Abstract
Background
Variants in CRX are associated with dominantly inherited retinopathy with considerable phenotypic variability. Many patients have central retinal degeneration; in some patients, we have observed an additional focus of degeneration in the nasal retina. This study explores this phenotypic association amongst patients with CRX-associated disease.
Methods
A retrospective review was conducted for all patients with dominant CRX-associated retinopathy at two UK centres. Analysis focused on patients with available ultra-widefield autofluorescence imaging and aimed to identify those with a specific bifocal degeneration pattern involving the nasal retina in both eyes.
Results
Sixty patients were identified, with ultra-widefield fundus imaging available for 50 patients. Of these, six male patients aged 26–74 years displayed a distinct pattern characterised by central retinal degeneration and an additional discrete area of altered autofluorescence in the nasal periphery. Pattern and full-field ERGs indicated macular dysfunction in all 6 cases, with generalised cone (n = 2) or cone and rod (n = 4) system involvement, with a locus that appeared to be post-phototransduction. The CRX variants found in these patients included missense variants (n = 2), frameshifting variants (n = 3), and a CRX whole gene deletion (n = 1), with no clear genotype-phenotype correlation identified.
Conclusions
We report a distinct pattern of bifocal retinal degeneration in some cases of CRX-associated retinopathy (12% in our cohort), not typically seen in other forms of inherited retinal disease. Recognising such phenotypes can guide genetic investigations or their interpretation, facilitating molecular diagnoses for effective family counselling, given the autosomal dominant inheritance and phenotypic variability of CRX-associated retinopathy.
Similar content being viewed by others
Introduction
The cone rod homeobox-containing gene (CRX; MIM *602225), located on chromosome 19q13.33, encodes a transcription factor essential for both photoreceptor development and survival [1,2,3]. Pathogenic CRX variants are associated with a range of retinal dystrophy phenotypes, including macular dystrophy [4], cone-rod dystrophy (MIM #120970) and Leber congenital amaurosis (MIM #613829) [5]. Over 150 disease-causing CRX variants have been reported, including missense, nonsense, frameshift and splice site variants, as well as multi-exon and whole gene deletions (The Human Gene Mutation Database® Professional 2023.4, accessed on 28 March 2024), most commonly causing dominant disease. In rare cases, biallelic variants in CRX have been reported in association with autosomal recessive Leber congenital amaurosis [6].
Dominant CRX-associated retinopathy exhibits considerable phenotypic variability, even within families sharing the same mutant CRX allele. Degeneration affecting the central or paracentral retina tends to be a consistent feature, with variable degrees of wider retinal involvement. In some patients, we have observed an additional, non-contiguous focus of degeneration in the nasal retina. This study aims to describe this previously unreported association in a series of patients with dominant CRX-associated retinopathy, and to explore the prevalence of such a pattern.
Methods
A retrospective review was conducted for all patients with molecularly confirmed CRX-associated retinopathy at two centres in London: Moorfields Eye Hospital and St Thomas’ Hospital. Analysis focused on patients with available ultra-widefield pseudocolour and autofluorescence imaging (Optos plc, Dunfermline, UK), and those with the specific bifocal degeneration pattern (with an additional locus in nasal retina) in both eyes were identified. Additional information collected included demographic data and molecular diagnosis from electronic patient records, and spectral-domain optical coherence tomography (SD-OCT; Heidelberg Spectralis, Heidelberg, Germany).
Visual electrophysiology performed for all 6 patients included dark-adapted (DA) and light-adapted (LA) full-field electroretinogram (ERG) and pattern electroretinogram (PERG) testing, incorporating the International Society for Clinical Electrophysiology of Vision (ISCEV) standards [7, 8], using gold foil corneal recording electrodes. Full-field ERGs were used to assess generalised rod and cone system function and pattern ERG P50 was used to assess macular function [9]. The ERG data were compared with a reference range from a group of healthy subjects (age range: 10–79 years) [10, 11]. The amplitudes of the main ISCEV Standard ERG components and b-wave to a-wave amplitude ratios were plotted as a percentage of the age-matched lower limit (5th percentile) of the reference range. Peak times were assessed as a difference from the age-matched upper limit (95th percentile) of the reference range.
The overall sex ratio in the CRX patient cohort was evaluated using a chi-square test. Fisher’s exact test was used to assess whether the occurrence of nasal degeneration was significantly associated with sex. Statistical significance was considered at a p-value of <0.05.
This study adhered to the tenets of the Declaration of Helsinki and received relevant local research ethics approval (Moorfields Eye Hospital and the Northwest London research ethics committee; 12/LO/0141). Written informed consent for genetic testing was obtained from all participating individuals.
Results
60 patients with molecularly confirmed CRX-associated retinopathy from 45 families were identified. In all cases, this was linked to heterozygous CRX variants causing dominant disease; no individuals with biallelic CRX variants causing autosomal recessive disease were identified in our patient cohort. Ultra-widefield pseudocolour and autofluorescence imaging was available for 50 patients. Among these, six patients (12%), all male, displayed a distinct pattern consisting of central retinal degeneration (involving the macula or posterior pole), along with an additional area of discrete abnormality in the nasal periphery with altered autofluorescence characteristics, which was non-contiguous with the macular degeneration, and which affected a similar location in both eyes (Fig. 1). This nasal degeneration was more pronounced on autofluorescence imaging compared to clinical examination and ultra-widefield pseudocolour imaging (Fig. 2). Patient characteristics and genetic findings for these six individuals are summarised in Table 1 (with variants classified according to the American College of Medical Genetics and Genomics (ACMG) variant classification guidelines)[12].
The non-contiguous nasal retinal degeneration is identifiable by an area of pigmentary alteration and pigment spicules in patients 5 and 6, but is not clearly discernible in patients 1–4. The yellow asterisk marking the area of nasal degeneration is positioned consistently in both Figs. 1, 2 for comparison.
Figure 3 depicts macular SD-OCT findings in all 6 patients; in one patient (Patient 5), SD-OCT imaging was also performed through the nasal area of retinal degeneration and showed loss of retinal structure and lamination throughout this region.
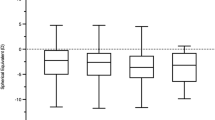
There was a high degree of inter-ocular ERG symmetry based on the ISCEV Standard DA 0.01, DA 10 ERG a- and b-waves, LA 30 Hz ERG and LA 3 (single flash) ERG a- and b-wave amplitudes (slope = 0.94; r2 = 0.97) and peak times (slope = 0.99; r2 = 0.99).
The PERG P50 and full-field ERG findings and patient ages at the time of testing are summarised in Fig. 4. PERG P50 was bilaterally subnormal in all cases, including 5 of 6 with bilaterally undetectable responses, consistent with severe macular dysfunction. Comparison of DA and LA ERGs (summarised in Fig. 4) revealed generalised retinal involvement confined to the cone system (n = 2), cone more than rod system dysfunction (n = 3) or similar severity of cone and rod system involvement (n = 1; subject 4). The DA 10 ERG b-waves were markedly delayed in 4 of 6 cases, including one with additional a-wave delay (patient 1); the LA ERGs showed relatively mild (n = 3) or borderline (n = 2) delay or were of normal timing (n = 1). The LA 3 (single flash) ERG b:a ratio was subnormal in 5 cases, and the DA 10 ERG b:a ratio subnormal in 4, in keeping with a possible locus of dysfunction post-phototransduction. In two of those with a low DA10 ERG b:a ratio, there was additional moderate (n = 1; patient 1) or mild (n = 1; patient 4) a-wave reduction, consistent with additional rod photoreceptor involvement.
Pattern and full-field ERG findings summarised in patients 1–6 tested according to ISCEV standard methods. A The amplitudes of the DA0.01 ERG, DA 10 ERG a- and b-waves, LA 30 Hz ERG and LA 3 ERG a- and b-wave are plotted as a percentage of the age-matched 5th percentile of the (“normal”) reference range. B The peak times of the main ERG components are plotted as a difference compared with the 95th percentile of the reference range. C The DA10 ERG and LA3 ERG b:a ratios are compared with age-associated reference values specific to the stimulus system used (5th percentiles of b:a ratio 1.1–1.2 for the DA10 ERGs; 2.9–3.1 for the LA3 ERGs). Broken lines indicate the limits of normality. Note that subject-specific values for the DA 10 ERG b-waves in (A) and (B) are plotted slightly laterally for clarity.
Discussion
In this study, we present data from six patients with CRX-associated retinopathy in whom a bifocal pattern of degeneration was discernible in both eyes: in each eye, there was a discrete area of altered autofluorescence in the nasal periphery that was not contiguous with the degeneration affecting the central retina. Bifocal retinal lesions have been described in progressive bifocal chorioretinal atrophy, a rare, early-onset chorioretinal dystrophy linked to a non-coding variant upstream of PDRM13 [13]. Our findings show that a proportion of patients with CRX-associated retinopathy (12% in our study) also exhibit bifocal areas of retinal degeneration, albeit with a distinct appearance. Electrophysiology was consistent with a cone or cone-rod pattern of dysfunction, with a possible locus that was post-phototransduction (Fig. 4c), as has been previously reported in CRX-associated disease [14,15,16].
The precise mechanism underlying this discrete nasal retinal degeneration remains uncertain. Some forms of inherited retinal disease show sectoral retinal pigmentary changes with a predilection for inferior and nasal involvement; this phenomenon is commonly associated with pathogenic RHO variants but has also been noted in connection with other genes [17]. In these cases, given the inferior retinal predilection, light exposure has been proposed as a contributing factor. It has also been hypothesised that gradients of gene expression in the retina may predispose certain retinal quadrants differently; further investigation is warranted to explore these potential mechanisms.
Interestingly, while the sex ratio with our overall CRX patient cohort is not significantly skewed (34 male 26 female; p > 0.05), it is notable that all six patients identified with nasal degeneration in our study were male (p = 0.031). Significant sex imbalances have been observed in certain autosomally-inherited macular dystrophies (such as those associated with ABCA4, BEST1 and EFEMP1),[18, 19] although the underlying mechanisms remain unclear. Messenger RNAs for oestrogen, progesterone, and androgen receptors have been detected in retinal cells [20, 21], and it may be that sex-specific hormonal differences may act as modifying factors influencing disease presentation.
We did not observe a specific genotype-phenotype correlation in our study; the presence of nasal degeneration did not correlate with any variant type, and was seen across ethnicities. Among the six patients in our series, a spectrum of disease variants was identified; two had missense variants, three had frameshift variants, and one harboured a large multi-gene deletion involving CRX, TPRX1 and SULT2A1 (Table 1). This deletion has recently been associated with a dominant late-onset macular disease [4], although none of the 8 patients reported in that study showed signs of nasal degeneration. Intra-familial variability was also observed; in one case (Patient 1), both the affected sister and father, despite sharing the same CRX disease allele, did not exhibit any signs of nasal degeneration, suggesting the potential influence of trans-acting or environmental modifiers.
Several limitations of our study should be acknowledged. The prevalence estimate should be interpreted in light of the small cohort size, reflecting the rarity of CRX-associated retinopathy. It is possible that some patients who did not initially exhibit nasal degeneration may go on to develop this over time; however, given that this feature was absent in some individuals with long disease durations exceeding 20 years, it does not appear to be an inevitable development in all cases of dominant CRX-associated retinopathy. Additionally, some patients have been noted to have areas of nasal degeneration that were contiguous with the more central degeneration; it is possible that these areas were previously non-contiguous and later became confluent over time. Furthermore, OCT imaging of the nasal retina is not routinely performed, and it is possible that some patients may have had nasal degeneration detectable by OCT, but not by autofluorescence imaging. Finally, OCT imaging through the nasal area of retinal degeneration was only available for one of the six patients in the study, and it remains uncertain if the OCT findings will be replicated in the other cases; future studies could investigate this more systematically.
There have been significant advances in genomic testing for inherited retinal disease in the UK, due to the success of initiatives including the 100,000 Genomes Project and, more recently, the NHS Genomic Medicine Service [22, 23]. Despite this progress, achieving a molecular diagnosis remains challenging, with 40–50% of cases remaining unresolved [24, 25], due in part to difficulties with variant identification and interpretation. Recognising distinctive phenotypes, such as the distinct pattern of nasal degeneration observed in some cases of CRX-associated retinal disease, which is not typically seen in other forms of inherited retinal disease, is important. This can aid in guiding genetic investigations and facilitate the identification of potentially pathogenic gene variants associated with specific phenotypic presentations. Given the autosomal dominant inheritance and phenotypic variability characteristic of CRX-associated retinopathy, obtaining a molecular diagnosis is particularly important for effective family counselling and access to emerging therapies [26, 27].
Summary
What was known before
-
Pathogenic CRX variants are associated with various retinal dystrophy phenotypes, including macular dystrophy, cone-rod dystrophy, and Leber congenital amaurosis.
-
Dominant CRX-associated retinopathy displays significant phenotypic variability.
What this study adds
-
A proportion of patients with CRX-associated retinopathy (12% in this study) exhibit bifocal areas of retinal degeneration, consisting of central retinal degeneration along with an additional discrete non-contiguous affected area in the nasal periphery with altered autofluorescence characteristics. This distinct pattern is not typically seen in other forms of inherited retinal disease.
-
Recognising distinct phenotypes can guide interpretation of genetic data towards potentially pathogenic variants in genes associated with the specific phenotypic presentation, facilitating personalised clinical care.
Data availability
Data supporting the findings of this study are available from the study authors on request.
References
Chen S, Wang QL, Nie Z, Sun H, Lennon G, Copeland NG, et al. Crx, a novel Otx-like paired-homeodomain protein, binds to and transactivates photoreceptor cell-specific genes. Neuron. 1997;19:1017–30.
Furukawa T, Morrow EM, Cepko CL. Crx, a novel otx-like homeobox gene, shows photoreceptor-specific expression and regulates photoreceptor differentiation. Cell. 1997;91:531–41.
Freund CL, Gregory-Evans CY, Furukawa T, Papaioannou M, Looser J, Ploder L, et al. Cone-rod dystrophy due to mutations in a novel photoreceptor-specific homeobox gene (CRX) essential for maintenance of the photoreceptor. Cell. 1997;91:543–53.
Yahya S, Smith CEL, Poulter JA, McKibbin M, Arno G, Ellingford J, et al. Late-onset autosomal dominant macular degeneration caused by deletion of the CRX gene. Ophthalmology. 2023;130:68–76.
Hull S, Arno G, Plagnol V, Chamney S, Russell-Eggitt I, Thompson D, et al. The phenotypic variability of retinal dystrophies associated with mutations in CRX, with report of a novel macular dystrophy phenotype. Investig Ophthalmol Vis Sci. 2014;55:6934–44.
Swaroop A, Wang QL, Wu W, Cook J, Coats C, Xu S, et al. Leber congenital amaurosis caused by a homozygous mutation (R90W) in the homeodomain of the retinal transcription factor CRX: direct evidence for the involvement of CRX in the development of photoreceptor function. Hum Mol Genet. 1999;8:299–305.
Robson AG, Frishman LJ, Grigg J, Hamilton R, Jeffrey BG, Kondo M, et al. ISCEV standard for full-field clinical electroretinography (2022 update). Doc Ophthalmol. 2022;144:165–77.
Thompson DA, Bach M, McAnany JJ, Šuštar Habjan M, Viswanathan S, Robson AG. ISCEV standard for clinical pattern electroretinography (2024 update). Doc Ophthalmol. 2024;148:75–85.
Robson AG, Nilsson J, Li S, Jalali S, Fulton AB, Tormene AP, et al. ISCEV guide to visual electrodiagnostic procedures. Doc Ophthalmol. 2018;136:1–26.
de Carvalho ER, Robson AG, Arno G, Boon CJF, Webster AA, Michaelides M. Enhanced S-cone syndrome: spectrum of clinical, imaging, electrophysiologic, and genetic findings in a retrospective case series of 56 patients. Ophthalmol Retin. 2021;5:195–214.
Georgiou M, Fujinami K, Vincent A, Nasser F, Khateb S, Vargas ME, et al. KCNV2-associated retinopathy: detailed retinal phenotype and structural endpoints-KCNV2 study group report 2. Am J Ophthalmol. 2021;230:1–11.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–23.
Silva RS, Arno G, Cipriani V, Pontikos N, Defoort-Dhellemmes S, Kalhoro A, et al. Unique noncoding variants upstream of PRDM13 are associated with a spectrum of developmental retinal dystrophies including progressive bifocal chorioretinal atrophy. Hum Mutat. 2019;40:578–87.
Nasser F, Kurtenbach A, Kohl S, Obermaier C, Stingl K, Zrenner E. Retinal dystrophies with bull’s-eye maculopathy along with negative ERGs. Doc Ophthalmol. 2019;139:45–57.
Nishiguchi KM, Kunikata H, Fujita K, Hashimoto K, Koyanagi Y, Akiyama M, et al. Association of CRX genotypes and retinal phenotypes confounded by variable expressivity and electronegative electroretinogram. Clin Exp Ophthalmol. 2020;48:644–57.
Jiang X, Mahroo OA. Negative electroretinograms: genetic and acquired causes, diagnostic approaches and physiological insights. Eye. 2021;35:2419–37.
Georgiou M, Grewal PS, Narayan A, Alser M, Ali N, Fujinami K, et al. Sector retinitis pigmentosa: extending the molecular genetics basis and elucidating the natural history. Am J Ophthalmol. 2021;221:299–310.
Cornelis SS, IntHout J, Runhart EH, Grunewald O, Lin S, Corradi Z, et al. Representation of women among individuals with mild variants in ABCA4-associated retinopathy: a meta-analysis. JAMA Ophthalmol. 2024;42:463–71.
Mishra AV, Vermeirsch S, Lin S, Martin-Gutierrez MP, Simcoe M, Pontikos N, et al. Sex distributions in Non-ABCA4 autosomal macular dystrophies. Investig Ophthalmol Vis Sci. 2024;65:9.
Marin-Castaño ME, Elliot SJ, Potier M, Karl M, Striker LJ, Striker GE, et al. Regulation of estrogen receptors and MMP-2 expression by estrogens in human retinal pigment epithelium. Investig Ophthalmol Vis Sci. 2003;44:50–9.
Wickham LA, Gao J, Toda I, Rocha EM, Ono M, Sullivan DA. Identification of androgen, estrogen and progesterone receptor mRNAs in the eye. Acta Ophthalmol Scand. 2000;78:146–53.
Turnbull C, Scott RH, Thomas E, Jones L, Murugaesu N, Pretty FB, et al. The 100,000 Genomes Project: bringing whole genome sequencing to the NHS. BMJ. 2018;361:k1687.
Barwell J, Snape K, Wedderburn S. The new genomic medicine service and implications for patients. Clin Med. 2019;19:273–7.
100000 Genomes Project Pilot Investigators, Smedley D, Smith KR, Martin A, Thomas EA, McDonagh EM, et al. 100,000 genomes pilot on rare-disease diagnosis in health care—preliminary report. N Engl J Med. 2021;385:1868–80.
Carss KJ, Arno G, Erwood M, Stephens J, Sanchis-Juan A, Hull S, et al. Comprehensive rare variant analysis via whole-genome sequencing to determine the molecular pathology of inherited retinal disease. Am J Hum Genet. 2016;100:75–90.
Kruczek K, Qu Z, Gentry J, Fadl BR, Gieser L, Hiriyanna S, et al. Gene therapy of dominant CRX-leber congenital amaurosis using patient stem cell-derived retinal organoids. Stem Cell Rep. 2021;16:252–63.
Sun C, Chen S. Gene augmentation for autosomal dominant CRX-associated retinopathies. Adv Exp Med Biol. 2023;1415:135–41.
Funding
Supported by the Wellcome Trust (grant nos.: 206619/Z/17/Z [OM] and 205174/Z/16/Z [MM]); Fight for Sight UK (Early Career Investigator Award, grant no. 5045/46, GA); the National Institute of Health Research Biomedical Research Centre (NIHR-BRC) at Moorfields Eye Hospital and UCL Institute of Ophthalmology (grant no NIHR203322, AGR); the Moorfields Eye Charity (Conference Grant, no. GR001560, SL), and Steven and Elizabeth Archer in memory of Marion Woods (GA). The funding organisations had no role in the design or conduct of this research. The views expressed are those of the author(s) and not necessarily those of the funding organisations.
Author information
Authors and Affiliations
Contributions
Conception and design: OAM, SL. Data collection: SL, AGR, MMoh, OAM. Analysis and interpretation: All authors. Writing— original draft preparation: SL, OAM. Writing—review and editing: All authors. Supervision and overall responsibility: OAM, ARW, GA, MMic.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lin, S., Arno, G., Robson, A.G. et al. Bifocal retinal degeneration observed on ultra-widefield autofluorescence in some cases of CRX-associated retinopathy. Eye 39, 951–957 (2025). https://doi.org/10.1038/s41433-024-03522-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-024-03522-2