Abstract
In recent years, the incidence of acute respiratory distress syndrome (ARDS) has been gradually increasing. Despite advances in supportive care, ARDS remains a significant cause of morbidity and mortality in critically ill patients. ARDS is characterized by acute hypoxaemic respiratory failure with diffuse pulmonary inflammation and bilateral edema due to excessive alveolocapillary permeability in patients with non-cardiogenic pulmonary diseases. Over the past seven decades, our understanding of the pathology and clinical characteristics of ARDS has evolved significantly, yet it remains an area of active research and discovery. ARDS is highly heterogeneous, including diverse pathological causes, clinical presentations, and treatment responses, presenting a significant challenge for clinicians and researchers. In this review, we comprehensively discuss the latest advancements in ARDS research, focusing on its heterogeneity, pathophysiological mechanisms, and emerging therapeutic approaches, such as cellular therapy, immunotherapy, and targeted therapy. Moreover, we also examine the pathological characteristics of COVID-19-related ARDS and discuss the corresponding therapeutic approaches. In the face of challenges posed by ARDS heterogeneity, recent advancements offer hope for improved patient outcomes. Further research is essential to translate these findings into effective clinical interventions and personalized treatment approaches for ARDS, ultimately leading to better outcomes for patients suffering from ARDS.
Similar content being viewed by others
Introduction
Acute respiratory distress syndrome (ARDS) has emerged as a critical and complex medical issue in recent years. It is characterized by acute hypoxaemic respiratory failure, accompanied by diffuse pulmonary inflammation and bilateral edema, which stem from excessive alveolocapillary permeability in patients suffering from non-cardiogenic pulmonary diseases. The Berlin definition, currently regarded as the gold standard, dominates the diagnostic landscape for ARDS. However, no foolproof method can definitively confirm or rule out this diagnosis. Compounding this diagnostic conundrum is the remarkable heterogeneity that characterizes ARDS. The underlying pathological causes, the way they present clinically, and how patients respond to treatment can vary dramatically from one individual to another. This variability presents a significant challenge to both clinicians working on the front lines and researchers dedicated to finding solutions.
Recent advances in research have yielded significant progress, particularly in the area of cell therapy. Mesenchymal stromal cells (MSCs), for example, have emerged as a promising therapeutic option due to their unique immunomodulatory and regenerative properties. These cells have shown potential in modulating the immune response and hastening tissue repair in the lungs. However, several challenges remain plentiful. One of the key obstacles is selecting the most suitable cell source. Options such as bone marrow-derived, adipose-derived, or umbilical cord-derived MSCs each have their pros and cons. Deciding on the optimal delivery method, whether it be intravenous injection for systemic effect, inhalation to target the lungs directly, or direct injection into the lung tissue for more precise targeting, is a topic of intense debate. Moreover, pinpointing the exact timing of intervention to achieve maximum therapeutic benefit is equally contentious. In the realm of targeted therapy, scientists have been painstakingly investigating specific molecular pathways implicated in ARDS pathogenesis. However, issues like off-target effects that could lead to unwanted side effects in other organs, potential drug resistance over time, and the need for comprehensive long-term safety evaluations have come to the fore. Personalized therapy is gaining momentum, intending to tailor treatment strategies based on individual patient profiles. However, the task of collecting and analyzing vast amounts of patient data to create an accurate and comprehensive profile, while integrating numerous factors into an effective treatment plan, remains a monumental challenge.
This review is wholeheartedly committed to bridging the knowledge gaps by conducting an exhaustive exploration of the current state of the art. Its primary objective is to succinctly analyze the heterogeneity, and pathophysiology of ARDS, with a particular focus on cell therapy, targeted therapy, and personalized therapy. By doing so, we aim to provide valuable insights and ultimately lead to improved patient outcomes.
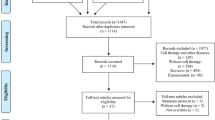
Historical perspective on the definition of ARDS
Before the 1960s, fluid overload was deemed the sole causative agent of congestive atelectasis according to clinical inspections and microscopic and macroscopic postmortem findings.1 Ashbaugh and colleagues initially described acute respiratory distress in adults with pathologic examination results, including loss of lung compliance, atelectasis, vascular congestion and hemorrhage, severe pulmonary edema, and hyaline membranes.2 Moreover, treatment with positive end-expiratory pressure (PEEP) and corticosteroids was found to be helpful. In 1971, “adult” respiratory distress syndrome was first reported as the abbreviation of the principles of management, including adequate support for oxygen transport, ventilation, and circulation using volume respirators with PEEP.3 Murry and coworkers proposed an expanded three-part definition of ARDS accompanied by a “lung injury score” that detailed the disease state, severity, and underlying cause or associated condition.4 Additional evidence later revealed that ARDS is not limited to adults but also occurs in pediatric patients.5,6 Therefore, the term “adult” was no longer appropriate as part of the definition of ARDS. In 1994, the first American-European Consensus Conference (AECC) issued criteria for acute lung injury (ALI) and ARDS, which included timing (acute onset), oxygenation, chest radiography, and elevated pulmonary capillary pressure, with “acute” used as part of the new definition of ARDS.7 However, the lack of standard criteria for diagnosing acute onset, the sensitivity of the oxygenation index to different ventilation settings, the reliability of chest radiography criteria, and the difficulty of distinguishing hydrostatic edema made it difficult for physicians to diagnose ARDS. After the publication of the clinical and physiological characteristics of ARDS patients in large study cohorts in 2012, the Berlin definition was proposed and stated that “ARDS is a type of acute diffuse, inflammatory lung injury, leading to increased pulmonary vascular permeability, increased lung weight, and loss of aerated lung tissue.” The Berlin definition provides more precise criteria for diagnosing ARDS, including timing, radiographic evidence, edema origin, and severity based on the oxygenation index and PEEP levels.8 The accurate and evidenced-based Berlin definition achieved a better ability to predict mortality.8 In 2015, the Kigali modification, which proposed a SpO2/FIO2 ratio ≤ 315 irrespective of PEEP as an alternative criterion, provided insights for diagnosing ARDS in resource-constrained regions where mechanical ventilators, arterial blood analysis, and chest radiography are unavailable.9 After over 70 years of struggling to treat ARDS, supportive care remains the main treatment approach, and few drugs have been proven effective for all patients.10,11 The etiology, physiology and microbiology of ARDS are highly heterogeneous,10 so personalized medicine approaches for patients with different phenotypes might be a goal of future treatment. The important stages in the evolution of ARDS definitions are shown in Fig. 1.
However, as our understanding of ARDS deepens, we should also be aware of some limitations in the definition of ARDS. The SpO2/FiO2 ratio has been clinically validated for diagnosing and stratifying ARDS patients, but it may be less accurate in poor perfusion states, above 97% oxygen saturation, and in patients with darker skin pigmentation.12 Bilateral opacities on chest X-rays were part of the Berlin Definition for ARDS, but they lack interobserver reliability. The radiographic diagnostic accuracy and agreement among raters were poor with the Berlin definition.13 The “Radiographic Assessment of Lung Edema” (RALE) score was introduced to assess the extent and density of alveolar opacities on chest X-rays in ARDS patients, showing preferable diagnostic accuracy.14 Encouragingly, recent research indicated that an AI-based model utilizing chest X-rays and incorporating specific LUS criteria15,16 could enhance the specificity and sensitivity of ARDS definitions.17
Epidemiology
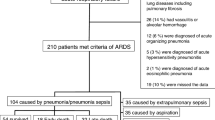
In recent years, the incidence of ARDS has shown a gradual upward trend,18,19,20 which is related to the introduction of the Berlin definition and an improved ability to identify ARDS patients.21 The incidence of ARDS is age dependent, increasing from 16/100,000 person-years for individuals 15–19 years of age to 306/100,000 person-years for individuals 75–84 years of age.18 In addition, the incidence of ARDS is also gender dependent, and men (62%) are more likely to develop ARDS than women (38%).22 The incidence of ARDS among ICU patients was investigated in a large-scale study; 10% of ICU patients met the criteria for ARDS, and a quarter of all critically ill patients who required mechanical ventilation developed ARDS.23 Despite advances in supportive care, ARDS remains a significant cause of morbidity and mortality in critically ill patients, with high mortality rates of 35% (for mild cases), 40% (for moderate cases), and 45% (for severe cases).8,23,24,25 However, there is no significant difference in overall hospital mortality between men (40.2%) and women (40.2%), although women have been reported to have higher mortality in patients with severe ARDS.22 In China, comprehensive studies of the prevalence, mortality, and risk factors of ALI/ARDS are lacking. However, a few regional studies have suggested that the epidemiology of ARDS in China is similar to that in Europe and the United States. Of 1814 patients in 20 ICUs in 9 provinces in China, 147 (8.1%) ICU patients met the criteria for ARDS, with an in-hospital mortality rate of 34.0%.26 However, in another multicentre prospective longitudinal study, the incidence of ARDS was low; of 18,793 ICU patients, only 3.6% met the criteria outlined in the Berlin definition of ARDS, with an in-hospital mortality rate of 244 (46.3%).27 Moreover, the epidemiology of COVID-19-related ARDS (CARDS) in China has varied among different cohort studies. According to several small sample studies, the probability that a COVID-19 patient will suffer from ARDS is 40–65%, with a mortality rate ranging from 50–75%.28,29 However, a large study including 1875 COVID-19 patients suggested that 19.3% of COVID-19 patients will develop CARDS, which is similar to other reported data.30 The reason for this difference may be related to the sample size or the inclusion and exclusion criteria.
Pneumonia is the most common cause of ARDS, followed by extrapulmonary sepsis, aspiration, and trauma.18,23,31 Notably, some viruses that cause pneumonia are more likely to cause ARDS, including SARS-CoV (2003), H1N1 influenza (2009), MERS-CoV (2012), and most notably SARS-CoV-2 (2019), which led to the COVID-19 pandemic. Of those hospitalized for COVID-19, 15–30% typically develop CARDS.32,33 Substantial evidence has shown that smoking cigarettes34,35 and chronic consumption of large amounts of alcohol36 increase the risk of developing ARDS. Additionally, blood product transfusion37 and e-cigarette or vaping product use-associated lung injury (EVALI) were identified as risk factors for ARDS in several trials.38,39,40 Notably, long-term exposure to air pollutants, especially ozone, has also been reported to be a potential modifiable environmental risk factor for ARDS.41,42
Pathogenesis of ARDS
The pathophysiology of ARDS is complex, and the mechanism includes the activation and dysregulation of multiple overlapping and interacting pathways associated with injury, inflammation, and coagulation, both in the lungs and systemically; this process involves a variety of cells.43 The pathological changes that occur in ARDS include alveolar epithelial injury, pulmonary endothelial injury, pulmonary macrophage injury, and pulmonary fibroblast injury, which are all observed in animal models of ALI/ARDS. Oxidative stress, inflammation, apoptosis, and barrier breakdown are observed in alveolar epithelial cells and pulmonary endothelial cells in mice with ALI,44,45,46,47 with increased levels of alveolar injury markers and endothelial injury markers.48,49 We provide a detailed summary of the pathological changes and potential mechanisms of ARDS below, shown in Fig. 2.
The pathological changes in ARDS. Acute respiratory distress syndrome affects not only pulmonary tissue but also extra-pulmonary tissues. Systemic pathological changes, such as immunoinflammation and immunothrombosis, occur throughout the body, and various cells are involved in these pathological changes including macrophage, monocyte, dendritic cell, neutrophil, eosinophil, T cell and endothelial cell. These changes are believed to contribute to cellular abnormalities within the pulmonary tissue, ultimately leading to damage to the alveolar-capillary barrier in ARDS. A variety of pulmonary pathological changes have been observed in the damaged lung tissue, including endothelial barrier dysfunction, the presence of cell-free hemoglobin, reduced resolution of pulmonary edema, cell death, cellular senescence, and cellular dysfunction. *M1: Proinflammatory phenotype of macrophages; NET: neutrophil extracellular trap; CFH: cell-free hemoglobin; AFC: alveolar fluid clearance
Systemic pathological changes and underlying mechanisms
ARDS is a syndrome that can impact pulmonary tissue as well as extrapulmonary tissues. Several systemic pathological changes, such as immune dysfunction, inflammatory responses, and abnormal coagulation, have been reported to occur during ARDS. Herein, we focus on the interactions between immune dysfunction and inflammation and the interactions between coagulation disorders and inflammation in the context of lung thrombosis, which are classified as immunoinflammation and immunothrombosis, respectively.
Immunoinflammation
Immunoinflammation, the initial immunological response that leads to inflammation and initiates a vicious cycle of immune responses and inflammation,50,51 is closely associated with the molecular pathogenesis of ARDS. In ARDS caused by infection, immune responses, including innate and adaptive immune responses, are first activated by pathogens. However, in noninfective ARDS, alveolar epithelial cell injury, pulmonary endothelial activation, and alveolar macrophage responses can recruit neutrophils and natural killer (NK) cells as well as monocytes, such as macrophages and dendritic cells, from the circulation, thus initiating the immune response during ARDS.52,53 An active immune response ultimately leads to immune disorders in ARDS patients, further promoting the inflammatory response through similar effector cells in both immune and inflammatory aetiologies. The activation of the adaptive immune system in ARDS involves T lymphocytes, B lymphocytes, antigen-presenting cells (APCs), and several influential factors, such as complement. We have summarized the cells and molecules involved in the above information in Table 1.54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69
Several key signaling pathways are involved in immunoinflammation during ARDS, including macrophages and endothelial cells. IL33-STAT3-MMP2/9 is reported to play an important role in macrophage polarization from anti-inflammatory phenotype (M2) to proinflammatory phenotype (M1), thus inducing lipopolysaccharide (LPS)-induced ALI and pulmonary inflammation.70 Macrophage polarization further leads to endothelial injury. Extracellular nicotinamide phosphoribosyltransferase (eNAMPT) from endothelial cells is responsible for endothelial inflammation and the subsequent disruption in the endothelial barrier, which depends on the TLR4 inflammatory pathway.71 Both macrophage and endothelial changes contribute to immunoinflammation in ARDS.
Immunothrombosis
Immunothrombosis, the interaction between the coagulation system and the innate immune system after infection, is an emerging pathogenic mechanism in ARDS, especially in CARDS. Neutrophils, macrophages, and other effectors are involved in the innate immune response, and platelets are the primary cells involved in immunothrombosis and complement signaling.72 The complement system participates in the immunothrombosis process in CARDS. Complement activation has been reported to be associated with enhanced thrombotic activity, and blockade of C5aR1 can alleviate platelet-mediated thrombogenicity in a neutrophil extracellular trap (NET)-dependent manner in ARDS.73 Increased NET formation is associated with microthrombus and platelet accumulation in the pulmonary circulation, indicating that NETs promote immunothrombosis in ARDS.72,74 Additionally, endothelial activation plays a pivotal role in immunothrombosis and aberrant coagulation since elevated levels of endothelium-derived glycoproteins have been detected in ARDS patients with blood type A and are associated with an increased risk of disseminated intravascular coagulation.75,76
There are also several key signaling pathways involved in the immunothrombosis during ARDS, especially in neutrophils. Formation of NETs is essential in immunothrombosis, and it relies on the CLEC5A-TLR2 activation in CARDS as extremely low level of NETs is detected in neutrophils with both CLEC5A and TLR2 ablation.77 While in bacterial infection-induced ARDS, CXCL2-CXCR2 signaling activation of neutrophils is more significant,78 because CXCL2 is more sensitive in response to molecules of bacterial origin.
Pulmonary pathological changes and underlying mechanisms
Due to systemic and pulmonary immunoinflammatory and immunothrombosis during ARDS, as well as subsequent disruption of the alveolar-capillary barrier, various cellular pathological changes, including various types of cell death, cellular senescence, and cellular dysfunction, have been demonstrated to occur in damaged pulmonary tissue. The potential underlying mechanism involves disruption of intracellular functions, such as excessive ROS accumulation, endoplasmic dysfunction, and mitochondrial dysfunction.
Endothelial barrier dysfunction
The impairment or degeneration of tight junction proteins is thought to accelerate endothelial barrier disruption and play a vital role in hyperpermeability during ARDS. Plasma from severe COVID-19 ARDS patients could impair the endothelial barrier integrity of primary human pulmonary microvascular endothelial cells in vitro, as indicated by decreased endothelial resistance measured by electrical cell impedance sensing (ECIS), transendothelial electrical resistance (TEER) and loss of occludin.79 Moreover, reductions in pulmonary ZO-1 and occludin levels were also observed in sepsis-related ARDS patients.47 In the endothelial barrier injury associated with ARDS, several signaling pathways have been identified as key regulators, including METTL3-mediated N6-methyladenosine modification of tripartite motif-containing (Trim)59 mRNA,80 NOX4 activation of CaMKII/ERK1/2/MLCK and Akt-FoxO1/3a signaling pathways,81 as well as CREB-mediated transcription of VE-cadherin.82 Although animal experiments targeting these signaling pathways have demonstrated efficacy, further research is needed to confirm their feasibility.
Cell-free hemoglobin
After the pulmonary capillary endothelium was destroyed, proteinaceous fluid and white blood cells flew into the alveolus, causing diffuse lung inflammation and coagulation.83 Red blood cells (RBCs) also crossed the pulmonary capillary endothelium and could be found in the alveoli of patients with ARDS.84,85 Lysis of RBCs within the intravascular and alveolar spaces results in the release of cell-free hemoglobin (CFH),86 which was harmful.85
The mechanism of CFH injury in acute respiratory distress syndrome may be specifically mediated through targeted cell surface receptor binding on the alveolar epithelium, as an in vitro study demonstrated that supplementation with antioxidants or iron chelators did not alter the effect of methemoglobin.87 Additionally, hemoglobin increased leukocyte-endothelial adhesion and activated lung microvascular endothelial cells through TLR4 signaling under inflammatory and hemolytic conditions.88 Similarly, a recent study of Schaaf KR reported that CFH was elevated in the airspace of most patients with ARDS and caused severe inflammation, and TLR4 on alveolar macrophages mediated the CFH-induced lung inflammation.89 These data suggest that TLR4 may be the key to targeting CFH in ARDS treatment.
CFH could be detected in the plasma of 80% of patients with sepsis,90 which was associated with mortality in patients with ARDS.91 This data has been used to argue the design of a clinical trial aimed at investigating acetaminophen’s effectiveness as a treatment for ARDS.92
Decreased resolution of pulmonary edema
Most patients with ARDS had impaired ability to clear pulmonary edema, which was associated with a higher mortality rate.93 Several mechanisms influence the resolution of alveolar edema in patients with ARDS, with the death of alveolar epithelial cells being the primary mechanism.94
Sodium enters through apical channels, especially the epithelial sodium channel (ENaC), and is then expelled into the lung interstitium by the Na/K-ATPase situated on the basolateral side. This process generates a localized osmotic gradient that facilitates the reabsorption of the water content from the edema fluid within the airspaces of the lungs.94 Moderate hypoxemia reduced apical sodium uptake through transcriptional effects and impaired ENaC transport, resulting 50% reduction of alveolar fluid clearance (AFC).95 In addition, cytokines in the airspace, including IL-1β, IL-8, and TGF-β, reduced vectorial fluid transport in alveolar epithelial cells by decreasing the expression and function of Na/K-ATPase and ENaC.96,97,98,99,100 There was also evidence that alveolar epithelial cell injury and dysfunction might be partially caused by mitochondrial damage leading to low intracellular ATP levels.101 Influenza virus infection could impair the function of ENaC, while bacterial and viral products could damage alveolar epithelial cells directly or indirectly.102,103,104 Therefore, multiple factors may lead to decreased resolution of pulmonary edema, revealing the complexity of improving AFC.
Cellular pathological changes
In the pathophysiology of ARDS, macrophages, neutrophils, alveolar epithelial cells, endothelial cells, etc., influence the pathological progression of ARDS through various mechanisms, mainly including cell death, cellular senescence, and cellular dysfunction, shown in Fig. 3.60,105,106,107,108,109,110,111,112,113,114,115
Cellular pathological changes in pulmonary tissue. In the pathological process of ARDS, neutrophils, macrophages, alveolar epithelial cells, endothelial cells, etc., interact with each other through various cytokines, leading to pathological changes including efferocytosis, NET formation, senescence, apoptosis, pyroptosis, ferroptosis, etc. *DAMPS damage-associated molecular patterns, MCP monocyte chemoattractant protein, MAPK mitogen-activated protein kinase, IL interleukin, METTL methyltransferase, GPX glutathione-peroxidase, NET neutrophil extracellular trap
Classifications and phenotypes
ARDS exhibits clinical heterogeneity. ARDS can be divided into subphenotypes based on clinical features, causes of lung injury, effective biomarkers, or clinical and biological variables. This heterogeneity may explain the lack of benefit observed in most randomized controlled trials (RCTs) evaluating various treatment strategies.116 One study reported that the ARDS subphenotype was stable within the first three days of enrollment, indicating that subphenotypic identification is feasible in clinical trials.117 Accurate subphenotypic classification of ARDS will improve clinical outcomes.
Clinical subphenotypes
Latent class models are applied to identify subphenotypes. Based on the clinical and biological data of two ARDS RCTs, Calfee CS et al. identified two ARDS subphenotypes (hyperinflammatory and hypoinflammatory).118 Compared to the hypoinflammatory subphenotype, the hyperinflammatory subphenotype was characterized by higher plasma levels of inflammatory biomarkers, a greater incidence of vasopressor use, lower serum bicarbonate levels, and a greater incidence of sepsis, with higher mortality and fewer ventilator-free days (VFDs) and organ failure-free days in both the ALVEOLI and ARMA cohorts.118 Data from several large-scale RCT studies indicates that the proportion of the hyperinflammatory phenotype is approximately 30–40%118,119,120,121 Multiple subsequent studies have demonstrated the existence of hyper and hypoinflammatory subphenotypes in different ways.119,120,121
A cluster analysis study that included 3875 ARDS patients identified three additional clinical subphenotypes of ARDS. Subphenotype I (40%) was associated with fewer abnormal laboratory values and less organ failure, with the lowest in-hospital mortality rate and the most VFDs and ICU-free days (IFDs), which was similar to the findings reported for the hypoinflammatory subphenotype. A higher white blood cell (WBC) count, higher temperature, a higher heart rate, a higher respiratory rate (RR), lower systolic blood pressure (SBP), and younger age characterized subphenotype II (32%), which was similar to the hyperinflammatory phenotype. Subphenotype III (28%) was characterized by older age, elevated serum creatinine and blood urea nitrogen (BUN) levels, and lower serum bicarbonate levels, with the least VFDs and IFDs, and the highest mortality rate, which was correlated with organ dysfunction, older age, and acidosis. Furthermore, these results were verified in three RCTs (ALVEOLI, FACTT, and SAILS trials),122,123,124 with a significant interaction between the three subphenotypes and treatment strategies in the ALVEOLI and FACTT trials. However, no apparent heterogeneity in treatment responsiveness was observed in the SAILS trial,125 suggesting that the treatment approach used may be effective across all subphenotypes of ARDS, or that the subphenotypes identified in the ALVEOLI and FACTT trials may not be as relevant or distinct in the SAILS population. It highlights the importance of considering the specific context and population of each trial when interpreting and generalizing research findings. These findings enhance the understanding of ARDS clinical subphenotypes and could be beneficial for the development of phenotype-specific treatment approaches.
Rapidly improving ARDS subphenotypes
The LUNG SAFE study,23 a worldwide analysis of current ARDS epidemiology, found that nearly one-sixth of patients meeting the Berlin definition no longer met these criteria after 24 hours. Prior research suggested that using standardized ventilator settings could improve the Pao2 to Fio2 ratio (Pao2:Fio2) in some ARDS patients, leading to a Pao2:Fio2 ≤ 300 after 24 hours.126,127,128,129 This subphenotype was named rapidly improving ARDS (riARDS). Using data from the large ARDSNet clinical trial population, a secondary analysis of 4361 unique patients in randomized controlled trials indicated that 458 (10.5%) no longer met ARDS criteria on the first study day after enrollment, with better outcomes than ARDS lasting longer than one day.130 Despite the unclear underlying pathobiology, riARDS, typically defined by early extubation, is widely recognized as an increasingly prevalent subphenotype. However, by including data from 280 COVID-19 patients who received invasive mechanical ventilation during the second pandemic wave in three ICUs, it was found that riARDS was only present in 4% of patients and was linked to a 55% mortality rate.131 It seemed that riARDS was not common among COVID-19 patients and was not associated with any survival benefit, in contrast to previous reports for non-COVID-19-related ARDS. These findings might help us better understand the trajectory of ARDS and its relationship with prognosis in COVID-19 patients.
Longitudinal phenotypes
ARDS is a dynamic process; most previous studies have captured only cross-sectional data, and longitudinal studies are relatively scarce. Recently, a study attempted to identify longitudinal phenotypes of ARDS and explore the dynamic changes in ARDS phenotypes.132 Chen H et al. identified a three-class model with different severities of pulmonary mechanics, organ dysfunction, chest CT features, and outcomes. Class 1 (66.1%) had fewer abnormal laboratory values and less organ dysfunction. Class 2 (16.9%), characterized by the highest minute ventilation, driving pressure, mechanical power (MP), and ventilatory ratio, and the lowest PaO2/FiO2, was called the pulmonary mechanical dysfunction phenotype. Class 3 (17%) was characterized by the highest creatinine and lactate levels, the lowest bicarbonate level and mean arterial pressure (MAP), and a greater proportion of patients who received vasopressors and was termed the extrapulmonary dysfunction phenotype. The authors also observed a significant interaction effect between phenotypes and the PEEP strategy when evaluating 60-day mortality. Significantly, most patients exhibited phenotypic changes at least once during the first four days of invasive ventilation, which shows the significance of this longitudinal phenotype study.
COVID-19-related phenotypes
Since the COVID-19 pandemic, studies have attempted to determine the prevalence of previously described ARDS phenotypes in patients with CARDS. A preliminary analysis by Sinha P suggested that the hyperinflammatory phenotype of ARDS was less prevalent in COVID-19 patients than in patients in previous ARDS cohorts, which challenges the theory that a cytokine storm is involved in CARDS.133 However, two subphenotypes of CARDS were proposed, and class 2 showed increased expression markers of coagulopathy and end-organ dysfunction, with mild inflammation, and was associated with higher 28-day mortality than class 1.134 Confirmation of this phenotype may suggest an important role for vascular dysfunction in the course and development of CARDS.
A longitudinal study of CARDS revealed no evidence of respiratory subphenotypes using cross-sectional data based on respiratory variables. Nevertheless, two subphenotypes developed during the first days of mechanical ventilation according to time-dependent analysis, with subphenotype 2 characterized by increasing minute ventilation, mechanical power, and ventilatory ratios.135 This finding reveals the importance of time as a critical variable in future subphenotype analyses of CARDS. Gattinoni L et al. classified two phenotypes of COVID-19 pneumonia, among which Type H is characterized by high elastance, high right-to-left shunting, high lung weight, and high recruitability, with 20–30% of patients meeting the severe ARDS criteria.136 These findings indicate that respiratory system elastance and recruitability could be signs of COVID-19-related phenotypes. Compared to ARDS patients, CARDS patients exhibited a greater median best PEEP, more collapse at low PEEP, and less hyperdistension at high PEEP.137
Many different phenotypes are likely to exist, overlapping in many respects and distinct in others. Based on the evidence of overlapping characteristics present in multiple subphenotypes, multimodal “omic” technologies would be beneficial for the accurate identification of ARDS subphenotypes. However, current evidence suggests that faster and more accurate identification of different phenotypes of ARDS is important for improving survival rates and prognosis, which also highlights the need for multimodal “omic” technologies.
Biomarker-driven subphenotypes
Biological subtyping of patients with other pulmonary and nonpulmonary diseases could improve patient selection for clinical trials of targeted therapies.138,139 Wood SL et al. first grouped ARDS patients based solely on biomarker concentrations. Cluster analysis of 20 biomarkers of inflammation, coagulation, and endothelial activation was performed, and no clinical data or outcomes were evaluated. The results suggested that ARDS patients could be classified into two subphenotypes: the “uninflamed” phenotype and the “reactive” phenotype. Patients with a reactive phenotype had high plasma levels of markers of inflammation, coagulation, and endothelial activation (IL-6, IFN-γ, angiopoietin 1/2, and plasminogen activator inhibitor-1), with increased ICU mortality.140 The pathogenesis of ARDS differs between patients with pulmonary(ARDSp) and extrapulmonary(ARDSexp) lung injury, which is related to the identification of biomarker-driven subphenotypes. In ARDSp, the alveolar epithelium is primarily affected, while ARDSexp involves injury to the microvascular endothelial cells.141 Biomarkers can play a significant role in this differentiation, as they reflect the underlying pathophysiology. Calfee CS et al. demonstrated that biomarkers of lung epithelial injury (surfactant protein D (SP-D) and advanced glycation end product receptor (RAGE)) are significantly more abundant in ARDSp patients than in ARDSexp patients, while the level of an endothelial injury biomarker (Ang II) is considerably lower.142 Similarly, the concentrations of IL-1β and IL-18 in BALF were significantly greater in ARDSp patients than in ARDSexp patients.143 Variable ventilation strategies have demonstrated differential effects on biomarker expression in ARDSp and ARDSexp, suggesting that the mechanisms underlying respiratory improvement may vary between these subphenotypes.144 Sigh ventilation has been shown to reduce alveolar collapse and inflammation in pulmonary ALI, but its effects are more complex in extrapulmonary ALI, where it may increase markers of inflammation, apoptosis, and fibrogenesis.145
Gene expression also differs among ARDS subphenotypes. If differences in leukocyte gene expression are considered, the “reactive” subphenotype in ARDS patients with sepsis is characterized by neutrophil activation and oxidative phosphorylation, whereas the “uninflamed” subphenotype is characterized by enrichment of mitogen-activated protein kinase (MAPK) pathway.146 These results may explain the protective effect of simvastatin on the “hyperinflammatory” subphenotype,147 which is due to the antioxidative effect of simvastatin on endothelial cells148 and leukocytes.149
Supportive therapy of ARDS
A recent report from an expert panel in the UK suggested that supportive management of patients with ARDS caused by COVID-19 should follow existing evidence-based ARDS guidelines.150 Here, we consider the evidence regarding the use of ventilation strategies, prone positioning, extracorporeal support, neuromuscular blockade (NMB), and corticosteroids for the management of ARDS. We also have summarized differences and up-to-date recommendations on supportive therapy for ARDS of recent American Thoracic Society (ATS)151 and European Society of Intensive Care Medicine (ESICM)152 clinical practice guidelines, shown in Table 2.
Ventilation strategies
Noninvasive respiratory support, rather than conventional oxygen therapy, might be considered as the initial respiratory management approach for adult patients with acute respiratory failure who are suspected of having ARDS if there are no contraindications for noninvasive respiratory support and if organ failure other than respiratory failure is absent.153 Patients on a high-flow nasal cannula oxygen (HFNO) or noninvasive ventilation (NIV) should be carefully managed in an environment where tracheal intubation can be conducted after the start of noninvasive respiratory support.
High-flow nasal cannula oxygen
High-flow nasal cannula oxygen has gained traction over the past decade, in large part due to a multicentre trial showing decreased mortality compared with noninvasive positive pressure ventilation (NPPV) and standard oxygen therapy in patients with acute hypoxemic respiratory failure,154 as well as improved patient comfort compared with NIV and invasive mechanical ventilation (IMV). Clinical practice guidelines have strongly endorsed HFNO therapy over standard oxygen therapy for patients with hypoxemic respiratory failure, as its use has been associated with reduced intubation rates and reduced escalation of respiratory support.155 HFNO therapy may be considered for patients with ARDS if the airway protective reflex is intact and the patient has stable hemodynamics. The benefits of this approach include decreased respiratory effort due to the washout of the anatomic dead space.
Noninvasive ventilation
Noninvasive ventilation is frequently used in patients with ARDS, although its use remains controversial. The potential benefits include the avoidance of ventilator-associated events and the need for deep sedation, which often occurs with IMV. In addition, appropriately titrated end-expiratory pressure could decrease injury related to vigorous spontaneous breathing.156 Potential harms include delayed (necessary) intubation, inability to control tidal volumes and monitor airway pressures, and an inconsistent mask seal, which could lead to cyclic recruitment-derecruitment of lung units, causing atelectrauma. A small randomized trial using a full-helmet interface in patients with moderate to severe ARDS showed reductions in the rates of intubation and mortality compared with those of standard facemask NIV.157 A study using a helmet interface (compared with HFNO) in patients with CARDS did not show a mortality benefit. Nevertheless, it did demonstrate reductions in intubation rate and ventilator days.158 Helmet NIV, which requires familiarity with the technology, is not routinely available in most hospitals and would benefit from further study in real-world settings before its widespread use.
Management with invasive mechanical ventilation
Lung-protective ventilation
Lung-protective ventilation (i.e., tidal volumes of <6 ml/kg of predicted body weight and plateau pressure ≤30 mm Hg) is a key recommendation based on the findings of the landmark ARMA trial,159 which showed reduced mortality and increased ventilation-free days. RCTs of novel ventilatory strategies have continued to reinforce the benefit of lung-protective ventilation.160,161,162
PEEP
PEEP is the pressure that maintains some degree of inflation during the end-expiratory pause. Higher PEEP increases the mean airway pressure, which usually improves oxygenation. And maintaining inflation during exhalation also decreases atelectrauma.163 The most commonly used method for PEEP selection is to apply an algorithm matching PEEP to the FiO2 the patient requires,159 which was tested in clinical trials by the ARDS network (ARDS Net) in the USA and is relatively simple to apply: the higher the fraction of oxygen required is, the higher the selected PEEP is. Three large trials122,164,165 tested the hypothesis that a higher-PEEP protocol would improve survival compared with the traditional ARDS Net PEEP protocol. However, no substantial differences in clinical outcomes were observed in any of the three trials, suggesting that a high-PEEP strategy was not superior for all patients with ARDS. Another trial applying an aggressive high-PEEP strategy plus high-pressure recruitment maneuvers revealed a statistically significant increase in mortality in the intervention arm.166 Therefore, heterogeneity of individual patient responses to PEEP strategies is recognized,167 leading to increasing interest in personalized PEEP strategies, although these strategies have not been demonstrated to yield additional benefits over conventional PEEP strategies.166,168
Driving pressure
Driving pressure (i.e., plateau pressure minus end-expiratory pressure) might be an independent predictor of survival in patients with ARDS.160 Amato et al. demonstrated that driving pressure was the key mediator of the benefits of PEEP and tidal volume strategies. An upper limit of 15 cm H2O for driving pressure is recommended, which could cause considerable lung stress169 and increased mortality.23,160 Conversely, two clinical trials revealed increased mortality in the setting of lower driving pressure (i.e., ≤15 cm H2O), suggesting that driving pressure might not be as valuable as initially expected for predicting mortality.166,170
Mechanical power
Mechanical power is a novel concept applied in the context of ARDS. MP refers to the amount of energy per unit of time transmitted to the respiratory system by a mechanical ventilator, as determined by volume, pressure, flow, and respiratory rate.171,172 MP might be a better driver of lung-protective ventilation than individual ventilator parameters, as it considers the balance of several parameters as a whole.173 Reanalyses of clinical trials and observational data showed that MP was associated with increased mortality.174,175 In a retrospective analysis of 8207 patients, a consistent increase in the risk of death was observed with an MP greater than 17 J/min.176 The complexity of interpreting MP limits its clinical use. However, recently, it was found that the driving pressure and RR components of MP were the best predictors of mortality.161 Although these variables can be easily measured at the bedside, the additional benefits of MP remain uncertain.
Prone positioning
In the supine position, the V˙/Q˙ mismatch leads to poor oxygenation. Shifting to the prone posture has several advantages, including reversal of the gravitational forces that move surrounding structures such as the heart and diaphragm, ultimately leading to more homogeneous lung perfusion. Starting from the observation that oxygenation improved in patients in the prone position, studies identified several physiological mechanisms underlying this improvement, including a decrease in the differential distribution of ventilation between the ventral and caudal lung regions and a shift in the density distribution of the edematous lung, increasing the V˙/Q˙ ratio.177,178 A series of randomized trials179,180,181,182 paralleled the evolution of this pathophysiological understanding. However, none of these trials individually showed a survival benefit of prone positioning; post hoc analysis suggested a potential benefit for the most severely hypoxemic patients when the prone position was combined with low stretch ventilation and applied for more extended periods (16 h).183 Based on these findings, a prospective study examined prone ventilation for 17 hours daily for patients with moderate or severe ARDS and showed a statistically significant survival benefit.184 Thus, the prone position should be strongly considered for patients meeting certain criteria (PaO2/FiO2 ratio persistently <150) without contraindications.
During the COVID-19 pandemic, prone positioning was used successfully in awake, non-intubated patients with acute hypoxemic respiratory failure.185,186 However, its benefit remains uncertain, with conflicting findings from clinical trials.187,188 As an adjunct to extracorporeal membrane oxygenation (ECMO) therapy, which is safe and effective, the use of the prone position was associated with a greater probability of surviving and being weaned off of ECMO at 90 days in a clinical trial.189 In another RCT involving 170 patients, prone positioning did not significantly reduce the time to successful weaning of ECMO compared with supine positioning in patients with severe ARDS supported by VV-ECMO.190
Complications resulting from prone positioning are rare. The PROSEVA study revealed no significant differences between groups in terms of nonscheduled extubation, hemoptysis, mainstem bronchus intubation, or cardiac arrest.184 A meta-analysis of eight RCTs revealed that patients with ARDS who underwent prone positioning had greater rates of endotracheal tube obstruction and pressure sores.191 Awake-prone positioning is also safe, with studies demonstrating no increased risks of complications or slightly increased rates of skin breakdown, line dislodgement, back pain, or generalized discomfort.187,192,193 However, careful attention must be given to the proning procedure to avoid disruption of vascular access catheters and endotracheal tubes and, while the patient is prone, to avoid pressure-related complications.
Neuromuscular blockade
The use of NMB in patients with moderate to severe ARDS has the potential benefit of decreasing ventilator-associated lung injury and improving mortality at 28 days without increasing the incidence of neuromuscular weakness.194 A large randomized study identified an adjusted mortality advantage of NMB (cisatracurium) in deeply sedated patients with moderate or severe ARDS.195 In addition, subsequent trials failed to show survival benefits in patients with moderate or severe ARDS who were randomly assigned to receive cisatracurium with deep sedation for 48 h compared with light sedation if tolerated and goal-oriented sedation if not tolerated.196,197 Importantly, in both trials, the duration of NMB in the study protocol was intentionally short (≤48 h), with no difference in the incidence of ICU-acquired weakness with NMB. Although NMB is thus not mandated for patients with moderate or severe ARDS, bolus and/or short-duration infusions of NMB agents are safe and could improve gas exchange and ventilator synchrony.
NMB must be used cautiously for patients who are unable to achieve ventilation synchrony within lung-protective targets, for patients with severe hypoxemia despite deep sedation, and for patients whose plateau pressures are high or difficult to measure accurately. Once initiated, clinicians should consider daily whether NMB remains helpful and consider discontinuation at the earliest opportunity.
Extracorporeal support
During the era of lung-protective ventilation, two RCTs, CESAR198 and EOLIA,199 investigated the role of venovenous ECMO for severe ARDS patients, with somewhat conflicting results. A post hoc Bayesian analysis showed a high probability that early ECMO was beneficial.200 Furthermore, in a subsequent meta-analysis of individual patient data, including both the CESAR and EOLIA RCTs, the precision of the treatment effect improved (combined data for 429 patients). A statistically significant improvement in 90-day mortality was observed in the ECMO group.201,202 Extracorporeal carbon dioxide removal (ECCO2R) is a low-flow form of venovenous support that has been studied in ARDS patients. The REST trial,203 which investigated ECCO2R in patients with acute hypoxaemic respiratory failure, revealed no difference in 90-day mortality, and there was an increased incidence of serious adverse events, including clinically significant bleeding, the need for more sedation and NMB and a longer duration of mechanical ventilation, in the ECCO2R group. On this basis, the use of ECCO2R for the treatment of ARDS is not recommended outside RCTs.
Evidence of the benefit of ECMO has been extended to COVID-19 patients.204 A comparative effectiveness study including 844 of 7345 eligible patients (11.5%) with COVID-19-associated respiratory failure who received ECMO in five countries was recently conducted; the results indicated that ECMO was associated with reduced mortality compared with that of supportive therapy.205 Although confirmation in an RCT would be desirable, these findings provide reassurance regarding the use of ECMO in a select population of patients with severe COVID-19.
Taken together, these data suggest that patients with severe ARDS could benefit from treatment with ECMO. Notably, patients receiving ECMO should receive an overall management strategy similar to that used in the EOLIA trial or comply with the criteria for ECMO defined by expert groups.206
Corticosteroids
Steroids have potent anti-inflammatory effects that could benefit patients with ARDS, but the role of corticosteroids in ARDS management has long been controversial. An early trial investigating the use of methylprednisolone (MPS) in patients with persistent ARDS revealed an association with an increased risk of late mortality (i.e., day 60 and day 180) when steroids were initiated beyond day 14 after ARDS onset.207 A multicentre trial investigated a high dose (i.e., 20 mg once daily for five days) followed by a lower dose (i.e., 10 mg once daily for five days) of dexamethasone, indicating that early administration of dexamethasone could reduce the duration of mechanical ventilation and overall mortality in patients with established moderate-to-severe ARDS.208 Consistently, a subsequent meta-analysis of 999 patients from eight RCTs with ARDS revealed a mortality benefit of corticosteroid use.209 However, steroid regimens differed between studies (e.g., different types, doses, and durations), and there were differences in the patient populations investigated (e.g., early vs. late ARDS and some studies were performed before lung-protective ventilation).
Corticosteroid use has increased after positive results of clinical trials of dexamethasone in patients with COVID-19 pneumonia,210 and a subsequent meta-analysis reported similar results.211 There was evidence of an association of corticosteroid use with hyperglycemia, but no specific evidence supports concerns about other adverse events. However, we must note that the results of the study performed by Moreno G showed that the use of glucocorticoids as coadjuvants was significantly associated with increased ICU mortality in patients with severe influenza pneumonia, suggesting that corticosteroids should not be used as coadjuvant treatment for patients with influenza pneumonia.212 Therefore, the potential benefits and harms of corticosteroid use in ARDS patients, especially those with influenza pneumonia-induced ARDS, still need stronger clinical evidence.
Cell therapy
In recent years, cell therapy has shown great promise in preclinical ARDS research. A wide range of cells have been identified as potential candidates, especially mesenchymal stromal cells whose therapeutic potential in treating ARDS has been confirmed in multiple preclinical studies and even clinical trials. The therapeutic effects of these cells mainly occur via two different mechanisms: direct cell interactions and the paracrine release of cellular components such as extracellular vesicles (EVs). Here, we summarize the latest mechanisms of different cell therapies for ARDS.
MSC-based cell therapy
MSC-based cell therapy in preclinical studies
Several animal studies have demonstrated that MSC therapy is a promising novel intervention for ARDS. The actions of MSCs involve several mechanisms, which are described in Fig. 4.
MSC-based cell therapy in ARDS. MSCs have demonstrated strong capabilities in the treatment of ARDS, mainly including regulating the differentiation of alveolar epithelial cells, activating immune cells such as dendritic cells and macrophages to modulate immune function, repairing barrier function, and exerting anti-inflammatory and anti-apoptotic effects. *AECII type II alveolar epithelial cells, AECI type I alveolar epithelial cells, YAP Yes-associated protein, SPC surfactant protein C, LGALS3 galectin3, T1α podoplanin, FoxM Forkhead box (Fox) transcription factor family, DCs dendritic cells, HGF hepatocyte growth factor, PGE prostaglandin, Ach acetylcholine, AFC alveolar fluid clearance, CXCL C-X-C motif ligand, HO-1 heme oxygenase-1
Anti-inflammatory effects
The anti-inflammatory pathway is a key mechanism underlying the treatment of ARDS with MSCs. After autologous transplantation of bone marrow-derived mesenchymal stromal cells (BM-MSCs) into sheep, decreases in total inflammatory cell numbers, neutrophil numbers, macrophage numbers, proinflammatory cytokine levels (IL-6 and tumor necrosis factor-alpha (TNF-α)), and total protein, IgM, and albumin levels were observed, while the level of an anti-inflammatory cytokine (IL-10) increased. BM-MSC transport can reduce local and systemic levels of inflammatory factors.213,214 Both adipose-derived mesenchymal stromal cells (AD-MSCs) and umbilical cord-derived mesenchymal stromal cells (UC-MSCs) attenuate inflammation and modulate inflammatory factors.215,216 Recently, Zhang X et al. proposed a novel potential anti-inflammatory mechanism of MSCs in ARDS involving the cholinergic anti-inflammatory pathway (CAP). The therapeutic efficacy of BM-MSCs can be significantly reduced by blocking the vagus nerve, administering drug inhibitors, or implementing gene knockout to inhibit CAP, and BM-MSC-derived prostaglandin E2 (PGE2) can promote acetylcholine (Ach) synthesis and release. Based on the efficacy of nAChR and α7nAChR agonists, a clinical study revealed that lobeline, a nicotinic cholinergic receptor agonist, attenuated pulmonary inflammation and alleviated respiratory symptoms in ARDS patients.24
Regulation of cell differentiation
In the late phase of ARDS, type II alveolar epithelial cells (AECIIs) differentiate to repair damaged type I alveolar epithelial cells (AECIs) due to their high progenitor cell capacity.217,218 FoxM1 is a member of the Forkhead box (Fox) transcription factor family, which is crucial for the differentiation of AECIIs into AECIs after ALI.219,220 BM-MSCs overexpressing FoxM1 attenuate pulmonary edema and fibrosis, mitigate oxidative damage and inflammatory responses, and restore vascular integrity221 via the Wnt/β-catenin pathway.222 Yes-associated protein (YAP) is also an essential molecule for the differentiation of AECIIs into AECIs. In particular, hUC-MSCs could inactivate YAP on AECIIs, thus inducing AECII differentiation into AECIs.223
In addition to promoting the differentiation of AECIIs into AECIs, MSCs can also differentiate directly into AECIIs, which is associated with the Hippo signaling pathway. Lats1 knockdown inhibits Hippo signaling activity in mBM-MSCs, thus increasing the retention of mBM-MSCs in ARDS lung tissue. mBM-MSCs with downregulated Hippo signaling differentiated into alveolar epithelial cells, reinforcing alveolar epithelial tight junctions.224 Significantly, when Lats1 activity decreases, YAP remains unphosphorylated, which stimulates the proliferative and antiapoptotic effects of the Hippo signaling pathway, thus promoting cell proliferation.225 In addition, activation of the noncanonical Wnt5a/JNK and/or Wnt5a/PKC pathway(s) promotes the differentiation of BM-MSCs into AECIIs and promotes their migration to injured lung tissue.226 The migration ability and homing ability of BM-MSCs in damaged lung tissue could also be enhanced by Vimentin-Rab7a and ROR2.227,228
Immunomodulation
HGF-overexpressing MSCs promote the differentiation of mature DCs (mDCs) into tolerogenic dendritic cells (DCregs) via direct cell‒cell contact, thus reducing ALI through the HGF/Akt pathway and the Notch pathway.229,230 Additionally, PGE2-primed hP-MSCs promote the polarization of macrophages from the M1 to M2 and regulate cytokine production, exerting strong protective effects against LPS-induced ALI.231 Preconditioning MSCs before administration alleviates ARDS by enhancing their immunomodulatory capacity, for example, BM-MSCs preconditioned with ARDS serum exert stronger immunotherapeutic effects through VEGF and PGE2.232
Anti-apoptosis effects
Alveolar epithelial injury is the primary pathophysiological mechanism underlying ARDS. BM-MSCs inhibit the apoptosis of alveolar epithelial cells in mice with ALI through the CXCL12/CXCR4 signaling axis.233 MSC-CM alleviates neutrophil apoptosis in the context of endotoxin-induced ALI by inhibiting the NF-κB pathway.234 BM-MSCs overexpressing HO-1 could improve the survival rate and attenuate lung impairment in ALI rats by inhibiting apoptosis and enhancing the paracrine effects of MSCs.235
Administration
One study compared different routes of stem cell administration; endobronchial and intravenous administration were equally effective for treating ARDS in sheep. The authors observed by endobronchial [18F]-FDG that labeled cells were trapped inside the lung with no systemic distribution. Administration via the intravenous route leads to a systemic distribution of the cells, which mainly lodge in the lung.236 Interestingly, whether MSC therapy is beneficial depends on the lung microenvironment at the time of administration. The results of one study showed that MSCs may have detrimental effects on the lung environment, inducing high levels of both IL-6 and fibronectin (FN) and low antioxidant capacity. Improving the lung environment before MSC administration could enhance the lung-protective effects of MSCs.237
Gene regulation
A study profiled the microRNAome and transcriptome of lungs from mice with endotoxin-induced ALI that were treated with either a placebo or MSCs and showed that MSCs regulate the expression of miR-27a and its various target genes, including VAV3, which is involved in sepsis-induced lung injury. In addition, increased miR-27a-5p expression was observed in patients who died from ARDS and had autopsy-proven diffuse alveolar damage (DAD) compared with patients who did not have DAD.238 BM-MSC-CM decreased miR-193b-5p expression and increased occludin protein expression in the lungs of septic mice model, and alleviated the loss of barrier function. Importantly, miR-193b-5p expression was increased and occludin protein expression was markedly decreased in lung autopsy samples from ARDS patients compared to those from non-ARDS controls. In addition, a study compared the minicircle DNA system to a conventional plasmid vector for the transfection of BM-MSCs; the results showed that minicircles can achieve more efficient and sustained expression of ANGPT1, further enhancing the therapeutic effect in an ALI mice model.239
Barrier function recovery
Hepatocyte growth factor (HGF) is required for the ability of BM-MSCs to restore lung permeability and ameliorate lung injury induced by LPS.240 HGF secreted by BM-MSCs promotes vascular endothelial barrier recovery via activation of the mTORC2/Akt pathway.241 TEER measurements, permeability assays, and immunohistological findings revealed that AD-MSCs enhance the barrier function of lung epithelial cells in vitro.242 Interestingly, BM-MSCs preconditioned by mechanical stretching in vitro also restore the permeability of endothelial cells treated with LPS.243 Moreover, BM-MSCs had the ability to restore AFC in an ex vivo perfused human lung, which was partially attributed to the increased sodium-dependent resolution of alveolar edema.244,245
MSC -based cell therapy in clinical studies
Clinical therapy with MSCs in ARDS patients
To date, many clinical studies have demonstrated the benefits of different MSC treatments in ARDS patients, as indicated by reduced inflammation and alveolar permeability and improved lung function, including tidal volume and compliance.246,247,248 Most trials have used 106 cells/kg, with the highest dose of 107 cells/kg being safe. Although some adverse events have been observed in trials, it has been proven that there is no correlation with MSC treatment. Notably, Simonson OE et al. described a 5-year follow-up of 2 patients with severe refractory ARDS who received a single intravenous injection of BM-MSCs at a dose of 2 × 106 cells/kg, including health-related quality of life (HRQoL), physical capacity, and pulmonary morphology and function. Both patients fully achieved a full physical and mental recovery.248,249 However, extensive studies with long follow-up periods are needed to confirm the safety of these treatments because of the small sample size. We look forward to the results of an ongoing phase III clinical trial of MSC therapy for ARDS. Additionally, the viability and efficacy of MSCs require more attention. More details are shown in Table 3.215,246,247,248,249,250,251,252,253
Clinical therapy with MSCs in CARDS patients
Although MSCs have been used to treat various diseases without safety concerns, these results may not be directly applicable to patients with COVID-19. Several trials have confirmed the safety of MSCs for treating SARS-CoV-2-induced ARDS, and MSC therapy has also been shown to improve the survival rates and clinical outcomes of patients.254,255,256 However, no efficacy of MSCs in patients with CARDS was demonstrated in two trials.257,258 Notably, patients who develop sepsis or multiorgan failure may not be good candidates for stem cell therapy because the death occurred 5-19 days after the first MSC infusion in four patients with multiorgan failure or sepsis.259 More details of these trials are shown in Table 4.254,255,256,257,258,259,260,261,262,263,264,265,266,267
Non-stem cell-based cell therapy in ARDS patients
In addition to stem cell treatment, several cell types, such as alveolar type II cells, mononuclear cells, and immune and matrix regulatory cells, have potential therapeutic effects on ARDS.
Type II alveolar epithelial cells
Like MSCs, AECIIs are recognized progenitor cells in the alveoli. These cells can rapidly proliferate and differentiate into AECIs after epithelial cell injury in the context of ARDS. Moreover, the underlying immunoregulatory and anti-inflammatory properties of AECIIs can restore pulmonary immune and inflammatory homeostasis under pathological conditions in ARDS.268 Intratracheal instillation of AECIIs was reported to elevate the levels of surfactant protein A (SPA) and SPC in the alveoli, thus exerting anti-inflammatory effects and consequently maintaining lung homeostasis in rats with ARDS. In addition, the anti-inflammatory effect of AECIIs was also demonstrated by their regulation of alveolar macrophage (AM) polarization, which is associated with a decreased AM1/AM2 ratio and alleviation of pulmonary inflammation.268 AECII treatment is comparable to MSC therapy. In rats with LPS-induced ALI, attenuated pulmonary inflammation has been observed after both MSC treatment and AECII treatment, with diminished expression of proinflammatory cytokines, fewer apoptotic cells in lung tissue, and restored pulmonary architecture in the two groups.269 All these results from preclinical models of ALI/ARDS have revealed the protective effects of AECII treatment and provided a potential therapeutic direction for ARDS treatment. However, there is still a paucity of data related to AECII treatment for patients with ARDS in the clinic.
Immunity- and matrix-regulatory cells
In a preclinical mouse model of ALI, Jun et al. generated immunity- and matrix-regulatory cells (IMRCs), which are derived from human embryonic stem cells (hESCs).270 Because of their high expression of immunomodulatory and matrix-regulatory genes, IMRCs exhibit superior immunomodulatory and antifibrotic potency under pathological conditions. Compared with traditional stem cell therapy and pirfenidone injections, intravenous administration of IMRCs to mice with ALI significantly improved lung tissue repair and exerted antifibrosis effects in a dose-dependent manner. Thus, hESC-derived IMRCs are expected to be an alternative cell therapy for ARDS treatment. However, the safety and efficacy of these treatments need to be evaluated in other studies.
Cell component therapy for ARDS patients
Extracellular vesicle-based therapy for ARDS patients
Although stem cells have therapeutic effects, they also have several disadvantages and adverse effects. Several cell products derived from stem cells, especially from MSCs, have been explored for efficacy and safety in the context of ARDS treatment. Among these cell products, stem cell-derived EVs play a central role in lung injury repair and respiratory function restoration and have advantages over MSC therapy, including low immunogenicity, prolonged in vivo stability, high delivery efficiency, and a low risk of inducing iatrogenic tumor formation.271 An increased number of microvesicles (MVs) has been observed in both ARDS patients and rodents with ALI, which indicates the critical role of MVs, especially EVs, in the initiation, development, and progression of ARDS. Endothelial cell-derived microparticles and leukocyte microparticles in the circulation have been identified as prognostic markers of ARDS development in clinical patients with sepsis.272,273 In a prospective trial, EV-derived or EV-encapsulated miRNAs were reported as biomarkers to distinguish ARDS patients with or without COVID-19, which might provide a new direction for treating CARDS,274 shown in Fig. 5.
Extracellular vesicle-based therapy in ARDS. EVs secreted by MSCs or other cells primarily exert their effects by cargos such as miRNAs and mitochondria. These contents can alleviate alveolar-capillary barrier damage, and regulate macrophage function, thereby achieving anti-inflammatory and immune regulatory functions. *EVs extracellular vesicles, MSC mesenchymal stromal cell, epi-EVs epithelium-derived extracellular vesicles, endo-EVs endothelium-derived extracellular vesicles
Nowadays, EVs, including MSC-derived EVs and EVs derived from other cells, which attenuate ALI mainly by regulating cellular activities such as apoptosis and autophagy,275 mitochondrial function, and alveolar epithelial-capillary barrier integrity in pulmonary tissues, have been widely applied in animal models of ARDS/ALI. Macrophage dysfunction appears to be essential in the pathogenesis of ARDS, and targeting macrophage dysfunction might thus be a therapeutic direction for treating ARDS. MSCs-EVs or MSCs-MVs promote macrophage phagocytosis of pathogens in lung tissue, thus attenuating pulmonary inflammation and lung injury in both mouse and rat ALI models.276,277 Further investigation demonstrated that miR-181a-5p enveloped in MSC-EVs could upregulate pSTAT5 and SOCS1 expression in alveolar macrophages, exerting anti-inflammatory and immunomodulatory effects in the context of ARDS.278 Additionally, MSCs-EVs modulate macrophage phenotypes and enhance polarization to the anti-inflammatory and highly phagocytic phenotype, which mainly depends on improved macrophage oxidative phosphorylation in mitochondria due to EV-mediated mitochondrial transfer.279 MSCs-EVs can regulate alveolar macrophage autophagy, enhance homeostasis in alveolar macrophages, and alleviate mitochondrial dysfunction-mediated barrier damage, thus reducing lung injury during ARDS via EV-mediated mitochondrial transfer.280,281,282,283 AD-MSC-EV administration also regulates endothelial functions in pulmonary tissue, with inhibition of lung hemorrhage and edema, attenuation of vascular hyperpermeability, and promotion of vascular repair in mice with ALI284; these effects rely on PI3K/Akt activation by EV-encapsulated miR-126 in endothelial cells.285 These findings indicate that MSCs-EVs exert powerful effects during ARDS therapy.
Interestingly, the anti-inflammatory and immunomodulatory properties of alveolar macrophages can also be regulated by epithelium- and endothelium-derived EVs (epi-EVs or endo-EVs) that target RGS1 activation and mediate the intracellular Ca2+ response in the context of ARDS, mainly through miR-27b-3p and miR-223, respectively.286 The intratracheal administration of endothelial progenitor cell-derived EVs (EPC-EVs) also reduces vascular permeability and inflammation via the overexpression of tight junction proteins, which suggests that EPC-EVs have endothelial protective effects in ARDS.287 However, contrary to previous results, pulmonary epithelial cell-derived EVs were reported to activate alveolar macrophages and aggravate pulmonary inflammation during ARDS because they are hyperoxia-induced, enriched in caspase-3, and thus proinflammatory.288 Thus, more research is needed to elucidate the potential prognostic and therapeutic effects of epi-EVs in ARDS.
Plasma therapy and plasma protein-based therapy
In recent decades, plasma therapy and plasma protein-based therapies have been widely used to treat patients with severe CARDS. However, convalescent plasma therapy (CPT) is controversial since previous research has shown conflicting outcomes in terms of the benefit or lack of benefit of this treatment. Recently, two randomized, double-blind, multicentre, phase 2 and phase 3 clinical trials have been conducted to investigate the efficacy and safety of CPT for severe influenza infection.289,290 The study results did not suggest that CPT has superior therapeutic effects compared to nonimmune plasma therapy, while convalescent plasma treatment seems safe and well tolerated. Shen and colleagues reported decreased viral loads and increased neutralizing antibody levels in CARDS patients’ plasma after CPT, and the patients’ symptoms and outcomes improved as well.291 Inspired by these case series, two clinical trials have been performed, with conflicting results. In the first study, when CARDS patients were treated with plasma, clinical improvements were observed, including reductions in disease severity, length of ICU stay, and the need for mechanical ventilation and better oxygenation,292 which indicates the efficacy of CPT in patients with CARDS. In contrast, in the second study, although no adverse effects were observed in the CPT group, significant improvements in clinical outcomes were not detected after CPT.293 The discrepancy between these two studies might be related to the use of different sources of CP resources, leading to a potential difference in the antibody level of the donors.
Further studies have investigated the presence of immunoglobulins and other monoclonal antibodies in the plasma to eliminate confounding factors. Intravenous immunoglobulins (IVIGs) can improve clinical outcomes in patients with CARDS by reducing mortality, length of ICU stay, and duration of mechanical ventilation.294,295,296,297 However, a multicentre, double-blind, placebo-controlled trial confirmed that IVIGs do not improve primary clinical outcomes, with a similar number of ventilation-free days on day 28 with or without IVIGs.298 In addition, IVIGs seem to increase the incidence of several serious adverse events in ARDS patients, such as septic shock, acute kidney injury, and bacterial pneumonia. There are two possible reasons for the differences in the results of these studies. First, the beneficial effects of IVIGs have been reported in retrospective observational studies, which are more prone to selection bias. Second, a nonbeneficial or detrimental impact of IVIGs has been demonstrated in more severe ARDS patients, which might cause poor clinical outcomes, even without IVIGs.
Targeted therapy
Targeted therapy is a treatment strategy in which specific molecules associated with a disease are targeted to regulate pathological and physiological processes and achieve therapeutic goals. Compared to traditional broad-spectrum methods, targeted therapy is more effective and has fewer side effects.299 Targeted therapy can be achieved through the use of antibody drugs,300 small molecule targeted drugs,301 gene therapy,302 or RNA interference technology.303 It is a highly personalized treatment approach that requires a deep understanding of the molecular mechanisms of the disease and has a wide range of applications thanks to the development of genomics and proteomics techniques.
Treatments targeting the immune system
Advantages
Since consensus on the definition of ARDS was reached in 1988, scientists have been trying to find specific therapeutic drugs for ARDS. However, many potential drugs have failed in clinical trials, mainly due to the significant clinical and biological heterogeneity of ARDS147; for example, the “low inflammatory” subtype and “hyperinflammatory” subtype,147,304 have different therapeutic characteristics. Individualized treatment plans can be selected for patients receiving targeted therapy based on phenotype and molecular pathology characteristics. This approach can achieve site-specific drug delivery and has good potential for reducing off-target effects and unnecessary toxicity and enhancing the therapeutic effects of drugs.301 Immune dysregulation is a vital pathogenic mechanism of ARDS that is characterized by sustained and excessive activation of the inflammatory response, abnormal elevation of cytokine levels, and suppression of anti-inflammatory responses. The immune phenotypes of different ARDS patients may be significantly different,305 so treatments targeting the immune system have become a vital approach for ARDS patients.
Targeted immunomodulatory therapies
Targeted immunomodulatory therapies for non-COVID-19-induced ARDS
-
(1)
Neutrophils
Neutrophils are the primary immune cells that cause the inflammatory response in ARDS. Sivelestat, a neutrophil elastase inhibitor, has been approved in Japan for the treatment of ALI in patients with systemic inflammatory response syndrome. A phase IV clinical trial recruited 177 patients in the Sivelestat group and 15 patients in the control group. The results showed that compared to those in the control group, the adjusted extubation rate and ICU discharge rate were significantly greater in the Sivelestat group, with a considerably higher adjusted 180-day survival rate (71.8% vs. 56.3%).306 A retrospective study also demonstrated that Sivelestat had beneficial effects on sepsis-related ARDS.307 In addition, a meta-analysis including six RCTs with a total of 804 ALI/ARDS patients showed that sivelestat may increase PaO2/PaCO2 but has little or no effect on the 28-30-day mortality rate, ventilator days, or duration of ICU stay.308 However, larger sample sizes are needed to verify the effectiveness of Sivelestat in the treatment of ARDS.
-
(2)
TNF-α
TNF-α is an essential inflammatory factor involved in ARDS that can induce cell death and inflammatory responses after binding to TNFR 1 and TNFR 2 on the cell membrane. In the context of acute injury, selective inhibition of TNFR1 may reduce the adverse effects associated with TNF-α while preserving or enhancing the protective effects of TNFR2. Based on this mechanism of action, the inhalation of GSK 1995057, a selective TNFR1 antagonist, is considered a possible therapeutic approach for preventing ARDS.309 A randomized controlled clinical trial involving 37 healthy individuals showed that the inhalation of GSK-1995057 can prevent the increase in neutrophil counts, inflammatory cytokine levels, and endothelial cell injury observed in healthy individuals exposed to inhaled endotoxin.310
-
(3)
GM-CSF
Granulocyte-macrophage colony-stimulating factor (GM-CSF) is a multifunctional cytokine that has potent effects on cell activation and differentiation and can enhance the antibacterial functions of bone marrow cells (macrophages, dendritic cells, and PMNs) and alveolar macrophages.311 Although a multicentre phase II trial showed that GM-CSF treatment in ARDS patients did not change the duration of mechanical ventilation compared to that of patients in the placebo group, it did reduce nonpulmonary organ failure and mortality (absolute reduction of 6%, relative reduction of 26%).312 Consistently, in phase II trials of sepsis patients with respiratory dysfunction, treatment with GM-CSF improved respiratory function.313
-
(4)
Vascular leakage
Vascular leakage is one of the main pathophysiological mechanisms of ARDS, and Abl family kinases are critical mediators affecting vascular permeability. Imatinib (STI-571, Gleevec) is a prototype Abl kinase inhibitor that has been shown to reduce the production of proinflammatory cytokines (TNFα, IL-8, and IL-1β) and alleviate lung injury in a mouse model of ALI.314 A series of case reports suggest that Abl kinase inhibitors may reduce vascular permeability in specific patients. Overbeek et al. described a patient with pulmonary arterial hypertension and suspected pulmonary veno-occlusive disease who showed improved dyspnea and reduced pulmonary edema within 24 hours of starting imatinib treatment.315 Carnevale et al. reported a patient with bleomycin-induced pneumonia who showed rapid improvements in respiratory status and radiographic findings after imatinib treatment.316 Aman et al. reported that a patient with idiopathic vascular leakage experienced a nearly complete recovery after starting imatinib treatment, including resolution of dyspnea and cough and normalization of vascular leakage-related parameters.317 Therefore, Abl kinase inhibitors with different specificities may help alleviate vascular inflammation and leakage and may become targeted drugs for the treatment of ARDS.
-
(5)
Antibiotics
It has been reported that some antibiotics, including macrolides and tetracyclines, have pleiotropic immunomodulatory effects in addition to antibacterial effects.318 In addition, increasing evidence supports the beneficial effects of these antibiotics on acute inflammatory processes such as pneumonia and ARDS.319 A recent prospective randomized controlled trial demonstrated that the addition of clarithromycin to the standard of care enhances early clinical response and attenuates inflammation in patients with community-acquired pneumonia, and these changes were associated with changes in the immune response.320 Sauer A’s review systematically described preclinical and clinical studies on the immunomodulatory effects of antibiotics in ARDS and the underlying mechanisms of their immunomodulatory effects. That review concluded that this unique antibiotic is a potent modulator of the innate immune response and may improve immune dysregulation in ARDS. This effect depends on the administration time, frequency, dose, and degree of lung injury, but further studies are needed to resolve contradictory results from preclinical and clinical results.321
-
(6)
KGF
Keratinocyte Growth Factor (KGF) enhanced physiological outcomes and markers of alveolar epithelial cell function in various animal models of ARDS/ALI. In a human in vivo short-term model of acute lung injury and ARDS, KGF (palifermin) pretreatment increased bronchoalveolar lavage concentrations of SP-D, a marker of type II cell proliferation, indicating its promotion of epithelial cell survival, supporting its potential benefits in ARDS.322 However, a randomized Phase 2 clinical trial of KGF in patients with ARDS revealed that VFD over 28 days was reduced, but mortality was higher at 28 days in patients treated with KGF, suggesting that it might exacerbate clinical outcomes in ARDS.323 Therefore, KGF might not be used to treat patients with ARDS.
-
(7)
Tie-2 antagonist
The activation of Tie2 by angiopoietin-1 (Ang-1) leads to a reduction in inflammation and endothelial permeability in sepsis.324 Vasculotide (VT) is a polyethylene glycol-clustered Tie2-binding peptide that mimics the actions of Ang-1. VT has been shown to promote pulmonary endothelial stability and reduce lung permeability in various models of pneumococcal pneumonia. Treatment with the angiopoietin-1 mimetic vasculotide has been found to reduce pulmonary vascular leakage and preserve microcirculatory perfusion during cardiopulmonary bypass (CPB) in a rat model.325 Interestingly, combining VT with ampicillin significantly reduced pulmonary hyperpermeability, histological lung damage, and edema formation, without altering the immune response or bacterial burden.326
Targeted immunomodulatory therapies for CARDS
Upon SARS-CoV-2 invasion, the release of cytokines and chemokines may cause a “cytokine storm,” leading to ARDS and multiple organ dysfunction syndrome (MODS).327 Proinflammatory cytokines, monocytes, and neutrophils may be critical players in the development of the cytokine storm in patients with severe CARDS. Therefore, blocking cytokines may be a crucial strategy for CARDS treatment. Some drugs targeting immunopathology, such as interferons, thymosin, and related cytokine inhibitors, have shown therapeutic effects in patients with severe CARDS.
-
(1)
Thymosin
Thymosin is a physiologically active small peptide extracted from the thymus of humans and animals328 that can promote thymocyte differentiation and maturation and increase the number and activity of T cells.329 In patients with COVID-19, thymosin may limit disease progression by stimulating lymphocyte production, particularly in patients with reduced lymphocyte counts. A retrospective cohort study including 334 COVID-19 patients showed that the use of thymosin α1 significantly reduced the 28-day mortality rate and attenuated ALI in critically ill patients.330 However, another multicentre retrospective study including 771 patients did not find a correlation between thymosin α1 use and a decreased mortality rate among critically ill COVID-19 patients.331 This inconsistency may be due to differences in study subjects, COVID-19 severity, sex ratios, and thymosin dosage and timing. Thus, further clinical trials are needed to verify the effectiveness of thymosin α1.
-
(2)
GM-CSF
GM-CSF is believed to be a vital mediator of excessive inflammation in patients with COVID-19.332 Several clinical trials have investigated the use of monoclonal antibodies to treat COVID-19 by modulating the immune response via GM-CSF or its receptor (GM-CSFR) to reduce the inflammatory signaling activated by the GM-CSF axis. Among the investigated antibodies, lenzilumab (a recombinant monoclonal antibody against GM-CSF)333 and mavrilimumab (a monoclonal antibody against GM-CSFRα)334 have been shown in small prospective cohort studies to be associated with reduced mortality and improved systemic hyperinflammation in patients with severe COVID-19. However, a randomized, double-blind, placebo-controlled trial of Gimsilumab, a monoclonal antibody against GM-CSF, in 225 COVID-19 pneumonia patients revealed no significant changes in mortality, non-IMV-free survival, non-IMV duration, time to hospital discharge, or systemic inflammation.335 Therefore, the efficacy of anti-GM-CSF or anti-GM-CSFR therapy for CARDS patients remains unclear. Additionally, the recombinant human granulocyte colony-stimulating factor (rhG-CSF) could reduce the occurrence of CARDS.336 However, rhG-CSF fails to alleviate the severity in patients with COVID-19, and the underlying therapeutic effects and potential mechanisms remain ambiguous in CARDS.
-
(3)
Interleukin
IL-1β and IL-6 play pivotal roles in cytokine storm-related pathways, mediating pathological processes such as fever, pulmonary inflammation, and fibrosis by binding to Toll-like receptors.337 Anakinra, a 17 kDa recombinant, nonglycosylated human IL-1 receptor antagonist.338 Blocking IL-1 can serve as an adjunctive therapeutic approach for the management of patients with severe COVID-19. An RCT including 30 COVID-19 patients demonstrated that the anakinra group had a significantly lower need for IMV than did the control group, with significantly shorter hospital stays and no notable increase in infection rates.339 Another small-sample retrospective study indicated that high-dose (5 mg/kg intravenous infusion) anakinra significantly improved patient survival and improved the clinical condition, inflammatory factors, and mechanical ventilation requirements of CARDS patients outside the ICU compared to low-dose anakinra (100 mg subcutaneous injection twice daily).340 A meta-analysis of 1185 patients with moderate to severe COVID-19 revealed a significant reduction in 28-day mortality with anakinra use.341
Sarilumab is a human monoclonal antibody that directly inhibits the binding of IL-6 to its receptor.342 It inhibits both soluble and membrane-bound forms of the IL-6 receptor, potentially suppressing the activation of proinflammatory signals in pulmonary epithelial cells and immune cells.343 An open-label, randomized, controlled phase II clinical trial demonstrated the safety and potential efficacy of early use of 400 mg sarilumab in patients with COVID-19 pneumonia and features of systemic inflammation.344 In a multicentre phase III clinical trial, 416 COVID-19 pneumonia patients were randomized to receive different doses of sarilumab (200 mg or 400 mg). Although sarilumab did not demonstrate differential efficacy overall, there was a survival difference between the sarilumab 400 mg group and the placebo group on day 29 in critically ill patients (88% vs. 79%), suggesting that appropriate IL-6-targeted immunomodulatory treatment in critically ill COVID-19 patients may improve patient prognosis.345
-
(4)
Complement system
COVID-19 is characterized by severe pulmonary inflammation and activation of coagulation, leading to adverse disease outcomes associated with the activation of the complement system, particularly the C5A-C5AR axis.68 Blocking the C5A-C5AR1 axis can limit the infiltration of myeloid cells into damaged organs, preventing excessive pulmonary inflammation and endothelial cell dysfunction.346 A multicentre, double-blind, randomized phase 3 trial, which included 368 patients with CARDS, showed a significant reduction in the all-cause mortality rate at 28 days after anti-C5a antibody (vilobelimab) therapy.347 Ruxolitinib, an inhibitor of Janus kinases 1 and 2, which play a crucial role in inflammation, has shown promise in treating COVID-19 patients with severe systemic inflammation.348,349 In a nonrandomized prospective phase II multicentre study, ruxolitinib was used for targeted inhibition of Janus kinase-mediated cytokine signaling and was found to improve the prognosis of patients with COVID-19-induced ARDS when given immediately after disease deterioration.350 In summary, vilobelimab and ruxolitinib have shown potential as treatments for treating CARDS, but more clinical trials and animal experiments are needed to develop effective complement inhibitors for COVID-19 treatment.
-
(5)
NETs
The ability of neutrophils to form NETs may contribute to organ damage and mortality in COVID-19 patients, as supported by autopsy findings; this may be related to the oxidative damage caused by the release of extracellular DNA.351,352 Dornase Alfa is a recombinant human deoxyribonuclease I that degrades extracellular DNA and has mucolytic properties.351 A pilot, nonrandomized, case‒controlled clinical trial revealed that the Dornase Alfa group exhibited a significant improvement in the PaO2/FiO2 ratio on day two and a substantial improvement in static lung compliance on days 3-5 compared to the control group. Furthermore, Dornase Alfa treatment improved oxygenation in the BALF and reduced DNA release via the formation of myeloperoxidase (MPO) complexes.353 This finding suggested that Dornase Alfa may have therapeutic potential in mitigating the severity of CARDS by reducing NET-mediated lung injury.
-
(6)
TNFSF14
Lymphocyte-inducing protein (LIGHT or TNFSF14) is a cytokine that competes with glycoprotein D to prevent viruses from entering T cells and plays a critical role in creating a network of cytokines and receptors that regulate the host defence system and the communication systems that control immune responses.354 The efficacy and safety of CERC-002, a human neutralizing antibody against TNFSF14, for treating COVID-19-induced ARDS patients were assessed. Among 83 patients, those who received CERC-002 treatment had a significantly higher rate of survival free of respiratory failure (83.9%) than did those who received a placebo (64.5%) at day 28, as well as lower 28-day and 60-day mortality rates.355 These findings suggest that CERC-002 may be a promising treatment option for patients with CARDS.
-
(7)
NLRP3
One of the essential functions of the innate immune system is to recognize pathogens by triggering the NLRP3 inflammasome.356 DFV890 is a novel, potent, and selective oral NLRP3 inhibitor.357 Madurka et al. conducted a multicentre study including 143 patients with COVID-19 pneumonia who were randomized to the DFV890 + standard-of-care (SoC) group or the SoC-alone group. The results showed that the DFV890 group achieved better outcomes than the SoC group, with clinical improvement ≥1 grade, earlier viral clearance, earlier survival without mechanical ventilation, and lower mortality.358 However, further studies are needed to confirm its safety and efficacy in larger patient populations and to identify the optimal dosing and treatment regimens.
Targeted immunotherapy has emerged as a promising approach for treating ARDS; however, several challenges must be overcome to maximize its therapeutic potential. The heterogeneity of ARDS presents a significant challenge in identifying specific therapeutic targets that can benefit all patients uniformly. Moreover, the timing of immunotherapy is crucial, as initiating treatment either too early or too late may have detrimental effects on the clinical outcome. Additionally, the potential for off-target effects, including immune suppression or undesired effects on nonpathogenic cells, may limit the safety of immunotherapy. Cost is another critical factor that may limit the availability and accessibility of targeted immunotherapy. In this regard, personalized medicine strategies may represent a future direction for targeted immunotherapy. These strategies aim to develop patient-specific treatments that consider individual factors such as genetics, comorbidities, and disease severity. The use of biomarkers and advanced imaging techniques may also aid in identifying appropriate targets and monitoring treatment response. Furthermore, combination therapies that target multiple pathways or utilize different modalities, such as gene therapy or cell-based therapies, may provide a more comprehensive and effective approach to improve outcomes in ARDS patients.
Other targeted therapies
In addition to targeted immunomodulatory therapies, there are many other potential targeted drugs for ARDS treatment. NLRP3, NF-κB, STAT, Nrf2, TNFR1, and SIRT1 are the most common targets of inhibition, and multiple miRNAs, which are key regulatory factors in signaling pathways, have also been shown to be beneficial in animal models of ARDS. Notably, natural products and traditional Chinese medicines have application prospects in ARDS treatment. However, most of these drugs are still in the preclinical stage, and there is a lack of information on their safety, ideal concentrations, administration methods, etc., in ARDS patients. More details are shown in Table 5.359,360,361,362,363,364,365,366,367,368,369,370,371,372,373,374,375,376,377,378,379,380,381,382,383,384,385,386,387,388,389,390,391,392,393,394,395,396,397,398,399,400,401,402,403,404,405,406,407,408,409,410,411,412,413,414,415,416,417,418,419,420,421,422,423,424,425,426,427,428,429,430,431,432,433,434,435,436,437,438,439,440,441,442,443,444,445
Personalized therapy for ARDS
Significant differences in genetic, biological, and environmental factors among ARDS patients, including differences in etiological profiles, immune profiles, and inflammation profiles, can lead to differences in responsiveness to treatment.446 Thus, evidence suggests that personalized medicine approaches should be used for patients with different ARDS subphenotypes. Before we achieve personalized medicine strategies for ARDS, we must determine the exact phenotypes of ARDS patients. As we discussed above, the selected treatments must be targeted and effective for the patient’s specific ARDS phenotype.447
Personalized medicine
To date, personalized medicine for ARDS patients has mainly depended on the microenvironment in pulmonary tissue and the whole body, clinical features, ventilator parameters, etc. However, ARDS clinical phenotypes provide a new therapeutic direction for personalized medicine. Several researchers have demonstrated that therapeutic effects can vary according to the subphenotype of ARDS, as discussed above. For example, patients with hyperinflammatory ARDS may benefit from treatments such as simvastatin, corticosteroids, and MSCs, while other patients may experience no benefit or even detrimental effects.147,448,449 Therefore, the investigation of personalized medicine approaches selected according to the clinical phenotypes of ARDS would be valuable in future studies.
Personalized mechanical ventilation
Personalized mechanical ventilation has recently emerged as a management approach for ARDS patients. In Jean’s study, the authors compared mortality and other clinical outcomes among several subgroups of ARDS patients, which were grouped according to lung morphology.450 The results showed that correct adjustment of the ventilator strategy according to lung morphology decreased mortality compared to that observed for unclassified patients and patients receiving a misaligned ventilator strategy, suggesting that personalized mechanical ventilation selected according to an accurate classification of lung morphology may be a potential therapeutic direction for ARDS patients. Furthermore, ventilator parameter-focused strategies might be beneficial for treating ARDS. Tidal volume was previously thought to be the primary factor involved in developing ventilator strategies. However, a recent study revealed that driving pressure, which is determined by tidal volume and lung elastance, is more important in the development of ventilator strategies,451 which indicates that driving pressure-targeted lung-protective ventilation strategies are useful for treating ARDS.
Organ function-dependent personalized strategy
Organ function is also important in the development of personalized management strategies for ARDS patients. It has been reported that PEEP, especially esophageal pressure-guided PEEP (Pes-guided PEEP), is associated with patient mortality in ARDS patients with variations in organ function.452 Pes-guided PEEP is associated with better clinical outcomes in patients with higher APACHE-II scores, which indicate severe multiorgan dysfunction in ARDS patients. In contrast, Pes-guided PEEP is associated with lower mortality among patients with better organ function. All the above results suggest that organ function-dependent PEEP strategies might be an alternative approach for personalized mechanical ventilation in ARDS patients. Organ function can also be instructive for personalized fluid strategies in ARDS patients. On the basis of their clinical symptoms and organ function parameters, ARDS patients can be divided into several phenotypes, including phenotype 2, which is characterized by more inflammation and less organ dysfunction, and phenotype 3, which is characterized by severe renal dysfunction and acidosis.125 Interestingly, the fluid-conservation strategy has beneficial effects on mortality in patients with phenotype 3 disease but detrimental effects on mortality in patients with phenotype 3 disease, indicating the potential of personalized fluid management strategies for patients with ARDS.
Other alternative therapy
Other treatments for ARDS, such as inhaled carbon monoxide, vitamins and other drugs have also been investigated. Recently, vitamins have emerged as agents for managing ARDS, as vitamin D appears to attenuate lung damage caused by CARDSs and ALI, according to preclinical studies.453 However, continuous infusion of vitamin C did not improve multiorgan function or attenuate serum markers of inflammation and vascular injury in patients with sepsis-related ARDS.454 This difference may have several causes. First, differences across species may have led to different results. Second, different phenotypes of ARDS have unique pathogenic mechanisms and clinical features, resulting in different responses to vitamin therapy. Finally, vitamins may display varying therapeutic effects even in a single disease model. Thus, additional studies are needed in the future. Additionally, there are several treatments that have been investigated less thoroughly in preclinical studies; these are listed in Table 6.455,456,457,458,459,460,461,462
Interestingly, several novel drug platforms have been reported in recent years. Lung-targeted liposomes are an organ-specific and effective method for drug delivery. The liposomal lipid composition mimics the lung surfactant composition and includes steroids, MPS, and N-acetyl cysteine (NAC), which exert significant therapeutic effects by attenuating pulmonary inflammation.463 At the same time, encapsulated dexamethasone decreases oxidative stress-induced lung injury by inhibiting protein accumulation, neutrophil accumulation, and lipid peroxidation in ARDS.464,465 Furthermore, liposome-encapsulated trans-crocetin (TC) is longer lasting than free TC, with a longer duration of oxygenation in vitro and an extended half-life in vivo in the context of CARDS.466 In addition, larger nanoparticles have greater cellular uptake. These agents are highly adaptable in cells due to the size-dependent anti-inflammatory properties of nanoparticles, resulting in therapeutic effects via activation of anti-inflammatory pathways in ARDS.467 In conclusion, these new drug delivery methods are more effective and safer than traditional drugs, providing a new therapeutic direction for the treatment of ARDS.
Response to treatment
Different responses to mechanical ventilation
The response of subphenotypes to mechanical ventilation was tested in several clinical trials. Patients randomized to the high- vs. low-PEEP strategy had mortality rates of 24% and 16% for the hypoinflammatory subphenotype, respectively, compared with 42% and 51%, respectively, for the hyperinflammatory subphenotype.118 Moreover, focal ARDS and nonfocal ARDS patients respond differently to mechanical ventilation. High PEEP and recruitment maneuvers decrease mortality for patients with nonfocal ARDS, as do high tidal volume, low PEEP, and prone positioning for those with focal ARDS. However, mortality increases substantially when mechanical ventilation parameters are not aligned with the subphenotype.450 These results are consistent with Constantin JM’s results, which emphasized the need for different recruitment maneuvers for patients with focal ARDS and nonfocal ARDS.468 Moreover, CT-based lung imaging patterns reveal some similarities between the hyperinflammatory subphenotype and nonfocal ARDS, including the mortality rate, incidence of sepsis, and expression of specific lung injury biomarkers, especially plasma sRAGE, which is associated with nonfocal ARDS.469 These results suggest that individualized ventilation strategies for patients with ARDS subphenotypes effectively improve patient prognosis. Two ARDS phenotypes were confirmed based on respiratory mechanics, gas exchange, and computed tomography-derived gas and tissue volumes. Compared to recruitable subphenotype, non-recruitable subphenotype is characterized by lower respiratory system elastance, dead space, and total lung tissue, a higher arterial pressure of oxygen/inspiratory fraction of oxygen (PaO2/FiO2) ratio, a more physiological pH and less inhomogeneous lung. In particular, the non-recruitable subphenotype had a lower success rate of recruitment maneuvers and a higher mortality rate than did recruitable subphenotype.470 Additionally, gravity influences the regional distribution of opening and closing pressure, hysteresis and atelectrauma, with higher values in the dorsal lung.471 It is likely that the dependent lung is prone to worse physiological conditions. Assessing the lung’s regional behavior with inspiratory and expiratory pressure–volume (PV) curves can help identify ARDS phenotypes and guide personalized mechanical ventilation settings.
Different responses to fluid therapy
Famous KR et al.’s analysis supported the existence of two ARDS subphenotypes, with higher inflammatory biomarker levels and hypotension characterizing subphenotype 2. In addition, they confirmed that these two ARDS subphenotypes responded differently to a randomized fluid management strategy. Patients with hypoinflammatory subphenotype had 90-day mortality rates of 26% in the fluid-conservative group and 18% in the fluid-liberal group, while these rates were 40% and 50% in these two groups, respectively, in patients with hyperinflammatory subphenotype.472
Different responses to pharmacotherapy
In addition to responding differently to mechanical ventilation and fluid therapy, ARDS subphenotypes also respond differently to pharmacotherapy. Survival was significantly improved in patients treated with simvastatin compared with patients treated with placebo among patients with a hyperinflammatory subphenotype.147 However, no treatment effect of rosuvastatin was observed among patients with the hyperinflammatory subphenotype.473
Conclusion
In recent years, the incidence of ARDS has been increasing gradually, compounded by the emergence of new causes of viral pneumonia, such as SARS-CoV-2, which make the occurrence and progression of ARDS more complicated. Notably, some novel factors, such as blood product transfusion, e-cigarettes, and ozone, have become risk factors for ARDS, which highlights the need to pay attention to the influence of these factors on ARDS. Over time, substantial progress has been made in understanding the epidemiology and biology of this heterogeneous syndrome. We now know that ARDS is highly heterogeneous in terms of clinical features, causes of lung injury, effective biomarkers, and clinical and biological variables, we also summarized the application of various treatments to treat ARDS in preclinical and clinical practice, shown in Fig. 6. However, personalized medicine approaches for patients with different phenotypes might be a goal of future treatment.
Main therapies of ARDS. With the deepening of research, the treatment methods of ARDS have developed many new factions based on traditional treatment methods. Clinical trials have confirmed the effectiveness of cell therapy in the treatment of ARDS, especially stem cells and cell components. In addition, targeted therapy with targeted immunotherapy as its core also shows good therapeutic effects. However, due to the significant heterogeneity of ARDS, emerging evidence has revealed that personalized medicine should be administered in different ARDS subphenotypes. *Targeted therapy: Targeted therapy for ARDS focuses on interrupting or modifying specific molecular, genetic, or cellular mechanisms underlying lung injury and inflammation, thus reducing symptoms and improving outcomes. Personalized therapy: Personalized treatment of ARDS refers to developing personalized treatment methods based on the individual characteristics of the patient, such as genetic makeup, medical history, and unique disease manifestations, to optimize treatment efficacy and minimize side effects. HFNO high-flow nasal cannula oxygen, NIV noninvasive ventilation, PEEP positive end-expiratory pressure, ARDS Acute respiratory distress syndrome, CARDS COVID-19 related acute respiratory distress syndrome, TNF-α tumor necrosis factor alpha, GM-CSF granulocyte-macrophage colony-stimulating factor, KGF keratinocyte Growth Factor, NET neutrophil extracellular trap, TNFSF14 lymphocyte-inducing protein, NLRP3 NOD-, LRR- and pyrin domain-containing 3, NF-κB nuclear factor kappa B, STAT signal transducer and activator of transcription, Nrf2: nuclear factor-E2-related factor 2
Future directions for ARDS treatment include identifying which treatment approaches apply broadly to any patient meeting the diagnostic criteria and which approaches should be personalized to specific aspects of physiology and biology that could be used to identify a more treatment-responsive subgroup. Traits associated with treatment response can be identified by biomarkers, which align with underlying pathophysiological mechanisms and can be targeted by specific therapeutics or interventions. Alternative biomarkers might also include imaging, physiology and clinical data that reflect an underlying pathophysiological process that could be responsive to therapy. The evidence base for optimal supportive care and interventions in ARDS patients continues to evolve to address areas of uncertainty. As we enter an era of precision medicine for critical illnesses, the future of ARDS management will move towards identifying biological phenotypes and traits associated with treatment response and delivering personalized therapeutic interventions.
To overcome the challenges associated with ARDS treatment, a multidisciplinary approach is required to combine the expertise of clinicians, scientists, and industry partners. This collaboration will facilitate the development and implementation of personalized medicine strategies. Ultimately, the successful implementation of personalized medicine strategies for ARDS treatment will depend on rigorous evaluations of safety and efficacy in large clinical trials, the development of innovative manufacturing and delivery technologies, and the establishment of a sustainable and equitable healthcare system that ensures access to this cutting-edge therapy for all patients in need.
References
Jenkins, M. T., Jones, R. F., Wilson, B. & Moyer, C. A. Congestive atelectasis; a complication of the intravenous infusion of fluids. Trans. Meet. Am. Surg. Assoc. Am. Surg. Assoc. 68, 7–27 (1950).
Ashbaugh, D. G., Bigelow, D. B., Petty, T. L. & Levine, B. E. Acute respiratory distress in adults. Lancet 2, 319–323 (1967).
Petty, T. L. & Ashbaugh, D. G. The adult respiratory distress syndrome. Clinical features, factors influencing prognosis and principles of management. Chest 60, 233–239 (1971).
Murray, J. F., Matthay, M. A., Luce, J. M. & Flick, M. R. An expanded definition of the adult respiratory distress syndrome. Am. Rev. Respir. Dis. 138, 720–723 (1988).
Baden, M. et al. A controlled trial of hydrocortisone therapy in infants with respiratory distress syndrome. Pediatrics 50, 526–534 (1972).
Liggins, G. C. & Howie, R. N. A controlled trial of antepartum glucocorticoid treatment for prevention of the respiratory distress syndrome in premature infants. Pediatrics 50, 515–525 (1972).
Bernard, G. R. et al. Report of the American-European consensus conference on ARDS: definitions, mechanisms, relevant outcomes and clinical trial coordination. The Consensus Committee. Intensive Care Med 20, 225–232 (1994).
Force, A. D. T. et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA 307, 2526–2533 (2012).
Riviello, E. D. et al. Hospital incidence and outcomes of the acute respiratory distress syndrome using the Kigali Modification of the Berlin definition. Am. J. Respir. Crit. Care Med 193, 52–59 (2016).
Matthay, M. A. et al. Phenotypes and personalized medicine in the acute respiratory distress syndrome. Intensive Care Med 46, 2136–2152 (2020).
Fujishima, S. Guideline-based management of acute respiratory failure and acute respiratory distress syndrome. J. Intensive Care 11, 10 (2023).
Wick, K. D., Matthay, M. A. & Ware, L. B. Pulse oximetry for the diagnosis and management of acute respiratory distress syndrome. Lancet Respir. Med 10, 1086–1098 (2022).
Peng, J. M. et al. Does training improve diagnostic accuracy and inter-rater agreement in applying the Berlin radiographic definition of acute respiratory distress syndrome? A multicenter prospective study. Crit. Care 21, 12 (2017).
Zimatore, C. et al. Accuracy of the Radiographic assessment of lung Edema score for the diagnosis of ARDS. Front Physiol. 12, 672823 (2021).
Farzaneh, N. et al. Collaborative strategies for deploying artificial intelligence to complement physician diagnoses of acute respiratory distress syndrome. NPJ Digit Med. 6, 62 (2023).
Arora, M. et al. Uncertainty-aware convolutional neural network for identifying bilateral opacities on Chest X-rays: A tool to aid diagnosis of acute respiratory distress syndrome. Bioengineering 10, 946 (2023).
Plantinga, C. et al. Use of lung ultrasound in the new definitions of acute respiratory distress syndrome increases the occurrence rate of acute respiratory distress syndrome. Crit. Care Med 52, e100–e104 (2024).
Papazian, L. et al. National incidence rate and related mortality for acute respiratory distress syndrome in France. Anaesth. Crit. Care Pain. Med 40, 100795 (2021).
Li, G. et al. Eight-year trend of acute respiratory distress syndrome: a population-based study in Olmsted County, Minnesota. Am. J. Respir. Crit. Care Med. 183, 59–66 (2011).
Linko, R. et al. Acute respiratory failure in intensive care units. FINNALI: a prospective cohort study. Intensive Care Med 35, 1352–1361 (2009).
Fan, E., Brodie, D. & Slutsky, A. S. Acute respiratory distress syndrome: advances in diagnosis and treatment. JAMA 319, 698–710 (2018).
McNicholas, B. A. et al. Demographics, management and outcome of females and males with acute respiratory distress syndrome in the LUNG SAFE prospective cohort study. Eur. Respir. J. 54, 1900609 (2019).
Bellani, G. et al. EpidemiologY, Patterns Of Care, And Mortality For Patients With Acute Respiratory Distress Syndrome In Intensive Care Units In 50 Countries. JAMA 315, 788–800 (2016).
Zhang, X. et al. Mesenchymal stromal cells alleviate acute respiratory distress syndrome through the cholinergic anti-inflammatory pathway. Signal Transduct. Target Ther. 7, 307 (2022).
Villar, J., Blanco, J. & Kacmarek, R. M. Current incidence and outcome of the acute respiratory distress syndrome. Curr. Opin. Crit. Care 22, 1–6 (2016).
Liu, L. et al. Practice of diagnosis and management of acute respiratory distress syndrome in mainland China: a cross-sectional study. J. Thorac. Dis. 10, 5394–5404 (2018).
Huang, X. et al. Incidence and outcomes of acute respiratory distress syndrome in intensive care units of mainland China: a multicentre prospective longitudinal study. Crit. Care 24, 515 (2020).
Wu, C. et al. Risk factors associated with acute respiratory distress syndrome and death in patients with Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med 180, 934–943 (2020).
Yang, X. et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 8, 475–481 (2020).
Qin, C. et al. Clinical characteristics and outcomes of COVID-19 patients with a history of Stroke in Wuhan, China. Stroke 51, 2219–2223 (2020).
Pisani, L. et al. Geoeconomic variations in epidemiology, ventilation management, and outcomes in invasively ventilated intensive care unit patients without acute respiratory distress syndrome: a pooled analysis of four observational studies. Lancet Glob. Health 10, e227–e235 (2022).
Attaway, A. H. et al. Severe COVID-19 pneumonia: pathogenesis and clinical management. BMJ 372, n436 (2021).
Aranda, J. et al. Long-term impact of COVID-19 associated acute respiratory distress syndrome. J. Infect. 83, 581–588 (2021).
Calfee, C. S. et al. Cigarette smoke exposure and the acute respiratory distress syndrome. Crit. Care Med 43, 1790–1797 (2015).
Moazed, F. et al. Cigarette smoke exposure and acute respiratory distress syndrome in sepsis: epidemiology, clinical features, and biologic markers. Am. J. Respir. Crit. Care Med 205, 927–935 (2022).
Simou, E., Leonardi-Bee, J. & Britton, J. The effect of alcohol consumption on the risk of ARDS: A systematic review and meta-analysis. Chest 154, 58–68 (2018).
Toy, P. et al. Transfusion-related acute lung injury: 36 years of progress (1985–2021). Ann. Am. Thorac. Soc. 19, 705–712 (2022).
Krishnasamy, V. P. et al. Update: Characteristics of a nationwide outbreak of E-cigarette, or Vaping, product use-associated lung injury - United States, August 2019-January 2020. MMWR Morb. Mortal. Wkly Rep. 69, 90–94 (2020).
Layden, J. E. et al. Pulmonary illness related to E-Cigarette Use in Illinois and Wisconsin - Final Report. N. Engl. J. Med. 382, 903–916 (2020).
Matsumoto, S. et al. Dose-dependent pulmonary toxicity of aerosolized Vitamin E Acetate. Am. J. Respir. Cell Mol. Biol. 63, 748–757 (2020).
Reilly, J. P. et al. Low to moderate air pollutant exposure and acute respiratory distress syndrome after severe trauma. Am. J. Respir. Crit. Care Med. 199, 62–70 (2019).
Ware, L. B. et al. Long-term Ozone exposure increases the risk of developing the acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 193, 1143–1150 (2016).
Bos, L. D. J. & Ware, L. B. Acute respiratory distress syndrome: causes, pathophysiology, and phenotypes. Lancet 400, 1145–1156 (2022).
Shi, X. et al. Magnesium Hydride Ameliorates Endotoxin-induced acute respiratory distress syndrome by inhibiting inflammation, oxidative stress, and cell apoptosis. Oxid. Med Cell Longev. 2022, 5918954 (2022).
Kosutova, P. et al. Effects of PDE3 Inhibitor Olprinone on the Respiratory Parameters, Inflammation, and Apoptosis in an Experimental Model of Acute Respiratory Distress Syndrome. Int. J. Mol. Sci. 21, 3382 (2020).
Birnhuber, A. et al. Between inflammation and thrombosis: endothelial cells in COVID-19. Eur. Respir. J. 58, 2100377 (2021).
Jiang, J. et al. Targeting NOX4 alleviates sepsis-induced acute lung injury via attenuation of redox-sensitive activation of CaMKII/ERK1/2/MLCK and endothelial cell barrier dysfunction. Redox Biol. 36, 101638 (2020).
Leisman, D. E. et al. Alveolar, endothelial, and organ injury marker dynamics in severe COVID-19. Am. J. Respir. Crit. Care Med. 205, 507–519 (2022).
Benatti, M. N., Fabro, A. T. & Miranda, C. H. Endothelial glycocalyx shedding in the acute respiratory distress syndrome after flu syndrome. J. Intensive Care 8, 72 (2020).
Gilan, O. et al. Selective targeting of BD1 and BD2 of the BET proteins in cancer and immunoinflammation. Science 368, 387–394 (2020).
Liu, Y., Zhang, D., Cheng, Y. & Li, Z. Elevated serum immunoinflammation-related protein complexes are associated with psychosis. Psychiatry Res. 230, 96–101 (2015).
Torres Acosta, M. A. & Singer, B. D. Pathogenesis of COVID-19-induced ARDS: implications for an ageing population. Eur. Respir. J. 56, 2002049 (2020).
Luyt, C. E. et al. Pulmonary infections complicating ARDS. Intensive Care Med 46, 2168–2183 (2020).
Li, D., Pan, L., Zhang, X. & Jiang, Z. Lower oligomeric form of surfactant protein D in murine acute lung injury induces M1 subtype macrophages through Calreticulin/p38 MAPK signaling pathway. Front Immunol. 12, 687506 (2021).
Hoepel, W. et al. High titers and low fucosylation of early human anti-SARS-CoV-2 IgG promote inflammation by alveolar macrophages. Sci. Transl. Med. 13, eabf8654 (2021).
Shen, Q. et al. Soluble SIRP-Alpha Promotes Murine Acute Lung Injury Through Suppressing Macrophage Phagocytosis. Front Immunol. 13, 865579 (2022).
Boada-Romero, E., Martinez, J., Heckmann, B. L. & Green, D. R. The clearance of dead cells by efferocytosis. Nat. Rev. Mol. Cell Biol. 21, 398–414 (2020).
Yamashita, M. et al. VEGF-C/VEGFR-3 signalling in macrophages ameliorates acute lung injury. Eur. Respir. J. 59, 2100880 (2022).
Zingaropoli, M. A. et al. Increased sCD163 and sCD14 Plasmatic Levels and Depletion of Peripheral Blood Pro-Inflammatory Monocytes, Myeloid and Plasmacytoid Dendritic Cells in Patients With Severe COVID-19 Pneumonia. Front Immunol. 12, 627548 (2021).
Gregoire, M. et al. Impaired efferocytosis and neutrophil extracellular trap clearance by macrophages in ARDS. Eur. Respir. J. 52, 1702590 (2018).
Ng, H. et al. Circulating Markers of Neutrophil Extracellular Traps Are of Prognostic Value in Patients With COVID-19. Arterioscler Thromb. Vasc. Biol. 41, 988–994 (2021).
Puuvuori, E. et al. PET Imaging of Neutrophil Elastase with (11)C-GW457427 in Acute Respiratory Distress Syndrome in Pigs. J. Nucl. Med 64, 423–429 (2023).
Zhu, C. et al. Homeostatic and early-recruited CD101(-) eosinophils suppress endotoxin-induced acute lung injury. Eur. Respir. J. 56, 1902354 (2020).
Grant, R. A. et al. Circuits between infected macrophages and T cells in SARS-CoV-2 pneumonia. Nature 590, 635–641 (2021).
Cuvelier, P. et al. Protective reactive thymus hyperplasia in COVID-19 acute respiratory distress syndrome. Crit. Care 25, 4 (2021).
Jouan, Y. et al. Phenotypical and functional alteration of unconventional T cells in severe COVID-19 patients. J. Exp. Med. 217, e20200872 (2020).
Unterman, A. et al. Single-cell multi-omics reveals dyssynchrony of the innate and adaptive immune system in progressive COVID-19. Nat. Commun. 13, 440 (2022).
Carvelli, J. et al. Association of COVID-19 inflammation with activation of the C5a-C5aR1 axis. Nature 588, 146–150 (2020).
Georg, P. et al. Complement activation induces excessive T cell cytotoxicity in severe COVID-19. Cell 185, 493–512 e425 (2022).
Zhang, W. et al. Extracellular CIRP-impaired Rab26 Restrains EPOR-mediated macrophage polarization in acute lung injury. Front. Immunol. 12, 768435 (2021).
Quijada, H. et al. Endothelial eNAMPT amplifies pre-clinical acute lung injury: efficacy of an eNAMPT-neutralising monoclonal antibody. Eur. Respir. J. 57, 2002536 (2021).
Middleton, E. A. et al. Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood 136, 1169–1179 (2020).
Skendros, P. et al. Complement and tissue factor-enriched neutrophil extracellular traps are key drivers in COVID-19 immunothrombosis. J. Clin. Invest. 130, 6151–6157 (2020).
O’Donnell, J. S., Peyvandi, F. & Martin-Loeches, I. Pulmonary immuno-thrombosis in COVID-19 ARDS pathogenesis. Intensive Care Med. 47, 899–902 (2021).
Rizzo, A. N. & Schmidt, E. P. ABO blood type: a window into the genetics of acute respiratory distress syndrome susceptibility. J. Clin. Invest. 131, e144075 (2021).
Reilly, J. P. et al. The ABO histo-blood group, endothelial activation, and acute respiratory distress syndrome risk in critical illness. J. Clin. Invest. 131, e139700 (2021).
Sung, P. S. et al. CLEC5A and TLR2 are critical in SARS-CoV-2-induced NET formation and lung inflammation. J. Biomed. Sci. 29, 52 (2022).
Adrover, J. M. et al. Programmed ‘disarming’ of the neutrophil proteome reduces the magnitude of inflammation. Nat. Immunol. 21, 135–144 (2020).
Michalick, L. et al. Plasma mediators in patients with severe COVID-19 cause lung endothelial barrier failure. Eur. Respir. J. 57, 2002384 (2021).
Chen, Y. et al. METTL3-Mediated N6-Methyladenosine mModification of Trim59 mRNA protects against sepsis-induced acute respiratory distress syndrome. Front Immunol. 13, 897487 (2022).
Artham, S. et al. Endothelial stromelysin1 regulation by the forkhead box-O transcription factors is crucial in the exudative phase of acute lung injury. Pharm. Res. 141, 249–263 (2019).
Xiong, S. et al. IL-1beta suppression of VE-cadherin transcription underlies sepsis-induced inflammatory lung injury. J. Clin. Invest. 130, 3684–3698 (2020).
Pugin, J., Verghese, G., Widmer, M. C. & Matthay, M. A. The alveolar space is the site of intense inflammatory and profibrotic reactions in the early phase of acute respiratory distress syndrome. Crit. Care Med. 27, 304–312 (1999).
Ware, L. B. & Matthay, M. A. The acute respiratory distress syndrome. N. Engl. J. Med. 342, 1334–1349 (2000).
Bastarache, J. A. et al. Low levels of tissue factor lead to alveolar haemorrhage, potentiating murine acute lung injury and oxidative stress. Thorax 67, 1032–1039 (2012).
Janz, D. R. & Ware, L. B. The role of red blood cells and cell-free hemoglobin in the pathogenesis of ARDS. J. Intensive Care 3, 20 (2015).
Mumby, S. et al. Methemoglobin-induced signaling and chemokine responses in human alveolar epithelial cells. Am. J. Physiol. Lung Cell Mol. Physiol. 306, L88–L100 (2014).
Conger, A. K. et al. Hemoglobin increases leukocyte adhesion and initiates lung microvascular endothelial activation via Toll-like receptor 4 signaling. Am. J. Physiol. Cell Physiol. 324, C665–C673 (2023).
Schaaf, K. R. et al. Cell-free hemoglobin triggers macrophage cytokine production via TLR4 and MyD88. Am. J. Physiol. Lung Cell Mol. Physiol. 326, L29–L38 (2024).
Janz, D. R. et al. Association between cell-free hemoglobin, acetaminophen, and mortality in patients with sepsis: an observational study. Crit. Care Med. 41, 784–790 (2013).
Bunger, V. et al. Potential of cell-free hemoglobin and haptoglobin as prognostic markers in patients with ARDS and treatment with veno-venous ECMO. J. Intensive Care 11, 15 (2023).
Ware, L. B. et al. Acetaminophen for prevention and treatment of organ dysfunction in critically ill patients with sepsis: The ASTER randomized clinical trial. JAMA 332, 390–400 (2024).
Ware, L. B. & Matthay, M. A. Alveolar fluid clearance is impaired in the majority of patients with acute lung injury and the acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 163, 1376–1383 (2001).
Matthay, M. A. Resolution of pulmonary edema. Thirty years of progress. Am. J. Respir. Crit. Care Med. 189, 1301–1308 (2014).
Vivona, M. L. et al. Hypoxia reduces alveolar epithelial sodium and fluid transport in rats: reversal by beta-adrenergic agonist treatment. Am. J. Respir. Cell Mol. Biol. 25, 554–561 (2001).
Frank, J. et al. Transforming growth factor-beta1 decreases expression of the epithelial sodium channel alphaENaC and alveolar epithelial vectorial sodium and fluid transport via an ERK1/2-dependent mechanism. J. Biol. Chem. 278, 43939–43950 (2003).
Lee, J. W. et al. Acute lung injury edema fluid decreases net fluid transport across human alveolar epithelial type II cells. J. Biol. Chem. 282, 24109–24119 (2007).
Pittet, J. F. et al. TGF-beta is a critical mediator of acute lung injury. J. Clin. Invest 107, 1537–1544 (2001).
Peters, D. M. et al. TGF-beta directs trafficking of the epithelial sodium channel ENaC which has implications for ion and fluid transport in acute lung injury. Proc. Natl Acad. Sci. USA 111, E374–E383 (2014).
Roux, J. et al. IL-8 inhibits cAMP-stimulated alveolar epithelial fluid transport via a GRK2/PI3K-dependent mechanism. FASEB J. 27, 1095–1106 (2013).
Islam, M. N. et al. Mitochondrial transfer from bone-marrow-derived stromal cells to pulmonary alveoli protects against acute lung injury. Nat. Med 18, 759–765 (2012).
Hickman-Davis, J. M. et al. Reactive species mediate inhibition of alveolar type II sodium transport during mycoplasma infection. Am. J. Respir. Crit. Care Med 173, 334–344 (2006).
Chen, X. J. et al. Influenza virus inhibits ENaC and lung fluid clearance. Am. J. Physiol. Lung Cell Mol. Physiol. 287, L366–373 (2004).
Song, W. et al. Respiratory syncytial virus inhibits lung epithelial Na+ channels by up-regulating inducible nitric-oxide synthase. J. Biol. Chem. 284, 7294–7306 (2009).
Harris, A. J. et al. IL4Ralpha signaling abrogates Hypoxic neutrophil survival and limits acute lung injury responses in vivo. Am. J. Respir. Crit. Care Med 200, 235–246 (2019).
Blazquez-Prieto, J. et al. Activation of p21 limits acute lung injury and induces early senescence after acid aspiration and mechanical ventilation. Transl. Res. 233, 104–116 (2021).
Hsu, C. G. et al. The lipid peroxidation product 4-hydroxynonenal inhibits NLRP3 inflammasome activation and macrophage pyroptosis. Cell Death Differ. 29, 1790–1803 (2022).
Jiao, Y. et al. Exosomal miR-30d-5p of neutrophils induces M1 macrophage polarization and primes macrophage pyroptosis in sepsis-related acute lung injury. Crit. Care 25, 356 (2021).
Qin, X. et al. Caspase-1-mediated extracellular vesicles derived from pyroptotic alveolar macrophages promote inflammation in acute lung injury. Int J. Biol. Sci. 18, 1521–1538 (2022).
Xia, B. et al. SARS-CoV-2 envelope protein causes acute respiratory distress syndrome (ARDS)-like pathological damages and constitutes an antiviral target. Cell Res. 31, 847–860 (2021).
Zhang, H. et al. Neutrophil extracellular traps mediate m(6)A modification and regulates sepsis-associated acute lung injury by activating ferroptosis in alveolar epithelial cells. Int J. Biol. Sci. 18, 3337–3357 (2022).
D’Agnillo, F. et al. Lung epithelial and endothelial damage, loss of tissue repair, inhibition of fibrinolysis, and cellular senescence in fatal COVID-19. Sci. Transl. Med. 13, eabj7790 (2021).
Ruhl, L. et al. Endothelial dysfunction contributes to severe COVID-19 in combination with dysregulated lymphocyte responses and cytokine networks. Signal Transduct. Target Ther. 6, 418 (2021).
Qian, Y. et al. TRIM47 is a novel endothelial activation factor that aggravates lipopolysaccharide-induced acute lung injury in mice via K63-linked ubiquitination of TRAF2. Signal Transduct. Target Ther. 7, 148 (2022).
Kang, S. et al. IL-6 trans-signaling induces plasminogen activator inhibitor-1 from vascular endothelial cells in cytokine release syndrome. Proc. Natl Acad. Sci. USA 117, 22351–22356 (2020).
McNicholas, B., Madden, M. G. & Laffey, J. G. Machine learning classifier models: the future for acute respiratory distress syndrome phenotyping? Am. J. Respir. Crit. Care Med. 202, 919–920 (2020).
Delucchi, K. et al. Stability of ARDS subphenotypes over time in two randomised controlled trials. Thorax 73, 439–445 (2018).
Calfee, C. S. et al. Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir. Med. 2, 611–620 (2014).
Maddali, M. V. et al. Validation and utility of ARDS subphenotypes identified by machine-learning models using clinical data: an observational, multicohort, retrospective analysis. Lancet Respir. Med. 10, 367–377 (2022).
Sinha, P. et al. Development and validation of parsimonious algorithms to classify acute respiratory distress syndrome phenotypes: a secondary analysis of randomised controlled trials. Lancet Respir. Med. 8, 247–257 (2020).
Sinha, P., Churpek, M. M. & Calfee, C. S. Machine learning classifier models can identify acute respiratory distress syndrome phenotypes using readily available clinical data. Am. J. Respir. Crit. Care Med. 202, 996–1004 (2020).
Brower, R. G. et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N. Engl. J. Med. 351, 327–336 (2004).
National Heart, L. et al. Comparison of two fluid-management strategies in acute lung injury. N. Engl. J. Med. 354, 2564–2575 (2006).
National Heart, L. et al. Rosuvastatin for sepsis-associated acute respiratory distress syndrome. N. Engl. J. Med. 370, 2191–2200 (2014).
Liu, X. et al. Identification of distinct clinical phenotypes of acute respiratory distress syndrome with differential responses to treatment. Crit. Care 25, 320 (2021).
Villar, J. et al. An early PEEP/FIO2 trial identifies different degrees of lung injury in patients with acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 176, 795–804 (2007).
Villar, J. et al. A universal definition of ARDS: the PaO2/FiO2 ratio under a standard ventilatory setting-a prospective, multicenter validation study. Intensive Care Med 39, 583–592 (2013).
Villar, J. et al. A clinical classification of the acute respiratory distress syndrome for predicting outcome and guiding medical therapy. Crit. Care Med. 43, 346–353 (2015).
Ferguson, N. D. et al. Screening of ARDS patients using standardized ventilator settings: influence on enrollment in a clinical trial. Intensive Care Med. 30, 1111–1116 (2004).
Schenck, E. J. et al. Rapidly improving ARDS in therapeutic randomized controlled trials. Chest 155, 474–482 (2019).
Gavrielatou, E. et al. Rapidly improving acute respiratory distress syndrome in COVID-19: a multi-centre observational study. Respir. Res. 23, 94 (2022).
Chen, H. et al. Longitudinal phenotypes in patients with acute respiratory distress syndrome: a multi-database study. Crit. Care 26, 340 (2022).
Sinha, P. et al. Prevalence of phenotypes of acute respiratory distress syndrome in critically ill patients with COVID-19: a prospective observational study. Lancet Respir. Med. 8, 1209–1218 (2020).
Ranjeva, S. et al. Identifying clinical and biochemical phenotypes in acute respiratory distress syndrome secondary to coronavirus disease-2019. EClinicalMedicine 34, 100829 (2021).
Bos, L. D. J. et al. Longitudinal respiratory subphenotypes in patients with COVID-19-related acute respiratory distress syndrome: results from three observational cohorts. Lancet Respir. Med. 9, 1377–1386 (2021).
Gattinoni, L. et al. COVID-19 pneumonia: different respiratory treatments for different phenotypes? Intensive Care Med. 46, 1099–1102 (2020).
Perier, F. et al. Electrical impedance tomography to titrate positive end-expiratory pressure in COVID-19 acute respiratory distress syndrome. Crit. Care 24, 678 (2020).
Durham, A. L., Caramori, G., Chung, K. F. & Adcock, I. M. Targeted anti-inflammatory therapeutics in asthma and chronic obstructive lung disease. Transl. Res. 167, 192–203 (2016).
Wood, S. L., Pernemalm, M., Crosbie, P. A. & Whetton, A. D. Molecular histology of lung cancer: from targets to treatments. Cancer Treat. Rev. 41, 361–375 (2015).
Bos, L. D. et al. Identification and validation of distinct biological phenotypes in patients with acute respiratory distress syndrome by cluster analysis. Thorax 72, 876–883 (2017).
Pelosi, P. et al. Pulmonary and extrapulmonary acute respiratory distress syndrome are different. Eur. Respir. J. Suppl. 42, 48s–56s (2003).
Calfee, C. S. et al. Distinct molecular phenotypes of direct vs indirect ARDS in single-center and multicenter studies. Chest 147, 1539–1548 (2015).
Peukert, K. et al. Inhibition of Caspase-1 with Tetracycline ameliorates acute lung injury. Am. J. Respir. Crit. Care Med. 204, 53–63 (2021).
Samary, C. S. et al. Lung functional and biologic responses to variable ventilation in experimental pulmonary and extrapulmonary acute respiratory distress Syndrome. Crit. Care Med. 44, e553–e562 (2016).
Moraes, L. et al. Effects of sigh during pressure control and pressure support ventilation in pulmonary and extrapulmonary mild acute lung injury. Crit. Care. 18, 474 (2014).
Bos, L. D. J. et al. Understanding heterogeneity in biologic phenotypes of acute respiratory distress Syndrome by leukocyte expression profiles. Am. J. Respir. Crit. Care Med 200, 42–50 (2019).
Calfee, C. S. et al. Acute respiratory distress syndrome subphenotypes and differential response to simvastatin: secondary analysis of a randomised controlled trial. Lancet Respir. Med. 6, 691–698 (2018).
Kim, K. J., Kim, K. S., Kim, N. R. & Chin, H. S. Effects of simvastatin on the expression of heme oxygenase-1 in human RPE cells. Invest Ophthalmol. Vis. Sci. 53, 6456–6464 (2012).
Manfredini, V. et al. Simvastatin treatment prevents oxidative damage to DNA in whole blood leukocytes of dyslipidemic type 2 diabetic patients. Cell Biochem. Funct. 28, 360–366 (2010).
Griffiths, M. et al. RAND appropriateness panel to determine the applicability of UK guidelines on the management of acute respiratory distress syndrome (ARDS) and other strategies in the context of the COVID-19 pandemic. Thorax 77, 129–135 (2022).
Qadir, N. et al. An update on management of adult patients with acute respiratory distress syndrome: An Official American Thoracic Society Clinical Practice Guideline. Am. J. Respir. Crit. Care Med 209, 24–36 (2024).
Grasselli, G. et al. ESICM guidelines on acute respiratory distress syndrome: definition, phenotyping and respiratory support strategies. Intensive Care Med. 49, 727–759 (2023).
Tasaka, S. et al. ARDS clinical practice guideline 2021. Respir. Investig. 60, 446–495 (2022).
Nishimura, M. High-flow nasal cannula oxygen therapy devices. Respir. Care 64, 735–742 (2019).
Rochwerg, B. et al. The role for high flow nasal cannula as a respiratory support strategy in adults: a clinical practice guideline. Intensive Care Med. 46, 2226–2237 (2020).
Morais, C. C. A. et al. High positive end-expiratory pressure renders spontaneous effort noninjurious. Am. J. Respir. Crit. Care Med. 197, 1285–1296 (2018).
Patel, B. K. et al. Effect of noninvasive ventilation delivered by helmet vs face mask on the rate of endotracheal intubation in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA 315, 2435–2441 (2016).
Grieco, D. L. et al. Effect of helmet noninvasive ventilation vs high-flow nasal oxygen on days free of respiratory support in patients with COVID-19 and moderate to severe hypoxemic respiratory failure: The HENIVOT randomized clinical trial. JAMA 325, 1731–1743 (2021).
Acute Respiratory Distress Syndrome, N. et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N. Engl. J. Med. 342, 1301–1308 (2000).
Amato, M. B. et al. Driving pressure and survival in the acute respiratory distress syndrome. N. Engl. J. Med. 372, 747–755 (2015).
Costa, E. L. V. et al. Ventilatory variables and mechanical power in patients with acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 204, 303–311 (2021).
Beitler, J. R. & Walkey, A. J. The staying power of pressure- and volume-limited ventilation in acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 204, 247–249 (2021).
Lachmann, B. Open up the lung and keep the lung open. Intensive Care Med 18, 319–321 (1992).
Mercat, A. et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA 299, 646–655 (2008).
Meade, M. O. et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA 299, 637–645 (2008).
Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial, I. et al. Effect of lung recruitment and titrated Positive End-Expiratory Pressure (PEEP) vs Low PEEP on mortality in patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA 318, 1335–1345 (2017).
Goligher, E. C. et al. Oxygenation response to positive end-expiratory pressure predicts mortality in acute respiratory distress syndrome. A secondary analysis of the LOVS and ExPress trials. Am. J. Respir. Crit. Care Med. 190, 70–76 (2014).
Beitler, J. R. et al. Effect of Titrating Positive End-Expiratory Pressure (PEEP) With an Esophageal Pressure-Guided Strategy vs an Empirical High PEEP-Fio2 strategy on death and days free from mechanical ventilation among patients with acute respiratory distress syndrome: a randomized clinical trial. JAMA 321, 846–857 (2019).
Chiumello, D., Carlesso, E., Brioni, M. & Cressoni, M. Airway driving pressure and lung stress in ARDS patients. Crit. Care 20, 276 (2016).
Nanki, M. et al. Evaluation of the effect of metoprolol on energy metabolism in the ischaemic myocardium in relation to regional myocardial blood flow. Cardiovasc. Res. 21, 660–667 (1987).
Marini, J. J., Rocco, P. R. M. & Gattinoni, L. Static and dynamic contributors to ventilator-induced lung injury in clinical practice. pressure, energy, and power. Am. J. Respir. Crit. Care Med. 201, 767–774 (2020).
Cressoni, M. et al. Mechanical power and development of ventilator-induced lung injury. Anesthesiology 124, 1100–1108 (2016).
Gattinoni, L. et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med 42, 1567–1575 (2016).
Bhalla, A. K. et al. Mechanical power in pediatric acute respiratory distress syndrome: a PARDIE study. Crit. Care 26, 2 (2022).
Coppola, S. et al. Effect of mechanical power on intensive care mortality in ARDS patients. Crit. Care 24, 246 (2020).
Serpa Neto, A. et al. Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med. 44, 1914–1922 (2018).
Pelosi, P. et al. Vertical gradient of regional lung inflation in adult respiratory distress syndrome. Am. J. Respir. Crit. Care Med 149, 8–13 (1994).
Gattinoni, L. et al. Body position changes redistribute lung computed-tomographic density in patients with acute respiratory failure. Anesthesiology 74, 15–23 (1991).
Gattinoni, L. et al. Lung recruitment in patients with the acute respiratory distress syndrome. N. Engl. J. Med 354, 1775–1786 (2006).
Taccone, P. et al. Prone positioning in patients with moderate and severe acute respiratory distress syndrome: a randomized controlled trial. JAMA 302, 1977–1984 (2009).
Guerin, C. et al. Effects of systematic prone positioning in hypoxemic acute respiratory failure: a randomized controlled trial. JAMA 292, 2379–2387 (2004).
Gattinoni, L., Taccone, P., Carlesso, E. & Marini, J. J. Prone position in acute respiratory distress syndrome. Rationale, indications, and limits. Am. J. Respir. Crit. Care Med. 188, 1286–1293 (2013).
Sud, S. et al. Effect of prone positioning during mechanical ventilation on mortality among patients with acute respiratory distress syndrome: a systematic review and meta-analysis. CMAJ 186, E381–E390 (2014).
Guerin, C. et al. Prone positioning in severe acute respiratory distress syndrome. N. Engl. J. Med. 368, 2159–2168 (2013).
Coppo, A. et al. Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respir. Med. 8, 765–774 (2020).
Thompson, A. E., Ranard, B. L., Wei, Y. & Jelic, S. Prone positioning in awake, nonintubated patients with COVID-19 hypoxemic respiratory failure. JAMA Intern. Med. 180, 1537–1539 (2020).
Alhazzani, W. et al. Effect of awake prone positioning on endotracheal intubation in patients with COVID-19 and acute respiratory failure: a randomized clinical trial. JAMA 327, 2104–2113 (2022).
Ehrmann, S. et al. Awake prone positioning for COVID-19 acute hypoxaemic respiratory failure: a randomised, controlled, multinational, open-label meta-trial. Lancet Respir. Med 9, 1387–1395 (2021).
Petit, M. et al. Prone-positioning for severe acute respiratory distress syndrome requiring extracorporeal membrane oxygenation. Crit. Care Med. 50, 264–274 (2022).
Schmidt, M. et al. Prone positioning during extracorporeal membrane oxygenation in patients with severe ARDS: The PRONECMO randomized clinical trial. JAMA 330, 2343–2353 (2023).
Munshi, L. et al. Prone position for acute respiratory distress syndrome. a systematic review and meta-analysis. Ann. Am. Thorac. Soc. 14, S280–S288 (2017).
Rampon, G. et al. Smartphone-guided self-prone positioning vs usual care in nonintubated hospital ward patients with COVID-19: A pragmatic randomized clinical trial. Chest 162, 782–791 (2022).
Li, J. et al. Awake prone positioning for non-intubated patients with COVID-19-related acute hypoxaemic respiratory failure: a systematic review and meta-analysis. Lancet Respir. Med. 10, 573–583 (2022).
Torbic, H., Krishnan, S., Harnegie, M. P. & Duggal, A. Neuromuscular blocking agents for ARDS: A systematic review and meta-analysis. Respir. Care 66, 120–128 (2021).
Papazian, L. et al. Neuromuscular blockers in early acute respiratory distress syndrome. N. Engl. J. Med. 363, 1107–1116 (2010).
National Heart, L. et al. Early neuromuscular blockade in the acute respiratory distress syndrome. N. Engl. J. Med. 380, 1997–2008 (2019).
Ely, E. W. et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA 289, 2983–2991 (2003).
Peek, G. J. et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet 374, 1351–1363 (2009).
Combes, A. et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N. Engl. J. Med. 378, 1965–1975 (2018).
Goligher, E. C. et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome and posterior probability of mortality benefit in a post hoc Bayesian analysis of a randomized clinical trial. JAMA 320, 2251–2259 (2018).
Combes, A. et al. ECMO for severe ARDS: systematic review and individual patient data meta-analysis. Intensive Care Med. 46, 2048–2057 (2020).
Camporota, L. et al. Consensus on the referral and admission of patients with severe respiratory failure to the NHS ECMO service. Lancet Respir. Med. 9, e16–e17 (2021).
McNamee, J. J. et al. Effect of lower tidal volume ventilation facilitated by extracorporeal carbon dioxide removal vs standard care ventilation on 90-day mortality in patients with acute hypoxemic respiratory failure: The REST randomized clinical trial. JAMA 326, 1013–1023 (2021).
Hajage, D. et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: An emulated target trial analysis. Am. J. Respir. Crit. Care Med. 206, 281–294 (2022).
Urner, M. et al. Venovenous extracorporeal membrane oxygenation in patients with acute COVID-19 associated respiratory failure: comparative effectiveness study. BMJ 377, e068723 (2022).
Combes, A. et al. Position paper for the organization of extracorporeal membrane oxygenation programs for acute respiratory failure in adult patients. Am. J. Respir. Crit. Care Med. 190, 488–496 (2014).
Steinberg, K. P. et al. Efficacy and safety of corticosteroids for persistent acute respiratory distress syndrome. N. Engl. J. Med. 354, 1671–1684 (2006).
Villar, J. et al. Dexamethasone treatment for the acute respiratory distress syndrome: a multicentre, randomised controlled trial. Lancet Respir. Med. 8, 267–276 (2020).
Chaudhuri, D. et al. Corticosteroids in COVID-19 and non-COVID-19 ARDS: a systematic review and meta-analysis. Intensive Care Med. 47, 521–537 (2021).
Group, R. C. et al. Dexamethasone in hospitalized patients with Covid-19. N. Engl. J. Med 384, 693–704 (2021).
WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, et al.Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: A meta-analysis. JAMA 324, 1330–1341 (2020).
Moreno, G. et al. Corticosteroid treatment in critically ill patients with severe influenza pneumonia: a propensity score matching study. Intensive Care Med. 44, 1470–1482 (2018).
Sadeghian Chaleshtori, S. et al. Prevention of LPS-induced acute respiratory distress syndrome in sheep by bone marrow-derived mesenchymal stem/stromal cells. Life Sci. 263, 118600 (2020).
Rojas, M. et al. Human adult bone marrow-derived stem cells decrease severity of lipopolysaccharide-induced acute respiratory distress syndrome in sheep. Stem Cell Res. Ther. 5, 42 (2014).
Wilson, J. G. et al. Mesenchymal stem (stromal) cells for treatment of ARDS: a phase 1 clinical trial. Lancet Respir. Med. 3, 24–32 (2015).
Silva, J. D. et al. Mesenchymal stem cells from bone marrow, adipose tissue, and lung tissue differentially mitigate lung and distal organ damage in experimental acute respiratory distress syndrome. Crit. Care Med 46, e132–e140 (2018).
Kasper, M. & Barth, K. Potential contribution of alveolar epithelial type I cells to pulmonary fibrosis. Biosci. Rep. 37, BSR20171301 (2017).
Zeng, L. et al. The cellular kinetics of lung alveolar epithelial cells and its relationship with lung tissue repair after acute lung injury. Respir. Res. 17, 164 (2016).
Huang, X. et al. Endothelial Hypoxia-Inducible Factor-1alpha is required for vascular repair and resolution of inflammatory lung injury through Forkhead Box Protein M1. Am. J. Pathol. 189, 1664–1679 (2019).
Liu, Y. et al. FoxM1 mediates the progenitor function of type II epithelial cells in repairing alveolar injury induced by Pseudomonas aeruginosa. J. Exp. Med. 208, 1473–1484 (2011).
Luo, Y. et al. Overexpression of FoxM1 enhanced the protective effect of bone marrow-derived mesenchymal stem cells on lipopolysaccharide-induced acute lung injury through the activation of Wnt/beta-Catenin signaling. Oxid. Med. Cell Longev. 2023, 8324504 (2023).
Luo, Y. et al. Overexpression of FoxM1 optimizes the therapeutic effect of bone marrow mesenchymal stem cells on acute respiratory distress syndrome. Stem Cell Res. Ther. 14, 27 (2023).
Chen, X. Y. et al. YAP-regulated type II alveolar epithelial cell differentiation mediated by human umbilical cord-derived mesenchymal stem cells in acute respiratory distress syndrome. Biomed. Pharmacother. 159, 114302 (2023).
Li, L. et al. Mesenchymal stem cells with downregulated Hippo signaling attenuate lung injury in mice with lipopolysaccharide‑induced acute respiratory distress syndrome. Int. J. Mol. Med. 43, 1241–1252 (2019).
Zhang, Q. et al. Hippo signalling governs cytosolic nucleic acid sensing through YAP/TAZ-mediated TBK1 blockade. Nat. Cell Biol. 19, 362–374 (2017).
Liu, A. et al. Wnt5a through noncanonical Wnt/JNK or Wnt/PKC signaling contributes to the differentiation of mesenchymal stem cells into type II alveolar epithelial cells in vitro. PLoS One 9, e90229 (2014).
Cai, S. X. et al. The orphan receptor Tyrosine Kinase ROR2 facilitates MSCs to repair lung injury in ARDS animal model. Cell Transpl. 25, 1561–1574 (2016).
Wang, K. et al. Vimentin-Rab7a pathway mediates the migration of MSCs and lead to therapeutic effects on ARDS. Stem Cells Int. 2021, 9992381 (2021).
Lu, Z. et al. Mesenchymal stem cells induce dendritic cell immune tolerance via paracrine hepatocyte growth factor to alleviate acute lung injury. Stem Cell Res. Ther. 10, 372 (2019).
Lu, Z. et al. Mesenchymal stem cells activate Notch signaling to induce regulatory dendritic cells in LPS-induced acute lung injury. J. Transl. Med. 18, 241 (2020).
Hezam, K. et al. Superior protective effects of PGE2 priming mesenchymal stem cells against LPS-induced acute lung injury (ALI) through macrophage immunomodulation. Stem Cell Res. Ther. 14, 48 (2023).
Xu, A. L. et al. Mesenchymal stem cells reconditioned in their own serum exhibit augmented therapeutic properties in the setting of acute respiratory distress syndrome. Stem Cells Transl. Med 8, 1092–1106 (2019).
He, X. et al. Mesenchymal stem cells inhibited the apoptosis of alveolar epithelial cells caused by ARDS through CXCL12/CXCR4 axis. Bioengineered 13, 9060–9070 (2022).
Su, V. Y., Lin, C. S., Hung, S. C. & Yang, K. Y. Mesenchymal stem cell-conditioned medium induces neutrophil apoptosis associated with inhibition of the NF-kappaB pathway in Endotoxin-induced acute lung injury. Int. J. Mol. Sci. 20, 2208 (2019).
Chen, X. et al. Mesenchymal stem cells overexpressing heme oxygenase-1 ameliorate lipopolysaccharide-induced acute lung injury in rats. J. Cell Physiol. 234, 7301–7319 (2019).
Cardenes, N. et al. Cell therapy for ARDS: efficacy of endobronchial versus intravenous administration and biodistribution of MAPCs in a large animal model. BMJ Open Respir. Res. 6, e000308 (2019).
Islam, D. et al. Identification and modulation of microenvironment is crucial for effective mesenchymal stromal cell therapy in acute lung injury. Am. J. Respir. Crit. Care Med 199, 1214–1224 (2019).
Younes, N. et al. Mesenchymal stromal/stem cells modulate response to experimental sepsis-induced lung injury via regulation of miR-27a-5p in recipient mice. Thorax 75, 556–567 (2020).
Florian, M. et al. Gene engineered mesenchymal stem cells: greater transgene expression and efficacy with minicircle vs. plasmid DNA vectors in a mouse model of acute lung injury. Stem Cell Res. Ther. 12, 184 (2021).
Hu, S. et al. The hepatocyte growth factor-expressing character is required for mesenchymal stem cells to protect the lung injured by lipopolysaccharide in vivo. Stem Cell Res. Ther. 7, 66 (2016).
Meng, S. S. et al. mTORC2 activation mediated by mesenchymal stem cell-secreted hepatocyte growth factors for the recovery of lipopolysaccharide-induced vascular endothelial barrier. Stem Cells Int 2021, 9981589 (2021).
Ishii, M. et al. Increased in vitro intercellular barrier function of lung epithelial cells using Adipose-derived mesenchymal stem/stromal cells. Pharmaceutics 13, 1264 (2021).
Li, J. Z. et al. Mechanically stretched mesenchymal stem cells can reduce the effects of LPS-induced injury on the pulmonary microvascular endothelium barrier. Stem Cells Int. 2020, 8861407 (2020).
McAuley, D. F. et al. Clinical grade allogeneic human mesenchymal stem cells restore alveolar fluid clearance in human lungs rejected for transplantation. Am. J. Physiol. Lung Cell Mol. Physiol. 306, L809–L815 (2014).
Gennai, S. et al. Microvesicles derived from human mesenchymal stem cells restore alveolar fluid clearance in human lungs rejected for transplantation. Am. J. Transplant. 15, 2404–2412 (2015).
Yip, H. K. et al. Human Umbilical cord-derived mesenchymal stem cells for acute respiratory distress syndrome. Crit. Care Med 48, e391–e399 (2020).
Wick, K. D. et al. Mesenchymal stromal cells reduce evidence of lung injury in patients with ARDS. JCI Insight 6, e148983 (2021).
Simonson, O. E. et al. Five-year follow-up after mesenchymal stromal cell-based treatment of severe acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 202, 1051–1055 (2020).
Simonson, O. E. et al. In vivo effects of mesenchymal stromal cells in two patients with severe acute respiratory distress syndrome. Stem Cells Transl. Med. 4, 1199–1213 (2015).
Chang, Y. et al. Intratracheal administration of umbilical cord blood-derived mesenchymal stem cells in a patient with acute respiratory distress syndrome. J. Korean Med. Sci. 29, 438–440 (2014).
Gorman, E. et al. Repair of acute respiratory distress syndrome by stromal cell administration (REALIST) trial: A phase 1 trial. EClinicalMedicine 41, 101167 (2021).
Zheng, G. et al. Treatment of acute respiratory distress syndrome with allogeneic adipose-derived mesenchymal stem cells: a randomized, placebo-controlled pilot study. Respir. Res. 15, 39 (2014).
Matthay, M. A. et al. Treatment with allogeneic mesenchymal stromal cells for moderate to severe acute respiratory distress syndrome (START study): a randomised phase 2a safety trial. Lancet Respir. Med. 7, 154–162 (2019).
Gregoire, C. et al. Bone marrow-derived mesenchymal stromal cell therapy in severe COVID-19: Preliminary results of a Phase I/II clinical trial. Front Immunol. 13, 932360 (2022).
Lanzoni, G. et al. Umbilical cord mesenchymal stem cells for COVID-19 acute respiratory distress syndrome: A double-blind, phase 1/2a, randomized controlled trial. Stem Cells Transl. Med. 10, 660–673 (2021).
Whittaker Brown, S. A. et al. Mesenchymal stromal cell therapy for acute respiratory distress syndrome due to coronavirus disease 2019. Cytotherapy 24, 835–840 (2022).
Monsel, A. et al. Treatment of COVID-19-associated ARDS with mesenchymal stromal cells: a multicenter randomized double-blind trial. Crit. Care 26, 48 (2022).
Aghayan, H. R. et al. Human placenta-derived mesenchymal stem cells transplantation in patients with acute respiratory distress syndrome (ARDS) caused by COVID-19 (phase I clinical trial): safety profile assessment. Stem Cell Res. Ther. 13, 365 (2022).
Hashemian, S. R. et al. Mesenchymal stem cells derived from perinatal tissues for treatment of critically ill COVID-19-induced ARDS patients: a case series. Stem Cell Res. Ther. 12, 91 (2021).
Kouroupis, D. et al. Umbilical cord-derived mesenchymal stem cells modulate TNF and soluble TNF Receptor 2 (sTNFR2) in COVID-19 ARDS patients. Eur. Rev. Med Pharm. Sci. 25, 4435–4438 (2021).
Bukreieva, T. et al. Treatment of acute respiratory distress syndrome caused by COVID-19 with human umbilical cord mesenchymal stem cells. Int. J. Mol. Sci. 24, 4435 (2023).
Iglesias, M. et al. Mesenchymal stem cells for the compassionate treatment of severe acute respiratory distress Syndrome Due to COVID 19. Aging Dis. 12, 360–370 (2021).
Dilogo, I. H. et al. Umbilical cord mesenchymal stromal cells as critical COVID-19 adjuvant therapy: A randomized controlled trial. Stem Cells Transl. Med. 10, 1279–1287 (2021).
Chen, M. C. et al. pcMSC modulates immune dysregulation in patients with COVID-19-induced refractory acute lung injury. Front Immunol. 13, 871828 (2022).
Bowdish, M. E. et al. A randomized trial of mesenchymal stromal cells for moderate to severe acute respiratory distress syndrome from COVID-19. Am. J. Respir. Crit. Care Med. 207, 261–270 (2023).
Kaffash Farkhad, N. et al. Mesenchymal stromal cell therapy for COVID-19-induced ARDS patients: a successful phase 1, control-placebo group, clinical trial. Stem Cell Res. Ther. 13, 283 (2022).
Sadeghi, B. et al. Conquering the cytokine storm in COVID-19-induced ARDS using placenta-derived decidua stromal cells. J. Cell Mol. Med. 25, 10554–10564 (2021).
Guillamat-Prats, R. et al. Intratracheal instillation of alveolar type II cells enhances recovery from acute lung injury in rats. J. Heart Lung Transpl. 37, 782–791 (2018).
Guillamat-Prats, R. et al. Alveolar Type II cells or mesenchymal stem cells: comparison of two different cell therapies for the treatment of acute lung injury in rats. Cells 9, 1816 (2020).
Wu, J. et al. Immunity-and-matrix-regulatory cells derived from human embryonic stem cells safely and effectively treat mouse lung injury and fibrosis. Cell Res. 30, 794–809 (2020).
Hu, Q. et al. Extracellular vesicles in the pathogenesis and treatment of acute lung injury. Mil. Med Res. 9, 61 (2022).
Guervilly, C. et al. High levels of circulating leukocyte microparticles are associated with better outcome in acute respiratory distress syndrome. Crit. Care 15, R31 (2011).
Takei, Y. et al. Increase in circulating ACE-positive endothelial microparticles during acute lung injury. Eur. Respir. J. 54, 1801188 (2019).
Meidert, A. S. et al. Extracellular vesicle Associated miRNAs regulate signaling pathways involved in COVID-19 Pneumonia and the progression to severe acute respiratory Corona Virus-2 Syndrome. Front Immunol. 12, 784028 (2021).
Li, G. et al. Plasma extracellular vesicle delivery of miR-210-3p by targeting ATG7 to promote sepsis-induced acute lung injury by regulating autophagy and activating inflammation. Exp. Mol. Med. 53, 1180–1191 (2021).
Monsel, A. et al. Therapeutic effects of human mesenchymal stem cell-derived microvesicles in severe pneumonia in mice. Am. J. Respir. Crit. Care Med. 192, 324–336 (2015).
Varkouhi, A. K. et al. Extracellular vesicles from Interferon-gamma-primed human umbilical cord mesenchymal stromal cells reduce escherichia coli-induced acute lung injury in rats. Anesthesiology 130, 778–790 (2019).
Su, Y. et al. Mesenchymal stromal cells-derived extracellular vesicles reprogramme macrophages in ARDS models through the miR-181a-5p-PTEN-pSTAT5-SOCS1 axis. Thorax 78, 617–630 (2023).
Morrison, T. J. et al. Mesenchymal stromal cells modulate macrophages in clinically relevant lung injury models by extracellular vesicle mitochondrial transfer. Am. J. Respir. Crit. Care Med. 196, 1275–1286 (2017).
Mao, G. C. et al. BMSC-derived exosomes ameliorate sulfur mustard-induced acute lung injury by regulating the GPRC5A-YAP axis. Acta Pharm. Sin. 42, 2082–2093 (2021).
Liu, X. et al. BMSC-derived exosomes ameliorate LPS-induced acute lung injury by miR-384-5p-controlled alveolar macrophage autophagy. Oxid. Med Cell Longev. 2021, 9973457 (2021).
Xia, L. et al. AdMSC-derived exosomes alleviate acute lung injury via transferring mitochondrial component to improve homeostasis of alveolar macrophages. Theranostics 12, 2928–2947 (2022).
Dutra Silva, J. et al. Mesenchymal stromal cell extracellular vesicles rescue mitochondrial dysfunction and improve barrier integrity in clinically relevant models of ARDS. Eur. Respir. J. 58, 2002978 (2021).
Shah, T. et al. Alk5/Runx1 signaling mediated by extracellular vesicles promotes vascular repair in acute respiratory distress syndrome. Clin. Transl. Med. 7, 19 (2018).
Mizuta, Y. et al. Exosomes from adipose tissue-derived mesenchymal stem cells ameliorate histone-induced acute lung injury by activating the PI3K/Akt pathway in endothelial cells. Stem Cell Res. Ther. 11, 508 (2020).
Feng, Z. et al. Epithelium- and endothelium-derived exosomes regulate the alveolar macrophages by targeting RGS1 mediated calcium signaling-dependent immune response. Cell Death Differ. 28, 2238–2256 (2021).
Zhou, Y. et al. Exosomes from endothelial progenitor cells improve outcomes of the lipopolysaccharide-induced acute lung injury. Crit. Care 23, 44 (2019).
Moon, H. G. et al. Lung epithelial cell-derived extracellular vesicles activate macrophage-mediated inflammatory responses via ROCK1 pathway. Cell Death Dis. 6, e2016 (2015).
Beigel, J. H. et al. Immune plasma for the treatment of severe influenza: an open-label, multicentre, phase 2 randomised study. Lancet Respir. Med. 5, 500–511 (2017).
Beigel, J. H. et al. Anti-influenza immune plasma for the treatment of patients with severe influenza A: a randomised, double-blind, phase 3 trial. Lancet Respir. Med. 7, 941–950 (2019).
Shen, C. et al. Treatment of 5 critically ill patients with COVID-19 with Convalescent plasma. JAMA 323, 1582–1589 (2020).
Allahyari, A. et al. Efficacy and safety of convalescent plasma therapy in severe COVID-19 patients with acute respiratory distress syndrome. Int Immunopharmacol. 93, 107239 (2021).
Ray, Y. et al. A phase 2 single center open label randomised control trial for convalescent plasma therapy in patients with severe COVID-19. Nat. Commun. 13, 383 (2022).
Cao, W. et al. High-dose intravenous immunoglobulin as a therapeutic option for deteriorating patients with Coronavirus disease 2019. Open Forum Infect. Dis. 7, ofaa102 (2020).
Shao, Z. et al. Clinical efficacy of intravenous immunoglobulin therapy in critical ill patients with COVID-19: a multicenter retrospective cohort study. Clin. Transl. Immunol. 9, e1192 (2020).
Xie, Y. et al. Effect of regular intravenous immunoglobulin therapy on prognosis of severe pneumonia in patients with COVID-19. J. Infect. 81, 318–356 (2020).
Cao, W. et al. High-dose Intravenous Immunoglobulin in severe coronavirus disease 2019: A Multicenter Retrospective Study in China. Front Immunol. 12, 627844 (2021).
Mazeraud, A. et al. Intravenous immunoglobulins in patients with COVID-19-associated moderate-to-severe acute respiratory distress syndrome (ICAR): multicentre, double-blind, placebo-controlled, phase 3 trial. Lancet Respir. Med. 10, 158–166 (2022).
Green, M. R. Targeting targeted therapy. N. Engl. J. Med. 350, 2191–2193 (2004).
Thomas, A., Teicher, B. A. & Hassan, R. Antibody-drug conjugates for cancer therapy. Lancet Oncol. 17, e254–e262 (2016).
Zhao, Z., Ukidve, A., Kim, J. & Mitragotri, S. Targeting strategies for tissue-specific drug delivery. Cell 181, 151–167 (2020).
Goncalves, G. A. R. & Paiva, R. M. A. Gene therapy: advances, challenges and perspectives. Einstein 15, 369–375 (2017).
Barresi, V., Musmeci, C., Rinaldi, A. & Condorelli, D. F. Transcript-targeted therapy based on RNA Interference and Antisense Oligonucleotides: Current applications and novel molecular targets. Int. J. Mol. Sci. 23, 8875 (2022).
Sinha, P. & Calfee, C. S. Phenotypes in acute respiratory distress syndrome: moving towards precision medicine. Curr. Opin. Crit. Care 25, 12–20 (2019).
Meyer, N. J., Gattinoni, L. & Calfee, C. S. Acute respiratory distress syndrome. Lancet 398, 622–637 (2021).
Aikawa, N. et al. Reevaluation of the efficacy and safety of the neutrophil elastase inhibitor, Sivelestat, for the treatment of acute lung injury associated with systemic inflammatory response syndrome; a phase IV study. Pulm. Pharm. Ther. 24, 549–554 (2011).
Gao, X. et al. Efficacy, safety, and pharmacoeconomics of sivelestat sodium in the treatment of septic acute respiratory distress syndrome: a retrospective cohort study. Ann. Palliat. Med. 10, 11910–11917 (2021).
Pu, S. et al. Effect of sivelestat sodium in patients with acute lung injury or acute respiratory distress syndrome: a meta-analysis of randomized controlled trials. BMC Pulm. Med. 17, 148 (2017).
Zhang, N., Wang, Z. & Zhao, Y. Selective inhibition of Tumor necrosis factor receptor-1 (TNFR1) for the treatment of autoimmune diseases. Cytokine Growth Factor Rev. 55, 80–85 (2020).
Proudfoot, A. et al. Novel anti-tumour necrosis factor receptor-1 (TNFR1) domain antibody prevents pulmonary inflammation in experimental acute lung injury. Thorax 73, 723–730 (2018).
Wu, H. et al. Keratinocyte growth factor augments pulmonary innate immunity through epithelium-driven, GM-CSF-dependent paracrine activation of alveolar macrophages. J. Biol. Chem. 286, 14932–14940 (2011).
Paine, R. 3rd et al. A randomized trial of recombinant human granulocyte-macrophage colony stimulating factor for patients with acute lung injury. Crit. Care Med. 40, 90–97 (2012).
Presneill, J. J. et al. A randomized phase II trial of granulocyte-macrophage colony-stimulating factor therapy in severe sepsis with respiratory dysfunction. Am. J. Respir. Crit. Care Med. 166, 138–143 (2002).
Kim, I. K. et al. Effect of tyrosine kinase inhibitors, imatinib and nilotinib, in murine lipopolysaccharide-induced acute lung injury during neutropenia recovery. Crit. Care 17, R114 (2013).
Overbeek, M. J. et al. Possible role of imatinib in clinical pulmonary veno-occlusive disease. Eur. Respir. J. 32, 232–235 (2008).
Carnevale-Schianca, F. et al. Complete resolution of life-threatening bleomycin-induced pneumonitis after treatment with imatinib mesylate in a patient with Hodgkin’s lymphoma: hope for severe chemotherapy-induced toxicity? J. Clin. Oncol. 29, e691–e693 (2011).
Aman, J. et al. Reversal of vascular leak with imatinib. Am. J. Respir. Crit. Care Med 188, 1171–1173 (2013).
Tauber, S. C. & Nau, R. Immunomodulatory properties of antibiotics. Curr. Mol. Pharm. 1, 68–79 (2008).
Spyridaki, A. et al. Effect of clarithromycin in inflammatory markers of patients with ventilator-associated pneumonia and sepsis caused by Gram-negative bacteria: results from a randomized clinical study. Antimicrob. Agents Chemother. 56, 3819–3825 (2012).
Giamarellos-Bourboulis, E. J. et al. Clarithromycin for early anti-inflammatory responses in community-acquired pneumonia in Greece (ACCESS): a randomised, double-blind, placebo-controlled trial. Lancet Respir. Med. 12, 294–304 (2024).
Sauer, A., Peukert, K., Putensen, C. & Bode, C. Antibiotics as immunomodulators: a potential pharmacologic approach for ARDS treatment. Eur. Respir. Rev. 30, 210093 (2021).
Shyamsundar, M. et al. Keratinocyte growth factor promotes epithelial survival and resolution in a human model of lung injury. Am. J. Respir. Crit. Care Med. 189, 1520–1529 (2014).
McAuley, D. F. et al. Keratinocyte growth factor for the treatment of the acute respiratory distress syndrome (KARE): a randomised, double-blind, placebo-controlled phase 2 trial. Lancet Respir. Med. 5, 484–491 (2017).
Gutbier, B. et al. Vasculotide reduces pulmonary hyperpermeability in experimental pneumococcal pneumonia. Crit. Care 21, 274 (2017).
Dekker, N. A. M. et al. Vasculotide, an angiopoietin-1 mimetic, reduces pulmonary vascular leakage and preserves microcirculatory perfusion during cardiopulmonary bypass in rats. Br. J. Anaesth. 121, 1041–1051 (2018).
Lask, A. et al. Adjunctive therapy with the Tie2 agonist Vasculotide reduces pulmonary permeability in Streptococcus pneumoniae infected and mechanically ventilated mice. Sci. Rep. 12, 15531 (2022).
Li, H. P. et al. Therapeutic agents rounding up the immunopathology of COVID-19. Ther. Clin. Risk Manag. 17, 657–668 (2021).
King, R. & Tuthill, C. Immune modulation with Thymosin Alpha 1 treatment. Vitam. Horm. 102, 151–178 (2016).
Matteucci, C. et al. Thymosin alpha 1 and HIV-1: recent advances and future perspectives. Future Microbiol. 12, 141–155 (2017).
Wu, M. et al. Thymosin alpha1 therapy in critically ill patients with COVID-19: A multicenter retrospective cohort study. Int. Immunopharmacol. 88, 106873 (2020).
Sun, Q. et al. The effect of thymosin alpha1 on mortality of critical COVID-19 patients: A multicenter retrospective study. Int. Immunopharmacol. 90, 107143 (2021).
Lang, F. M. et al. GM-CSF-based treatments in COVID-19: reconciling opposing therapeutic approaches. Nat. Rev. Immunol. 20, 507–514 (2020).
Temesgen, Z. et al. GM-CSF Neutralization with Lenzilumab in severe COVID-19 Pneumonia: A case-cohort study. Mayo Clin. Proc. 95, 2382–2394 (2020).
De Luca, G. et al. GM-CSF blockade with mavrilimumab in severe COVID-19 pneumonia and systemic hyperinflammation: a single-centre, prospective cohort study. Lancet Rheumatol. 2, e465–e473 (2020).
Cremin, B. J. A review of the ultrasonic appearances of posterior urethral valve and ureteroceles. Pediatr. Radio. 16, 357–364 (1986).
Cheng, L. L. et al. Effect of recombinant human granulocyte colony-stimulating factor for patients with Coronavirus Disease 2019 (COVID-19) and Lymphopenia: A randomized clinical trial. JAMA Intern Med. 181, 71–78 (2021).
Shrivastava, G. et al. Inflammasomes and its importance in viral infections. Immunol. Res 64, 1101–1117 (2016).
Mertens, M. & Singh, J. A. Anakinra for rheumatoid arthritis: a systematic review. J. Rheumatol. 36, 1118–1125 (2009).
Kharazmi, A. B. et al. A randomized controlled clinical trial on efficacy and safety of anakinra in patients with severe COVID-19. Immun. Inflamm. Dis. 10, 201–208 (2022).
Cavalli, G. et al. Interleukin-1 blockade with high-dose anakinra in patients with COVID-19, acute respiratory distress syndrome, and hyperinflammation: a retrospective cohort study. Lancet Rheumatol. 2, e325–e331 (2020).
Kyriazopoulou, E. et al. Effect of anakinra on mortality in patients with COVID-19: a systematic review and patient-level meta-analysis. Lancet Rheumatol. 3, e690–e697 (2021).
Smolen, J. S. et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2022 update. Ann. Rheum. Dis. 82, 3–18 (2023).
Hirano, T. & Murakami, M. COVID-19: A new virus, but a familiar receptor and Cytokine Release Syndrome. Immunity 52, 731–733 (2020).
Merchante, N. et al. Early Use of Sarilumab in patients hospitalized with COVID-19 Pneumonia and features of systemic inflammation: the SARICOR randomized clinical trial. Antimicrob. Agents Chemother. 66, e0210721 (2022).
Lescure, F. X. et al. Sarilumab in patients admitted to hospital with severe or critical COVID-19: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Respir. Med. 9, 522–532 (2021).
Aiello, S. et al. C5a and C5aR1 are key drivers of microvascular platelet aggregation in clinical entities spanning from aHUS to COVID-19. Blood Adv. 6, 866–881 (2022).
Vlaar, A. P. J. et al. Anti-C5a antibody (vilobelimab) therapy for critically ill, invasively mechanically ventilated patients with COVID-19 (PANAMO): a multicentre, double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Respir. Med. 10, 1137–1146 (2022).
Pairo-Castineira, E. et al. Genetic mechanisms of critical illness in COVID-19. Nature 591, 92–98 (2021).
La Rosee, F. et al. The Janus kinase 1/2 inhibitor ruxolitinib in COVID-19 with severe systemic hyperinflammation. Leukemia 34, 1805–1815 (2020).
Neubauer, A. et al. The janus-kinase inhibitor ruxolitinib in SARS-CoV-2 induced acute respiratory distress syndrome (ARDS). Leukemia 35, 2917–2923 (2021).
Shak, S. et al. Recombinant human DNase I reduces the viscosity of cystic fibrosis sputum. Proc. Natl Acad. Sci. USA 87, 9188–9192 (1990).
DeLeo, F. R. & Allen, L. H. Phagocytosis and neutrophil extracellular traps. Fac. Rev. 9, 25 (2020).
Holliday, Z. M. et al. Non-randomized trial of Dornase Alfa for acute respiratory distress syndrome secondary to Covid-19. Front Immunol. 12, 714833 (2021).
Ward-Kavanagh, L. K., Lin, W. W., Sedy, J. R. & Ware, C. F. The TNF receptor superfamily in co-stimulating and co-inhibitory responses. Immunity 44, 1005–1019 (2016).
Perlin, D. S. et al. Randomized, double-blind, controlled trial of human anti-LIGHT monoclonal antibody in COVID-19 acute respiratory distress syndrome. J. Clin. Invest. 132, e153173 (2022).
Zhao, C. & Zhao, W. NLRP3 Inflammasome-A Key Player in Antiviral Responses. Front. Immunol. 11, 211 (2020).
Schwaid, A. G. & Spencer, K. B. Strategies for Targeting the NLRP3 Inflammasome in the Clinical and Preclinical Space. J. Med. Chem. 64, 101–122 (2021).
Madurka, I. et al. DFV890: a new oral NLRP3 inhibitor-tested in an early phase 2a randomised clinical trial in patients with COVID-19 pneumonia and impaired respiratory function. Infection 51, 641–654 (2023).
Manayi, A. et al. Arglabin could target inflammasome-induced ARDS and cytokine storm associated with COVID-19. Mol. Biol. Rep. 48, 8221–8225 (2021).
Yue, Y., Jin, F. & Yue, X. The effect of Borago officinalis on the signaling pathway of the NLRP3 inflammasome complex, TLR4 and some inflammatory cytokines in type II diabetic patients with acute respiratory distress syndrome. Cell. Mol. Biol. 67, 178–183 (2021).
Saeedi-Boroujeni, A., Mahmoudian-Sani, M. R., Bahadoram, M. & Alghasi, A. COVID-19: A case for inhibiting NLRP3 inflammasome, suppression of inflammation with Curcumin? Basic Clin. Pharm. Toxicol. 128, 37–45 (2021).
Niu, X. et al. Tectoridin alleviates lipopolysaccharide-induced inflammation via inhibiting TLR4-NF-kappaB/NLRP3 signaling in vivo and in vitro. Immunopharmacol. Immunotoxicol. 44, 641–655 (2022).
Gao, Z. et al. Emodin protects against acute pancreatitis-associated lung injury by inhibiting NLPR3 Inflammasome activation via Nrf2/HO-1 signaling. Drug Des. Dev. Ther. 14, 1971–1982 (2020).
Shi, X. et al. HSF1 protects Sepsis-induced acute lung injury by inhibiting NLRP3 Inflammasome Activation. Front. Immunol. 13, 781003 (2022).
Zhang, Y. et al. Melatonin alleviates acute lung injury through inhibiting the NLRP3 inflammasome. J. Pineal Res. 60, 405–414 (2016).
Li, J. et al. A 4-Benzene-Indol derivative alleviates LPS-induced acute lung injury through inhibiting the NLRP3 inflammasome. Front Immunol. 13, 812164 (2022).
He, G. et al. Fudosteine attenuates acute lung injury in septic mice by inhibiting pyroptosis via the TXNIP/NLRP3/GSDMD pathway. Eur. J. Pharm. 926, 175047 (2022).
Meng, Q. et al. Nano-chemically modified Tetracycline-3 (nCMT-3) attenuates acute lung injury via blocking sTREM-1 release and NLRP3 Inflammasome activation. Shock 57, 749–758 (2022).
Yang, J. et al. Glibenclamide alleviates LPS-induced acute lung injury through NLRP3 Inflammasome signaling pathway. Mediators Inflamm. 2022, 8457010 (2022).
Pan, P. et al. FUNDC1 regulates autophagy by inhibiting ROS-NLRP3 signaling to avoid apoptosis in the lung in a Lipopolysaccharide-induced mouse model. Shock 56, 773–781 (2021).
Saeedi-Boroujeni, A. et al. Tranilast: a potential anti-Inflammatory and NLRP3 inflammasome inhibitor drug for COVID-19. Immunopharmacol. Immunotoxicol. 43, 247–258 (2021).
Wang, L., Lei, W., Zhang, S. & Yao, L. MCC950, a NLRP3 inhibitor, ameliorates lipopolysaccharide-induced lung inflammation in mice. Bioorg. Med. Chem. 30, 115954 (2021).
Ming, T. et al. Dexmedetomidine alleviates blunt chest trauma and hemorrhagic shock‑resuscitation‑induced acute lung injury through inhibiting the NLRP3 inflammasome. Mol. Med. Rep. 22, 2507–2515 (2020).
Wang, S. S., Yan, C. S. & Luo, J. M. NLRC4 gene silencing-dependent blockade of NOD-like receptor pathway inhibits inflammation, reduces proliferation and increases apoptosis of dendritic cells in mice with septic shock. Aging 13, 1440–1457 (2021).
Wang, F. et al. PIM2 deletion alleviates lipopolysaccharide (LPS)-induced respiratory distress syndrome (ARDS) by suppressing NLRP3 inflammasome. Biochem. Biophys. Res. Commun. 533, 1419–1426 (2020).
Li, Y. et al. Pirfenidone ameliorates lipopolysaccharide-induced pulmonary inflammation and fibrosis by blocking NLRP3 inflammasome activation. Mol. Immunol. 99, 134–144 (2018).
Long, F. et al. RBM3 is associated with acute lung injury in septic mice and patients via the NF-kappaB/NLRP3 pathway. Inflamm. Res. 72, 731–744 (2023).
Zhang, H. et al. Sivelestat sodium attenuates acute lung injury by inhibiting JNK/NF-kappaB and activating Nrf2/HO-1 signaling pathways. Biomol. Biomed. 23, 457–470 (2023).
Bernardo, L. R. et al. Milonine attenuates the lipopolysaccharide-induced acute lung injury in mice by modulating the Akt/NF-kappaB signaling pathways. Acad. Bras. Cienc. 94, e20211327 (2022).
Wang, S. et al. Allyl methyl trisulfide protected against LPS-induced acute lung injury in mice via inhibition of the NF-kappaB and MAPK pathways. Front. Pharm. 13, 919898 (2022).
Tung, Y. T. et al. Aspirin attenuates Hyperoxia-Induced Acute Respiratory Distress Syndrome (ARDS) by suppressing pulmonary inflammation via the NF-kappaB Signaling Pathway. Front Pharm. 12, 793107 (2021).
Gong, F. et al. OLFM4 regulates lung epithelial cell function in sepsis-associated ARDS/ALI via LDHA-Mediated NF-kappaB Signaling. J. Inflamm. Res. 14, 7035–7051 (2021).
Qian, H. et al. Andrographolide sulfonate attenuates alveolar hypercoagulation and fibrinolytic inhibition partly via NF-kappaB pathway in LPS-induced acute respiratory distress syndrome in mice. Biomed. Pharmacother. 143, 112209 (2021).
Tirunavalli, S. K. et al. Dehydrozingerone ameliorates Lipopolysaccharide induced acute respiratory distress syndrome by inhibiting cytokine storm, oxidative stress via modulating the MAPK/NF-kappaB pathway. Phytomedicine 92, 153729 (2021).
Xu, G. et al. Berberine administrated with different routes attenuates inhaled LPS-induced acute respiratory distress syndrome through TLR4/NF-kappaB and JAK2/STAT3 inhibition. Eur. J. Pharm. 908, 174349 (2021).
Liu, B. et al. Emodin improves alveolar hypercoagulation and inhibits pulmonary inflammation in LPS-provoked ARDS in mice via NF-kappaB inactivation. Int. Immunopharmacol. 88, 107020 (2020).
Wang, Q. et al. Gentiopicroside (GENT) protects against sepsis induced by lipopolysaccharide (LPS) through the NF-kappaB signaling pathway. Ann. Transl. Med. 7, 731 (2019).
Pooladanda, V. et al. Nimbolide protects against endotoxin-induced acute respiratory distress syndrome by inhibiting TNF-alpha mediated NF-kappaB and HDAC-3 nuclear translocation. Cell Death Dis. 10, 81 (2019).
Zhang, Q. et al. Euphorbia factor L2 alleviates lipopolysaccharide-induced acute lung injury and inflammation in mice through the suppression of NF-kappaB activation. Biochem. Pharm. 155, 444–454 (2018).
Jangam, A. et al. Anti-inflammatory and antioxidant activities of Gymnema Sylvestre extract rescue acute respiratory distress syndrome in rats via modulating the NF-kappaB/MAPK pathway. Inflammopharmacology 31, 823–844 (2023).
Jin, Y. et al. Osthole protects against acute lung injury by suppressing NF-kappaB-dependent inflammation. Mediators Inflamm. 2018, 4934592 (2018).
Kan, X. et al. Effect of Palrnatine on lipopolysaccharide-induced acute lung injury by inhibiting activation of the Akt/NF-kappaB pathway. J. Zhejiang Univ. Sci. B 22, 929–940 (2021).
Olajide, O. A. et al. Garcinia kola and garcinoic acid suppress SARS-CoV-2 spike glycoprotein S1-induced hyper-inflammation in human PBMCs through inhibition of NF-kappaB activation. Phytother. Res. 35, 6963–6973 (2021).
Olimpio, F., Carvalho, J., Kaminsky, V. & Aimbire, F. Lacticaseibacillus rhamnosus attenuates acute lung inflammation in a murine model of acute respiratory distress syndrome: Relevance to cytokines associated to STAT4/T-bet and STAT3/RORɣt. Micro. Pathog. 173, 105831 (2022).
Wang, Q. et al. MCTR1 enhances the resolution of lipopolysaccharide-induced lung injury through STAT6-mediated resident M2 alveolar macrophage polarization in mice. J. Cell Mol. Med. 24, 9646–9657 (2020).
Jin, H. et al. Surfactant protein C dampens inflammation by decreasing JAK/STAT activation during lung repair. Am. J. Physiol. Lung Cell Mol. Physiol. 314, L882–L892 (2018).
Zhao, J. et al. Protective effect of suppressing STAT3 activity in LPS-induced acute lung injury. Am. J. Physiol. Lung Cell Mol. Physiol. 311, L868–L880 (2016).
Namkoong, H. et al. Clarithromycin expands CD11b+Gr-1+ cells via the STAT3/Bv8 axis to ameliorate lethal endotoxic shock and post-influenza bacterial pneumonia. PLoS Pathog. 14, e1006955 (2018).
Li, C. et al. Losartan, a selective antagonist of AT1 receptor, attenuates seawater inhalation induced lung injury via modulating JAK2/STATs and apoptosis in rat. Pulm. Pharm. Ther. 45, 69–79 (2017).
Cui, Y. et al. MiR-29a-3p improves acute lung injury by reducing alveolar epithelial cell PANoptosis. Aging Dis. 13, 899–909 (2022).
Huang, Z. et al. MicroRNA-155-5p modulates the progression of acute respiratory distress syndrome by targeting interleukin receptors. Bioengineered 13, 11732–11741 (2022).
Li, J., Zeng, X. & Wang, W. miR-122-5p downregulation attenuates lipopolysaccharide-induced acute lung injury by targeting IL1. Rn. Exp. Ther. Med. 22, 1278 (2021).
He, B. et al. MicroRNA-574-5p attenuates acute respiratory distress syndrome by targeting HMGB1. Am. J. Respir. Cell Mol. Biol. 64, 196–207 (2021).
Li, P., Yao, Y., Ma, Y. & Chen, Y. MiR-30a-5p ameliorates LPS-induced inflammatory injury in human A549 cells and mice via targeting RUNX2. Innate Immun. 27, 41–49 (2021).
Meng, L., Cao, H., Wan, C. & Jiang, L. MiR-539-5p alleviates sepsis-induced acute lung injury by targeting ROCK1. Folia Histochem. Cytobiol. 57, 168–178 (2019).
Xi, X., Yao, Y., Liu, N. & Li, P. MiR-297 alleviates LPS-induced A549 cell and mice lung injury via targeting cyclin dependent kinase 8. Int. Immunopharmacol. 80, 106197 (2020).
Yuan, Z. et al. TREM-1-accentuated lung injury via miR-155 is inhibited by LP17 nanomedicine. Am. J. Physiol. Lung Cell Mol. Physiol. 310, L426–L438 (2016).
You, Q. et al. MiR-802 alleviates lipopolysaccharide-induced acute lung injury by targeting Peli2. Inflamm. Res 69, 75–85 (2020).
Liang, Y. et al. MiR-124-3p helps to protect against acute respiratory distress syndrome by targeting p65. Biosci Rep. 40, BSR20192132 (2020).
Khan, M. J. et al. Inhibition of miRNA-34a promotes M2 macrophage polarization and improves LPS-induced lung injury by targeting Klf4. Genes 11, 966 (2020).
Niemiec, S. M. et al. Lung function improves after delayed treatment with CNP-miR146a following acute lung injury. Nanomedicine 40, 102498 (2022).
Wang, Y. M. et al. Mucin 1 inhibits ferroptosis and sensitizes Vitamin E to alleviate sepsis-induced acute lung injury through GSK3beta/Keap1-Nrf2-GPX4 pathway. Oxid. Med Cell Longev. 2022, 2405943 (2022).
Wang, Y. et al. AUF1 protects against ferroptosis to alleviate sepsis-induced acute lung injury by regulating NRF2 and ATF3. Cell Mol. Life Sci. 79, 228 (2022).
Zhang, C., Zhao, Y. & Yang, X. Azilsartan attenuates lipopolysaccharide-induced acute lung injury via the Nrf2/HO-1 signaling pathway. Immunol. Res. 70, 97–105 (2022).
Liang, W. et al. Sulforaphane-dependent up-regulation of NRF2 activity alleviates both systemic inflammatory response and lung injury after Hemorrhagic Shock/Resuscitation in Mice. Shock 57, 221–229 (2022).
Yang, W. et al. Ramelteon protects against human pulmonary microvascular endothelial cell injury induced by lipopolysaccharide (LPS) via activating nuclear factor erythroid 2-related factor 2 (Nrf2)/heme oxygenase-1 (HO-1) pathway. Bioengineered 13, 1518–1529 (2022).
Liu, Z. et al. Dasatinib protects against acute respiratory distress syndrome via Nrf2-regulated M2 macrophages polarization. Drug Dev. Res. 82, 1247–1257 (2021).
Hou, L. et al. MitoQ alleviates LPS-mediated acute lung injury through regulating Nrf2/Drp1 pathway. Free Radic. Biol. Med. 165, 219–228 (2021).
Feng, G. et al. EphA2 antagonism alleviates LPS-induced acute lung injury via Nrf2/HO-1, TLR4/MyD88 and RhoA/ROCK pathways. Int. Immunopharmacol. 72, 176–185 (2019).
Yao, P., Zhang, Z. & Cao, J. Isorhapontigenin alleviates lipopolysaccharide-induced acute lung injury via modulating Nrf2 signaling. Respir. Physiol. Neurobiol. 289, 103667 (2021).
Lee, W. et al. Botanical formulation, TADIOS, alleviates lipopolysaccharide (LPS)-Induced acute lung injury in mice via modulation of the Nrf2-HO-1 signaling pathway. J. Ethnopharmacol. 270, 113795 (2021).
Li, J. et al. Panaxydol attenuates ferroptosis against LPS-induced acute lung injury in mice by Keap1-Nrf2/HO-1 pathway. J. Transl. Med. 19, 96 (2021).
Patangrao Renushe, A. et al. Vincamine, an active constituent of Vinca rosea ameliorates experimentally induced acute lung injury in Swiss albino mice through modulation of Nrf-2/NF-kappaB signaling cascade. Int Immunopharmacol. 108, 108773 (2022).
Deng, Y. X. et al. Active ingredients targeting Nrf2 in the Mongolian medicine Qiwei Putao powder: Systematic pharmacological prediction and validation for chronic obstructive pulmonary disease treatment. J. Ethnopharmacol. 265, 113385 (2021).
Quach, H. T. et al. Allantopyrone A interferes with multiple components of the TNF receptor 1 complex and blocks RIP1 modifications in the TNF-alpha-induced signaling pathway. J. Antibiot. 70, 929–936 (2017).
Wilson, M. R. et al. Inhibition of TNF Receptor p55 By a domain antibody attenuates the initial phase of acid-induced lung injury in mice. Front Immunol. 8, 128 (2017).
Patel, S. et al. HJP272, a novel endothelin receptor antagonist, attenuates lipopolysaccharide-induced acute lung injury in hamsters. Lung 192, 803–810 (2014).
Malleo, G. et al. Etanercept reduces acute tissue injury and mortality associated to zymosan-induced multiple organ dysfunction syndrome. Shock 29, 560–571 (2008).
Zhang, Z. T. et al. Dexmedetomidine alleviates acute lung injury by promoting Tregs differentiation via activation of AMPK/SIRT1 pathway. Inflammopharmacology 31, 423–438 (2023).
Xu, S. et al. Melatonin attenuates sepsis-induced small-intestine injury by upregulating SIRT3-mediated oxidative-stress inhibition, mitochondrial protection, and autophagy induction. Front Immunol. 12, 625627 (2021).
Gong, Q. et al. DL-3-n-butylphthalide attenuates lipopolysaccharide-induced acute lung injury via SIRT1-dependent and -independent regulation of Nrf2. Int. Immunopharmacol. 74, 105658 (2019).
Yu-Wung Yeh, D. & Wang, J. J. Curcumin attenuates hemorrhagic shock and blood replenish resuscitation-induced impairment of pulmonary barrier function by increasing SIRT1 and reducing Malondialdehyde and TNF-alpha contents and neutrophil infiltration in lung in a dose-dependent fashion. Transpl. Proc. 52, 1875–1879 (2020).
Quan, M. et al. Tanshinone IIA protects against lipopolysaccharide-induced lung injury through targeting Sirt1. J. Pharm. Pharm. 71, 1142–1151 (2019).
Yang, X. et al. Hydroxytyrosol attenuates LPS-induced acute lung injury in mice by regulating autophagy and Sirtuin Expression. Curr. Mol. Med. 17, 149–159 (2017).
Xu, W. et al. Novel role of resveratrol: suppression of high-mobility group protein box 1 nucleocytoplasmic translocation by the upregulation of sirtuin 1 in sepsis-induced liver injury. Shock 42, 440–447 (2014).
Tsai, Y. F. et al. Carnosic acid inhibits reactive oxygen species-dependent neutrophil extracellular trap formation and ameliorates acute respiratory distress syndrome. Life Sci. 321, 121334 (2023).
Baron, S. et al. Selinexor, a selective inhibitor of nuclear export, inhibits human neutrophil extracellular trap formation in vitro. Front. Pharm. 13, 1030991 (2022).
Pan, W. H. et al. The Effect and Mechanism of Lipoxin A4 on Neutrophil Function in LPS-Induced Lung Injury. Inflammation 45, 1950–1967 (2022).
de Oliveira, G. P. et al. Glutamine therapy reduces inflammation and extracellular trap release in experimental acute respiratory distress syndrome of pulmonary origin. Nutrients 11, 831 (2019).
Chang, Y. W. et al. beta-Nitrostyrene derivatives attenuate LPS-mediated acute lung injury via the inhibition of neutrophil-platelet interactions and NET release. Am. J. Physiol. Lung Cell Mol. Physiol. 314, L654–L669 (2018).
Shang, T. et al. Xuebijing injection inhibited neutrophil extracellular traps to reverse lung injury in sepsis mice via reducing Gasdermin D. Front. Pharm. 13, 1054176 (2022).
Liu, Q. et al. Salvianolic Acid A protects against Lipopolysaccharide-induced acute lung injury by inhibiting Neutrophil NETosis. Oxid. Med. Cell Longev. 2022, 7411824 (2022).
Kao, T. I. et al. Bletinib ameliorates neutrophilic inflammation and lung injury by inhibiting Src family kinase phosphorylation and activity. Br. J. Pharm. 178, 4069–4084 (2021).
Yang, C. et al. Re-Du-Ning injection ameliorates LPS-induced lung injury through inhibiting neutrophil extracellular traps formation. Phytomedicine 90, 153635 (2021).
Gu, Z. et al. Polydatin alleviates severe traumatic brain injury induced acute lung injury by inhibiting S100B mediated NETs formation. Int. Immunopharmacol. 98, 107699 (2021).
Shah, F. A. et al. A research agenda for precision medicine in sepsis and acute respiratory distress syndrome: An Official American Thoracic Society Research Statement. Am. J. Respir. Crit. Care Med. 204, 891–901 (2021).
Ball, L., Silva, P. L., Rocco, P. R. M. & Pelosi, P. A critical approach to personalised medicine in ARDS. Lancet Respir. Med. 8, 218–219 (2020).
Reddy, K., Hardin, C. C. & McAuley, D. F. COVID-19-related Acute Respiratory Distress Syndrome Subphenotypes and differential response to Corticosteroids: Time for more precision? Am. J. Respir. Crit. Care Med. 204, 1241–1243 (2021).
Zhang, H., Li, Y. & Slutsky, A. S. Precision medicine for cell therapy in acute respiratory distress syndrome. Lancet Respir. Med. 7, e13 (2019).
Constantin, J. M. et al. Personalised mechanical ventilation tailored to lung morphology versus low positive end-expiratory pressure for patients with acute respiratory distress syndrome in France (the LIVE study): a multicentre, single-blind, randomised controlled trial. Lancet Respir. Med. 7, 870–880 (2019).
Goligher, E. C. et al. Effect of Lowering Vt on mortality in acute respiratory distress syndrome varies with respiratory system elastance. Am. J. Respir. Crit. Care Med. 203, 1378–1385 (2021).
Sarge, T. et al. Effect of Esophageal pressure-guided positive end-expiratory pressure on survival from acute respiratory distress syndrome: a risk-based and mechanistic reanalysis of the EPVent-2 Trial. Am. J. Respir. Crit. Care Med. 204, 1153–1163 (2021).
Xiao, D. et al. Could SARS-CoV-2-induced lung injury be attenuated by vitamin D? Int. J. Infect. Dis. 102, 196–202 (2021).
Fowler, A. A. et al. Effect of Vitamin C infusion on organ failure and biomarkers of inflammation and vascular injury in patients with sepsis and severe acute respiratory failure: The CITRIS-ALI randomized clinical trial. JAMA 322, 1261–1270 (2019).
Okamoto, H. et al. Recombinant Antithrombin attenuates acute respiratory distress syndrome in experimental Endotoxemia. Am. J. Pathol. 191, 1526–1536 (2021).
Suzuki, K. et al. Recombinant thrombomodulin protects against LPS-induced acute respiratory distress syndrome via preservation of pulmonary endothelial glycocalyx. Br. J. Pharm. 177, 4021–4033 (2020).
Brannon, E. R. et al. Polysalicylic acid polymer microparticle decoys therapeutically treat acute respiratory distress syndrome. Adv. Health. Mater. 11, e2101534 (2022).
Zhang, D. et al. Crocin alleviates lipopolysaccharide-induced acute respiratory distress syndrome by protecting against glycocalyx damage and suppressing inflammatory signaling pathways. Inflamm. Res. 69, 267–278 (2020).
Li, Q. et al. Oral IRAK4 inhibitor BAY-1834845 prevents acute respiratory distress syndrome. Biomed. Pharmacother. 153, 113459 (2022).
Xian, H. et al. Metformin inhibition of mitochondrial ATP and DNA synthesis abrogates NLRP3 inflammasome activation and pulmonary inflammation. Immunity 54, 1463–1477, e1411 (2021).
Wang, K. et al. Fluorous-tagged peptide nanoparticles ameliorate acute lung injury via lysosomal stabilization and inflammation inhibition in pulmonary macrophages. Small 18, e2203432 (2022).
Murphy, E. J. et al. Immunomodulatory activity of beta-glucan polysaccharides isolated from different species of mushroom - A potential treatment for inflammatory lung conditions. Sci. Total Environ. 809, 152177 (2022).
Arber Raviv, S. et al. Lung targeted liposomes for treating ARDS. J. Control Rel. 346, 421–433 (2022).
Kotta, S. et al. Lung targeted lipopolymeric microspheres of Dexamethasone for the treatment of ARDS. Pharmaceutics 13, 1347 (2021).
Muhammad, W. et al. ROS-responsive polymer nanoparticles with enhanced loading of dexamethasone effectively modulate the lung injury microenvironment. Acta Biomater. 148, 258–270 (2022).
Mertes, P. M. et al. Liposomal encapsulation of trans-crocetin enhances oxygenation in patients with COVID-19-related ARDS receiving mechanical ventilation. J. Control Release 336, 252–261 (2021).
Gao, W. et al. Size-dependent anti-inflammatory activity of a peptide-gold nanoparticle hybrid in vitro and in a mouse model of acute lung injury. Acta Biomater. 85, 203–217 (2019).
Constantin, J. M. et al. Lung morphology predicts response to recruitment maneuver in patients with acute respiratory distress syndrome. Crit. Care Med. 38, 1108–1117 (2010).
Mrozek, S. et al. Elevated Plasma Levels of sRAGE are associated with nonfocal CT-based lung imaging in patients with ARDS: A prospective multicenter study. Chest 150, 998–1007 (2016).
Wendel Garcia, P. D. et al. Latent class analysis to predict intensive care outcomes in Acute Respiratory Distress Syndrome: a proposal of two pulmonary phenotypes. Crit. Care 25, 154 (2021).
Scaramuzzo, G. et al. Gravitational distribution of regional opening and closing pressures, hysteresis and atelectrauma in ARDS evaluated by electrical impedance tomography. Crit. Care 24, 622 (2020).
Famous, K. R. et al. Acute respiratory distress syndrome subphenotypes respond differently to randomized fluid management strategy. Am. J. Respir. Crit. Care Med. 195, 331–338 (2017).
Sinha, P. et al. Latent class analysis of ARDS subphenotypes: a secondary analysis of the statins for acutely injured lungs from sepsis (SAILS) study. Intensive Care Med. 44, 1859–1869 (2018).
Acknowledgements
Figures are created with BioRender.com. We thank Yarong He and Haifang Yu for their valuable insights and suggestions. This work is supported by the Technological Innovation 2030-Major Project for the Prevention and Control of Cancer, Cardiovascular and Cerebrovascular Diseases, Respiratory Diseases, and Metabolic Diseases (2024ZD0520200/2024ZD0520204), Development Center for Medical Science & Technology, National Health Commission of the People’s Republic of China; the National Natural Science Foundation of China (82241060, 82272241, 82270392, 82402574); 1.3.5 Project for Disciplines of Excellence (ZYYC23008; ZYGD23035); Center of Excellence•International Cooperation Initiative Grant (139170032); China Postdoctoral Science Foundation (2023M732462); and by Projects of Sichuan Provincial Department of Science and Technology (2023ZYD0094).
Author information
Authors and Affiliations
Contributions
Wen Ma, Songling Tang, and Peng Yao reviewed the literature and made initial draft preparation; Tingyuan Zhou and Peng Liu designed and summarized the tables; Shiyuan Tang and Qingsheng Niu designed and drew the figures; Yao Chen reviewed the literature; Lu Gan and Yu Cao designed the outline and revised the manuscript. All authors have read and approved the article.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no competing interests. Yu Cao is the editorial board member of Signal Transduction and Targeted Therapy, but she has not been involved in the process of manuscript handling.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ma, W., Tang, S., Yao, P. et al. Advances in acute respiratory distress syndrome: focusing on heterogeneity, pathophysiology, and therapeutic strategies. Sig Transduct Target Ther 10, 75 (2025). https://doi.org/10.1038/s41392-025-02127-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41392-025-02127-9