Abstract
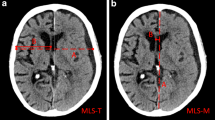
Meningeal lymphatic vessels (mLVs) were recently discovered to be involved in the waste drainage process in the brain, which has also been associated with a variety of neurological diseases. This research paper hypothesizes that the drainage function of mLVs may be affected after chronic subdural hematoma (CSDH) and the alterations of mLVs’ drainage may predict CSDH recurrence. In this prospective observational study, unenhanced 3D T2-fluid-attenuated inversion recovery (3D T2-FLAIR) MRI data were collected from CSDH patients and healthy participants for analysis. Patients with CSDH who underwent surgery received MRI scans before and after surgery, whereas healthy controls and patients with CSDH who received pharmaceutical treatment received only one MRI scan at enrollment. The signal unit ratio (SUR) of mLVs were then measured according to the MRI data and calculated to define mLVs’ drainage function. Finally, the relationship between mLVs’ drainage function and CSDH recurrence was analyzed accordingly. Thirty-four participants were enrolled in this study, including 27 CSDH patients and 7 controls. The SUR of mLVs in all CSDH patients changed significantly before and after surgery. Moreover, the drainage function of the mLVs ipsilateral to hematoma (mLVs-IH) in CSDH patients was significantly lower than that in the controls (p < 0.05). Last, a higher improvement rate of the drainage function of the mLVs-IH is correlated to a lower risk of recurrence (p < 0.05). This study revealed the mLVs’ drainage dysfunction after CSDH through non-invasive MRI. Furthermore, the drainage function of mLVs is an independent predictive factor of CSDH recurrence.




Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Abbreviations
- AUC:
-
Area under the curve
- CFS:
-
Clinical frailty score
- CSDH:
-
Chronic subdural hematoma
- dCLV:
-
Deep cervical lymph vessel
- GCS:
-
Glasgow Coma Scale
- ICC:
-
Interclass correlation coefficient
- Lo-mLVs:
-
Lower mLVs
- mLVs:
-
Meningeal lymphatic vessels
- mLVs-CH:
-
mLVs contralateral to hematoma
- mLVs-IH:
-
mLVs ipsilateral to hematoma
- MRI:
-
Magnetic resonance imaging
- MRS:
-
Modified Rankin scale
- ROC:
-
Receiver operating characteristic
- SSS:
-
Superior sagittal sinus
- SUR:
-
Signal unit ratio
- dCLNs:
-
Deep cervical lymphatic nodes
- T2-FLAIR:
-
T2-fluid-attenuated inversion recovery
- TBI:
-
Traumatic brain injury
References
Du B, Xu J, Hu J, Zhong X, Liang J, Lei P, Wang H, Li W, Peng Y, Shan A, et al. A clinical study of the intra-neuroendoscopic technique for the treatment of subacute-chronic and chronic septal subdural hematoma. Front Neurol. 2019;10:1408.
Rauhala M, Helén P, Huhtala H, Heikkilä P, Iverson GL, Niskakangas T, Öhman J, Luoto TM. Chronic subdural hematoma-incidence, complications, and financial impact. Acta Neurochir (Wien). 2020;162(9):2033–43.
Scerrati A, Visani J, Ricciardi L, Dones F, Rustemi O, Cavallo MA, De Bonis P. To drill or not to drill, that is the question: nonsurgical treatment of chronic subdural hematoma in the elderly. A systematic review. Neurosurg Focus. 2020;49(4):E7.
Hutchinson PJ, Edlmann E, Bulters D, Zolnourian A, Holton P, Suttner N, Agyemang K, Thomson S, Anderson IA, Al-Tamimi YZ, et al. Trial of dexamethasone for chronic subdural hematoma. N Engl J Med. 2020;383(27):2616–27.
Kolias AG, Chari A, Santarius T, Hutchinson PJ. Chronic subdural haematoma: modern management and emerging therapies. Nat Rev Neurol. 2014;10(10):570–8.
Dinsmore J, Wiles MD. Surgical management of chronic subdural haematoma: looking beyond anaesthetic technique. Anaesthesia. 2022;77(5):519–22.
Stanisic M, Lyngstadaas SP, Pripp AH, Aasen AO, Lindegaard K-F, Ivanovic J, Ilstad E, Konglund A, Sandell T, Ellingsen O, et al. Chemokines as markers of local inflammation and angiogenesis in patients with chronic subdural hematoma: a prospective study. Acta Neurochir (Wien). 2012;154(1)
Pripp AH, Stanišić M. The correlation between pro- and anti-inflammatory cytokines in chronic subdural hematoma patients assessed with factor analysis. PLoS One. 2014;9(2):e90149.
Ding X-B, Wang X-X, Xia D-H, Liu H, Tian H-Y, Fu Y, Chen Y-K, Qin C, Wang J-Q, Xiang Z, et al. Impaired meningeal lymphatic drainage in patients with idiopathic Parkinson’s disease. Nat Med. 2021;27(3):411–8.
Ahn JH, Cho H, Kim J-H, Kim SH, Ham J-S, Park I, Suh SH, Hong SP, Song J-H, Hong Y-K, et al. Meningeal lymphatic vessels at the skull base drain cerebrospinal fluid. Nature. 2019;572(7767):62–6.
Da Mesquita S, Fu Z, Kipnis J. The meningeal lymphatic system: a new player in neurophysiology. Neuron. 2018;100(2):375–88.
Da Mesquita S, Louveau A, Vaccari A, Smirnov I, Cornelison RC, Kingsmore KM, Contarino C, Onengut-Gumuscu S, Farber E, Raper D, et al. Functional aspects of meningeal lymphatics in ageing and Alzheimer’s disease. Nature. 2018;560(7717):185–91.
Chen J, Wang L, Xu H, Xing L, Zhuang Z, Zheng Y, Li X, Wang C, Chen S, Guo Z, et al. Meningeal lymphatics clear erythrocytes that arise from subarachnoid hemorrhage. Nat Commun. 2020;11(1):3159.
Bolte AC, Dutta AB, Hurt ME, Smirnov I, Kovacs MA, McKee CA, Ennerfelt HE, Shapiro D, Nguyen BH, Frost EL, et al. Meningeal lymphatic dysfunction exacerbates traumatic brain injury pathogenesis. Nat Commun. 2020;11(1):4524.
Absinta M, Ha S-K, Nair G, Sati P, Luciano NJ, Palisoc M, Louveau A, Zaghloul KA, Pittaluga S, Kipnis J, et al. Human and nonhuman primate meninges harbor lymphatic vessels that can be visualized noninvasively by MRI. Elife. 2017;6
Zhou Y, Cai J, Zhang W, Gong X, Yan S, Zhang K, Luo Z, Sun J, Jiang Q, Lou M. Impairment of the glymphatic pathway and putative meningeal lymphatic vessels in the aging human. Ann Neurol. 2020;87(3):357–69.
Ringstad G, Eide PK. Cerebrospinal fluid tracer efflux to parasagittal dura in humans. Nat Commun. 2020;11(1):354.
Albayram MS, Smith G, Tufan F, Tuna IS, Bostancıklıoğlu M, Zile M, Albayram O. Non-invasive MR imaging of human brain lymphatic networks with connections to cervical lymph nodes. Nat Commun. 2022;13(1):203.
Liu X, Gao C, Yuan J, Xiang T, Gong Z, Luo H, Jiang W, Song Y, Huang J, Quan W, et al. Subdural haematomas drain into the extracranial lymphatic system through the meningeal lymphatic vessels. Acta Neuropathol Commun. 2020;8(1):16.
Gao C, Wei Y, Zhang X, Huang J, Nie M, Liu X, Yuan J, Wang D, Tian Y, Jiang W, et al. Craniocervical manual lymphatic drainage increases the efficiency of atorvastatin-based treatment of chronic subdural hematoma. Transl Stroke Res. 2023;14(5):667–677.
Gregorevic KJ, Hubbard RE, Lim WK, Katz B. The clinical frailty scale predicts functional decline and mortality when used by junior medical staff: a prospective cohort study. BMC Geriatr. 2016;16:117.
Bartley A, Bartek J, Jakola AS, Sundblom J, Fält M, Förander P, Marklund N, Tisell M. Effect of irrigation fluid temperature on recurrence in the evacuation of chronic subdural hematoma: a randomized clinical trial. JAMA Neurol. 2023;80(1):58–63.
Feghali J, Yang W, Huang J. Updates in chronic subdural hematoma: epidemiology, etiology, pathogenesis, treatment, and outcome. World Neurosurg. 2020;141:339–45.
Jiang R, Zhao S, Wang R, Feng H, Zhang J, Li X, Mao Y, Yuan X, Fei Z, Zhao Y, et al. Safety and efficacy of atorvastatin for chronic subdural hematoma in Chinese patients. A randomized clinicaltrial. JAMA Neurol. 2018;75(11):1338–46.
Wang X, Zhang A, Yu Q, Wang Z, Wang J, Xu P, Liu Y, Lu J, Zheng J, Li H, et al. Single-cell RNA sequencing and spatial transcriptomics reveal pathogenesis of meningeal lymphatic dysfunction after experimental subarachnoid hemorrhage. Adv Sci (Weinh). 2023;10(21):e2301428.
Zhou Y, Ran W, Luo Z, Wang J, Fang M, Wei K, Sun J, Lou M. Impaired peri-olfactory cerebrospinal fluid clearance is associated with ageing, cognitive decline and dyssomnia. EBioMedicine. 2022;86:104381.
Lindvall P, Koskinen L-OD. Anticoagulants and antiplatelet agents and the risk of development and recurrence of chronic subdural haematomas. J Clin Neurosci. 2009;16(10):1287–90.
Sarker A, Suh M, Choi Y, Park JY, Lee Y-S, Lee DS. Intrathecal [64Cu]Cu-albumin PET reveals age-related decline of lymphatic drainage of cerebrospinal fluid. Sci Rep. 2023;13(1):12930.
Rustenhoven J, Pavlou G, Storck SE, Dykstra T, Du S, Wan Z, Quintero D, Scallan JP, Smirnov I, Kamm RD, et al. Age-related alterations in meningeal immunity drive impaired CNS lymphatic drainage. J Exp Med. 2023;220(7)
Hos D, Bachmann B, Bock F, Onderka J, Cursiefen C. Age-related changes in murine limbal lymphatic vessels and corneal lymphangiogenesis. Exp Eye Res. 2008;87(5):427–32.
Yang Y, Wang X, Wang P. Signaling mechanisms underlying lymphatic vessel dysfunction in skin aging and possible anti-aging strategies. Biogerontology. 2023;24(5):727–40.
Huang Y-H, Lin W-C, Lu C-H, Chen W-F. Volume of chronic subdural haematoma: is it one of the radiographic factors related to recurrence? Injury. 2014;45(9):1327–31.
Jensen TSR, Andersen-Ranberg N, Poulsen FR, Bergholt B, Hundsholt T, Fugleholm K. The Danish chronic subdural hematoma study—risk factors for second recurrence. World Neurosurg. 2022;168:e178–86.
Edlmann E, Giorgi-Coll S, Whitfield PC, Carpenter KLH, Hutchinson PJ. Pathophysiology of chronic subdural haematoma: inflammation, angiogenesis and implications for pharmacotherapy. J Neuroinflammation. 2017;14(1):108.
Acknowledgements
We are grateful for the data support from the Second Affiliated Hospital, School of Medicine, Zhejiang University.
Funding
This study was supported by the National Natural Science Foundation of China (82371300, to SC), the National Natural Science Foundation of China (82201430, to YJF), the National Natural Science Foundation of China (82270823, to QW), the Zhejiang Provincial Natural Science Foundation of China (LY23H090014, to SC), and the Medical Health Science and Technology Project of Zhejiang Provincial Health Commission (WKJ-ZJ-2427, to SC).
Author information
Authors and Affiliations
Contributions
JHZ wrote the manuscript; SC, JZS, and WQ designed the manuscript; JHZ, LY, ZYZ, and XYW collected the study data; YJF, QY, HML, BRZ, and AKZ revised the manuscript; YBL, HCZ, KKW, and YZH participated in the design and coordination of the study. All authors read and approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethical Approval and Consent to Participate
Our study complies with the Declaration of Helsinki that the local ethics committee has approved the research protocol. All patients or their legally authorized representative signed a written informed consent.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
Supplemental Fig. 1 MRI image of patient NO.27 (A1, A2) are the two adjacent MRI images of patient NO.27 before treatment; (A3, A4) are the two adjacent MRI images of patient NO.27 after treatment. Supplemental Fig. 2 Relationship between outcome and suspicious factors. (a-d) Relationship between recurrence and suspicious (n=22); (e-f) Relationship between percentage change of SUR and prognostic scores (n=22). SUR: signal unit ratio. (DOCX 643 kb)
ESM 2
(DOCX 15 kb)
ESM 3
Supplemental Table 1 Basic clinical data of all subjects. (DOCX 25 kb)
ESM 4
Supplemental Table 2 The SUR of all patients. (DOCX 17 kb)
ESM 5
Supplemental Table 3 The SUR of all controls. (DOCX 15 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, J., Yu, L., Wang, X. et al. The Drainage Dysfunction of Meningeal Lymphatic Vessels Is Correlated with the Recurrence of Chronic Subdural Hematoma: a Prospective Study. Transl. Stroke Res. 16, 438–447 (2025). https://doi.org/10.1007/s12975-023-01227-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-023-01227-4