Abstract
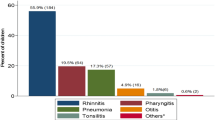
Otitis media (OM) or middle ear inflammation is a spectrum of diseases, including acute otitis media (AOM), otitis media with effusion (OME; ‘glue ear’) and chronic suppurative otitis media (CSOM). OM is among the most common diseases in young children worldwide. Although OM may resolve spontaneously without complications, it can be associated with hearing loss and life-long sequelae. In developing countries, CSOM is a leading cause of hearing loss. OM can be of bacterial or viral origin; during ‘colds’, viruses can ascend through the Eustachian tube to the middle ear and pave the way for bacterial otopathogens that reside in the nasopharynx. Diagnosis depends on typical signs and symptoms, such as acute ear pain and bulging of the tympanic membrane (eardrum) for AOM and hearing loss for OME; diagnostic modalities include (pneumatic) otoscopy, tympanometry and audiometry. Symptomatic management of ear pain and fever is the mainstay of AOM treatment, reserving antibiotics for children with severe, persistent or recurrent infections. Management of OME largely consists of watchful waiting, with ventilation (tympanostomy) tubes primarily for children with chronic effusions and hearing loss, developmental delays or learning difficulties. The role of hearing aids to alleviate symptoms of hearing loss in the management of OME needs further study. Insertion of ventilation tubes and adenoidectomy are common operations for recurrent AOM to prevent recurrences, but their effectiveness is still debated. Despite reports of a decline in the incidence of OM over the past decade, attributed to the implementation of clinical guidelines that promote accurate diagnosis and judicious use of antibiotics and to pneumococcal conjugate vaccination, OM continues to be a leading cause for medical consultation, antibiotic prescription and surgery in high-income countries.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 1 digital issues and online access to articles
$119.00 per year
only $119.00 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Bluestone, C. D. in Evidence-Based Otitis Media 2nd edn (eds Rosenfeld, R. M. & Bluestone, C. D. ) 121 (BC Decker Inc, 2003).
Monasta, L. et al. Burden of disease caused by otitis media: systematic review and global estimates. PLoS ONE 7, e36226 (2012). This comprehensive review provides global estimates on the burden of disease caused by OM.
Gulliford, M. et al. Selective decrease in consultations and antibiotic prescribing for acute respiratory tract infections in UK primary care up to 2006. J. Public Health (Oxf.) 31, 512–520 (2009).
Cullen, K., Hall, M. & Golosinskiy, A. Ambulatory surgery in the United States, 2006. National health statistics reports, no. 11, revised. CDChttps://www.cdc.gov/nchs/data/nhsr/nhsr011.pdf (2009).
Lieberthal, A. S. et al. The diagnosis and management of acute otitis media. Pediatrics 131, e964–e999 (2013).
Rosenfeld, R. M. & Kay, D. Natural history of untreated otitis media. Laryngoscope 113, 1645–1657 (2003).
Thompson, P. L. et al. Effect of antibiotics for otitis media on mastoiditis in children: a retrospective cohort study using the United kingdom general practice research database. Pediatrics 123, 424–430 (2009).
Rosenfeld, R. M. et al. Clinical practice guideline: otitis media with effusion (update). Otolaryngol. Head Neck Surg. 154, S1–S41 (2016).
Bennett, K. E., Haggard, M. P., Silva, P. A. & Stewart, I. A. Behaviour and development effects of otitis media with effusions into the teens. Arch. Dis. Child. 85, 91–95 (2001).
Chonmaitree, T. et al. Viral upper respiratory tract infection and otitis media complication in young children. Clin. Infect. Dis. 46, 815–823 (2008). This large prospective study reports a clear relationship between viral URTI and AOM and OME in children at the peak age of incidence of OM.
Alho, O., Oja, H., Koivu, M. & Sorri, M. Risk factors for chronic otitis media with effusion in infancy. Each otitis media episode induces a high but transient risk. Arch. Otolaryngol. Head Neck Surg. 121, 839–843 (1995).
Claessen, J. Q., Appelman, C. L., Touw-Otten, F. W., Hordijk, G. J. & de Melker, R. A. Persistence of middle ear dysfunction after recurrent acute otitis media. Clin. Otolaryngol. Allied Sci. 19, 35–40 (1994).
Verhoeff, M., van der Veen, E. L., Rovers, M. M., Sanders, E. A. M. & Schilder, A. G. M. Chronic suppurative otitis media: a review. Int. J. Pediatr. Otorhinolaryngol. 70, 1–12 (2006).
Rovers, M. M., Schilder, A. G., Zielhuis, G. A. & Rosenfeld, R. M. Otitis media. Lancet 363, 465–473 (2004). This review summarizes the state of knowledge in epidemiology, pathogenesis, diagnosis, treatment and prevention of OM up to 2004.
Tos, M. Epidemiology and natural history of secretory otitis. Am. J. Otol. 5, 459–462 (1984).
Zielhuis, G. A., Rach, G. H. & Van den Broek, P. The occurrence of otitis media with effusion in Dutch pre-school children. Clin. Otolaryngol. Allied Sci. 15, 147–153 (1990).
Williamson, I. G. et al. The natural history of otitis media with effusion — a three-year study of the incidence and prevalence of abnormal tympanograms in four South West Hampshire infant and first schools. J. Laryngol. Otol. 108, 930–934 (1994).
Paradise, J. L. et al. Otitis media in 2253 Pittsburgh-area infants: prevalence and risk factors during the first two years of life. Pediatrics 99, 318–333 (1997).
Chalmers, D. Otitis Media with Effusion in Children: The Dunedin Study (Mac Keith Press, 1989).
Casselbrant, M. L. & Mandel, E. M. in Evidence-Based Otitis Media (eds Rosenfeld, R. M. & Bluestone, C. D. ) 117–136 (BC Decker Inc., 1999).
Marchant, C. D. et al. Course and outcome of otitis media in early infancy: a prospective study. J. Pediatr. 104, 826–831 (1984).
Wals, P., Carbon, M., Sévin, E., Deceuninck, G. & Ouakki, M. Reduced physician claims for otitis media after implementation of pneumococcal conjugate vaccine program in the province of Quebec, Canada. Pediatr. Infect. Dis. J. 28, e271–e274 (2009).
Thomas, E. M. Recent trends in upper respiratory infections, ear infections and asthma among young Canadian children. Health Rep. 21, 1–6 (2010).
Grijalva, C. G., Nuorti, J. P. & Griffin, M. R. Antibiotic prescription rates for 460 acute respiratory tract infections in US ambulatory settings. JAMA 302, 758–766 (2009).
Marom, T. et al. Trends in otitis media-related health care utilization in the United States, 2001–2011. JAMA Pediatr. 168, 68–75 (2014).
Chonmaitree, T. et al. Acute otitis media and other complications of viral respiratory infection. Pediatrics 137, e2015355 (2016).
Plasschaert, A. I., Rovers, M. M., Schilder, A. G., Verheij, T. J. & Hak, E. Trends in doctor consultations, antibiotic perscription, and specialist referrals for otitis media in children: 1995–2003. Pediatrics 117, 1879–1986 (2006).
Lau, W. C. et al. Impact of pneumococcal conjugate vaccines on childhood otitis media in the United Kingdom. Vaccine 33, 5072–5079 (2015).
Leach, A. J. et al. Otitis media in children vaccinated during consecutive 7-valent or 10-valent pneumococcal conjugate vaccination schedules. BMC Pediatr. 14, 200 (2014).
Dallaire, F., Dewailly, E., Vezina, C., Bruneau, S. & Ayotte, P. Portrait of outpatient visits and hospitalizations for acute infections in Nunavik preschool children. Can. J. Public Health 97, 362–368 (2006).
Morris, P. S. et al. Otitis media in young Aboriginal children from remote communities in Northern and Central Australia: a cross-sectional survey. BMC Pediatr. 5, 27 (2005).
Todberg, T. et al. Incidence of otitis media in a contemporary Danish national birth cohort. PLoS ONE 9, e111732 (2014).
Macintyre, E. A. et al. Otitis media incidence and risk factors in a population-based birth cohort. Paediatr. Child Health 15, 437–442 (2010).
Zhang, Y. et al. Risk factors for chronic and recurrent otitis media — a meta-analysis. PLoS ONE 9, e86397 (2014).
Austeng, M. E. et al. Otitis media with effusion in children with Down syndrome. Int. J. Pediatr. Otorhinolaryngol. 77, 1329–1332 (2013).
Wilson, N. W. & Hogan, M. B. Otitis media as a presenting complaint in childhood immunodeficiency diseases. Curr. Allergy Asthma Rep. 6, 519–524 (2008).
Aydemir, G. & Ozkurt, F. E. Otitis media with effusion in primary schools in Princes' Islands, Istanbul: prevalence and risk factors. J. Int. Med. Res. 39, 866–872 (2011).
O'Reilly, R. C. et al. The role of gastric pepsin in the inflammatory cascade of pediatric otitis media. JAMA Otolaryngol. Head Neck Surg. 141, 350–357 (2015).
Brennan-Jones, C. G. et al. Prevalence and risk factors for parent-reported recurrent otitis media during early childhood in the Western Australian Pregnancy Cohort (Raine) study. J. Paediatr. Child Health 51, 403–409 (2015).
De Hoog, M. L. A. et al. Impact of early daycare on healthcare resource use related to upper respiratory tract infections during childhood: prospective WHISTLER cohort study. BMC Med. 12, 107 (2014).
Salah, M., Abdel-Aziz, M., Al-Farok, A. & Jebrini, A. Recurrent acute otitis media in infants: analysis of risk factors. Int. J. Pediatr. Otorhinolaryngol. 77, 1665–1669 (2013).
Rovers, M. M. et al. Is pacifier use a risk factor for acute otitis media? A dynamic cohort study. Fam. Pract. 25, 233–236 (2008).
Bowatte, G. et al. Breast feeding and childhood acute otitis media: a systematic review and meta-analysis. Acta Paediatr. Suppl. 104, 85–95 (2015).
Lasisi, A. O. et al. Clinical and demographic risk factors associated with chronic suppurative otitis media. Int. J. Pediatr. Otorhinolaryngol. 71, 1549–1554 (2007).
Taipale, A. et al. Chronic suppurative otitis media in children of Luanda, Angola. Acta Paediatr. 100, e84–e88 (2011).
Bluestone, C. D. in Evidence-Based Otitis Media 2nd edn (eds Rosenfeld, R. M. & Bluestone, C. D. ) 163–179 (BC Decker Inc, 2003).
Massa, H. M., Lim, D. J. & Cripps, A. W. in Mucosal Immunology 4th edn (eds Russel, M. W. & Lambrecht, B. ) 1423–1942 (2015). This is a comprehensive review of the innate and acquired immunology of the middle ear and the Eustachian tube.
Bluestone, C. D. & Klein, J. O. in Pediatric Otolaryngology 4th edn (eds Bluestone, C. D., Stoole, S. E. & Alper, C. M. ) 497–535 (2003).
Faden, H. et al. Relationship between nasopharyngeal colonization and the development of otitis media in children. J. Infect. Dis. 175, 1440–1445 (1997).
Leach, A. J., Boswell, J. B., Asche, V., Nienhuys, T. G. & Mathews, J. D. Bacterial colonization of the nasopharynx predicts very early onset and persistence of otitis media in Australian aboriginal infants. Pediatr. Infect. Dis. J. 13, 983–989 (1994).
Coker, T. R. et al. Diagnosis, microbial epidemiology, and antibiotic treatment of acute otitis media in children: a systematic review. JAMA 304, 2161–2169 (2010).
Ngo, C. C., Massa, H. M., Thornton, R. B. & Cripps, A. W. Predominant bacteria isolated from the middle ear fluid of children experiencing otitis media: a systematic review. PLoS ONE 11, e0150949 (2016). This systematic review provides recent global estimates on the predominant bacterial pathogens involved in OM.
Sun, W. et al. Association between early bacterial carriage and otitis media in Aboriginal and non-Aboriginal children in a semi-arid area of Western Australia: a cohort study. BMC Infect. Dis. 12, 366 (2012).
Watson, K. et al. Upper respiratory tract bacterial carriage in Aboriginal and non-Aboriginal children in a semi-arid area of Western Australia. Pediatr. Infect. Dis. J. 25, 782–790 (2006).
Smith-Vaughan, H. et al. Measuring nasal bacterial load and its association with otitis media. BMC Ear Nose Throat Disord. 6, 10 (2006).
Slinger, R. et al. Multiple combination antibiotic susceptibility testing of nontypeable Haemophilus influenzae biofilms. Diagn. Microbiol. Infect. Dis. 56, 247–253 (2006).
Garcia-Cobos, S. et al. Frequent carriage of resistance mechanisms to β-lactams and biofilm formation in Haemophilus influenzae causing treatment failure and recurrent otitis media in young children. J. Antimicrob. Chemother. 69, 2394–2399 (2014).
Lampikoski, H., Aarnisalo, A. A., Jero, J. & Kinnari, T. J. Mastoid biofilm in chronic otitis media. Otol. Neurotol. 33, 785–788 (2012).
Gu, X., Keyoumu, Y., Long, L. & Zhang, H. Detection of bacterial biofilms in different types of chronic otitis media. Eur. Arch. Otorhinolaryngol. 271, 2877–2883 (2014).
Van Hoecke, H. et al. Haemophilus influenzae biofilm formation in chronic otitis media with effusion. Eur. Arch. Otorhinolaryngol. 5 March 2016 [epub ahead of print].
Hall-Stoodley, L. et al. Direct detection of bacterial biofilms on the middle-ear mucosa of children with chronic otitis media. JAMA 296, 202–211 (2006).
Novotny, L. A. et al. Antibodies against the majority subunit of type IV pili disperse nontypeable Haemophilus influenzae biofilms in a LuxS-dependent manner and confer therapeutic resolution of experimental otitis media. Mol. Microbiol. 96, 276–292 (2015).
Nokso-Koivisto, J., Marom, T. & Chonmaitree, T. Importance of viruses in acute otitis media. Curr. Opin. Pediatr. 27, 110–115 (2015).
Abramson, J. S. & Hudnor, H. R. Role of the sialophorin (CD43) receptor in mediating influenza A virus-induced polymorphonuclear leukocyte dysfunction. Blood 85, 1615–1619 (1995).
Patel, J. A., Nair, S., Revai, K., Grady, J. & Chonmaitree, T. Nasopharyngeal acute phase cytokines in viral upper respiratory infection: impact on acute otitis media in children. Pediatr. Infect. Dis. J. 28, 1002–1007 (2009).
Bakaletz, L. O. Immunopathogenesis of polymicrobial otitis media. J. Leukoc. Biol. 87, 213–222 (2010). This comprehensive review discusses the host innate and acquired immune response involved in the pathogenesis of AOM, including information on viral-induced pathological changes in the nasopharynx and the middle ear in animal models.
Avadhanula, V. et al. Respiratory viruses augment the adhesion of bacterial pathogens to respiratory epithelium in a viral species- and cell type-dependent manner. J. Virol. 80, 1629–1636 (2006).
Pittet, L. A., Hall-Stoodley, L., Rutkowski, M. R. & Harmsen, A. G. Influenza virus infection decreases tracheal mucociliary velocity and clearance of Streptococcus pneumoniae. Am. J. Respir. Cell Mol. Biol. 42, 450–460 (2010).
Buchman, C. A. & Brinson, G. M. Viral otitis media. Curr. Allergy Asthma Rep. 3, 335–340 (2003).
Revai, K., Patel, J. A., Grady, J. J. & Chonmatree, T. Tympanometric findings in young children during upper respiratory tract infections with and without acute otitis media. Pediatr. Infect. Dis. J. 27, 292–295 (2008).
Revai, K., Mamidi, D. & Chonmaitree, T. Association of nasopharyngeal bacterial colonization during upper respiratory tract infection and the development of acute otitis media. Clin. Infect. Dis. 46, e34–e37 (2008).
Canafax, D. M. et al. Amoxicillin middle ear fluid penetration and pharmacokinetics in children with acute otitis media. Pediatr. Infect. Dis. J. 17, 149–156 (1998).
Chonmaitree, T. et al. Virus and bacteria enhance histamine production in middle ear fluids of children with acute otitis media. J. Infect. Dis. 169, 1265–1270 (1994).
Chonmaitree, T. et al. Role of leukotriene B4 and interleukin-8 in acute bacterial and viral otitis media. Ann. Otol. Rhinol. Laryngol. 105, 968–974 (1996).
Jossart, G. H. et al. Effect of Streptococcus pneumoniae and influenza A virus on middle ear antimicrobial pharmacokinetics in experimental otitis media. Pharm. Res. 11, 860–864 (1994).
Chonmaitree, T., Ruohola, A. & Hendley, J. O. Presence of viral nucleic acids in the middle ear: acute otitis media pathogen or bystander? Pediatr. Infect. Dis. J. 31, 325–330 (2012).
Chonmaitree, T. et al. Symptomatic and asymptomatic respiratory viral infections in the first year of life: association with acute otitis media development. Clin. Infect. Dis. 60, 1–9 (2015).
Murphy, T. F. et al. Panel 5: microbiology and immunology panel. Otolaryngol. Head Neck Surg. 148, E64–E89 (2013).
Trune, D. R., Kempton, B., Hausman, F. A., Larrain, B. E. & MacArthur, C. J. Correlative mRNA and protein expression of middle and inner ear inflammatory cytokines during mouse acute otitis media. Hear. Res. 326, 49–58 (2015).
Leichtle, A., Lai, Y., Wollenberg, B., Wasserman, S. I. & Ryan, A. F. Innate signaling in otitis media: pathogenesis and recovery. Curr. Allergy Asthma Rep. 11, 78–84 (2011).
Kurabi, A., Pak, K., Ryan, A. F. & Wasserman, S. I. Innate Immunity: orchestrating inflammation and resolution of otitis media. Curr. Allergy Asthma Rep. 16, 6 (2016).
Mittal, R. et al. Role of innate immunity in the pathogenesis of otitis media. Int. J. Infect. Dis. 29, 259–267 (2014).
Morris, P. Chronic suppurative otitis media. BMJ Clin. Evid. 2012, 0507 (2012).
Mittal, R. et al. Current concepts in the pathogenesis and treatment of chronic suppurative otitis media. J. Med. Microbiol. 64, 1103–1116 (2015).
Elmorsy, S. et al. The role of IL8 in different types of otitis media and bacterialogical correlation. J. Int. Adv. Otol. 6, 269–273 (2010).
Si, Y. et al. Attenuated TLRs in middle ear mucosa contributes to susceptibility of chronic suppurative otitis media. Hum. Immunol. 75, 771–776 (2014).
Rye, M. S. et al. Unraveling the genetics of otitis media: from mouse to human and back again. Mamm. Genome 22, 66–82 (2011).
Mittal, R. et al. Immunity genes and susceptibility to otitis media: a comprehensive review. J. Genet. Genomics 41, 567–581 (2014).
Alper, C. M., Winther, B., Hendley, J. O. & Doyle, W. J. Cytokine polymorphisms predict the frequency of otitis media as a complication of rhinovirus and RSV infections in children. Eur. Arch. Otorhinolaryngol. 266, 199–205 (2009).
Shaikh, N. et al. Responsiveness and construct validity of a symptom scale for acute otitis media. Pediatr. Infect. Dis. J. 28, 9–12 (2009).
Rothman, R., Owens, T. & Simel, D. L. Does this child have acute otitis media? JAMA 289, 1633–1640 (2003).
Laine, M. K., Tähtinen, P. A., Ruuskanen, O., Huovinen, P. & Ruohola, A. Symptoms or symptom-based scores cannot predict acute otitis media at otitis-prone age. Pediatrics 125, 1154–1161 (2010).
Rosenfeld, R. M. Diagnostic certainty for acute otitis media. Int. J. Pediatr. Otorhinolaryngol. 64, 89–95 (2002).
Kaleida, P. H. et al. Mastering diagnostic skills: enhancing proficiency in otitis media, a model for diagnostic skills training. Pediatrics 124, e714–e720 (2009).
Pichichero, M. E. & Poole, M. D. Assessing diagnostic accuracy and tympanocentesis skills in the management of otitis media. Arch. Pediatr. Adolesc. Med. 155, 1137–1142 (2001).
Shaikh, N. et al. Development and preliminary evaluation of a parent-reported outcome instrument for clinical trials in acute otitis media. Pediatr. Infect. Dis. J. 28, 5–8 (2009).
Friedman, N. R. et al. Development of a practical tool for assessing the severity of acute otitis media. Pediatr. Infect. Dis. J. 25, 101–107 (2006).
Roland, P. S. et al. Clinical practice guideline: cerumen impaction. Otolaryngol. Head Neck Surg. 139, S1–S21 (2008).
McCormick, D. P., Lim-Melia, E., Saeed, K., Baldwin, C. D. & Chonmaitree, T. Otitis media: can clinical findings predict bacterial or viral etiology? Pediatr. Infect. Dis. J. 19, 256–258 (2000).
Karma, P. H., Penttilä, M. A., Sipilä, M. M. & Kataja, M. J. Otoscopic diagnosis of middle ear effusion in acute and non-acute otitis media. I. The value of different otoscopic findings. Int. J. Pediatr. Otorhinolaryngol. 17, 37–49 (1989).
Shaikh, N. et al. Otoscopic signs of otitis media. Pediatr. Infect. Dis. J. 30, 822–826 (2011).
Armengol, C. E. & Hendley, J. O. Shagrination during acute otitis media. J. Pediatr. 164, 870–870.e1 (2014).
Lundberg, T., Hellström, S. & Sandström, H. Development and validation of a new grading scale for otitis media. Pediatr. Infect. Dis. J. 32, 341–345 (2013).
McCormick, D. P. et al. Bullous myringitis: a case–control study. Pediatrics 112, 982–986 (2003).
Shekelle, P. et al. Diagnosis, Natural History and Late Effects of Otitis Media with Effusion: Evidence Report/Technology Assessment No. 55 (AHRQ Publication, 2003).
Jones, W. S. & Kaleida, P. H. How helpful is pneumatic otoscopy in improving diagnostic accuracy? Pediatrics 112, 510–513 (2003).
American Academy of Pediatrics. Section on Infectious Diseases. A view through the otoscope: distinguishing acute otitis media from otitis media with effusion. AAPhttp://www2.aap.org/sections/infectdis/video.cfm (accessed 5 January 2016).
Forrest, C. B. et al. Improving adherence to otitis media guidelines with clinical decision support and physician feedback. Pediatrics 131, e1071–e1081 (2013). This large primary care-based cluster RCT including 140,000 OM visits shows that clinical decision support and performance feedback improve adherence to OM guidelines.
Lannon, C., Peterson, L. E. & Goudie, A. Quality measures for the care of children with otitis media with effusion. Pediatrics 127, e1490–e1497 (2011).
Lee, D. H. How to improve the accuracy of diagnosing otitis media with effusion in a pediatric population. Int. J. Pediatr. Otorhinolaryngol. 74, 151–153 (2010).
Schilder, A. G., Zielhuis, G. A., Haggard, M. P. & van den Broek, P. Long-term effects of otitis media with effusion: otomicroscopic findings. Am. J. Otol. 16, 365–372 (1995).
Onusko, E. Tympanometry. Am. Fam. Physician 70, 1713–1720 (2004).
Takata, G. S. et al. Evidence assessment of the accuracy of methods of diagnosing middle ear effusion in children with otitis media with effusion. Pediatrics 112, 1379–1387 (2003).
Abbott, P., Rosenkranz, S., Hu, W., Gunsekera, H. & Reath, J. The effect and acceptability of tympanometry and pneumatic otoscopy in general practitioner diagnosis and management of childhood ear disease. BMC Fam. Pract. 15, 181 (2014).
American Speech-Language-Hearing Association. Guidelines for audiologic screening. 1. Guidelines for screening infants and children for outer and middle ear disorders, birth through 18 years. ASHAhttp://www.asha.org/policy/GL1997-00199/#sec1.3 (1997).
Hunter, L. L., Preve, B. A., Kei, J. & Sanford, C. A. Pediatric applications of wideband acoustic immittance measures. Ear Hear. 34 (Suppl. 1), 36S–42S (2013).
Combs, J. T. & Combs, M. K. Acoustic reflectometry: spectral analysis and the conductive hearing loss of otitis media. Pediatr. Infect. Dis. J. 15, 683–686 (1996).
Erkkola-Anttinen, N., Laine, M. K., Tähtinen, P. A. & Ruohola, A. Parental role in the diagnostics of otitis media: can layman parents use spectral gradient acoustic reflectometry reliably? Int. J. Pediatr. Otorhinolaryngol. 79, 1516–1521 (2015).
Chianese, J. et al. Spectral gradient acoustic reflectometry compared with tympanometry in diagnosing middle ear effusion in children aged 6 to 24 months. Arch. Pediatr. Adolesc. Med. 161, 884–888 (2007).
Muderris, T. et al. Consumer acoustic reflectometry: accuracy in diagnosis of otitis media with effusion in children. Int. J. Pediatr. Otorhinolaryngol. 77, 1771–1774 (2013).
Puhakka, T., Pulkkinen, J. U., Silvennoinen, H. & Heikkinen, T. Comparison of spectral gradient acoustic reflectometry and tympanometry for detection of middle-ear effusion in children. Pediatr. Infect. Dis. J. 33, e183–e186 (2014).
Simpson, S. A. et al. Identification of children in the first four years of life for early treatment for otitis media with effusion. Cochrane Database Syst. Rev. 1, CD004163 (2007).
Boone, R. T., Bower, C. M. & Martin, P. F. Failed newborn hearing screens as presentation for otitis media with effusion in the newborn population. Int. J. Pediatr. Otorhinolaryngol. 69, 393–397 (2005).
Holster, I. L., Hoeve, L. J., Wieringa, M. H., Willis-Lorrier, R. M. S. & de Gier, H. H. W. Evaluation of hearing loss after failed neonatal hearing screening. J. Pediatr. 155, 646–650 (2009).
Boudewyns, A. et al. Otitis media with effusion: an underestimated cause of hearing loss in infants. Otol. Neurotol. 32, 799–804 (2011).
Fortanier, A. C. et al. Pneumococcal conjugate vaccines for preventing otitis media. Cochrane Database Syst. Rev. 4, CD001480 (2014).
Eskola, J. et al. Efficacy of a pneumococcal conjugate vaccine against acute otitis media. N. Engl. J. Med. 344, 403–409 (2001).
Black, S. et al. Efficacy, safety and immunogenicity of heptavalent pneumococcal conjugate vaccine in children. Pediatr. Infect. Dis. J. 19, 187–195 (2000).
Casey, J. R., Adlowitz, D. G. & Pichichero, M. E. New patterns in the otopathogens causing acute otitis media six to eight years after introduction of pneumococcal conjugate vaccine. Pediatr. Infect. Dis. J. 29, 304–309 (2010).
Casey, J. R., Kaur, R., Friedel, V. C. & Pichichero, M. E. Acute otitis media otopathogens during 2008 to 2010 in Rochester, New York. Pediatr. Infect. Dis. J. 32, 805–809 (2013).
Shea, K. M., Weycker, D., Stevenson, A. E., Strutton, D. R. & Pelton, S. I. Modeling the decline in pneumococcal acute otitis media following the introduction of pneumococcal conjugate vaccines in the US. Vaccine 29, 8042–8048 (2011).
Dagan, R., Pelton, S., Bakaletz, L. & Cohen, R. Prevention of early episodes of otitis media by pneumococcal vaccines might reduce progression to complex disease. Lancet Infect. Dis. 16, 480–492 (2016). This review provides evidence to support the hypothesis that the prevention of vaccine serotype pneumococcal OM in early life leads to a reduction of subsequent and more-complex disease caused by non-vaccine serotypes and non-typeable H. influenzae.
Ben-Shimol, S. et al. Near-elimination of otitis media caused by 13-valent pneumococcal conjugate vaccine (PCV) serotypes in southern Israel shortly after sequential introduction of 7-valent/13-valent PCV. Clin. Infect. Dis. 59, 1724–1732 (2014).
Veenhoven, R. et al. Effect of conjugate pneumococcal vaccine followed by polysaccharide pneumococcal vaccine on recurrent acute otitis media: a randomised study. Lancet 361, 2189–2195 (2003).
Prymula, R. et al. Pneumococcal capsular polysaccharides conjugated to protein D for prevention of acute otitis media caused by both Streptococcus pneumoniae and non-typable Haemophilus influenzae: a randomised double-blind efficacy study. Lancet 367, 740–748 (2006).
van den Bergh, M. R. et al. Effects of the 10-valent pneumococcal nontypeable Haemophilus influenzae protein D-conjugate vaccine on nasopharyngeal bacterial colonization in young children: a randomized controlled trial. Clin. Infect. Dis. 56, e30–e39 (2013).
Tregnaghi, M. W. et al. Efficacy of pneumococcal nontypable Haemophilus influenzae protein D conjugate vaccine (PHiD-CV) in young Latin American children: a double-blind randomized controlled trial. PLoS Med. 11, e1001657 (2014).
Heikkinen, T. et al. Influenza vaccination in the prevention of acute otitis media in children. Am. J. Dis. Child. 145, 445–448 (1991).
Clements, D. A., Langdon, L., Bland, C. & Walter, E. Influenza A vaccine decreases the incidence of otitis media in 6- to 30-month old children in day care. Arch. Pediatr. Adolesc. Med. 149, 113–117 (1995).
Belshe, R. B. et al. Live attenuated versus inactivated influenza vaccine in infants and young children. N. Engl. J. Med. 356, 685–696 (2007).
Block, S. L., Heikkinen, T., Toback, S. L., Zheng, W. & Ambrose, C. S. The efficacy of live attenuated influenza vaccine against influenza associated acute otitis media in children. Pediatr. Infect. Dis. J. 30, 203–207 (2011).
Norhayati, M. N., Ho, J. J. & Azman, M. Y. Influenza vaccines for preventing acute otitis media in infants and children. Cochrane Database Syst. Rev. 3, CD010089 (2015).
Committee on Infectious Diseases, American Academy of Pediatrics. Recommendations for prevention and control of influenza in children, 2015–2016. Pediatrics 136, 792–808 (2015).
NHS. Children's flu vaccine. NHShttp://www.nhs.uk/conditions/vaccinations/pages/which-children-are-eligible-for-the-flu-vaccine.aspx (2016).
Rijksinstituut voor Volksegezondheid en Milieu/LCI. Richtlijn Influenza (ed. Meijer, A. ) 1–19 (2003).
Koivunen, P., Kontiokari, T., Neimelä, M., Pokka, T. & Uhari, M. Time to development of acute otitis media during an upper respiratory tract infection in children. Pediatr. Infect. Dis. J. 18, 303–305 (1999).
Winther, B., Block, S. L., Reisinger, K. & Dutkowski, R. Impact of oseltamivir treatment on the incidence and course of acute otitis media in children with influenza. Int. J. Pediatr. Otorhinolaryngol. 74, 684–688 (2010).
Heinonen, S. et al. Early oseltamivir treatment of influenza in children 1–3 years of age: a randomized controlled trial. Clin. Infect. Dis. 51, 887–894 (2010).
Jefferson, T. et al. Neuraminidase inhibitors for preventing and treating influenza in adults and children. Cochrane Database Syst. Rev. 4, CD008965 (2014).
Schapowal, A., Klein, P. & Johnston, S. L. Echinacea reduces the risk of recurrent respiratory tract infections and complications: a meta-analysis of randomized controlled trials. Adv. Ther. 32, 187–200 (2015).
Uhari, M., Kontiokari, T., Koskela, M. & Niemelä, M. Xylitol chewing gum in prevention of acute otitis media: double blind randomised trial. BMJ 9, 1180–1184 (1996).
Azarpazhooh, A., Limeback, H., Lawrence, H. P. & Shah, P. S. Xylitol for preventing acute otitis media in children up to 12 years of age. Cochrane Database Syst. Rev. 11, CD007095 (2011).
Vernacchio, L. et al. Xylitol syrup for the prevention of acute otitis media. Pediatrics 133, 289–295 (2014).
Niittynen, L., Pitkäranta, A. & Korpela, R. Probiotics and otitis media in children. Int. J. Pediatr. Otorhinolaryngol. 76, 465–470 (2012).
Kumpu, M. et al. The use of the probiotic Lactobacillus rhamnosus GG and viral findings in the nasopharynx of children attending day care. J. Med. Virol. 85, 1632–1638 (2013).
Luoto, R. et al. Prebiotic and probiotic supplementation prevents rhinovirus infections in preterm infants: a randomized, placebo-controlled trial. J. Allergy Clin. Immunol. 133, 405–413 (2014).
Liu, S., Hu, P., Du, X., Zhou, T. & Pei, X. Lactobacillus rhamnosus GG supplementation for preventing respiratory infections in children: a meta-analysis of randomized, placebo-controlled trials. Indian Pediatr. 50, 377–381 (2013).
Uhari, M., Mäntysaari, K. & Niemelä, M. A meta-analytic review of the risk factors for acute otitis media. Clin. Infect. Dis. 22, 1079–1083 (1996).
Daly, K. A. & Giebink, G. S. Clinical epidemiology of otitis media. Pediatr. Infect. Dis. J. 19, S31–S36 (2000).
Nelson, A. M. A comprehensive review of evidence and current recommendations related to pacifier usage. J. Pediatr. Nurs. 27, 690–699 (2012).
Bertin, L. et al. A randomized, double-blind, multicentre controlled trial of ibuprofen versus acetaminophen and placebo for symptoms of acute otitis media in children. Fundam. Clin. Pharmacol. 10, 387–392 (1996).
Foxlee, R. et al. Topical analgesia for acute otitis media. Cochrane Database Syst. Rev. 3, CD005657 (2006).
ISRCTN Registry. Children's drops for ear pain in acute otitis media: the CEDAR randomised controlled trial. ISRCTNhttp://www.isrctn.com/ISRCTN09599764 (2014).
Venekamp, R. P., Sanders, S., Glasziou, P. P., Del Mar, C. B. & Rovers, M. M. Antibiotics for acute otitis media in children. Cochrane Database Syst. Rev. 6, CD000219 (2015).
Costelloe, C., Metcalfe, C., Lovering, A., Mant, D. & Hay, D. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ 340, c2096 (2010).
Rovers, M. M. et al. Antibiotics for acute otitis media: a meta-analysis with individual patient data. Lancet 368, 1429–1435 (2006). This novel approach meta-analysis of individual patient data from six RCT trials provides important information on subgroups of children with AOM who benefit more or less from oral antibiotics.
Centre for Clinical Practice at NICE (UK). Respiratory tract infections — antibiotic prescribing: prescribing of antibiotics for self-limiting respiratory tract infections in adults and children in primary care. NICEhttp://www.ncbi.nlm.nih.gov/books/NBK53632/ (2008).
Venekamp, R. P., Damoiseaux, R. A. & Schilder, A. G. Acute otitis media in children. BMJ Clin. Evid.http://clinicalevidence.bmj.com/x/systematic-review/0301/overview.html (2014).
Coleman, C. & Moore, M. Decongestants and antihistamines for acute otitis media in children. Cochrane Database Syst. Rev. 3, CD001727 (2008).
Chonmaitree, T. et al. A randomized, placebo-controlled trial of the effect of antihistamine or corticosteroid treatment in acute otitis media. J. Pediatr. 143, 377–385 (2003).
van Buchem, F. L., Dunk, J. H. & van't Hof, M. A. Therapy of acute otitis media: myringotomy, antibiotics, or neither? A double blind study in children. Lancet 318, 883–887 (1981). This is one of the first RCTs in the field of OM providing evidence that myringotomy (tympanocentesis; commonly practiced at the time) is not effective as a treatment modality in children with AOM.
Engelhard, D. et al. Randomised study of myringotomy, amoxicillin/clavulanate, or both for acute otitis media in infants. Lancet 2, 141–143 (1989).
Kaleida, P. H. et al. Amoxicillin or myringotomy or both for acute otitis media: results of a randomised clinical trial. Pediatrics 87, 466–474 (1991).
Leach, A. J. & Morris, P. S. Antibiotics for the prevention of acute and chronic suppurative otitis media in children. Cochrane Database Syst. Rev. 4, CD00440 (2006).
McDonald, S., Langton Hewer, C. D. & Nunez, D. A. Grommets (ventilation tubes) for recurrent acute otitis media in children. Cochrane Database Syst. Rev. 4, CD004741 (2008).
Hellström, S. et al. Ventilation tube treatment: a systematic review of the literature. Otolaryngol. Head Neck Surg. 145, 383–395 (2011).
Lous, J., Ryborg, C. T. & Thomsen, J. L. A systematic review of the effect of tympanostomy tubes in children with recurrent acute otitis media. Int. J. Pediatr. Otorhinolaryngol. 75, 1058–1061 (2011).
Rosenfeld, R. M. et al. Clinical practice guideline: tympanostomy tubes in children. Otolaryngol. Head Neck Surg. 149, S1–35 (2013).
Boonacker, C. W. et al. Adenoidectomy with or without grommets for children with otitis media: an individual patient data meta-analysis. Health Technol. Assess. 18, 1–118 (2014).
Griffin, G. & Flynn, C. A. Antihistamines and/or decongestants for otitis media with effusion (OME) in children. Cochrane Database Syst. Rev. 9, CD003423 (2011).
Simpson, S. A., Lewis, R., van der Voort, J. & Butler, C. C. Oral or topical nasal steroids for hearing loss associated with otitis media with effusion in children. Cochrane Database Syst. Rev. 5, CD001935 (2011).
Venekamp, R. P. et al. Antibiotics for otitis media with effusion in children. Cochrane Database Syst. Rev. 6, CD009163 (2016).
National Institute for Health and Clinical Excellence. Surgical management of otitis media with effusion in children. NICE Clinical Guideline 60. Developed by the National Collaborating Centre for Women's and Children's Health. NICEhttp://www.nice.org.uk/nicemedia/pdf/CG60NICEguideline.pdf (2008).
Rovers, M. M. et al. Grommets in otitis media with effusion: an individual patient data meta-analysis. Arch. Dis. Child. 90, 480–485 (2005).
Williamson, I. et al. An open randomised study of autoinflation in 4- to 11-year-old school children with otitis media with effusion in primary care. Health Technol. Assess. 19, 1–150 (2015).
ISRCTN Registry. Oral steroids for resolution of otitis media with effusion in children. ISRCTNhttp://www.isrctn.com/ISRCTN49798431 (2012).
Miller, B. J. & Elhassan, H. A. Balloon dilatation of the Eustachian tube: an evidence-based review of case series for those considering its use. Clin. Otolaryngol. 38, 525–532 (2013).
Kay, D. J., Nelson, M. & Rosenfeld, R. M. Meta-analysis of tympanostomy tube sequelae. Otolaryngol. Head Neck Surg. 124, 374–380 (2001).
van Dongen, T. M., van der Heijden, G. J., Freling, H. G., Venekamp, R. P. & Schilder, A. G. Parent-reported otorrhea in children with tympanostomy tubes: incidence and predictors. PLoS ONE 8, e69062 (2013).
Ah-Tye, C., Paradise, J. L. & Colborn, D. K. Otorrhea in young children after tympanostomy-tube placement for persistent middle-ear effusion: prevalence, incidence, and duration. Pediatrics 107, 1251–1258 (2001).
Syed, M. I., Suller, S., Browning, G. G. & Akeroyd, M. A. Interventions for the prevention of postoperative ear discharge after insertion of ventilation tubes (grommets) in children. Cochrane Database Syst. Rev. 4, CD008512 (2013).
Van Dongen, T. M. et al. Acute otorrhea in children with tympanostomy tubes: prevalence of bacteria and viruses in the post-pneumococcal conjugate vaccine era. Pediatr. Infect. Dis. J. 34, 355–360 (2015).
van Dongen, T. M., van der Heijden, G. J., Venekamp, R. P., Rovers, M. M. & Schilder, A. G. A trial of treatment for acute otorrhea in children with tympanostomy tubes. N. Engl. J. Med. 370, 723–733 (2014). This landmark RCT provides evidence that topical antibiotics are more effective than oral antibiotics and initial observation in children with ventilation tubes who develop acute ear discharge.
van Dongen, T. M., Schilder, A. G., Venekamp, R. P., de Wit, G. A. & van der Heijden, G. J. Cost-effectiveness of treatment of acute otorrhea in children with tympanostomy tubes. Pediatrics 135, e1182–e1189 (2015).
Roland, P. S. et al. Topical ciprofloxacin/dexamethasone otic suspension is superior to ofloxacin otic solution in the treatment of children with acute otitis media with otorrhea through tympanostomy tubes. Pediatrics 113, e40–e46 (2004).
Roland, P. S. et al. Topical ciprofloxacin/dexamethasone is superior to ciprofloxacin alone in pediatric patients with acute otitis media and otorrhea through tympanostomy tubes. Laryngoscope 113, 2116–2122 (2003).
Macfadyen, C. A., Acuin, J. M. & Gamble, C. L. Systemic antibiotics versus topical treatments for chronically discharging ears with underlying eardrum perforations. Cochrane Database Syst. Rev. 1, CD005608 (2006).
Macfadyen, C. A., Acuin, J. M. & Gamble, C. L. Topical antibiotics without steroids for chronically discharging ears with underlying eardrum perforations. Cochrane Database Syst. Rev. 4, CD004618 (2005).
Pappas, S. et al. Topical antibiotic ear drops: are they safe? Int. J. Clin. Pract. 60, 115–119 (2006).
Iacovou, E., Vlastarakos, P. V., Papacharalampous, G., Kyrodimos, E. & Nikolopoulos, T. P. Is cartilage better than temporalis muscle fascia in type I tympanoplasty? Implications for current surgical practice. Eur. Arch. Otorhinolaryngol. 270, 2803–2813 (2013).
Mohamad, S. H., Khan, I. & Hussain, S. S. Is cartilage tympanoplasty more effective than fascia tympanoplasty? A systematic review. Otol. Neurotol. 33, 699–705 (2012).
Klein, J. O. The burden of otitis media. Vaccine 19, S2–S8 (2001).
Dakin, H., Petrou, S., Haggard, M., Benge, S. & Williamson, I. Mapping analyses to estimate health utilities based on responses to the OM8-30 otitis media questionnaire. Qual. Life Res. 19, 65–80 (2010).
Sneeuw, K. C., Sprangers, M. A. & Aaronson, N. K. The role of health care providers and significant others in evaluating the quality of life of patients with chronic disease. J. Clin. Epidemiol. 55, 1130–1143 (2002).
Rosenfeld, R. M., Goldsmith, A. J., Tetlus, L. & Balzano, A. Quality of life for children with otitis media. Arch. Otolaryngol. Head Neck Surg. 123, 1049–1054 (1997).
Milovanovic, J. et al. Precision-scored parental report questions and HL-scaled tympanometry as informative measures of hearing in otitis media 1: large-sample evidence on determinants and complementarity to pure-tone audiometry. Int. J. Pediatr. Otorhinolaryngol. 83, 113–131 (2016).
Phillips, J. S., Haggard, M. & Yung, M. A new health-related quality of life measure for active chronic otitis media (COMQ-12): development and initial validation. Otol. Neurotol. 35, 454–458 (2014).
Bellussi, L. et al. Quality of life and psycho-social development in children with otitis media with effusion. Acta Otorhinolaryngol. Ital. 25, 359–364 (2005).
Hall, A. J., Maw, R., Midgley, E., Golding, J. & Steer, C. Glue ear, hearing loss and IQ: an association moderated by the child's home environment. PLoS ONE 9, e87021 (2014).
Goldberg, D. P. & Hillier, V. F. A scaled version of the General Health Questionnaire. Psychol. Med. 9, 139–145 (1979).
Chow, Y., Wabnitz, D. A. & Ling, J. Quality of life outcomes after ventilating tube insertion for otitis media in an Australian population. Int. J. Pediatr. Otorhinolaryngol. 71, 543–547 (2007).
Streiner, D. L., Norman, G. R. & Cairney, J. Health Measurement Scales: a Practical Guide to Their Development and Use (Oxford Univ. Press, 2014).
Heidemann, C. H. et al. The Otitis Media-6 questionnaire: psychometric properties with emphasis on factor structure and interpretability. Health Qual. Life Outcomes 11, 201 (2013).
Boruk, M., Lee, P., Faynzilbert, Y. & Rosenfeld, R. Caregiver well-being and child quality of life. Otolaryngol. Head Neck Surg. 136, 159–168 (2007).
Ryborg, C. T. et al. Quality of life in children with otitis media — a cohort study. Fam. Pract. 31, 30–37 (2014).
Brouwer, C. N. M. et al. The impact of recurrent acute otitis media on the quality of life of children and their caregivers. Clin. Otolaryngol. 30, 258–265 (2005).
Kujala, T. et al. Quality of life after surgery for recurrent otitis media in a randomized controlled trial. Pediatr. Infect. Dis. J. 33, 715–719 (2014).
Brouwer, C. N. et al. Effect of pneumococcal vaccination on quality of life in children with recurrent acute otitis media: a randomized, controlled trial. Pediatrics 115, 273–279 (2005).
Pettigrew, M. M. et al. Viral–bacterial interactions and risk of acute otitis media complicating upper respiratory tract infection. J. Clin. Microbiol. 49, 3750–3755 (2011).
Marom, T. et al. Complementary and alternative medicine treatment options for otitis media: a systematic review. Medicine (Baltimore) 95, e2695 (2016).
Sanford, C. A., Schooling, T. & Frymark, T. Determining the presence of absence of middle ear disorders: an evidence-based systematic review on the diagnostic accuracy of selected assessment instruments. Am. J. Audiol. 21, 251–268 (2012).
Liu, K., Casey, J. & Pichichero, M. Serum intercellular adhesion molecule 1 variations in young children with acute otitis media. Clin. Vaccine Immunol. 17, 1909–1916 (2010).
Liu, K. & Pichichero, M. E. Clinical significance of serum S100A12 in acute otitis media in young children. Pediatr. Infect. Dis. J. 31, e56–e58 (2012).
Patel, J. A. et al. Systemic cytokine response profiles associated with respiratory virus-induced acute otitis media. Pediatr. Infect. Dis. J. 28, 407–411 (2009).
Liu, K., Kaur, R., Almudevar, A. & Pichichero, M. E. Higher serum levels of interleukin 10 occur at onset of acute otitis media caused by Streptococcus pneumoniae compared to Haemophilus influenzae and Moraxella catarrhalis. Laryngoscope 123, 1500–1505 (2013).
Pichichero, M. E. & Almudevar, A. Serum cytokine biomarkers accurately predict presence of acute otitis media infection and recovery caused by Haemophilus influenzae. Int. J. Pediatr. Otorhinolaryngol. 83, 200–204 (2016).
Ede, L. C., O'Brien, J., Chonmaitree, T., Han, Y. & Patel, J. A. Lactate dehydrogenase as a marker of nasopharyngeal inflammatory injury during viral upper respiratory infection: implications for acute otitis media. Pediatr. Res. 73, 349–354 (2013).
Pettigrew, M. M. et al. Panel 6: vaccines. Otolaryngol. Head Neck Surg. (in the press).
Daniels, C. C., Rogers, P. D. & Shelton, C. M. A. Review of pneumococcal vaccines: current polysaccharide vaccine recommendations and future protein antigens. J. Pediatr. Pharmacol. Ther. 21, 27–35 (2016).
Murphy, T. F. Vaccines for nontypeable Haemophilus influenzae: the future Is now. Clin. Vaccine Immunol. 22, 459–466 (2015).
Cripps, A. W. & Otczyk, D. C. Prospects for a vaccine against otitis media. Expert Rev. Vaccines 5, 517–534 (2006).
Murphy, T. F., Bakaletz, L. O., Kyd, J. M., Watson, B. & Klein, D. L. Vaccines for otitis media: proposals for overcoming obstacles to progress. Vaccine 23, 2696–2702 (2005).
Murphy, T. F. Vaccine development for non-typeable Haemophilus influenzae and Moraxella catarrhalis: progress and challenges. Expert Rev. Vaccines 4, 843–853 (2005).
Mazur, N. I. et al. Lower respiratory tract infection caused by respiratory syncytial virus: current management and new therapeutics. Lancet Respir. Med. 11, 888–900 (2015).
Venekamp, R. P., Prasad, V. & Hay, A. D. Are topical antibiotics an alternative to oral antibiotics for children with acute otitis media and ear discharge? BMJ 352, i308 (2016).
Khoo, X. et al. Formulations for trans-tympanic antibiotic delivery. Biomaterials 34, 1281–1288 (2013).
International Society for Otitis Media. 18th International Symposium on Recent Advances in Otitis Media (ISOM, 2015).
Hong, P., Bance, M. & Gratzer, P. F. Repair of tympanic membrane perforation using novel adjuvant therapies: a contemporary review of experimental and tissue engineering studies. Int. J. Pediatr. Otorhinolaryngol. 77, 3–12 (2013).
Kanemaru, S. et al. Regenerative treatment for tympanic membrane perforation. Otol. Neurotol. 32, 1218–1223 (2011).
Harman, N. L. et al. The importance of integration of stakeholder views in core outcome set development: otitis media with effusion in children with cleft palate. PLoS ONE 10, e0129514 (2015).
Lehmann, D. et al. The Kalgoorlie Otitis Media Research Project: rationale, methods, population characteristics and ethical considerations. Paediatr. Perinat Epidemiol. 22, 60–71 (2008).
Wiertsema, S. P. & Leach, A. J. Theories of otitis media pathogenesis, with a focus on Indigenous children. Med. J. Aust. 191, S50–S54 (2009).
Vijayasekaran, S. et al. New findings in the pathogenesis of otitis media. Laryngoscope 122, S61–S62 (2012).
Onerci, M. in Diagnosis in Otorhinolaryngology: an Illustrated Guide Ch. 1 (ed. Onerci, M. ) (Springer, 2010).
Leibovitz, E. et al. Is bilateral acute otitis media clinically different than unilateral acute otitis media? Pediatr. Infect. Dis. J. 26, 589–592 (2007).
McCormick, D. P., Chandler, S. M. & Chonmaitree, T. Laterality of acute otitis media: different clinical and microbiological characteristics. Pediatr. Infect. Dis. J. 26, 583–588 (2007).
Uitti, J. M., Laine, M. K., Tähtinen, P. A., Ruuskanen, O. & Ruohola, A. Symptoms and otoscopic signs in bilateral and unilateral acute otitis media. Pediatrics 131, e398–e405 (2013).
Acknowledgements
A.G.M.S. leads the evidENT team at University College London (UCL), UK, which is supported by a National Institute for Health Research (NIHR), Research Professorship Award. T.C. is supported, in part, by grants R01 DC005841 and UL1 TR001439 from the US NIH.
Author information
Authors and Affiliations
Contributions
Introduction (A.G.M.S. and R.P.V.); Epidemiology (M.L.C.); Mechanisms/pathophysiology (A.W.C. and T.C.); Diagnosis, screening and prevention (R.M.R. and T.C.); Management (A.G.M.S. and R.P.V.); Quality of life (M.P.H.); Outlook (all authors); Overview of Primer (A.G.M.S.).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Schilder, A., Chonmaitree, T., Cripps, A. et al. Otitis media. Nat Rev Dis Primers 2, 16063 (2016). https://doi.org/10.1038/nrdp.2016.63
Published:
DOI: https://doi.org/10.1038/nrdp.2016.63