Abstract
Antimicrobial resistance (AMR) is a global public health issue. Rapid and accurate antimicrobial susceptibility tests (AST) on bacteria isolates would facilitate appropriate choice of antibiotics, in which patients receive appropriate treatment and the emergence of multidrug-resistant organisms could be prevented simultaneously. In this study, we have developed a microfluidic device named Self Dilution for Faster Antimicrobial Susceptibility Testing (SDFAST). This SlipChip-based device consists of two layers of microchips, allowing injection of bacterial suspension and antibiotics by simply connecting the two chips. By slipping one microchip against another in a single press of the microchip, the antibiotics can be diluted within seconds and be well mixed with bacterial samples. By combining SDFAST with a water-soluble tetrazolium salt-8 (WST-8) assay, a range of clinically prevalent bacteria, including Acinetobacter baumannii, Escherichia coli, Klebsiella pneumoniae, and Staphylococci species, were tested under various antibiotics. Color analysis after 4–6 h of incubation showed an abrupt change in the WST-8 color of certain wells with diluted antibiotics, proving that instrument-free and immediate identification of minimum inhibitory concentration (MIC) could be achieved. The testing on 51 clinical isolates had an agreement of 92%, proving the accuracy of our method. These results validated its advantages of simple operation, rapid testing, and low sample consumption comparing to conventional methods, which require 16–24 h of incubation. Therefore, our method shows great potential to be further developed into a medical instrument for automated medical testing and point-of-care diagnosis.

Similar content being viewed by others
Introduction
Antimicrobial resistance (AMR) has been one of humanity’s major health threats in the 21st Century. It was estimated that AMR had contributed to 1.14 million deaths directly and 4.71 million in total in 2021, with, Staphylococcus aureus (S. aureus), Acinetobacter baumannii (A. baumannii) and Escherichia coli (E. coli) becoming few of the most important pathogens1. Even worse, with the outbreak of a pandemic such as coronavirus disease 2019, AMR has further been aggravated due to the overestimation of co-infection by bacteria and viruses in patients and resultant unnecessary prescription of antibiotics2. Consequently, such an exacerbation must be halted. To alleviate its threat, the determination of the minimum inhibitory concentration (MIC), the minimum concentration of an antibiotic that inhibits the visible growth of a bacterial species after overnight incubation via antimicrobial susceptibility tests (AST), is a gold-standard approach3. If MICs of antibiotics could be determined accurately in a short period of time, antibiotics of appropriate concentrations could be prescribed to patients to prevent overdosage, thus mitigating the AMR.
Currently, AST is performed either using an agar-based or broth microdilution method. The agar-based method is widely utilized, but it can only provide qualitative determination of bacterial susceptibility: The bacteria are designated to be “resistant”, “intermediate”, or “susceptible” from the results. In comparison, the broth microdilution method can provide more accurate MIC determination. A bacterial solution of the same concentration is reacted with antibiotics with different concentrations, and the MIC is determined by identifying the well with the lowest concentration of antibiotic showing no or little turbidity4. Meanwhile, both methods bear significant demerits. One major problem is the long incubation time, which is typically 16–24 h5,6. The long incubation time leads to a delay in the reporting of AST results, which in turn delays the time to appropriate treatment, especially when the patient is infected with an antibiotic-resistant strain. Moreover, both methods need to be performed in well-equipped clinical or microbiology laboratories, limiting their widespread use. There is an urgent clinical need to develop an alternative AST that is portable, technically simple, quantitative and with a short turn-around time.
To achieve so, several types of microfluidics-based platforms have been experimented with in the past, including microchips7,8, droplet-based platforms9,10,11, microchannels12,13, dipsticks (lab-on-a-stick)14, and discs (lab-on-a-disc)15. The advantages of microfluidics technology have been demonstrated over conventional methods, exhibiting excellent potential for point-of-care testing (POCT)6,16. For instance, they have high throughput and can be automated easily to perform testing on many samples, reducing the errors due to manual operation17; they require low volumes of samples and chemicals that reduce the waste of medical resources. Nonetheless, the development of such platforms faces various challenges. Despite high accuracy, microfluidic devices relying on optical/fluorescence detection or observation of individual bacterium have to be operated with costly and/or bulky equipment like spectrometers and microscopes, limiting their possibility of remote testing. These methods also require expertise in microbiology to operate, making them less user-friendly. On the other hand, devices like dipsticks and discs are portable and more user-friendly, but they could suffer from lower sensitivity. In this study, we aim to exploit the characteristics of the microfluidic chips while improving the possibility of applying such devices in POCT. Especially, we have investigated SlipChip, a microfluidic gadget that generates and dilutes droplets by sliding two chips with complementary designs. Using no pumps or valves, it can accomplish multiplexed microfluidic processes and can be preloaded with reagents or user-loaded on-site, depending on the application18.
The feasibility of SlipChip AST has been previously demonstrated, albeit with some demerits: a recent study presented a phenotypic AST using gradient-droplet SlipChip. It generated accurate colorimetric results from mixing E. coli, of both reference strains and clinical isolates from patients with urinary tract infections (UTIs), with four antibiotics respectively19. However, the antibiotics had to be diluted in the device by diffusion for 24 h, which was time-consuming and inflexible when a wider range of antibiotics had to be tested. Another study showed that SlipChip could be applied in AST on blood samples20: the device integrated dielectrophoresis, SlipChip, and preloaded multiplex array PCR. E. coli and S. aureus in blood cultures were incubated with antibiotics, and the MIC values or ranges were obtained by entropy-based image analysis. The device proved to be more precise and accurate compared to the broth microdilution method, while it was unfriendly to non-professionals as it required complicated calculations and image analysis. Moreover, previous studies mostly focused on a few most prominent species with small ranges of MICs, while in clinical settings, the testing conditions can be more complex. This includes a wide variety of bacterial species and a large range of MICs, as well as the situation when bacterial species with small MIC differences needed to be differentiated.
Therefore, in this study, we introduce SDFAST (Self Dilution for Faster Antimicrobial Susceptibility Testing), which can tackle the disadvantages of both conventional methods and previous SlipChip AST studies. Compared to conventional methods, we incorporate the microchips with the colorimetric water-soluble tetrazolium salt-8 (WST-8) assay21, and the device can generate results after 4–6 h of incubation, which was a significant reduction in turn-around-time (Fig. 1). Conventional methods rely on changes in turbidity or inhibition zones on agar. When there is a small difference in MICs (≤1 µg/mL) between two samples, it is difficult to identify it from these indicators. In comparison, colorimetric assay shows characteristic color changes that can be easily identified. To illustrate, a comparative study between the CCK-8 assay and disc diffusion proves that the colorimetric assay was sensitive to the growth of drug resistance as drug concentrations increased by 10-fold, while the changes in inhibition zones were obscure22. Also, it is easy to quantify the color changes at low costs. In our study, we analyzed the color intensity in each well on ImageJ, a free image processing program. In the POC setting, this can be carried out by simple photographers like smartphones, and deep learning23. These features ensure the accuracy of our method.
Schematic diagram of comparison between SDFAST and current method (e.g., disc diffusion). One of the main disadvantages of the current method is the long duration of testing, especially that incubation requires over 20 h. In SDFAST, however, incubation is shortened to 4–6 h, which allows doctors to obtain rapid AST results and prescribe corresponding antibiotics to patients in one day. In the diagram, a part of the SDFAST is shown to demonstrate how the test of one bacteria-antibiotic combination is carried out
Compared to previous studies, our design can achieve “self-diluting”, which means serial dilution of antibiotics is carried out within the microfluidic system, and the time for such a process is only in seconds. This feature removes the need for diluting and injecting antibiotics outside of the system manually, or waiting overnight for automatic dilution within the system. Our study has addressed two POCT issues. First, we overcome the user-friendly limitation by utilizing a sensitive colorimetric assay and ImageJ analysis, which can be mastered by non-professionals shortly24. Second, we have demonstrated that our device can be used for a wide range of samples, with variations in bacterial species and MIC ranges. It is also possible to apply the device for overall MIC detection with multiple species25. We have demonstrated the capability of SDFAST and its potential in POCT. For instance, a patient’s sample could be tested with multiple antibiotics to determine the optimal prescription or multiple samples could be tested with a particular antibiotic to examine its efficacy regularly. The AST could be completed within the same day of sample submission, allowing quick prescriptions and updates on antibiotic efficacies after obtaining results.
Materials and methods
Device design and fabrication
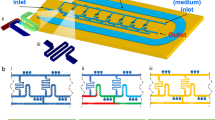
The SDFAST device (Fig. 2a) consisted of a top chip (Fig. 2b), serving as a lid to keep the system sealed, and a bottom chip (Fig. 2c), serving as wells holding the droplets. There were ten rows of discrete wells on each chip, and eight of them formed four bacteria-antibiotic combinations, allowing four tests to be carried out simultaneously. After combining the two chips with a complementary design, the originally discrete wells were connected to form channels that were ready for solution injection. The bottom chip consisted of nanowalls of the same size that hold a constant volume of droplets. The top chip consisted of wells of different sizes, and the volume of droplets in the wells decreased by one-half for each successive well (Fig. 2d–f). All the wells were connected with an inlet connecting channels and an outlet.
Dimensions and wells responsible for in-system dilution. a A photo of the SDFAST device. The device consists of b a top chip and c a bottom chip. The purple frames highlight two lines of wells that are responsible for in-system dilution, demonstrated in (d): the top chip consists of lines of wells with decreasing volumes from left to right, while the bottom chip consists of those with constant volumes. During slip, the wells of the top chip formed droplets with decreasing volumes, diluting the solution. Meanwhile, those of the bottom chip formed droplets of constant volumes. After slipping, the droplets from both chips merge together. This process is further shown in (e), a cross-section of the two chips. The respective dimensions are listed in (f). The 3D models were built using Blender 4.1
Both chips were fabricated from a 3 mm thick poly(methyl methacrylate) (PMMA) sheet with the help of the micro-milling machine. PMMA was utilized due to its excellent optical properties, suitable hardness with resistance to scratching, as well as its high impact strength and dimensional stability26. Micro-milling instead of current chemical etching methods was selected for fabrication due to the higher speed and flexibility27: Each set of chips can be fabricated in as short as under 30 min, and the parameters can be easily modified with the system application on the computer.
There were 5 steps in the fabrication process: (1) prototyping, (2) converting into respective toolpaths, (3) drilling of inlets and outlets, (4) milling of wells on chips, and (5) cutting out and cleaning the final product. The design was first made using AutoCAD software, which was only based on the top view since the micro-milling applications only accept 2.5D objects. Converted into dxf. file format, the file was imported into the micro-milling software, which converted the design into a CAM diagram in the user interface. Several operations were done to generate the required tool paths. The inlets and outlets were assigned to the 2.5D drilling layer, whereas the wells were assigned to the 2.5D milling layer. The cutting areas were converted into polygons for the machine to accept them as 3D objects. Each component’s height was then defined via the 2.5D blind function. The 2.5D cutting function was then used to generate the toolpaths. Suitable tools were selected so that the patterns could be appropriately fabricated, and the toolpaths were ready for fabrication. After calibrating the distance between the material surface and the tooltip, the machine started the drilling and milling processes: the drilling of the inlets and outlets on the chips was done using the 0.9 mm spiral drilling tool, followed by the milling of wells on the chips using the 0.5 mm End Mill tool. The fabricated chips were then cut out of the PMMA sheet using 1 mm/2 mm End Mill tools. Upon the completion of all the toolpaths, the chips were removed from the machine using a pair of clean forceps. The surface of the chips was first cleaned by compressed air to remove dirt and extra debris, then rinsed with deionized water and ethanol, and finally dried by compressed air.
Working principle
The working principle of the device involved three phases: loading, droplet formation, and mixing, in which two types of solutions (demonstrated by red and green food dyes in Fig. 3a) were diluted and mixed as droplets. During the loading phase (Fig. 3ai), the inlets, outlets, and wells were aligned by assembling the chips, forming a fluidic path along each line of wells. The solutions were then injected into the wells by inserting a pipette tip into the inlet, filling up the lines of wells entirely (Movie 1). The outlets were left open in the loading phase to facilitate pressure dissipation, and extra solutions could escape from them. During the droplet formation phase (Fig. 3aii), the top chip was pushed, which allowed independent droplets to be formed, and the inlets and outlets were disconnected from the fluidic channels. A closed system was thus formed, and the droplets were encapsulated within the wells. In this phase, self-diluting occurred: the lines of wells with decreasing volumes (Fig. 2d) formed droplets with decreasing concentrations, thus diluting the antibiotic. During the mixing phase (Fig. 3aiii and Movie 2), the top chip was further pushed to overlap the droplets of two types of solutions in the corresponding wells. The droplets were then mixed and chemical reactions took place, where the change in color intensity could be observed after completion of reactions. The overlapped droplets with constant and varied volumes (green droplets on top and red at the bottom) represented the AST line (indicated by orange arrows). This change in color intensity between wells with different concentrations of antibiotics could be further measured, such as that in WST-8 colorimetric assay (Fig. 3b, c).
SDFAST chips working principle. a A schematic diagram demonstrating the working principle of the device. The red color represents bacteria, and the green color represents antibiotics. The parts in the purple frame are enlarged to show the details of each step, and photos of the color dye patterns in each step are shown. The 3D models were built using Blender 4.1. b An example of SDFAST results from mixing Ciprofloxacin (CIP) with A. baumannii, using WST-8 assay. An abrupt change in color intensity (from colorless to orange) was observed at the 5th nanowell, indicating the MIC. c Photo of the color pattern of the WST-8 assay
Experimental protocol
On-chip AST procedure
The chips were first rinsed with deionized water and dried. Then, a thin layer of water repellent was applied on the contacting surfaces of the two plates. The repellent consists of fluoroalkylsilanes, which create a chemical bond with glass surfaces, causing water to bead up and roll off and the chip surface to be hydrophobic. The chips were then placed into an oven for 15 min at 60 °C for the repellent to bond to the surface. 1% surfactant in FC-40 (v/v) was prepared and added to the contacting surfaces, and the whole surface had to be covered by the mixture. The FC-40 facilitated sealing and had a high boiling point of 158–173 °C, which prevented the issue of evaporation18. This ensured the controlled volume of sample and reactants to generate more accurate and reproducible experimental results. 1% surfactant was added to the FC-40, as it was found to be the optimal concentration to prevent leakage (Fig. S1). It increased the surface tension of FC-40 such that the droplets were kept intact and would not adhere to the chip surface during the slipping process. After the pretreatment, the plates were clipped together by clips and ready for use.
The injection was divided into two sets, the former being the control lines and the latter being the testing lines: the former positive control lines filled with bacterial solution, and the latter testing lines consisted of one line with constant volume in each well, filled with bacterial solution, and adjacent line with varied volumes, filled with antibiotic solution. The solutions were injected using a micropipette with 0.1–20 μL tips. For lines with constant volume, 20 μL of solution was required to fill up one entire line, while for lines with varied volumes, 10 μL of solution was required. The excess solution was expelled from the hole adjacent to the end side of each line and could be removed carefully with KimWipes. After filling the wells, the chips were slipped such that the lower line aligned and overlapped with the upper line, and the solutions were mixed. The chips were then placed inside a Petri dish with an FC-40 bath, and the dish was sealed with parafilm. The chips were incubated at 37 °C for 6 h and taken out for analysis. To determine on-chip MIC, the well-representing MIC was first identified. It was the last well from left to right in the nanowell sequence that showed no abrupt color change.
MIC calculation
After identification of the well representing MIC, the MIC value was calculated by dividing the concentration of antibiotics before injection by dilution factors (Table S1). Each dilution factor was calculated by the dilution formulae:
where C0 is the concentration of the drug before injection, and Vn is the volume of the nth nanowell in the top chip (from left to right) (Fig. 2d, f); Cn is the concentration of the drug in the nth well and Vs is the volume of droplet after slipping, i.e., the droplets from the top and bottom chips are merged; Dn is the dilution factor in the nth well. For example, when the concentration of the drug before injection is 10 µg/mL, C0 = 10 µg/mL; V1 = 840 nL; Vs = 840 nL (top chip) + 840 nL (bottom chip) = 1680 nL. Therefore, C1 = 5 µg/mL and D1 = 10 µg/mL/5 µg/mL = 2. By repeating the calculation, D1 to D8 are calculated (Table S1).
To calculate the MIC value, the following formula was applied:
where n is the nth well that represents the MIC. Using the same example, if the 1st well is identified to represent the MIC, then MIC = 10 µg/mL/2 = 5 µg/mL; if the 3rd well is identified, MIC = 10 µg/mL/(2 × 1.5 × 1.665) = 2.00 µg/mL.
Data quantification
The colorimetric results generated from on-chip AST were further quantified. Photographs of the colorimetric results were taken with a single-lens reflex camera and analyzed using the “Measure” function in ImageJ. This function measured the red, green, and blue (RGB) values of each pixel in a selected area, and the average of the RGB values represented the brightness value of each pixel. The brightness values were added up and were divided by the number of pixels in the selected area, resulting in a “Mean” value28. Since the RGB values of the color white were the highest (R255, G255, B255), while those of black color were the lowest (R0, G0, B0), brightness was inversely proportional to the color intensity. This implied that the wells with pale color (negative control or no WST-8 color change) had higher “Mean” values than those with orange color (positive control or have WST-8 color change)29,30.
To analyze the color intensities of wells, three values, namely background, positive control and sample, were obtained. The background value was obtained by averaging the “Mean” values by measuring the brightness of each well. This value had to be calculated, as images could be taken under light of different brightness, and a comparison of results between two experimental setups (two sets of microchips) could be interfered with by it. Canceling the background value ensured that the color intensity in positive control and sample lines was only affected by color change in WST-8. The values after canceling the background value were said to be “corrected”. The positive control value served as a reference compared to values from the sample line. To calculate this value, the “Mean” value of each well in the positive line was first measured, and the raw positive control value was calculated by averaging all the “Mean” values. Then, the corrected positive control value was obtained by deducting the raw by negative control. To analyze the sample line, the “Mean” value of each well was measured. The negative control was deducted by each “Mean” value to yield a series of corrected color intensity (y-axis values). At last, a graph of corrected color intensity against the nanowell sequence (x-axis values; from the 1st to the 8th well) was plotted using GraphPad Prism 8. The error was represented by the standard deviation (SD) from averaging the color intensities from three trials. Furthermore, a comparison between the color intensity of wells in one sample line was visualized by a heatmap, which simulated the color pattern observed on-chip.
Examination of on-chip AST
Preparation of antibiotics and bacterial samples
Three parts of experiments were conducted to examine the capability of on-chip AST: (1) bacterial model testing with three common species of bacteria, which aimed at proving the accuracy of SDFAST initially; (2) testing with 16 bacterial samples in same genus with known MICs, which aimed at further demonstrating the device’s performance with different species in same genus; (3) testing with 51 bacterial isolates in varied genera with unknown MICs, which aimed at stimulating the device’s role as POC device in clinical scenario.
In Part (1), three species of bacteria, namely Escherichia coli (E. coli), Acinetobacter baumannii (A. baumannii), and Klebsiella pneumoniae (K. pneumonia), were selected for the experiment. For the antibiotics, ceftazidime (CTZ), ciprofloxacin (CIP), and levofloxacin (LVX) were selected. The combinations of these bacteria and antibiotics were studied, as the three antibiotics have been considered more resistant within their respective drug groups, namely cephalosporin and quinolone. Statistics also showed some of the strongest correlations between these combinations and resistance, with the combinations of the above bacteria with quinolones accounting for the top 5 among 72 studied combinations and A. baumannii—cephalosporin and E. coli—cephalosporin for the top 1531. The bacteria were cultured on Mueller–Hinton (MH) agar plates. A single colony was picked from the culture plate and was inoculated in MH Broth (Sigma-Aldrich) at 37 °C overnight. The inoculum (O.D. at 600 nm = 0.5) was then diluted 1000 times with MH Broth and mixed with WST-8 indicator (Beyotime). The volume ratio of diluted inoculum: WST-8: MH Broth is 1:20:179. The antibiotic solutions were prepared by dissolving the desired amount of antibiotics (solid or liquid) into deionized (DI) water, and the solutions were diluted by DI water according to the desired concentrations to be tested. CIP, which was only slightly soluble in water, was dissolved by adding a few drops of 37% hydrochloric acid (Sigma-Aldrich) beforehand.
In Part (2), 16 strains of Staphylococci species (aureus, capitis, caprae, and haemolyticus) (samples with known MICs) were obtained from the Department of Microbiology, Queen Mary Hospital, Hong Kong. The bacterial samples were prepared as Part (1) described. Vancomycin hydrochloride solution (100 mg/mL in DMSO) was diluted with DI water to the desired concentrations for each strain.
In Part (3), 51 clinical isolates were obtained from the Department of Microbiology. They were prepared in 0.5 McFarland standard in saline solution (mixing 0.05 mL of 1.175% barium chloride dihydrate with 9.95 mL of 1% sulfuric acid) and were provided by the Department of Microbiology. The volume ratio of the sample in saline: WST-8: MH Broth is 9:2:9.
Comparative study
The MIC values from SDFAST were compared to those from conventional methods, which were broth microdilution and E-test in our study. In Part (1), SDFAST was compared with broth microdilution. Referring to the guidelines of Clinical & Laboratory Standards Institute (CLSI)32, the methodology of broth microdilution is as follows: in a horizontal line of 96-well plates, 100 µL of antibiotic was added to the first well, and 50 µL of MHB was added to the rest of the wells. 50 µL of antibiotic was transferred from the first well to the second well and was mixed well with MHB, such that the antibiotic was diluted 2-fold. Then, 50 µL of diluted antibiotic was transferred from the second well to the third well, and the dilution continued. When the last well was reached, 50 µL of solution was removed from it. 50 µL of bacterial solution (diluted 1000 times) was added to each well with diluted antibiotic. The 96-well plate was incubated at 37 °C overnight, and the absorbance was analyzed by a plate reader at 600 nm. An abrupt rise in absorbance indicated the MIC and the MIC was calculated. The MIC values obtained were compared to those from SDFAST.
The SDFAST results from both Parts (2) and (3) were compared to those obtained by E-test (bioMérieux) from the Department of Microbiology. The testing was performed according to the guidance of the company: 16 strains of Staphylococci species in Part (2) and 51 clinical isolates were first prepared in 0.5 McFarland standard in saline solution respectively. The solution was then spread onto MH agar plates evenly and was let dry and absorbed by the agar plates. An E-test strip with Vancomycin was placed onto each agar plate using a pair of forceps. The plates were incubated at 37 °C overnight and then taken out for MIC determination. The ellipse of inhibition of bacteria was observed, and the MIC value was determined by reading the scale on the strip. The MIC values obtained were compared to those from SDFAST.
For testing clinical isolates, we followed the instructions of CLSI on evaluating a commercial AST in comparison to a standard one. The accuracy of the on-chip AST was determined by essential agreement (EA)33, which was calculated by the following formula:
in which the NEA is the number of tested samples with the same MIC, or that within 2-fold dilution as the reference method, and NT is the number of tested samples. The SDFAST AST was considered to be accurate if EA ≥ 90%.
Results and discussion
Self-diluting property of the SDFAST device
Preliminary tests were carried out to confirm if our device could perform serial dilution in the system in seconds. This characteristic was proved by the results of both preliminary tests (Fig. S3a, b) and on-chip AST (Figs. 3b, S2a, b). In preliminary tests, as the volume of wells in the top plate became smaller, the blue food dye became more diluted, resulting in reduced color intensity. This applied as well to bacterial samples, in which fewer colonies were found from wells with smaller volumes. In the results of on-chip AST, only the wells on the right side showed color change, indicating that the antibiotic had been diluted sufficiently in those wells. This resulted in most bacteria surviving and changing the assay color.
Testing with three species of bacteria
In Part (1), we performed AST on a total of 9 bacteria-antibiotic combinations. The experiment aimed at testing whether our device can perform AST initially, as well as its accuracy compared to the reference broth microdilution method. Quantification of WST-8 results on A. baumannii, E. coli, and K. pneumoniae (Fig. 4) showed that the color intensity increased quickly as the antibiotic concentration reached below the corresponding MIC. All the bacteria-antibiotic combinations showed a general trend, in which the color intensity was low for the first few wells, but rose abruptly at a particular well and then remained higher than the first few wells as the sequence shifted to the right. The colorless or very pale yellow well before the abrupt change in each line, which corresponds to the lowest concentration that could inhibit bacterial growth, represented the corresponding MIC, which could be easily identified by the naked eye. After the identification, the MIC value was calculated based on dilution rates. The comparison between the values from SDFAST and those from broth microdilution showed that their MICs were similar or only 2-fold apart from each other, which indicated the accuracy of our device and that it could be an alternative to the conventional method, regardless of the different genera of bacteria as well as types of antibiotics (Table 1). Moreover, SDFAST generally gave a smaller value than broth microdilution. The above results prove that the SDFAST is an effective method that yields obvious results for users who have scarce knowledge in microbiology and analytical chemistry, as they could identify the well-representing MIC immediately by noticing the abrupt color change in the testing line and thus calculating out the MIC by dilution rate.
Changes in color intensities in nanowell sequence from wells on left to right in a A. baumannii, b E. coli, and c K. pneumoniae, demonstrated by line graphs and heatmaps. The wells before the abrupt changes, indicated by the blue frames in heatmaps, represented the corresponding MICs. Each bacteria–antibiotic combination was tested in triplicate
Testing with Staphylococci Species
In Part (2), apart from the most investigated and clinically significant coagulase-positive S. aureus, we have also tested several coagulase‑negative Staphylococci (CoNS). These species could be collectively as prevalent as S.aureus, as found in clinical34,35,36 and non-clinical settings37. Despite being regarded as milder pathogens in causing diseases, they can contribute to AMR significantly, as CoNS themselves have developed multidrug resistance over time. For instance, a study on the MIC changes of S. epidermidis between 1999 and 2012 in the US summarized that the species had developed higher resistance to selected fluoroquinolones over 13 years38. Another study showed that around 94% of the CoNS samples were resistant toward at least one of the 11 selected antibiotics37. Furthermore, CoNS has been suggested as a reservoir for resistance genes39, and their interactions with S. aureus could aggravate drug resistance of the later bacteria, which could be achieved by the transfer of resistance plasmids40,41. The evidence demonstrates the necessity to measure and monitor the resistance growth of CoNS.
Besides verifying the accuracy of SDFAST in monitoring Gram-positive bacteria, the MIC ranges of bacteria were also different from those in Part (1). Differentiating samples with small MIC differences is particularly significant when the cutoff values are small. Therefore, we aimed to confirm if our device was able to achieve this behavior by testing Staphylococci with a small MIC range of 0.19–1.5 µg/mL. The results were similar to the previous section, in which the same trend was observed in all samples: the color intensity remained low when the concentration of antibiotic was higher than MIC and increased abruptly after passing MIC (Fig. 5). The wells representing MICs could be identified easily, and the comparison also showcased the similarity in results between our device and the reference (Table 2). In our model study, the SDFAST could identify the MICs with high accuracy (EA = 100%) as well as in a short period of time. Compared to broth microdilution and E-test, which require overnight incubation, our device could pinpoint the MICs within 6 h of incubation. In some cases, this duration could even be shortened to 4 h. It also could differentiate between samples with similar MICs, with 80% of the samples having identical or very close MICs to the E-test.
Testing on clinical isolates
In Part (3), 51 clinical isolates were tested, in which the wide variety of MIC ranges and species simulated the application of our device on POCT. This aimed at comparing the accuracy of our method with E-test, a commercial method applied in microbiology laboratories. The results showed a high EA among clinical isolates with a range of common bacteria species (Tables 3 and S2). As EA > 90%, our method was considered to be accurate. The variety of bacteria tested was larger than that of previous studies. In previous SlipChip AST studies, only few of the most prominent bacterial species, such as E. coli and S. aureus, were tested. Our paper provided a more comprehensive study in various species and proved the high utility of our WST-8-incorporated device.
Moreover, we observed that SDFAST tended to give lower MIC than standard E-test. 62.7% (32 samples) of the samples were found to have a lower value. This could be explained by looking into both methods. In E-test, although it was suggested by the manufacturer that the reading should be made at where the lower part of the ellipse intersects the strip42, reading was made slightly above the end of the ellipse in clinical practice to ensure majority of bacteria have been killed at a higher concentration of antibiotic. Therefore, the resultant MIC was higher. In SDFAST, the choice of initial concentration of antibiotic before injection could affect the reading. For instance, in our tests, 256 and 4 µg/mL of VAN was used to cover bacteria with higher and lower range of MIC respectively. Meanwhile, some isolates like those of E. faecium and Nostoc sp. were with MICs larger than 256 µg/mL. Since the maximal concentration of antibiotic in droplet was 128 µg/mL, these bacteria were shown to have MICs of 128 µg/mL, which was smaller than the reading by E-test. Therefore, it was suggested that the initial concentration of antibiotics had to be decided carefully based on the known ranges of MICs of bacteria by calculating the consecutive concentrations in one testing line.
Interpretation of the overall results
In Figs. 4 and 5, after 3 repeated trials, the SD values were small in the MIC-indicating and susceptibility-indicating wells. This indicated that color intensities at these wells were stable over multiple times of testing. In resistant-indicating wells, the fluctuation was larger, but still acceptable, as the color intensities of most first resistant-indicating wells still exceeded those of MIC-indicating ones. Therefore, the device could generate repeatable MIC values.
For the sensitivity, most results from our method and reference were reported as values instead of ranges. These values have often been reported as ranges in previous studies, which made it difficult to determine the sensitivity. For example, the results of E. Coli-LEV combination from a microchip AST and reference were 1–10 µg/mL and >8 µg/mL respectively20. Even if some of our results were reported as ranges, such as those in Nostoc sp.—VAN combination (Table S2), the MIC values were high that they would always be determined as “resistant” in practice, having less impact on AMR categorization.
Table S3 illustrates a comparison between our method and other 10 methods (commercial and/or microfluidic) with known EAs. It shows that both the accuracy and time for incubation of our method are comparable to both commercial and previous microfluidic methods. It is noticeable that microfluidic methods featuring a shorter incubation time do not guarantee a high enough accuracy (EA ≥ 90%), and some commercial methods have a wide variation in incubation time. For example, the time required by VITEK 2 can vary much according to bacterial species. Furthermore, the comparison has shown the advantages of SDFAST self-diluting feature: QMAC-dRAST has a selection of certain antibiotics with fixed concentration range, while SDFAST enables high versatility in antibiotic and concentration range selections. The flow rates have to be controlled carefully in ladder-shaped system to achieve stable antibiotic dilution, and Handyfuge-AST has a small dilution range, while SDFAST can achieve regular dilution rate with larger dilution range. The device design is simpler than the other methods, while maintaining its accuracy and short reaction time.
Limitations and perspectives
Although our study has shown the capability of SDFAST, there were still some challenges and unresolved issues. Firstly, some results required further investigation. One of them was that the Enterococci isolates required a longer incubation period than others. The reason behind it was unknown, but it was hypothesized that the bacteria either grow more slowly than those in other families, or that they did not grow efficiently in aerobic condition while trapped in droplets. Secondly, although the incubation time had been greatly reduced compared to conventional methods, it was still lengthened due to miniaturization. To illustrate, in a study on WST-8, color changes were observed within 2–4 h in macroscopic setting43, while the time was lengthened to 4–6 h in microfluidic setting. This issue is common in microfluidic phenotypical AST relying on color changes, as microfluidic droplets contain less bacteria44. Further study should be conducted to resolve this problem.
Despite simple operation and the in-system dilution feature, our current device still requires users to manually perform some steps, such as drug injection and chip slipping. These steps could be automated, so that a large quantity of samples could be processed effortlessly, and the errors by manual operation can be minimized. Some possible modifications are suggested here: first, a pumpless pressure-driven method could be applied for automatic injection of bacterial and antibiotic solutions. Studies have demonstrated that solutions could be extracted from chambers and injected into microfluidic channels driven by siphon45,46,47. Since our system features multiplex testing of different bacteria-antibiotic combinations, we envisage that users can add bacteria and antibiotic solutions into reservoirs manually according to needs, and the injection can be carried out automatically by pressure difference. The system is portable, and the flow rate can be adjusted to realize injection of microliter of solutions (in our device, 10–20 µL per channel) in seconds48. Second, a pusher block can be introduced to push the upper chip upwards, generating and mixing droplets automatically. This is incorporated with a frame used for fixing the position of the clipped device, so that the chips are not misaligned during slipping. Third, commercial thermal control and sensing system can be implemented to replace the bulky incubator. Fourth, the colorimetric change can be recorded by a smartphone or low-cost camera. The analysis and calculation of color intensities and resultant MIC values can then be performed rapidly by a combination of image processing software, cloud drives and deep learning models49. With this modification, users can obtain MIC values quickly after inputting the images, without the need to calculate manually. Furthermore, this allows a large quantity of results from different bacteria-antibiotic combinations to be collected. The MIC values can therefore be updated timely for the reference of medical professionals.
Conclusion
The SDFAST device is an effective microfluidic gadget that could serve as a POC diagnostic tool. Consisting of two microchips, the device allows the injection of samples with bacteria and antibiotics by forming fluidic paths after connecting the chips. The solutions can be mixed by slipping one microchip against another in a single press of the microchip. In our study, the SDFAST was operated with WST-8 assay, in which prevalent bacteria, including A. baumannii, E. coli, K. pneumoniae, and Staphylococci, were tested under various antibiotics. The results proved the advantages of our device, not only that the MIC can be determined in a simple and quicker way by non-professionals without a spectrophotometer, but also that the device operates with much fewer medical resources compared to the conventional methods, such as broth microdilution and E-test. The experiments have demonstrated that SDFAST device facilitates the effective mixing of bacteria and antibiotics and gives readings that could be easily comprehended and analyzed, even by users with little knowledge of relevant subjects.
References
Naghavi, M. et al. Global burden of bacterial antimicrobial resistance 1990–2021: a systematic analysis with forecasts to 2050. Lancet 404, 1199–1226 (2024).
Langford, B. J. et al. Antibiotic prescribing in patients with COVID-19: rapid review and meta-analysis. Clin. Microbiol. Infect. 27, 520–531 (2021).
Andrews, J. M. Determination of minimum inhibitory concentrations. J. Antimicrob. Chemother. 48(Suppl. SA), 5–16 (2001).
Balouiri, M., Sadiki, M. & Ibnsouda, S. K. Methods for in vitro evaluating antimicrobial activity: a review. J. Pharm. Anal. 6, 71–79 (2016).
Humphries, R. M. et al. The continued value of disk diffusion for assessing antimicrobial susceptibility in clinical laboratories: report from the Clinical and Laboratory Standards Institute Methods Development and Standardization Working Group. J. Clin. Microbiol. 56, 8 (2018).
Benkova, M., Soukup, O. & Marek, J. Antimicrobial susceptibility testing: currently used methods and devices and the near future in clinical practice. J. Appl. Microbiol. 129, 806–822 (2020).
Kim, S. C., Cestellos-Blanco, S., Inoue, K. & Zare, R. N. Miniaturized antimicrobial susceptibility test by combining concentration gradient generation and rapid cell culturing. Antibiotics 4, 455–466 (2015).
Safavieh, M. et al. Rapid real-time antimicrobial susceptibility testing with electrical sensing on plastic microchips with printed electrodes. ACS Appl. Mater. Interfaces 9, 12832–12840 (2017).
Kaushik, A. M. et al. Accelerating bacterial growth detection and antimicrobial susceptibility assessment in integrated picoliter droplet platform. Biosens. Bioelectron. 97, 260–266 (2017).
Postek, W. & Garstecki, P. Droplet microfluidics for high-throughput analysis of antibiotic susceptibility in bacterial cells and populations. Acc. Chem. Res. 55, 605–615 (2022).
Ruszczak, A., Bartkova, S., Zapotoczna, M., Scheler, O. & Garstecki, P. Droplet-based methods for tackling antimicrobial resistance. Curr. Opin. Biotechnol. 76, 102755 (2022).
Matsumoto, Y. et al. A microfluidic channel method for rapid drug-susceptibility testing of Pseudomonas aeruginosa. PLoS ONE 11, 2 (2016).
Chen, C. H. et al. Antimicrobial susceptibility testing using high surface-to-volume ratio microchannels. Anal. Chem. 82, 1012–1019 (2010).
Reis, N. M., Pivetal, J., Loo-Zazueta, A. L., Barros, J. M. S. & Edwards, A. D. Lab on a stick: multi-analyte cellular assays in a microfluidic dipstick. Lab Chip 16, 2891–2899 (2016).
Li, S. et al. Handyfuge microfluidic for on-site antibiotic susceptibility testing. Anal. Chem. 95, 6145–6155 (2023).
Hassan, S. U. & Zhang, X. Microfluidics as an emerging platform for tackling antimicrobial resistance (AMR): a review. Curr. Anal. Chem. 16, 41–51 (2020).
Zhu, X., Chu, J. & Wang, Y. Advances in microfluidics applied to single cell operation. Biotechnol. J. 13, 2 (2018).
Du, W., Li, L., Nichols, K. P. & Ismagilov, R. F. SlipChip. Lab Chip 9, 2286–2292 (2009).
Liu, X. et al. Formation and parallel manipulation of gradient droplets on a self-partitioning SlipChip for phenotypic antimicrobial susceptibility testing. ACS Sens. 7, 1977-–11984 (2022).
Yi, Q. et al. Direct antimicrobial susceptibility testing of bloodstream infection on SlipChip. Biosens. Bioelectron. 135, 200–207 (2019).
Tsukatani, T. et al. Colorimetric microbial viability assay based on reduction of water-soluble tetrazolium salts for antimicrobial susceptibility testing and screening of antimicrobial substances. Anal. Biochem. 393, 117–125 (2009).
Zhao, R. et al. A rapid screening platform for antibiotic susceptibility testing based on a simple colorimetric method. Analyst 148, 4148–4155 (2023).
Lee, S. et al. Rapid deep learning-assisted predictive diagnostics for point-of-care testing. Nat. Commun. 15, 1695 (2024).
Woolf, M. S., Dignan, L. M., Scott, A. T. & Landers, J. P. Digital postprocessing and image segmentation for objective analysis of colorimetric reactions. Nat. Protoc. 16, 218–238 (2021).
Reszetnik, G. et al. Next-generation rapid phenotypic antimicrobial susceptibility testing. Nat. Commun. 15, 9719 (2024).
Hashim, A. & Abbas, B. Recent review on poly-methyl methacrylate (PMMA)—-polystyrene (PS) blend doped with nanoparticles for modern applications. Res. J. Agric. Biol. Sci. 14, 6–12 (2019).
Hassan, S. U., Morgan, H., Zhang, X. & Niu, X. Droplet interfaced parallel and quantitative microfluidic-based separations. Anal. Chem. 87, 3895–3901 (2015).
Ferreira, T. & Rasband, W. The ImageJ User Guide—Version 1.44, pp 130 http://imagej.nih.gov/ij/docs/user-guide.pdf (2011).
Nguyen, D. H., Zhou, T., Shu, J. & Mao, J. Quantifying chromogen intensity in immunohistochemistry via reciprocal intensity. Cancer InCytes 2, 1 (2013).
Vrekoussis, T. et al. Image analysis of breast cancer immunohistochemistry-stained sections using ImageJ: an RGB-based model. Anticancer Res. 29, 4995–4998 (2009).
Olesen, S. W. et al. The distribution of antibiotic use and its association with antibiotic resistance. eLife 7, e39435 (2018).
Clinical and Laboratory Standards Institute. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically, 10th Edition. 27-29 (CLSI, 2015).
Humphries, R. M. et al. CLSI methods development and standardization working group best practices for evaluation of antimicrobial susceptibility tests. J. Clin. Microbiol. 56, 4 (2018).
Serra, N. et al. Staphylococcus aureus and coagulase-negative staphylococci from bloodstream infections: frequency of occurrence and antimicrobial resistance, 2018–2021. Life 13, 1356 (2023).
Chong, J., Caya, C., Lévesque, S. & Quach, C. Heteroresistant vancomycin intermediate coagulase negative Staphylococcusin the NICU: a systematic review. PLOS ONE 11, e0164136 (2016).
Tornero, E. et al. Prosthetic Joint Infections due to Staphylococcus aureus and coagulase-negative staphylococci. Int. J. Artif. Organs 35, 884–892 (2012).
Xu, Z. et al. The prevalence, antibiotic resistance and mecA characterization of coagulase negative staphylococci recovered from non-healthcare settings in London, UK. Antimicrob. Resist. Infect. Control 7, 73 (2018).
May, L., Klein, E. Y., Rothman, R. E. & Laxminarayan, R. Trends in antibiotic resistance in coagulase-negative staphylococci in the United States, 1999 to 2012. Antimicrob. Agents Chemother. 58, 1404–1409 (2014).
Ikhimiukor, O. O. et al. Leaky barriers to gene sharing between locally co-existing coagulase-negative Staphylococcus species. Commun. Biol. 6, 482 (2023).
Becker, K., Heilmann, C. & Peters, G. Coagulase-negative staphylococci. Clin. Microbiol. Rev. 27, 4 (2014).
Fišarová, L., Pantůček, R., Botka, T. & Doškař, J. Variability of resistance plasmids in coagulase-negative staphylococci and their importance as a reservoir of antimicrobial resistance. Res. Microbiol. 170, 105–111 (2019).
Reller, L. B., Weinstein, M., Jorgensen, J. H. & Ferraro, M. J. Antimicrobial susceptibility testing: a review of general principles and contemporary practices. Clin. Infect. Dis. 49, 1749–1755 (2009).
Yang, X., Zhong, Y., Wang, D. & Lu, Z. A simple colorimetric method for viable bacteria detection based on cell counting Kit-8. Anal. Methods 13, 5211–5215 (2021).
Needs, S. H. et al. Challenges in microfluidic and point-of-care phenotypic antimicrobial resistance tests. Front. Mech. Eng. 6, 73 (2020).
Marimuthu, M. & Kim, S. Pumpless steady-flow microfluidic chip for cell culture. Anal. Biochem. 437, 161–163 (2013).
Reis, N. M. et al. Gravity-driven microfluidic siphons: fluidic characterization and application to quantitative immunoassays. ACS Sens. 6, 12 (2021).
Jeong, G. S. et al. Siphon-driven microfluidic passive pump with a yarn flow resistance controller. Lab Chip 14, 4213–4219 (2014).
Wang, X. et al. A hydrostatic pressure-driven passive micropump enhanced with siphon-based autofill function. Lab Chip 18, 2167–2177 (2018).
Duan, S. et al. Deep learning-assisted ultra-accurate smartphone testing of paper-based colorimetric ELISA assays. Anal. Chim. Acta 1248, 340868 (2023).
Acknowledgements
We would like to thank Department of Microbiology, Queen Mary Hospital, Hong Kong for preparing clinical isolates and performing comparative testing. We would also like to acknowledge Dr. Sihan Liu for the preparation of the schematic diagram. This work was supported by the Health@InnoHK program of the Innovation and Technology Commission of the Hong Kong SAR Government. The work was also supported by The University of Hong Kong (202009185087), Collaborative Research Fund (C7165-20GF) and General Research Fund (17307919 and 17303123) of the Research Grants Council of Hong Kong, Hong Kong.
Author information
Authors and Affiliations
Contributions
J.K.W., M.X., K.K.T., and S.U.H. planned the research; M.X. and S.U.H. designed and fabricated the device; J.K.W. and M.X. performed the antimicrobial testing; J.K.W., M.X., and S.U.H. analyzed the data; J.K.W., L.N., H.L., K.K.T., H.C.S., and S.U.H. wrote and refined the paper.
Corresponding authors
Ethics declarations
Conflict of interest
H.C. Shum is a scientific advisor of EN Technology Limited, MicroDiagnostics Limited, Upgrade Biopolymers Limited, and PharmaEase Tech Limited in which he owns some equity; he is also a director of the research center, Advanced Biomedical Instrumentation Center Limited. The works in the paper are however not directly related to the works of these three entities, as far as we know.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wat, J.KH., Xu, M., Nan, L. et al. Rapid antimicrobial susceptibility tests performed by self-diluting microfluidic chips for drug resistance studies and point-of-care diagnostics. Microsyst Nanoeng 11, 110 (2025). https://doi.org/10.1038/s41378-025-00938-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41378-025-00938-y