Abstract
Background and Objectives
Penicillin/beta-lactamase inhibitors are often used to treat aspiration pneumonia in patients resuscitated after cardiac arrest (CA). The impact of hypothermic temperature control on the pharmacokinetics of amoxicillin/clavulanate (AMO/CLAV) and ampicillin/sulbactam (AMP/SULB) has not been studied. Our objective was to evaluate the effects of hypothermic temperature control on the plasma and soft tissue pharmacokinetics of AMO/CLAV and AMP/SULB, including pulmonary concentrations of AMP/SULB, in patients resuscitated after CA.
Methods
This prospective clinical study involved ten adult patients after CA receiving either AMO/CLAV 2 g/0.2 g or AMP/SULB 2 g/1 g intravenously every 8 h. Patients underwent hypothermic temperature control (33 ± 1 °C) for 24 h, followed by normothermia. Plasma, urine, muscle, and subcutaneous pharmacokinetics were measured and plasma protein-binding assessed for each subject. Microdialysis determined unbound drug concentrations in soft tissues. The pulmonary concentration of AMP/SULB was analyzed in the epithelial lining fluid.
Results
No significant differences in plasma pharmacokinetics or renal excretion of AMO/CLAV and AMP/SULB were observed between the two temperature conditions. Soft tissue concentrations showed no consistent trend. Pharmacokinetic/pharmacodynamic targets (time that the unbound plasma concentrations were above the minimal inhibitory concentration [MIC] for MIC up to 8 mg/L) were met but not for 16 mg/L. Pulmonary concentrations of AMP/SULB in the epithelial lining fluid showed no clear trend.
Conclusion
This study indicates that hypothermic temperature control does not significantly affect plasma concentrations, soft tissue concentrations, or renal excretion of AMO/CLAV and AMP/SULB in patients resuscitated after CA. However, pulmonary concentrations of AMP/SULB exhibited interindividual variability.
Graphical Abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Avoid common mistakes on your manuscript.
Hypothermic temperature control did not significantly alter plasma or soft tissue pharmacokinetics of amoxicillin/clavulanate or ampicillin/sulbactam. |
Pharmacokinetic/pharmacodynamic targets (including time that the unbound plasma concentrations were above the minimal inhibitory concentration) were met for minimal inhibitory concentrations up to 8 mg/L but not for 16 mg/L. |
Pulmonary concentrations of ampicillin/sulbactam in epithelial lining fluid showed interindividual variability. |
1 Introduction
Sudden cardiac arrest (CA), particularly out-of-hospital CA remains a major global health issue and a leading cause of adult death [1]. In Europe, resuscitation attempts average 56 per 100,000 individuals annually, but survival rates to hospital discharge are only around 10% [2].
Current joint guidelines from the European Resuscitation Council and the European Society of Intensive Care Medicine recommend continuous core temperature monitoring and fever prevention (> 37.7 °C) for at least 72 h in comatose patients after return of spontaneous circulation (ROSC). The ideal temperature target is debated and ranges from 32 to 36 °C or fever prevention above 37.7 °C [3, 4]. If initiated early after ROSC, hypothermic temperature control with a target of 32–34 °C primarily acts by lowering metabolic demand in ischemic tissue and can reduce cerebral reperfusion injury in comatose patients after CA [4, 5].
However, hypothermia can alter peripheral blood flow and organ metabolism, potentially affecting drug pharmacokinetics, making standard dosing less effective [6].
Early-onset and ventilator-associated pneumonia are common complications in survivors of CA admitted to the intensive care unit (ICU). Although post-ROSC hypothermia can dampen inflammatory responses, it may increase lung susceptibility to infections, potentially contributing to a greater pneumonia risk [7].
Empiric treatments for early-onset pneumonia in intubated survivors of CA often include broad-spectrum penicillin/beta-lactamase inhibitors such as amoxicillin/clavulanate (AMO/CLAV) and ampicillin/sulbactam (AMP/SULB) [8, 9]. In clinical practice, empiric antibiotics are frequently started early in cooled survivors of CA to prevent aspiration pneumonia, although European guidelines recommend antibiotics only when pneumonia is confirmed [10]. A trial showed that early prophylactic antibiotics in survivors of CA under hypothermic temperature control reduced early ventilator-associated pneumonia but not mortality [9]. Consequently, the American Heart Association and Neurocritical Care Society recommend early, short-term antibiotic prophylaxis [11].
Microdialysis is often used to measure unbound drug concentrations in tissues such as plasma, muscles, and subcutaneous tissue [12, 13]. Although a comprehensive understanding of plasma and tissue pharmacokinetics of commonly used antibiotics under normothermic conditions has been obtained, their pharmacokinetic behavior during hypothermia in resuscitated adults remains largely unexplored [14,15,16,17,18]. Understanding tissue pharmacokinetics of antibiotics is key for optimizing treatment in critically ill patients, as altered renal and liver function, capillary leakage, and hypoalbuminemia all affect drug distribution and clearance. Adequate drug levels at infection sites are crucial for effective treatment and preventing resistance, especially in patients in the ICU who require adjusted dosing [19].
This study aimed to investigate the pharmacokinetic profiles of AMO/CLAV and AMP/SULB in the plasma, muscle, subcutaneous adipose tissue, urine, and epithelial lining fluid (ELF) of patients resuscitated after CA during hypothermia and normothermia.
2 Material and Methods
2.1 Ethics
This prospective, open-labelled, single-center study was approved by the ethics committee of the Medical University of Vienna (EC: 1348/2015) and the Austrian Agency for Health and Food Safety. It was registered at the European Union Drug Regulating Authorities Clinical Trials Database (EUDRACT 2015-001793-18) and conducted according to International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use good clinical practice guidelines and the Declaration of Helsinki. Since the participants were unconscious, consent was obtained from survivors once they could understand the study. The treating team informed patients’ relatives about their inclusion in the study, but the ethics committee did not mandate this as a requirement. The study procedures were conducted at the Department of Emergency Medicine (ED) and the ICU at the Medical University of Vienna from April 2016 to June 2022.
2.2 Study Population and Procedure
We included comatose, intubated patients aged ≥18 years who experienced witnessed CA of any rhythm, were eligible for hypothermic temperature control, and received AMO/CLAV or AMP/SULB for suspected or confirmed aspiration pneumonia. Exclusion criteria included pregnancy, unwitnessed CA, non-sustained ROSC, body mass index (BMI) outside the range of 18–40 kg/m2, significant coagulopathies or hemorrhagic conditions (platelet count < 50 G/L), a glomerular filtration rate < 50 mL/min/1.73 m2, advanced malignancies, terminal illnesses, or signs of impending clinical deterioration.
All patients underwent the same procedures during two study phases: the hypothermic phase and the subsequent normothermic phase. During each study period, plasma, microdialysate, and urine were collected at predetermined intervals after antibiotic steady state. In the AMP/SULB group, bronchial mucosa ELF was collected in both phases.
2.2.1 Hypothermic Temperature Control
Hypothermic temperature control procedures followed ED guidelines targeting 33 ± 1 °C for 24 h after sustained ROSC, followed by rewarming at 0.5 °C/h [20]. Normothermia (36.5 ± 1 °C) was maintained for at least 72 h using physical or pharmacological methods. Cooling was achieved noninvasively with Arctic Sun® 5000 (Bard Medical Division, C.R. Bard, Inc., Louisville, CO, USA) or external surface cooling pads (EMCOOL-Spad®, EMCOOLS AG, Pfaffstaetten, Austria, and TTcool-pad 302, Everynear GmbH, Baden, Austria) or invasively with Thermogard®XP (ZOLL Medical, Cologne; Germany). Body temperature was monitored with an esophageal temperature probe.
2.2.2 Study Medication
Patients received either 2 g amoxicillin/0.2 g clavulanate (Curam® 2.2 g powder for infusion solution, Sandoz GmbH, Vienna, Austria) or 2 g ampicillin/1 g sulbactam (Unasyn 3g Dry Vials®, Pfizer Corporation Austria Ges.m.b.H, Vienna, Austria). Antibiotics were prepared in 100 mL 0.9% saline solution (physiological saline solution “Fresenius”- Infusions Solution, Fresenius Kabi Austria GmbH., Graz, Austria) and administered via infusion pump intravenously over 15 min every 8 h. The line was flushed with 50 mL 0.9% saline after infusion. Antibiotics were given at least twice before sampling to ensure steady-state conditions.
2.2.3 Clinical Pneumonia Surveillance
C-reactive protein levels (normal: \(\le \hspace{0.17em}\)0.49 mg/dL) were measured daily. Chest X-rays or computed tomography scans were performed at the physician’s discretion, and pneumonia signs were evaluated by the attending radiologist.
2.3 Sampling
2.3.1 Plasma Sampling
Blood samples (4 mL) were collected via an arterial catheter into lithium–heparin tubes. To measure total drug concentrations in plasma, samples were drawn at baseline (before the next antibiotic administration) and at 0.5, 1, 1.5, 2, 3, 4, and 6 h after start of drug infusion. The sample collection schedule was identical for both study periods. Samples were refrigerated immediately, centrifuged at + 4 °C, 2600g, 10 min, and the plasma was frozen at − 20 °C within 1 h.
2.3.2 Urine Sampling
Urine was collected at 0–2, 2–4, and 4–6 h after drug administration. About 5 mL per sample was refrigerated and frozen at − 20 °C within 1 h.
2.3.3 Bronchoalveolar Lavage, ELF Collection
To investigate antibiotic distribution in the bronchial mucosa, ELF was collected via bronchoscopy from endotracheally intubated patients. This procedure was conducted exclusively in the AMP/SULB group as part of an exploratory approach to assess target site antibiotic penetration. A single bronchoalveolar lavage (BAL) was performed at 2, 4, or 6 h after starting antibiotic administration during each study period. Up to three 20 mL saline aliquots were instilled and aspirated. BAL samples were mixed, filtered, and centrifuged at 2000g, 4 °C, 10 min, and the supernatant was frozen at − 20 °C within 1 h.
Bronchoscopies were performed using a flexible video bronchoscope (EB-1970K by Pentax©, HOYA Corporation, Tokyo, Japan). To determine the dilution factor of ELF in BAL, the urea method was applied as described previously [21].
2.3.4 Microdialysis
In the present study, two microdialysis probes were inserted into one of the patient’s thighs. The microdialysis catheters (63 Microdialysis Catheter 60/10, M Dialysis AB, Solna, Sweden) with a membrane length of 10 mm and a molecular weight cut-off of 20 kDa, were inserted into the subcutaneous adipose tissue and into the quadriceps muscle. Throughout the entire study (both sampling periods), microdialysis probes were perfused with 0.9% saline solution at a flow rate of 2 µL/min. Following an equilibration period of 30 min, microdialysis samples were collected at baseline (before antibiotic drug administration) and at 0–1, 1–2, 3–4, 4–5, and 5–6 h after drug administration. All microdialysis samples were immediately placed in a portable refrigerator box and frozen at − 20 °C within 1 h from collection.
After the last sample of each study day, each probe was calibrated using the retrodialysis method to calculate the concentration in the interstitial space fluid, as previously described [22]. For this part of the experiment, the perfusion medium for calibration contained a known concentration of the respective antibiotics and beta-lactamase inhibitor, and the relative loss rate was determined.
2.3.5 Sample Handling and Storage
At the end of the study day, plasma, microdialysate, ELF, and urine samples were transferred from − 20 °C to − 80 °C and stored at − 80 °C until analysis.
2.3.6 Sample Analysis: High-Performance Liquid Chromatography Method and Ultrafiltration
The high-performance liquid chromatography equipment consisted of a Shimadzu Prominence modular system with a three-channel degasser (DGU 20A3R), quaternary solvent pump (LC 20AD), autosampler (SIL 20AC HT, set to 6 °C), column oven (CTO 20AC, set to 40 °C), photodiode array detector (SPD M30A, detection wavelengths: AMP/SULB 205 nm, AMO 227 nm, CLAV 215 nm) equipped with cells of 10 mm or 85 mm optical path length, system controller CBM 20A, and LabSolution software (all from Shimadzu Europe, Duisburg, Germany). The flow rate was 0.4 mL/min, and the injection volume was 1–2 µL, for BAL 5 µL. Separation was performed isocratically using a Cortecs T3 2.7 µ 100 × 3 mm analytical column (Waters, Eschborn, Germany) preceded by a guard column (Nucleoshell RP18 2.7 µ 4 × 3 mm, Macherey-Nagel, Düren, Germany). The mobile phase consisted of 0.1 M sodium phosphate buffer/acetonitrile 90:10 (v/v), pH 3.1, for the determination of AMP/SULB, and 97:3 (v/v), pH 3.3, for the determination of AMO/CLAV. SULB and CLAV were eluted after 2.1 min, AMP and AMO after 4.2 min.
Total drug concentrations were analyzed according to a published protocol [23]. In brief, serum (100 µL) was buffered with 25 mM sodium phosphate buffer (pH 6.0, 200 µL) and deproteinized with acetonitrile (500 µL). The precipitated protein was separated by centrifugation, the acetonitrile was extracted into dichloromethane (1.5 mL), and an aliquot of the aqueous layer was injected. The free concentrations were measured using a published ultrafiltration method [24]. In brief, plasma (300 µL) was mixed with 10 µL potassium phosphate (3M, pH 7.43 ± 0.02) in a Vivafree™ 500 30 kD Hydrosart® centrifugal ultrafiltration device (Vivaproducts Inc., Littleton, MA, USA) before ultrafiltration at 37 °C. Microdialysate or BAL were injected directly, and urine after dilution 1:50 with 10 mM sodium phosphate buffer, pH 6.0.
The lower limit of quantification (LLOQ) for AMP/SULB and AMO/CLAV was 0.3/0.5 and 0.3/0.2 mg/L, respectively, in plasma, and 0.03/0.05 and 0.03/0.02 mg/L, respectively, in saline, which was used as a surrogate for the other matrices. Based on in-process quality controls (high/low), the relative standard deviation (SD) for precision was < 3%/≤ 7% for AMP/SULB and < 3%/< 5% for AMO/CLAV, respectively; the inaccuracy was < 3% for all substances. The estimated LLOQ (signal-to-noise ratio = 5) in BAL (injection volume 5 µL) was 0.02/0.01 for AMP/SULB and 0.01/0.01 mg/L for AMO/CLAV; the LLOQ in urine was estimated at < 30/50 and < 30/20 mg/L, respectively. The accuracy of the determination of free drug in plasma cannot be specified, as the extent of protein binding in a particular sample is not known. The precision was assessed by analyzing spiked pooled plasma of healthy subjects; in these samples, the mean ± SD unbound fraction of AMP/SULB and AMO/CLAV was 80.6 ± 6.9%/91.7 ± 6.9% and 87.3 ± 1.9%/81.7 ± 3.4%, respectively.
2.4 Pharmacokinetic Analysis
The pharmacokinetic data were analyzed using Phoenix® WinNonlin® Build 8.0 (Certara USA, Inc., Princeton, NJ, USA). We employed a non-compartmental analysis for this study to determine the pharmacokinetic parameters.
2.4.1 Plasma Protein Binding
Plasma protein binding was assessed for each subject at three distinct timepoints using ultrafiltration. Mean plasma protein binding per subject was used to calculate unbound drug concentrations, which were used for pharmacokinetic analysis.
2.4.2 Pharmacokinetic Parameters
We determined key plasma pharmacokinetic parameters, including maximum plasma concentration, elimination half-life, apparent volume of distribution, total body clearance, and area under the concentration–time curve from 0 to 6 h.
We also calculated the duration that unbound plasma concentrations exceeded the minimal inhibitory concentration [MIC] (fT>MIC) for AMO and AMP, using MIC values of 4 mg/L, 8 mg/L, and 16 mg/L, representing the upper range for relevant pathogens per European Committee on Antimicrobial Susceptibility Testing MIC distributions [25]. Calculations of the fT>MIC were based on the individual concentrations from each study subject.
2.4.3 Exposure Comparison
To compare drug exposure between the normothermic and hypothermic states, we calculated concentration ratios (individual concentration at each timepoint in normothermia divided by the concentration at the same time point in hypothermia) for plasma, muscle, and subcutaneous tissue.
2.5 Data Analysis
2.5.1 Urine Excretion
The amount of drug excreted in urine within the first 6 h after infusion initiation at the targeted temperature (hypo- or normothermia) was quantified based on concentration measurements at various urine sampling intervals. This was expressed as a percentage of the administered drug dose for one dosing interval.
2.6 Statistical Methods
Data presentation included mean values ± SDs or geometric means with 95% confidence intervals, as appropriate. A paired, parametric t test was used to test for statistical significance of differences, at a two-sided p value of < 0.05.
3 Results
3.1 Study Population
The study included 10 patients (nine males, one female). Demographics and resuscitation details are available in Tables 1 and 2 in the electronic supplementary material (ESM). Causes of CA and post-resuscitation care specifics are detailed in Table 3 in the ESM. Laboratory results for both phases are in Tables 1 and 4 in the ESM. Mean ± SD C-reactive protein increased from 4.7 ± 8.4 mg/dL (AMO/CLAV group) and 1.1 ± 1.2 mg/dL (AMP/SULB group) during hypothermia to 15.1 ± 6.1 mg/dL and 8.5 ± 4.9 mg/dL, respectively, in normothermia. Medical history and relevant pharmacotherapy are in Tables 5 and 6, respectively, in the ESM.
In the AMO/CLAV group (one female, four males, age 62 ± 16 years, weight 93 ± 12 kg, BMI 30 ± 5 kg/m2), four of the five developed aspiration pneumonia on day 1. The remaining patient, who had hypoxic CA from grape aspiration, had the obstruction removed bronchoscopically after ROSC. In the AMP/SULB group (five males, age 56 ± 13 years, weight 103 ± 21 kg, BMI 29 ± 7 kg/m2), all five showed pneumonia signs from aspiration on day 1.
One minor adverse event—a small skin bleed after removal of the microdialysis probe—occurred, with no further complications. No allergic reactions to antibiotics were observed.
3.2 Pharmacokinetic Analysis
3.2.1 Steady-State Concentration–Time Profiles
Figure 1 illustrates the mean unbound plasma concentration–time profiles for hypothermic and normothermic states. CLAV levels were nearly identical in both conditions. AMO peaked within the first hour, slightly higher during normothermia, and AMP and SULB had higher concentrations during hypothermia. However, no significant differences were observed.
3.2.2 Comparison of Plasma Pharmacokinetic Parameters
The plasma pharmacokinetic parameters and drug amounts excreted in urine for AMO/CLAV and AMP/SULB during hypothermia and normothermia are detailed in Tables 1 and 2, respectively. No statistically significant differences between the two temperature states were observed.
3.2.3 Concentration Ratios
Table 3 presents the ratios of normothermic to hypothermic concentrations in plasma, muscle tissue, and subcutaneous adipose tissue. Notably, there was a trend indicating higher plasma concentrations of AMO/CLAV during hypothermia, with mean ratios of 0.87 for AMO and 0.76 for CLAV. Conversely, the plasma exposure of AMP/SULB remained comparable across the two temperature conditions.
3.2.4 Tissue Concentration Differences
Significant differences in tissue concentrations between hypothermic and normothermic states were observed for AMO and CLAV in subcutaneous tissue, with p values of 0.029 and 0.012, respectively. However, the overall analysis of the remaining soft tissue concentrations revealed no consistent trend between the hypothermic and normothermic states (Table 3).
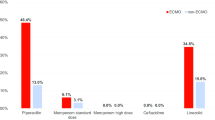
3.2.5 Pharmacokinetic/Pharmacodynamic Targets
Table 4 displays the fT>MIC values for MICs of 4 mg/L, 8 mg/L, and 16 mg/L for both AMO and AMP. For MICs up to 8 mg/L, the mean fT>MIC exceeded 50% of the dosing interval for both antimicrobial agents, indicating adequate exposure. The comparison between hypothermia and normothermia in terms of pharmacokinetic/pharmacodynamic target attainment (% fT>MIC) did not show statistically significant differences.
3.2.6 Pulmonary Concentrations of AMP and SULB
Pulmonary AMP and SULB concentrations were measured in the ELF of five patients at 2, 4, or 6 h (±1 h) after antibiotic administration. AMP was detectable in all BAL samples, and SULB was undetectable in one due to interference. Two patients missed BAL sampling after transfer from the ED to the ICU, leading to missing AMP/SULB data for one patient in the normothermic phase and another in the hypothermic phase. In one patient, BAL was performed at different time points during the two phases for organizational reasons: during hypothermia (2 h after antibiotic administration) and during normothermia (6 h after antibiotic administration). ELF concentrations are shown in Fig. 2.
4 Discussion
This is the first study to examine the effects of hypothermia on the pharmacokinetics of AMO/CLAV and AMP/SULB in plasma, muscle, subcutaneous tissue, and ELF in resuscitated adults. It aimed to assess how controlled hypothermia (33 ± 1 °C) affects pharmacokinetics and antibiotic efficacy in treating aspiration pneumonia after ROSC.
The plasma pharmacokinetic parameters of AMP/SULB aligned with those from previous studies in healthy individuals and patients with normal renal function [15, 26, 27]. Similarly, AMO/CLAV pharmacokinetic parameters were consistent with published data [28, 29].
We expected altered antibiotic pharmacokinetics between the two temperature phases in our cohort of hypothermic, critically ill patients receiving multiple medications after surviving CA.
In a large multinational study on beta-lactams (including AMO and AMP) in critically ill patients, plasma concentrations varied significantly, leading to inconsistent achievement of pharmacokinetic targets [30]. Hypothermia may slow drug absorption, especially for oral drugs, and reduce the volume of distribution, potentially increasing toxicity because of altered perfusion, blood pH, and drug properties [31]. Most research, which is particularly lacking in antibiotics, relies on animal studies, indicating a gap in the understanding of the full impact of hypothermia on drug pharmacokinetics and pharmacodynamics in humans [31, 32].
In the present study, we could not identify statistically significant differences in plasma concentrations, pharmacokinetic parameters, or the amount of drug excreted in urine of AMO/CLAV and AMP/SULB between the hypothermic and normothermic phases.
Antibiotic penetration into peripheral soft tissues was not impaired during the hypothermic state. Although no consistent trend was observed between hypothermic and normothermic conditions, AMO and CLAV showed significantly higher subcutaneous tissue concentrations during hypothermia. These findings suggest that although hypothermia does not broadly affect antibiotic penetration into soft tissues, it may influence the distribution of specific antibiotics.
The pulmonary ELF concentration of AMP and SULB in our small cohort showed no clear trend for reliable interpretation. However, in two patients, concentrations of AMP and SULB were similar at the respective sampling time points during both the hypothermia and the normothermia phases. In one patient, low concentrations were observed in the 2-h BAL (hypothermia) and high concentrations in the 6-h BAL (normothermia). No relevant clinical reason could be identified for these extreme values compared with the other available samples at the respective time points. Previous studies have reported a significant variability in ELF exposure. A comprehensive review highlighted this variability, especially in critically ill patients with lower respiratory tract infections, and emphasized the need for further research to optimize dosing regimens and understand the relationship between ELF concentrations and clinical outcomes [33].
Literature indicates that the causative micro-organisms in early-onset pneumonia after ROSC of patients resuscitated from out-of-hospital CA are most frequently Staphylococcus aureus, Streptococcus pneumoniae, Streptococcus spp., Haemophilus influenzae, Escherichia coli, and Klebsiella pneumoniae [34, 35].
According to our data, bactericidal fT>MIC of AMO and of AMP in plasma was ≥ 50%, but < 100% (of the dosing interval) for MIC values of 4 mg/L and 8 mg/L, and < 50% for a MIC of 16 mg/L. There was no statistically significant difference in achievement of pharmacokinetic/pharmacodynamic targets, expressed as % fT>MIC, between normothermia and hypothermia in the ten patients analyzed.
5 Limitations
Our study has several limitations that must be considered.
First, the small sample size and predominantly male, exclusively white demographic may limit the generalizability of the findings. However, this aligns with evidence that sudden CA more frequently affects men because of higher cardiovascular disease incidences and mortality rates [36]. Additionally, critically ill patients, particularly those who undergo resuscitation, often develop acute kidney injury within the first 48 h after CA [37, 38], necessitating antibiotic dose adjustments. Our study included only patients with normal renal function and excluded those with renal impairment, which limits the data on how renal dysfunction affects antibiotic pharmacokinetics during hypothermia, an important area for future research. We also excluded patients who underwent extracorporeal cardiopulmonary resuscitation or veno-arterial extracorporeal membrane oxygenation (ECMO) following ROSC. As the use of ECMO in resuscitation is growing, this exclusion is significant, particularly given the impact of ECMO on beta-lactam pharmacokinetics, underscoring the need for tailored drug monitoring and further research in ECMO settings [39, 40]. Lastly, the antibiotics were administered via short infusions, which contrasts with guidelines recommending prolonged or continuous infusions in critically ill patients, especially those with septic shock or high severity scores, to optimize therapeutic outcomes [41]. Continuous infusions are more commonly used in the ICU setting, whereas short infusions are typically used in emergency contexts such as in the ED.
6 Conclusion
Our study showed no significant differences in relevant pharmacokinetic parameters of AMP/SULB and AMO/CLAV for plasma and renal excretion between hypothermia and normothermia. Antibiotic penetration into peripheral soft tissues remained unaffected during hypothermia. In our small cohort, the pulmonary ELF concentrations of AMP and SULB showed no clear trend. Pharmacokinetic/pharmacodynamic targets (fT>MIC) for MICs up to 8 mg/L were met but not for 16 mg/L.
Further research in larger cohorts and with other antibiotics is needed to better understand the impact of controlled hypothermia on antibiotic therapy in patients resuscitated after CA.
References
Perkins GD, Graesner JT, Semeraro F, Olasveengen T, Soar J, Lott C, et al. European Resuscitation Council Guidelines 2021: executive summary. Resuscitation. 2021;161:1–60. https://doi.org/10.1016/j.resuscitation.2021.02.003.
Gräsner JT, Wnent J, Herlitz J, Perkins GD, Lefering R, Tjelmeland I, et al. Survival after out-of-hospital cardiac arrest in Europe—results of the EuReCa TWO study. Resuscitation. 2020;148:218–26. https://doi.org/10.1016/j.resuscitation.2019.12.042.
Sandroni C, Nolan JP, Andersen LW, Böttiger BW, Cariou A, Cronberg T, et al. ERC-ESICM guidelines on temperature control after cardiac arrest in adults. Intensive Care Med. 2022;48(3):261–9. https://doi.org/10.1007/s00134-022-06620-5.
Behringer W, Böttiger BW, Biasucci DG, Chalkias A, Connolly J, Dodt C, et al. Temperature control after successful resuscitation from cardiac arrest in adults: a joint statement from the European Society for Emergency Medicine (EUSEM) and the European Society of Anaesthesiology and Intensive Care (ESAIC). Eur J Emerg Med. 2024;31(2):86–9. https://doi.org/10.1097/mej.0000000000001106.
Behringer W, Skrifvars MB, Taccone FS. Postresuscitation management. Curr Opin Crit Care. 2023;29(6):640–7. https://doi.org/10.1097/MCC.0000000000001116.
Anderson KB, Poloyac SM, Kochanek PM, Empey PE. Effect of hypothermia and targeted temperature management on drug disposition and response following cardiac arrest: a comprehensive review of preclinical and clinical investigations. Ther Hypothermia Temp Manag. 2016;6(4):169–79. https://doi.org/10.1089/ther.2016.0003.
Hasslacher J, Steinkohl F, Ulmer H, Lehner G, Klein S, Mayerhoefer T, et al. Increased risk of ventilator-associated pneumonia in patients after cardiac arrest treated with mild therapeutic hypothermia. Acta Anaesthesiol Scand. 2022;66(6):704–12. https://doi.org/10.1111/aas.14063.
Rafailidis PI, Ioannidou EN, Falagas ME. Ampicillin/sulbactam: current status in severe bacterial infections. Drugs. 2007;67(13):1829–49. https://doi.org/10.2165/00003495-200767130-00003.
Francois B, Cariou A, Clere-Jehl R, Dequin PF, Renon-Carron F, Daix T, et al. Prevention of early ventilator-associated pneumonia after cardiac arrest. N Engl J Med. 2019;381(19):1831–42. https://doi.org/10.1056/NEJMoa1812379.
Nolan JP, Sandroni C, Bottiger BW, Cariou A, Cronberg T, Friberg H, et al. European Resuscitation Council and European Society of Intensive Care Medicine Guidelines 2021: post-resuscitation care. Resuscitation. 2021;161:220–69. https://doi.org/10.1016/j.resuscitation.2021.02.012.
Hirsch KG, Abella BS, Amorim E, Bader MK, Barletta JF, Berg K, et al. Critical care management of patients after cardiac arrest: a scientific statement from the American Heart Association and Neurocritical Care Society. Neurocrit Care. 2024;40(1):1–37. https://doi.org/10.1007/s12028-023-01871-6.
Muller M, Schmid R, Georgopoulos A, Buxbaum A, Wasicek C, Eichler HG. Application of microdialysis to clinical pharmacokinetics in humans. Clin Pharmacol Ther. 1995;57(4):371–80. https://doi.org/10.1016/0009-9236(95)90205-8.
Brunner M, Derendorf H, Müller M. Microdialysis for in vivo pharmacokinetic/pharmacodynamic characterization of anti-infective drugs. Curr Opin Pharmacol. 2005;5(5):495–9. https://doi.org/10.1016/j.coph.2005.04.010.
Benson JM, Nahata MC. Sulbactam/ampicillin, a new beta-lactamase inhibitor/beta-lactam antibiotic combination. Drug Intell Clin Pharm. 1988;22(7–8):534–41. https://doi.org/10.1177/106002808802200702.
Meyers BR, Wilkinson P, Mendelson MH, Walsh S, Bournazos C, Hirschman SZ. Pharmacokinetics of ampicillin-sulbactam in healthy elderly and young volunteers. Antimicrob Agents Chemother. 1991;35(10):2098–101. https://doi.org/10.1128/AAC.35.10.2098.
Arancibia A, Guttmann J, González G, González C. Absorption and disposition kinetics of amoxicillin in normal human subjects. Antimicrob Agents Chemother. 1980;17(2):199–202. https://doi.org/10.1128/aac.17.2.199.
Sjövall J, Alván G, Huitfeldt B. Intra- and inter-individual variation in pharmacokinetics of intravenously infused amoxycillin and ampicillin to elderly volunteers. Br J Clin Pharmacol. 1986;21(2):171–81. https://doi.org/10.1111/j.1365-2125.1986.tb05172.x.
Crombez T, Hachimi-Idrissi S. The influence of targeted temperature management on the pharmacokinetics of drugs administered during and after cardiac arrest: a systematic review. Acta Clin Belg. 2017;72(2):116–22. https://doi.org/10.1080/17843286.2017.1291782.
Veiga RP, Paiva JA. Pharmacokinetics-pharmacodynamics issues relevant for the clinical use of beta-lactam antibiotics in critically ill patients. Crit Care. 2018;22(1):233. https://doi.org/10.1186/s13054-018-2155-1.
Poppe M, Clodi C, Schriefl C, Mueller M, Sunder-Plaßmann R, Reiter B, et al. Targeted temperature management after cardiac arrest is associated with reduced metabolism of pantoprazole—a probe drug of CYP2C19 metabolism. Biomed Pharmacother. 2022;146: 112573. https://doi.org/10.1016/j.biopha.2021.112573.
Zeitlinger M, Schwameis R, Burian A, Burian B, Matzneller P, Muller M, et al. Simultaneous assessment of the pharmacokinetics of a pleuromutilin, lefamulin, in plasma, soft tissues and pulmonary epithelial lining fluid. J Antimicrob Chemother. 2016;71(4):1022–6. https://doi.org/10.1093/jac/dkv442.
Matzneller P, Osterreicher Z, Reiter B, Lackner E, Stimpfl T, Zeitlinger M. Tissue pharmacokinetics of telavancin in healthy volunteers: a microdialysis study. J Antimicrob Chemother. 2016;71(11):3179–84. https://doi.org/10.1093/jac/dkw269.
Kees F. Preparation for HPLC of samples in biological matrices, and problems of degradation. In: High performance liquid chromatography in medical microbiology. Stuttgart: F. Fischer Verlag; 1986.
Lier C, Dejaco A, Kratzer A, Kees MG, Kees F, Dorn C. Free serum concentrations of antibiotics determined by ultrafiltration: extensive evaluation of experimental variables. Bioanalysis. 2024. https://doi.org/10.1080/17576180.2024.2365526.
The European Committee on Antimicrobial Susceptibility Testing. Antimicrobial wild type distributions of microorganisms 2024. https://mic.eucast.org/search/?search%5Bmethod%5D=mic&search%5Bantibiotic%5D=8&search%5Bspecies%5D=-1&search%5Bdisk_content%5D=-1&search%5Blimit%5D=50.
Blum RA, Kohli RK, Harrison NJ, Schentag JJ. Pharmacokinetics of ampicillin (2.0 grams) and sulbactam (1.0 gram) coadministered to subjects with normal and abnormal renal function and with end-stage renal disease on hemodialysis. Antimicrob Agents Chemother. 1989;33(9):1470–6. https://doi.org/10.1128/aac.33.9.1470.
Foulds G. Pharmacokinetics of sulbactam/ampicillin in humans: a review. Rev Infect Dis. 1986;8(Suppl 5):S503–11. https://doi.org/10.1093/clinids/8.supplement_5.503.
Carlier M, Noë M, De Waele JJ, Stove V, Verstraete AG, Lipman J, et al. Population pharmacokinetics and dosing simulations of amoxicillin/clavulanic acid in critically ill patients. J Antimicrob Chemother. 2013;68(11):2600–8. https://doi.org/10.1093/jac/dkt240.
Crass RL, Pai MP. Pharmacokinetics and pharmacodynamics of β-lactamase inhibitors. Pharmacotherapy. 2019;39(2):182–95. https://doi.org/10.1002/phar.2210.
Roberts JA, Paul SK, Akova M, Bassetti M, De Waele JJ, Dimopoulos G, et al. DALI: defining antibiotic levels in intensive care unit patients: are current β-lactam antibiotic doses sufficient for critically ill patients? Clin Infect Dis. 2014;58(8):1072–83. https://doi.org/10.1093/cid/ciu027.
van den Broek MP, Groenendaal F, Egberts AC, Rademaker CM. Effects of hypothermia on pharmacokinetics and pharmacodynamics: a systematic review of preclinical and clinical studies. Clin Pharmacokinet. 2010;49(5):277–94. https://doi.org/10.2165/11319360-000000000-00000.
Zhou J, Poloyac SM. The effect of therapeutic hypothermia on drug metabolism and response: cellular mechanisms to organ function. Expert Opin Drug Metab Toxicol. 2011;7(7):803–16. https://doi.org/10.1517/17425255.2011.574127.
Drwiega EN, Rodvold KA. Penetration of antibacterial agents into pulmonary epithelial lining fluid: an update. Clin Pharmacokinet. 2022;61(1):17–46. https://doi.org/10.1007/s40262-021-01061-7.
François B, Cariou A, Clere-Jehl R, Dequin PF, Renon-Carron F, Daix T, et al. Prevention of early ventilator-associated pneumonia after cardiac arrest. N Engl J Med. 2019;381(19):1831–42. https://doi.org/10.1056/NEJMoa1812379.
Perbet S, Mongardon N, Dumas F, Bruel C, Lemiale V, Mourvillier B, et al. Early-onset pneumonia after cardiac arrest: characteristics, risk factors and influence on prognosis. Am J Respir Crit Care Med. 2011;184(9):1048–54. https://doi.org/10.1164/rccm.201102-0331OC.
Empana JP, Lerner I, Valentin E, Folke F, Bottiger B, Gislason G, et al. Incidence of sudden cardiac death in the European Union. J Am Coll Cardiol. 2022;79(18):1818–27. https://doi.org/10.1016/j.jacc.2022.02.041.
Patyna S, Riekert K, Buettner S, Wagner A, Volk J, Weiler H, et al. Acute kidney injury after in-hospital cardiac arrest in a predominant internal medicine and cardiology patient population: incidence, risk factors, and impact on survival. Ren Fail. 2021;43(1):1163–9. https://doi.org/10.1080/0886022X.2021.1956538.
Geri G, Guillemet L, Dumas F, Charpentier J, Antona M, Lemiale V, et al. Acute kidney injury after out-of-hospital cardiac arrest: risk factors and prognosis in a large cohort. Intensive Care Med. 2015;41(7):1273–80. https://doi.org/10.1007/s00134-015-3848-4.
Polain A, Gorham J, Romeo I, Belliato M, Peluso L, Partipilo F, et al. Prediction of insufficient beta-lactam concentrations in extracorporeal membranous oxygenation patients. Microorganisms. 2021. https://doi.org/10.3390/microorganisms9112219.
Cheng V, Abdul-Aziz MH, Roberts JA, Shekar K. Optimising drug dosing in patients receiving extracorporeal membrane oxygenation. J Thorac Dis. 2018;10(Suppl 5):S629–41. https://doi.org/10.21037/jtd.2017.09.154.
Guilhaumou R, Benaboud S, Bennis Y, Dahyot-Fizelier C, Dailly E, Gandia P, et al. Optimization of the treatment with beta-lactam antibiotics in critically ill patients—guidelines from the French Society of Pharmacology and Therapeutics (Société Française de Pharmacologie et Thérapeutique—SFPT) and the French Society of Anaesthesia and Intensive Care Medicine (Société Française d’Anesthésie et Réanimation—SFAR). Crit Care. 2019;23(1):104. https://doi.org/10.1186/s13054-019-2378-9.
Acknowledgements
The authors offer their sincere thanks to the ED team and the ICU teams of the Medical University of Vienna (ICU 13I2, 13I3, 13H1, and 13H3) for their support and collaboration throughout the duration of the study. Peter Matzneller is currently employed at the Service of Rheumatology, Hospital of Merano, South Tyrol Health System ASDAA-SABES, South Tyrol, Italy. Beatrix Wulkersdorfer is currently employed at the Orthopedic Clinic-SKA Zicksee, Otto-Pohanka-Platz 1, 7161 St. Andrae am Zicksee, Austria.
Funding
Open access funding provided by Medical University of Vienna.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the Medical Scientific Fund of the Mayor of the City Vienna (project number: 15092).
Conflict of interest
Markus Zeitlinger is an editorial board member of Clinical Pharmacokinetics and was not involved in the selection of peer reviewers for the manuscript nor any of the subsequent editorial decisions. The other authors have no competing interests to declare that are relevant to the content of this article.
Availability of data and materials
The datasets generated during the current study are available from the corresponding author upon reasonable request.
Author contributions
Alexandra-Maria Stommel: conceptualization, validation, formal analysis, investigation, data curation, writing—original draft, writing—review and editing, and visualization. Peter Matzneller: conceptualization, investigation, and writing—review and editing. Valentin al Jalali: formal analysis, data curation, visualization, and writing—review and editing. Beatrix Wulkersdorfer: investigation, data curation, writing—review and editing, and project administration. Edith Lackner: investigation, writing—review and editing, and project administration. Matthias Mueller: investigation and writing—review and editing. Christoph Dorn: methodology, validation, formal analysis, investigation, resources, data curation, and writing—review and editing. Michael Holzer: writing—review and editing and supervision. Markus Zeitlinger: conceptualization, methodology, validation, resources, writing—review and editing, supervision, project administration, and funding acquisition.
Ethics approval
The study was approved by the ethics committee of the Medical University of Vienna, Austria (EC: 1348/2015) and the Austrian Agency for Health and Food Safety. It was registered in the European Union Drug Regulating Authorities Clinical Trials Database (EUDRACT 2015-001793-18) and conducted according to International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use good clinical practice guidelines and the Declaration of Helsinki.
Consent to participate
Since the participants were unconscious, informed written consent was obtained from survivors once they were able to comprehend the study. The treating team informed patients’ relatives about their inclusion in the study, but the ethics committee did not mandate this as a requirement.
Consent for publication
Not applicable.
Code availability
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Stommel, AM., Matzneller, P., al Jalali, V. et al. Impact of Hypothermic Temperature Control on Plasma and Soft Tissue Pharmacokinetics of Penicillin/Beta-Lactamase Inhibitor Combinations in Patients Resuscitated After Cardiac Arrest. Clin Pharmacokinet 64, 691–701 (2025). https://doi.org/10.1007/s40262-025-01497-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-025-01497-1