each core DEG were shown. The values at the bottom represent the enrichment score. A value larger than 0 indicates a positive correlation between the gene and the pathway, and a value smaller than 0 indicates a negative correlation
3.5 Crucial DEGs of gout patients predicted pan-cancer occurrence and prognosis
We continued to investigate if the crucial genes were associated with tumor development by comparing their expression in tumoral and normal tissues from the TCGA database (Fig. 10). Among 33 types of cancers, ESCA (Esophageal carcinoma), HNSC (Head and Neck squamous cell carcinoma), LIHC (Liver hepatocellular carcinoma), LUAD (Lung adenocarcinoma), READ (Rectum adenocarcinoma), and STAD (Stomach adenocarcinoma) demonstrated enhanced expression of the crucial DEGs simultaneously. Utilizing the survival data of the TCGA patients, we analyzed the links between their expression and pan-cancer survival (Fig. 11). The expressions of the crucial DEGs not only elevated in certain tumors but also significantly correlated to the overall survival of the patients, such as ADK in BLCA and GMPS in KICH. Among them, LIHC was noteworthy as it harbored upregulation of all the crucial genes and three of them significantly influence patient prognosis.
Pan-cancer expression of the core genes. Pan-cancer expression of 5 core genes was analyzed using the TIMER2 database (http://timer.comp-genomics.org/timer/)
Pan-cancer survival analyses concerning the core genes. Red indicates that patients with high expression of the indicated gene experienced a poor prognosis, blue indicates that patients with high expression enjoyed a favorable prognosis, and X indicates that the association of gene expression and tumor survival failed to reach statistical significance
4 Discussion
According to our discoveries, DEGs of gout reflected the profound dysfunction of purine metabolism. Core DEGs involved in purine metabolism effectively distinguished gout patients from healthy controls and manifested significant correlations with immune infiltration. Last but not least, pan-cancer analyses uncovered the expression changes of these core DEGs and their association with the overall survival of tumor patients. The study not only notifies the metabolic and immune disorders underlying hyperuricemia and gout but also provides genomic evidence of the tumor risks of gout patients.
Purine dysbolism, arising from the functional deficiency of genes mediating purine synthesis and excretion, is one of the key pathophysiological processes along gout development. For instance, mutations in the PRPS1 gene can lead to increased purine nucleotide synthesis [32,33,34], while mutations in the HPRT1 gene may reduce the salvage pathway of purines [35], both of which can lead to increased serum uric acid levels. Abnormalities in the ABCG2 gene may affect the excretion of uric acid in the kidneys, further aggravating hyperuricemia [36, 37]. Our analyses cast a light on other purine metabolism executors, like GMPS (Guanine Monophosphate Synthase), GART (Glycinamide Ribonucleotide Synthetase-Aminoimidazole Ribonucleotide Synthetase-Glycinamide Ribonucleotide Transformylase), and ADA (Adenosine Deaminase). GMPS catalyzes the oxidation of IMP to GMP in the guanine nucleotide pathway during de novo synthesis of purine nucleotides [38], GART is a trifunctional polypeptide responsible for IMP synthesis [39], and ADA catalyzes the hydrolysis of adenosine to inosine in the purine catabolic pathway [40]. Though seldom reported by previous documents on gout pathology, they were markedly reduced in gout patients compared with healthy controls (Fig. 4). Thus, further investigation into their role in hyperuricemia might broaden our understanding of gout development.
Reduced activity of purine catalysis intertwined with immune disorders to aggravate the disease. First, purine metabolites, especially ATP and adenosine, as signaling molecules, can regulate the activity of immune cells by binding to purine receptors on the surface of immune cells. For example, ATP, as an exogenous nucleotide, can affect the physiological functions of cells, including the regulation of immune cells, by activating specific purine receptors, such as P2 receptors [41]. In addition, abnormal purine metabolism, such as defects in hypoxanthine–guanine phosphoribosyltransferase (HPRT), can lead to excessive purine production and gout, which in turn affects the immune response [42]. In inflammatory responses, purine metabolites such as adenosine can regulate the activation of immune cells, especially T cells, through their anti-inflammatory effects [43]. Adenosine can inhibit the release of inflammatory cytokines and promote the production of anti-inflammatory cytokines, thereby controlling the inflammatory process to a certain extent [44]. Accumulation of urate not only results in hyperuricemia and gouty arthritis but also fosters immune programming [16, 45]. Neutrophils [46], macrophages, and T lymphocytes play a vital role in the inflammatory process of gout [47]. Cytokines such as IL-1β [48] and TNF-α [49] promote gout inflammation, while anti-inflammatory factors such as IL-10 [50] try to alleviate the inflammatory response [21]. Consistently, proportions of immunocytes concerning both innate and acquired immunity were universally changed according to our results (Fig. 6).
The immune reprogramming incited by purine metabolites lays the basis of tumor development upon gout pathophysiology. For example, NAD+ metabolism affects the immune escape ability of tumor cells by regulating the expression of the immune checkpoint PD-L1. By supplementing NAD+ precursors, the sensitivity of tumors to anti-PD-1/PD-L1 antibody treatment can be enhanced, thus providing a new strategy for tumor immunotherapy [51]. An analysis identified that 19 urine metabolites, mainly adenosine and inosine, were packaged in tumor-derived exosomes from head and neck squamous cell carcinoma (HNSCC) patients. Adenosine chief mediated the immune escape of HNSCC cells due to its immunosuppressive roles [52]. In addition, Immune cells and inflammatory factors activated by urate crystals may promote the occurrence and development of tumors. Therefore, the association between gout and tumor risk has gradually become a research hotspot. Some epidemiological studies have shown that the incidence of certain cancers in gout patients is significantly increased, and serum uric acid levels are associated with increased cancer-related mortality [30, 53]. Our analyses expanded the whelm of the field and inquired into the pan-cancer potential among gout patients (Figs. 10, 11). Most cancer types harbored a certain amount of dysregulation concerning key DEGs. Among the five core DEGs, ADK and NME5 were upregulated, while DCK, GMPS, and PLOR3D were downregulated in gout patients. Taking LIHC as an example, ADK was negatively correlated, and the three downregulated DEGs were positively correlated with tumor survival. NME5 showed an insignificant positive association with survival. Genes might exert tumor-specific function during tumorigenesis, and the switch between oncogene and tumor suppressor of gout pathology deserves future validation. The liver is one of the crucial organs responsible for urate regulation [54], and it deserved due alert of tumor development given that all key DEGs were upregulated in the LIHC cohort and some were associated with survival.
5 Limitation
The study conducted analyses on a single cohort with a small size. The key DEGs identified by the study were unpopular among gout research and might require further confirmation through laboratory experiments and validation in a separate, larger cohort. Immune landscape analyses were conducted using the TIMER tool, which might not be suitable for PBMC samples as the algorithm also recognized granulocytes.
6 Conclusion
In all, the study connected the metabolic disorders of gout patients with their immunity reprogramming and tumor risk by mining into the genetic alterations. Declined disposition of purine metabolites influenced immune homeostasis, and both of them led to inclined tumor risk. These findings provide new perspectives for understanding the role of purine metabolism in immune regulation and tumor development. Our analyses screened a list of crucial DEGs that explained the purine dysbolism-immunity disorder-tumor escape cascade and provided potential targets for gout treatment. Future studies need to further explore how these genetic variants interact with environmental factors and how they affect an individual’s susceptibility to gout and the course of the disease. At the same time, immunomodulatory therapy and tumor risk assessment for gout patients will also be important directions for future research. Through these efforts, we look forward to bringing more precise and personalized treatment options to gout patients, improving their quality of life, and reducing the risk of related complications.
Data availability
The sources of data analyzed during the current study are indicated in Materials and methods section.
References
Leask MP, Crisan TO, Ji A, Matsuo H, Kottgen A, Merriman TR. The pathogenesis of gout: molecular insights from genetic, epigenomic and transcriptomic studies. Nat Rev Rheumatol. 2024;20(8):510–23. https://doi.org/10.1038/s41584-024-01137-1.
Toyoda Y, et al. Identification of GLUT12/SLC2A12 as a urate transporter that regulates the blood urate level in hyperuricemia model mice. Proc Natl Acad Sci U S A. 2020;117(31):18175–7. https://doi.org/10.1073/pnas.2006958117.
Li R, et al. Tea consumption is associated with an increased risk of hyperuricemia in an occupational population in Guangdong, China. Int J Gen Med. 2022;15:2747–57. https://doi.org/10.2147/IJGM.S355253.
Zeng L, et al. Multimodal machine learning-based marker enables early detection and prognosis prediction for hyperuricemia. Adv Sci (Weinh). 2024. https://doi.org/10.1002/advs.202404047.
Ding X, et al. Cross-sectional and longitudinal associations of PAHs exposure with serum uric acid and hyperuricemia among Chinese urban residents: the potential role of oxidative damage. Environ Pollut. 2024;360:124664. https://doi.org/10.1016/j.envpol.2024.124664.
Liu YR, Wang JQ, Li J. Role of NLRP3 in the pathogenesis and treatment of gout arthritis. Front Immunol. 2023;14:1137822. https://doi.org/10.3389/fimmu.2023.1137822.
Wang X, et al. Identification of potential biomarkers of gout through weighted gene correlation network analysis. Front Immunol. 2024;15:1367019. https://doi.org/10.3389/fimmu.2024.1367019.
Asiimwe IG, Walker L, Sofat R, Jorgensen AL, Pirmohamed M. Genetic determinants of thiazide-induced hyperuricemia, hyperglycemia, and urinary electrolyte disturbances—a genome-wide evaluation of the UK Biobank. Clin Pharmacol Ther. 2024;115(6):1408–17. https://doi.org/10.1002/cpt.3229.
Zhang M, et al. Atavistic strategy for the treatment of hyperuricemia via ionizable liposomal mRNA. Nat Commun. 2024;15(1):6463. https://doi.org/10.1038/s41467-024-50752-9.
Sandoval-Plata G, Morgan K, Abhishek A. Variants in urate transporters, ADH1B, GCKR and MEPE genes associate with transition from asymptomatic hyperuricaemia to gout: results of the first gout versus asymptomatic hyperuricaemia GWAS in Caucasians using data from the UK Biobank. Ann Rheum Dis. 2021;80(9):1220–6. https://doi.org/10.1136/annrheumdis-2020-219796.
Cho C, et al. Large-scale cross-ancestry genome-wide meta-analysis of serum urate. Nat Commun. 2024;15(1):3441. https://doi.org/10.1038/s41467-024-47805-4.
Han Y, Dong C, Hu M, Wang X, Wang G. Unlocking the adenosine receptor mechanism of the tumour immune microenvironment. Front Immunol. 2024;15:1434118. https://doi.org/10.3389/fimmu.2024.1434118.
Ma Q, et al. Soluble uric acid inhibits beta2 integrin-mediated neutrophil recruitment in innate immunity. Blood. 2022;139(23):3402–17. https://doi.org/10.1182/blood.2021011234.
Wu H, Wang Y, Ren Z, Li Y, Huang J, Lin Z, Zhang B. Overnutrition-induced gout: An immune response to NLRP3 inflammasome dysregulation by XOD activity increased in quail. Front Immunol. 2022;13:1074867. https://doi.org/10.3389/fimmu.2022.1074867.
Chen Y, Liu M, Lu M, Luo L, Han Z, Liu X. Exploring the impact of m(6)A modification on immune diseases: mechanisms and therapeutic implication. Front Immunol. 2024;15:1387582. https://doi.org/10.3389/fimmu.2024.1387582.
Li D, et al. The dysregulation of immune cells induced by uric acid: mechanisms of inflammation associated with hyperuricemia and its complications. Front Immunol. 2023;14:1282890. https://doi.org/10.3389/fimmu.2023.1282890.
Saveljeva S, et al. A purine metabolic checkpoint that prevents autoimmunity and autoinflammation. Cell Metab. 2022;34(1):106–24. https://doi.org/10.1016/j.cmet.2021.12.009.
Yu H, et al. Single-cell transcriptomics reveals variations in monocytes and Tregs between gout flare and remission. JCI Insight. 2023. https://doi.org/10.1172/jci.insight.171417.
Lee KG, Hong BK, Lee S, Lee N, Kim SW, Kim D, Kim WU. Nuclear receptor coactivator 6 is a critical regulator of NLRP3 inflammasome activation and gouty arthritis. Cell Mol Immunol. 2024;21(3):227–44. https://doi.org/10.1038/s41423-023-01121-x.
Gu H, et al. MSU crystal deposition contributes to inflammation and immune responses in gout remission. Cell Rep. 2023;42(10):113139. https://doi.org/10.1016/j.celrep.2023.113139.
Ea HK, et al. Systemic inflammatory cytokine profiles in patients with gout during flare, intercritical and treat-to-target phases: TNFSF14 as new biomarker. Ann Rheum Dis. 2024;83(7):945–56. https://doi.org/10.1136/ard-2023-225305.
Lei Y, Cui TJ, Wang XH, Zhang XM, Tang C, Zheng ZH. Plasma adsorption in refractory chronic gouty arthritis flare: a case report. Front Immunol. 2022;13:1045982. https://doi.org/10.3389/fimmu.2022.1045982.
Abbas AA, Abdulkader HA, Giordo R, Ashour HM, Erre GL, Pintus G, Zayed H. Implications and theragnostic potentials of circular RNAs in rheumatic diseases. Int J Biol Macromol. 2023;235:123783. https://doi.org/10.1016/j.ijbiomac.2023.123783.
Zhao L, et al. Role of N6-methyladenosine in tumor neovascularization. Cell Death Dis. 2024;15(8):563. https://doi.org/10.1038/s41419-024-06931-z.
Yang M, et al. NAD(+) metabolism enzyme NNMT in cancer-associated fibroblasts drives tumor progression and resistance to immunotherapy by modulating macrophages in urothelial bladder cancer. J Immunother Cancer. 2024. https://doi.org/10.1136/jitc-2024-009281.
Xu S, Zhang Y, Yang Y, Dong K, Zhang H, Luo C, Liu SM. A m(6)A regulators-related classifier for prognosis and tumor microenvironment characterization in hepatocellular carcinoma. Front Immunol. 2024;15:1374465. https://doi.org/10.3389/fimmu.2024.1374465.
Hu L, et al. U-shaped association of serum uric acid with all-cause and cause-specific mortality in US adults: a cohort study. J Clin Endocrinol Metab. 2020. https://doi.org/10.1210/clinem/dgz068.
Tambaro FP, Wierda WG. Tumour lysis syndrome in patients with chronic lymphocytic leukaemia treated with BCL-2 inhibitors: risk factors, prophylaxis, and treatment recommendations. Lancet Haematol. 2020;7(2):e168–76. https://doi.org/10.1016/S2352-3026(19)30253-4.
Sasaki K, et al. Prediction of early (4-week) mortality in acute myeloid leukemia with intensive chemotherapy. Am J Hematol. 2022;97(1):68–78. https://doi.org/10.1002/ajh.26395.
Xie Y, et al. Hyperuricemia and gout are associated with cancer incidence and mortality: a meta-analysis based on cohort studies. J Cell Physiol. 2019;234(8):14364–76. https://doi.org/10.1002/jcp.28138.
Battelli MG, Bortolotti M, Polito L, Bolognesi A. Metabolic syndrome and cancer risk: the role of xanthine oxidoreductase. Redox Biol. 2019;21: 101070. https://doi.org/10.1016/j.redox.2018.101070.
Chen P, Li J, Ma J, Teng M, Li X. A small disturbance, but a serious disease: the possible mechanism of D52H-mutant of human PRS1 that causes gout. IUBMB Life. 2013;65(6):518–25. https://doi.org/10.1002/iub.1154.
Porrmann J, et al. Novel PRPS1 gain-of-function mutation in a patient with congenital hyperuricemia and facial anomalies. Am J Med Genet A. 2017;173(10):2736–42. https://doi.org/10.1002/ajmg.a.38359.
Dewulf JP, Marie S, Nassogne MC. Disorders of purine biosynthesis metabolism. Mol Genet Metab. 2022;136(3):190–8. https://doi.org/10.1016/j.ymgme.2021.12.016.
Jang G, et al. Therapeutic gene correction for Lesch-Nyhan syndrome using CRISPR-mediated base and prime editing. Mol Ther Nucleic Acids. 2023;31:586–95. https://doi.org/10.1016/j.omtn.2023.02.009.
Stiburkova B, et al. Functional non-synonymous variants of ABCG2 and gout risk. Rheumatology (Oxford). 2017;56(11):1982–92. https://doi.org/10.1093/rheumatology/kex295.
Hoque KM, et al. The ABCG2 Q141K hyperuricemia and gout associated variant illuminates the physiology of human urate excretion. Nat Commun. 2020;11(1):2767. https://doi.org/10.1038/s41467-020-16525-w.
Zhang P, et al. Dietary intake of fructose increases purine de novo synthesis: a crucial mechanism for hyperuricemia. Front Nutr. 2022;9:1045805. https://doi.org/10.3389/fnut.2022.1045805.
Ng A, Uribe RA, Yieh L, Nuckels R, Gross JM. Zebrafish mutations in gart and paics identify crucial roles for de novo purine synthesis in vertebrate pigmentation and ocular development. Development. 2009;136(15):2601–11. https://doi.org/10.1242/dev.038315.
Cao J, Liu Q, Hao H, Bu Y, Tian X, Wang T, Yi H. Lactobacillus paracasei X11 ameliorates hyperuricemia and modulates gut microbiota in mice. Front Immunol. 2022;13: 940228. https://doi.org/10.3389/fimmu.2022.940228.
Linden J, Koch-Nolte F, Dahl G. Purine release, metabolism, and signaling in the inflammatory response. Annu Rev Immunol. 2019;37:325–47. https://doi.org/10.1146/annurev-immunol-051116-052406.
MacDermot KD, Allsop J, Watts RW. The rate of purine synthesis de nova in blood mononuclear cells in vitro from patients with familial hyperuricaemic nephropathy. Clin Sci (Lond). 1984;67(2):249–58. https://doi.org/10.1042/cs0670249.
Leikeim L, et al. Adenosine signalling in T-cell activation favours development of IL-17 positive cells with suppressive properties. Immunology. 2023;169(1):42–56. https://doi.org/10.1111/imm.13608.
Hasko G, Pacher P, Deitch EA, Vizi ES. Shaping of monocyte and macrophage function by adenosine receptors. Pharmacol Ther. 2007;113(2):264–75. https://doi.org/10.1016/j.pharmthera.2006.08.003.
Cabau G, Crisan TO, Kluck V, Popp RA, Joosten LAB. Urate-induced immune programming: consequences for gouty arthritis and hyperuricemia. Immunol Rev. 2020;294(1):92–105. https://doi.org/10.1111/imr.12833.
Mitroulis I, Kambas K, Ritis K. Neutrophils, IL-1beta, and gout: is there a link? Semin Immunopathol. 2013;35(4):501–12. https://doi.org/10.1007/s00281-013-0361-0.
Antonioli L, Pacher P, Hasko G. Adenosine and inflammation: it’s time to (re)solve the problem. Trends Pharmacol Sci. 2022;43(1):43–55. https://doi.org/10.1016/j.tips.2021.10.010.
Renaudin F, et al. Gout and pseudo-gout-related crystals promote GLUT1-mediated glycolysis that governs NLRP3 and interleukin-1beta activation on macrophages. Ann Rheum Dis. 2020;79(11):1506–14. https://doi.org/10.1136/annrheumdis-2020-217342.
Diaz-Torne C, et al. The inflammatory role of silent urate crystal deposition in intercritical gout. Rheumatology (Oxford). 2021;60(11):5463–72. https://doi.org/10.1093/rheumatology/keab335.
Jeong JH, et al. CD14(+) cells with the phenotype of infiltrated monocytes consist of distinct populations characterized by anti-inflammatory as well as pro-inflammatory activity in gouty arthritis. Front Immunol. 2017;8:1260. https://doi.org/10.3389/fimmu.2017.01260.
Lv H, et al. NAD(+) metabolism maintains inducible PD-L1 expression to drive tumor immune evasion. Cell Metab. 2021;33(1):110–27. https://doi.org/10.1016/j.cmet.2020.10.021.
Ludwig N, Gillespie DG, Reichert TE, Jackson EK, Whiteside TL. Purine metabolites in tumor-derived exosomes may facilitate immune escape of head and neck squamous cell carcinoma. Cancers (Basel). 2020. https://doi.org/10.3390/cancers12061602.
Chen YH, et al. Spontaneous resolution of acute gouty arthritis is associated with rapid induction of the anti-inflammatory factors TGFbeta1, IL-10 and soluble TNF receptors and the intracellular cytokine negative regulators CIS and SOCS3. Ann Rheum Dis. 2011;70(9):1655–63. https://doi.org/10.1136/ard.2010.145821.
Major TJ, Dalbeth N, Stahl EA, Merriman TR. An update on the genetics of hyperuricaemia and gout. Nat Rev Rheumatol. 2018;14(6):341–53. https://doi.org/10.1038/s41584-018-0004-x.
Funding
The study was supported by the Guangdong Natural Science Foundation (No.2022A1515110656), and the President’s Fund of Nanfang Hospital, Southern Medical University, Project 2022A034.
Author information
Authors and Affiliations
Contributions
Conceptualization: Wei-nan Lai and Lu-shan Xiao; Data acquisition and processing: Lin-na Li; Interpretation of Results: Lin-na Li and Hao Wang; Writing-original draft: Lin-na Li; Writing-review and editing: Lin-na Li, Hao Wang and Lushan Xiao, Wei-nan Lai. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, Ln., Wang, H., Xiao, Ls. et al. Purine metabolism-associated key genes depict the immune landscape in gout patients. Discov Onc 16, 193 (2025). https://doi.org/10.1007/s12672-025-01956-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12672-025-01956-y