Abstract
Research concerning psychiatric issues relating to opioid drugs currently focuses primarily on their role in reinforcing addictive behaviors, given the recent proliferation of lethal abuse of illicit opiates in the United States and around the world. In contrast, this article will review the mechanism of action of opioids in affective disorders and the available evidence and potential for their use, especially in the treatment of resistant major depression. Buprenorphine is the opioid derivative of special interest; we review this and other opioid derivatives, highlighting the growing role of opioids in treating depressive illnesses and other related psychopathologies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Notes
Samidorphan combined with buprenorphine differs from naloxone combined with buprenorphine, as naloxone is not absorbed sublingually, and leaves buprenorphine’s μ-activity unaffected when administered sublingually. Naloxone is intended to prevent illicit administration of buprenorphine parenterally, as parenteral naloxone blocks μ-activity.
References
Goodman and Gilman’s. The pharmacological basis of therapeutics, 13th edn. Dec 5, 2017 by Laurence Brunton and Bjorn Knollmann; 2017.
Brownstein MJ. A brief history of opiates, opioid peptides and opioid receptors. Proc Natl Acad Sci USA. 1993;90:5391–3.
Baraka A. Historical aspects of opium. Middle East J Anesthesiol. 2000;15:423–36.
Weber MM, Emrich HM. Current and historical concepts of opiate treatment in psychiatric disorders. Int Clin Psychopharmacol. 1988;3(3):255–66.
Kraeplin E. Manic depressive illness and paranoia. Edinburgh: Livingstone; 1921.
Mayer-Gross W, Slater E, Roth M. Clinical psychiatry. Baltimore: Williams and Wilkins; 1954.
Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, Norquist G, Howland RH, Lebowitz B, McGrath PJ, Shores-Wilson K, Biggs MM, Balasubramani GK, Fava M, STAR*D Study Team. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163(1):28–40.
Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, Niederehe G, Thase ME, Lavori PW, Lebowitz BD, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163:1905–17.
Tenor Peter L. Psychotherapeutic benefits of opioid agonist therapy. J Addict Dis. 2008;27(3):49–65.
Contet C, Kieffer BL, Befort K. Mu opioid receptor: a gateway to drug addiction. Curr Opin Neurobiol. 2004;14(3):370–8.
Lutz P, Kieffer B. Opioid receptors: distinct roles in mood disorders. Trends Neurosci. 2013;36(3):195–206.
Nutt DJ. Relationship of neurotransmitters to the symptoms of major depressive disorder. J Clin Psychiatry. 2008;69(suppl E1):4–7.
Svingos AL, Chavkin C, Colago EE, Pickel VM. Major coexpression of kappa-opioid receptors and the dopamine transporter in nucleus accumbens axonal profiles. Synapse. 2001;42(3):185–92.
Carlezon W Jr, Beguin C, Knoll AT, Cohen BM. Kappa opioid ligands in the study and treatment of mood disorders. Pharmacol Ther. 2009;123:334–43.
Bear DM, Kessler RM. United States Patent 8,883,831; 2014a.
Bear DM, Kessler RM. US Patent Application PCT/US2014/013874. Washington, DC; 2014b.
Mischoulon D, Hylek L, Yeung AS, Clain AJ, Baer L, Cusin C, Ionefscu DF, Alpert JE, Soskin DP, Fava M. Randomized, proof of concept trial of low dose naltrexone for patients with breakthrough symptoms of major depressive disorder on antidepressants. J Affect Disord. 2017;208:6–14.
Berrocos E, Sanchez-Blazquez P, Garzón J, Mico JA. Opiates as antidepressants. Curr Pharm Design. 2009;15:1612–22.
Lauterbach EC. Treatment resistant depression with loss of antidepressant response: rapid—acting antidepressant action of dextromethorphan, a possible treatment bridging molecule. Psychopharmacol Bull. 2016;46(2):53–8.
Snyder CB, Pert SH. Opiate receptor: demonstration in nervous tissue. Science. 1973;179(4077):1011–4.
Parker KJ, Schatzberg AF, Lyons DM. Neuroendocrine aspects of hypercortisolism in major depression. Horm Behav. 2003;43(1):60–6.
Vuong C, Van Uum SH, O’Dell LE, Lutfy K, Friedman TC. The effects of opioids and opioid analogs on animal and human endocrine systems. Endocr Rev. 2010;31(1):98–132.
Dickenson AH. NMDA receptor antagonists: interactions with opioids. Acta Anaesthesiol Scand. 1997;41(1 Pt 2):112–5.
Schwartz-Lifshitz M, Zalsman G, Giner L, Oquendo MA. Can we really prevent suicide? Curr Psychiatry Rep. 2012;14(6):624–33.
Gross-Isseroff R, Dillon KA, Israeli M, Biegon A. Regionally selective increases in mu opioid receptor density in the brains of suicide victims. Brain Res. 1990;530(2):312–6.
Gabilondo AM, Meana JJ, García-Sevilla JA. Increased density of mu-opioid receptors in the postmortem brain of suicide victims. Brain Res. 1995;682(1–2):245–50.
Kennedy SE, Koeppe RA, Young EA, Zubieta JK. Dysregulation of endogenous opioid emotion regulation circuitry in major depression in women. Arch Gen Psychiatry. 2006;63(11):1199–208.
Scarr E, Money TT, Pavey G, Neo J, Dean B. Mu opioid receptor availability in people with psychiatric disorders who died by suicide: a case control study. BMC Psychiatry. 2012;28(12):126.
Kosten T, Morgan C, Kosten TA. Depressive symptoms during buprenorphine treatment of opioid abusers. J Subst Abuse Treat. 1990;7:51–4.
Dean AJ, Bell J, Mascord DJ, Parker G, Christie MJ. A randomised, controlled trial of fluoxetine in methadone maintenance patients with depressive symptoms. J Affect Disord. 2002;72:85–90.
Dean AJ, Bell J, Christie MJ, Mattick RP. Depressive symptoms during buprenorphine vs. methadone maintenance: findings from a randomised, controlled trial in opioid dependence. Eur Psychiatry. 2004;19:510–3.
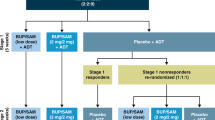
Fava M, Memisoglu A, Thase ME, Bodkin JA, Trivedi MH, de Somer M, Du Y, Leigh-Pemberton R, DiPetrillo L, Silverman B, et al. Opioid modulation with buprenorphine/samidorphan as adjunctive treatment for inadequate response to antidepressants: a randomized double-blind placebo-controlled trial. Am J Psychiatry. 2016;173(5):499–508.
Leander JD. Buprenorphine has potent kappa opioid receptor antagonist activity. Neuropharmacology. 1987;26(9):1445–7.
Knoll AT, Carlezon WA. Dynorphin, stress, and depression. Brain Res. 2010;1314:56–73.
Thase ME, Stanford AD, Memisoglu A, Martin W, Claxton A, Bodkin JA, Trivedi MH, Fava M, Pathak S. Long-term efficacy, safety and tolerability of adjunctive ALKS 5461 as adjunctive treatment in patients with major depressive disorder enrolled in an ongoing Phase 3 study: poster session presented at American Psychiatric Association annual meeting. NY: NYC; 2018.
Emrich HM, Vogt P, Herz A, Kissling W. Antidepressant effects of buprenorphine. Lancet. 1982;2(8300):709.
Morgan L, Calloway E. Buprenorphine responders. Biol Psychiat. 1990;28(12):1078–80.
Bodkin JA, Zornberg GL, Lukas SE, Cole JO. Buprenorphine treatment of refractory depression. J Clin Psychopharmacol. 1995;15(1):49–57.
Nyhuis PW, Gastpar M, Scherbaum N. Opiate treatment in depression refractory to antidepressants and electroconvulsive therapy. J Clin Psychopharmacol. 2008;28(5):593–5.
Karp JF, Butters MA, Begley AE, Miller MD, Lenze EJ, Blumberger DM, Mulsant BH, Reynolds CF 3rd. Safety, tolerability, and clinical effect of low-dose buprenorphine for treatment-resistant depression in mid-life and older adults. J Clin Psychiatry. 2014;75(8):e785–93.
Ehrich E, Turncliff R, Du Y, Leigh-Pemberton R, Fernandez E, Jones R, Fava M. Evaluation of opioid modulation in major depressive disorder. Neuropsychopharmacology. 2015;40:1448–55.
Yowell Y, Bar G, Mashiah M, Baruch Y, Briskman I, Asherov J, Lotan A, Rigbi A, Panksepp J. Ultra-low-dose buprenorphine as a time-limited treatment for severe suicidal ideation: a randomized controlled trial. Am J Psychiatry. 2016;173(5):491–8.
Guerdjikova A, Walsh B, Shan K, Halseth AE, Dunayevich E, McElroy SL. Concurrent improvement in both binge eating and depressive symptoms with naltrexone/bupropion therapy in overweight or obese subjects with major depressive disorder in an open-label, uncontrolled study. Adv Ther. 2017;34(10):2307–15.
Murphy B, Ravichandran C, Babb SM, Cohen BM. Naltrexone in bipolar disorder with depression: a double-blind, placebo-controlled study. Clin Psychopharmacol. 2014;34(6):749–51.
Raffa RB, Friderichs E, Reimann W, Shank RP, Codd EE, Vaught JL. Opioid and nonopioid components independently contribute to the mechanism of action of tramadol, an ‘atypical’ opioid analgesic. J Pharmacol Exp Ther. 1992;260(1):275–85.
Raffa RB, Buschmann H, Christoph T, Eichenbaum G, Englberger W, Flores CM, Hertrampf T, Kögel B, Schiene K, Straßburger W, Terlinden R, Tzschentke TM. Mechanistic and functional differentiation of tapentadol and tramadol. Expert Opin Pharmacother. 2012;13(10):1437–49.
Shapira NA, Verduin ML, DeGraw JD. Treatment of refractory major depression with tramadol monotherapy. J Clin Psychiatry. 2001;62(3):205–6.
Spencer C. The efficacy of intramuscular tramadol as a rapid-onset antidepressant. Aust N Z J Psychiatry. 2000;34(6):1032–3.
Rougemont-Bücking A, Gamma F, Panksepp J. Use of tramadol in psychiatric care: a comprehensive review and report of two cases. Swiss Med Wkly. 2017;147:w14428.
Press release 14 January 2009. E-therapeutics. http://www.firstwordpharma.com/node/39762#axzz54JR5qryu.
Press release 15 February 2016. E therapeutics https://www.fiercebiotech.com/biotech/e-therapeutics-reports-top-line-phase-iib-results-major-depressive-disorder.
Stanley B, Siever L. The Interpersonal Dimension of borderline personality disorder: toward a neuropeptide model. Am J Psychiatry. 2010;167:24–39.
Stanley B, Sher L, Wilson S, Ekman R, Huang YY, Mann JJ. Non suicidal self-injurious behavior, endogenous opioids and monoamine neurotransmitters. J Affect Disord. 2010;124(1–2):134–40.
Bresin K, Gordon KH. Endogenous opioids and nonsuicidal self-injury: a mechanism of affect regulation. Neurosci Biobehav Rev. 2013;37(3):374–83.
Resnick R, Falk F. Buprenorphine: pilot trials in borderline patients and opiate dependence—treatment of a common disorder? Monograph. In: Harris LS, editor. Problems of drug dependence. Washington, DC: National Institute on Drug Abuse Research; 1987. p. 155–68.
Koran LM, Aboujaoude E, Bullock KD, Franz B, Gamel N, Elliott M. Double-blind treatment with oral morphine in treatment-resistant obsessive-compulsive disorder. J Clin Psychiatry. 2005;66(3):353–9.
Shapira NA, Keck PE Jr, Goldsmith TD, et al. Open-label pilot study of tramadol hydrochloride in treatment-refractory obsessive-compulsive disorder. Depress Anxiety. 1997;6:170–3.
Goldsmith TB, Shapira NA, Keck PE Jr. Rapid remission of OCD with tramadol hydrochloride. Am J Psychiatry. 1999;156:660–1.
Liddell Malcolm B, Aziz Victor, Briggs Patrick, Kanakkehewa Nimalee, Rawi Omar. Buprenorphine augmentation in the treatment of refractory obsessive–compulsive disorder. Ther Adv Psychopharmacol. 2013;3(1):15–9.
Ahmadpanah M, Reihani A, Ghaleiha A, Soltanian A, Haghighi M, Jahangard L, Sadeghi Bahmani D, Holsboer-Trachsler E, Brand S. Buprenorphine augmentation improved symptoms of OCD, compared to placebo—results from a randomized, double-blind and placebo-controlled clinical trial. J Psychiatr Res. 2017;94:23–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Parnika Saxena has no conflicts of interest to declare. J. Alexander Bodkin has a potential conflict due to longstanding efforts to advance the development of buprenorphine as an effective treatment for resistant depressive illness. He has helped Alkermes to engage in a development program of a buprenorphine/samidorphan preparation for use as an adjunctive treatment for resistant depression. This guidance was provided gratis; however, compensation was provided for participation in annual day-long group meetings with a group of academics held by Alkermes in Boston. His lab was also provided with funding for their work on a study on the long-term safety and efficacy of Alkermes’s buprenorphine/samidorphan preparation. Dr Bodkin will not benefit financially if the Alkermes preparation is approved and marketed, nor will he be harmed financially if it is not approved. Dr Bodkin authored one of the first American studies of buprenorphine in depression in 1995 and is one of the leading experts in the US on the use of opioids in depressive illness. He has assessed legal cases over the years as an expert on behalf of psychiatrists facing regulatory or civil litigation for having used opioids in treating resistant depression.
Funding
No sources of funding were used to assist with the preparation of this review.
Rights and permissions
About this article
Cite this article
Saxena, P.P., Bodkin, J.A. Opioidergic Agents as Antidepressants: Rationale and Promise. CNS Drugs 33, 9–16 (2019). https://doi.org/10.1007/s40263-018-0584-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-018-0584-7