Abstract
Seasonal epidemics of influenza viruses are responsible for a significant global public health burden. Vaccination remains the most effective way to prevent infection; however, due to the persistence of antigenic drift, vaccines must be updated annually. The selection of vaccine strains occurs months in advance of the influenza season to allow adequate time for production in eggs. RNA vaccines offer the potential to accelerate production and improve efficacy of influenza vaccines. We leveraged the nucleoside-modified RNA (modRNA) platform technology and lipid nanoparticle formulation process of the COVID-19 mRNA vaccine (BNT162b2; Comirnaty®) to create modRNA vaccines encoding hemagglutinin (HA) (modRNA-HA) for seasonal human influenza strains and evaluated their preclinical immunogenicity and toxicity. In mice, a monovalent modRNA vaccine encoding an H1 HA demonstrated robust antibody responses, HA-specific Th1-type CD4+ T cell responses, and HA-specific CD8+ T cell responses. In rhesus and cynomolgus macaques, the vaccine exhibited durable functional antibody responses and HA-specific IFN-γ+ CD4+ T cell responses. Immunization of mice with monovalent, trivalent, and quadrivalent modRNA-HA vaccines generated functional antibody responses targeting the seasonal influenza virus(es) encoded in the vaccines that were greater than, or similar to, those of a licensed quadrivalent influenza vaccine. Monovalent and quadrivalent modRNA-HA vaccines were well-tolerated by Wistar Han rats, with no evidence of systemic toxicity. These nonclinical immunogenicity and safety data support further evaluation of the modRNA-HA vaccines in clinical studies.
Similar content being viewed by others
Introduction
Influenza is a serious viral respiratory illness responsible for annual epidemics that result in significant morbidity and mortality worldwide1,2. In the United States, the Centers for Disease Control and Prevention (CDC) estimates that influenza epidemics have resulted in 9.4 to 41 million illnesses, 100,000 to 710,000 hospitalizations, and 4900 to 52,000 deaths annually between 2010 and 20223. Vaccination is the foremost public health strategy to combat the annual disease burden and economic costs associated with seasonal influenza4,5. Licensed seasonal influenza vaccines target up to four influenza strains: two influenza A subtypes (H1N1 and H3N2) and two influenza B lineages (B/Yamagata and B/Victoria). The World Health Organization (WHO) and the United States Food and Drug Administration’s (FDA) Vaccines and Related Biological Products Advisory Committee (VRBPAC) recently recommended the removal of the B/Yamagata lineage from seasonal influenza vaccines due to the lack of recent circulation of these viruses6,7
Influenza hemagglutinin (HA) is the most abundant glycoprotein on the surface of influenza A and B viruses (IAV and IBV, respectively). The HA protein is responsible for recognition and attachment of the virus to sialic acid receptors and mediating virus entry into host cells8. Thus, HA is a major target of virus neutralizing antibodies and is a key antigen for influenza vaccine development. Small changes can occur in the influenza virus genome over time which lead to changes in the HA surface protein, known as antigenic drift. Annual updates to seasonal influenza vaccines are necessary to improve immune responses to new antigenic variants that have emerged since the previous season.
Most licensed seasonal influenza vaccines rely on traditional egg-based manufacturing processes, which allow for large-scale production but are slow to respond to dynamic virus evolution9. Additionally, the egg-based manufacturing process may introduce adaptive mutations that result in antigenic differences between the vaccine-encoded strain and circulating virus strains which could negatively impact vaccine effectiveness10. Cell- and recombinant-based seasonal influenza vaccines do not require eggs for manufacturing and, therefore, avoid the risk of egg-based adaptation and egg supply shortages during avian influenza outbreaks11; however, they are significantly more expensive to produce12,13.
Alternatively, nucleoside-modified mRNA (modRNA) vaccines allow for faster and more cost-effective manufacturing. The cell-free in vitro transcription process enables the production of large numbers of vaccine doses within a shorter time period than can be achieved with conventional vaccine platforms14. This capability has been proven with the modRNA vaccines used to combat the COVID-19 pandemic. It took only a few weeks from when the genomic sequence of SARS-CoV-2 was made public (January 2020) to when the first doses of SARS-CoV-2 modRNA vaccines were manufactured for clinical testing (February 2020)15. modRNA vaccine technology, if applied to influenza, has the potential to enable efficient delivery of a seasonally updated vaccine while minimizing the risk of vaccine mismatch.
For the first time, we describe the preclinical immunogenicity and safety of influenza modRNA vaccines (IRV), encoding full-length HA from seasonal human influenza strains, that utilize the modRNA platform technology and LNP formulation of the COVID-19 modRNA vaccine (BNT162b2; Comirnaty®) developed by Pfizer and BioNTech. This platform has a large database of information on different SARS-CoV-2 strains and has consistently been shown to be safe, well tolerated, immunogenic, and efficacious in the prevention of COVID-1916,17,18,19. Formulations of monovalent (mIRV), trivalent (tIRV), and quadrivalent (qIRV) modRNA-HA vaccines were tested for in vitro expression and immunogenicity in multiple animal species (mice, rhesus and cynomolgus macaques). Additionally, safety of both mIRV and qIRV was assessed in Wistar Han rats.
Results
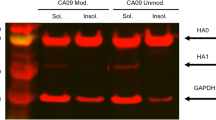
Monovalent, trivalent, and quadrivalent modRNA-HA efficiently express IAV and IBV HA proteins in vitro
modRNA constructs encoding codon-optimized, full-length HA proteins derived from A/Wisconsin/588/2019 (H1N1), A/Darwin/6/2021 (H3N2), B/Austria/1359417/2021 (B/Victoria), and B/Phuket/3073/2013 (B/Yamagata) were designed, synthesized, and encapsulated in LNPs. Expression of IAV and IBV HA from LNP-formulated mIRV, tIRV, and qIRV was confirmed in vitro. Influenza HA protein was expressed in HEK-293T cells in a dose-dependent manner from modRNA encoding the strain-specific HA antigen, as measured by flow cytometry (Supplementary Fig. 1A–D). The data demonstrate that the HA protein can be efficiently expressed from modRNA-HA vaccines regardless of valency (mIRV, tIRV, qIRV) or HA type (IAV or IBV).
Mice immunized with mIRV exhibit higher functional antibody responses and polyfunctional T cell responses post-boost as compared to an adjuvanted inactivated QIV
To evaluate immunogenicity of a monovalent modRNA-HA vaccine, mice (10 animals/group) were immunized with two doses of mIRV encoding the HA antigen from A/Wisconsin/588/2019 (H1N1) or a licensed adjuvanted QIV comparator (Fluad®) delivered 28 days apart. Sera were collected at immunologically relevant timepoints for evaluation of the magnitude and functionality of humoral responses. HA-specific antibody titers were measured by a hemagglutination inhibition assay (HAI) (Fig. 1a) and a microneutralization assay test (MNT) (Fig. 1b). Three weeks after the first dose (Day 21), mIRV and the QIV comparator induced similar HAI and MNT titers against A/Wisconsin/588/2019 (H1N1), however, mIRV induced statistically significantly higher HAI and MNT titers after the second dose compared to QIV. Two weeks after the second dose of mIRV (Day 42), HAI titers increased more than 6-fold (Fig. 1a) and MNT titers increased 68-fold (Fig. 1b) above titers obtained after the first dose (Day 21).
Female naïve BALB/c mice were immunized IM with two doses (prime + boost) of a monovalent modRNA-HA (H1) vaccine (mIRV; 0.2 μg; 10/group), a QIV comparator (Fluad®; 2.4 μg; 10/group), or saline (5/group). Functional antibody and virus neutralization responses against the mIRV strain A/Wisconsin/588/2019 (H1N1) were measured by HAI (a) and 50% MNT (b), respectively, on Days 21 (3 weeks post-prime) and 42 (2 weeks post-boost). Titers in (a, b) are reported as GMT with 95% CI. Each data point represents one animal. Statistical comparisons were performed using an independent sample t-test, ***p ≤ 0.0001. In the same study, T cell responses were analyzed by ICS using an HA peptide pool to stimulate T cells ex vivo using splenocytes harvested on Day 42. ICS assay results are expressed as mean ± SEM of the % of IFN-γ+ CD4+ T cells (c), IL-4+ CD4+ T cells (d), polyfunctional (IFN-γ+, IL-2+, TNF-α+, CD154+) CD4+ T cells (e), IFN-γ+ CD8+ T cells (f), and polyfunctional (IFN-γ+, TNF-α+, CD107a+) CD8+ T cells (g). Each data point represents one mouse. IM intramuscular, QIV quadrivalent influenza vaccine, HAI hemagglutination inhibition assay, MNT microneutralization assay, GMT geometric mean titer, LOD limit of detection for MNT assay, ICS intracellular cytokine staining, SEM standard error of the mean.
To evaluate HA-specific T cell responses, splenocytes were harvested two weeks after the second immunization, stimulated with peptides spanning the H1N1 HA protein from the vaccine strain (A/Wisconsin/588/2019), and assessed by intracellular cytokine staining for CD4+ T cells expressing IFN-γ, IL-4, IL-2, TNF-α and/or CD154, and CD8+ T cells expressing IFN-γ, TNF-α and/or CD107a. Immunization with two doses of mIRV induced a higher percentage of IFN-γ-producing CD4+ T cells than IL-4-producing CD4+ T cells (Fig. 1c), indicative of a Th1-biased response, whereas two doses of QIV induced a higher percentage of IL-4+ CD4+ T cells than IFN-γ+ CD4+ T cells (Fig. 1d), indicative of a Th2-biased response. A strong polyfunctional (IFN-γ+, IL-2+, TNF-α+, CD154+) CD4+ T cell response was also observed with the mIRV vaccine, but not with QIV (Fig. 1e). In addition, immunization with mIRV induced higher levels of IFN-γ+ CD8+ T cells (Fig. 1f) and polyfunctional (IFN-γ+, TNF-α+, CD107a+) CD8+ T cells (Fig. 1g) compared to QIV.
Rhesus and cynomolgus macaques immunized with mIRV exhibit durable functional antibody responses and polyfunctional T cell responses
To evaluate durability of the modRNA platform, immunogenicity of mIRV was evaluated in two species of NHPs, rhesus and cynomolgus macaques, for approximately 5 months following vaccination. A licensed comparator was not included in this study to limit animal numbers. Previously published studies have characterized the immune response to inactivated influenza vaccines, demonstrating induction of vaccine-specific antibody responses and variable cellular immune responses20,21,22,23,24,25. A total of three animals per group were immunized with two doses of mIRV (H1) 28 days apart. HA-specific antibodies were measured by HAI (Fig. 2a, b) and MNT (Fig. 2c, d). Vaccination with one dose of mIRV elicited a consistent pattern of HA-specific antibody responses against the homologous vaccine strain (A/Wisconsin/588/2019), inducing both HAI and neutralizing antibodies at three and four weeks after the first dose (Day 21 and Day 28) (Fig. 2a–d). Following the second immunization, HA-specific antibody levels peaked at one week after the second dose (Day 35) and then waned over the measured period of 19 weeks but stayed above baseline levels (Day -7). HAI and MNT titers plateaued from Day 105 through Day 168 of the study, maintaining levels comparable to those measured after the first dose (Day 21). T cell immunity was quantified by measuring cytokine-expressing peripheral CD4+ and CD8+ T cells after ex vivo stimulation of peripheral blood mononuclear cells (PBMCs) with HA peptide pools derived from the H1N1 vaccine strain (Fig. 2e, f). Immunization with mIRV induced IFN-γ-expressing CD4+ T cells with responses peaking approximately one week after the second dose (Day 35) and returning to baseline levels by Day 105 for both species. No change in peripheral CD8+ T cells was detected in either species after immunization (data not shown). Overall, the data provide evidence that an HA-containing modRNA vaccine elicits robust and durable humoral and cellular immune responses.
Rhesus and cynomolgus macaques were immunized IM with two doses (prime + boost) of a monovalent modRNA-HA (H1) vaccine (mIRV; 30 μg; 3/group). Functional antibody and virus neutralization responses against the mIRV strain A/Wisconsin/588/2019 (H1N1) were measured by HAI (a, b) and 50% MNT (c, d) 7 days before immunization (D-7); 7, 21, and 28 days after the prime; and 7, 14, 49, 77, 105, and 140 days after the boost (D35, D42, D77, D105, D133, and D168, respectively). Titer results are shown for rhesus (a, c) and cynomolgus (b, d) macaques. Each data point represents an individual NHP and the bar depicts the GMT of the 3 NHPs per group with 95% CI. In the same study, T cell responses were analyzed by ICS using an HA peptide pool to stimulate T cells ex vivo using PBMCs collected on D-7, D7, D35, D42, D77, D105, D133, and D168. ICS assay results are plotted as the % of IFN-γ+ cells within CD4+ T cell subsets for rhesus (e) and cynomolgus (f) macaques. Each data point represents an individual NHP and the bar depicts the median of the 3 NHPs per group with 95% CI. The connecting line in (a–d) shows the geomean group kinetics over time, and the line in (e, f) shows the median group kinetics over time. IM intramuscular, NHP nonhuman primate, HAI hemagglutination inhibition assay, MNT microneutralization assay, GMT geometric mean titer, LOD limit of detection for MNT assay, ICS intracellular cytokine staining, PMBCs peripheral mononuclear blood cells.
Immunization with two doses of qIRV in mice elicited functional antibody responses against IAV and IBV strains that were greater than or comparable to an adjuvanted inactivated QIV
As current licensed seasonal influenza vaccines are designed to protect against up to four different influenza viruses (H1N1, H3N2, B/Victoria, B/Yamagata), we next evaluated the immunogenicity of a quadrivalent modRNA-HA vaccine in mice. The qIRV encoded HAs from the WHO-recommended influenza strains for cell culture- or recombinant-based vaccines for use in the 2021–2022 northern hemisphere influenza season: A/Wisconsin/588/2019 (H1N1), A/Cambodia/e0826360/2020 (H3N2), B/Washington/02/2019 (B/Victoria), and B/Phuket/3073/2013 (B/Yamagata)26. Mice were immunized with two doses of qIRV or licensed adjuvanted QIV 28 days apart. Two weeks after the second immunization, functional antibodies against each of the four strains encoded by the vaccines were measured by HAI (Fig. 3a) and MNT (Fig. 3b). Immunization with qIRV induced statistically significant higher HAI and MNT titers against H1N1 and H3N2, and similar HAI and MNT titers against B/Victoria and B/Yamagata compared to QIV (Fig. 3a, b).
Female naïve BALB/c mice were immunized IM with two doses (prime + boost) of a quadrivalent modRNA-HA vaccine (qIRV; 0.8 μg (0.2 μg/HA); 10/group), a QIV comparator (Fluad®; 2.4 μg; 10/group), or saline (10/group). Functional antibody and virus neutralization responses against each of the four qIRV strains, A/Wisconsin/588/2019 (H1N1), A/Cambodia/e0826360/2020 (H3N2), B/Washington/02/2019 (B/Victoria), and B/Phuket/3073/2013 (B/Yamagata), were measured by HAI (a) and 50% MNT (b), respectively, on Day 42 (2 weeks post-boost). Due to reagent limitations, mouse sera from all groups (n = 10) were pooled in pairs for analysis and were not tested individually. All titers are reported as GMT with 95% CI. Each data point represents two paired animals. Statistical comparisons were performed using an independent sample t-test, ***, p ≤ 0.0001; ns not significant. IM intramuscular, QIV quadrivalent influenza vaccine, HAI hemagglutination inhibition assay, MNT microneutralization assay, GMT geometric mean titer, LOD limit of detection for MNT assay.
Immunization with two doses of tIRV or qIRV in mice elicited similar IAV and IBV neutralizing antibody responses as mIRV
Due to the absence of WHO-confirmed detection of naturally occurring B/Yamagata lineage influenza viruses since March 2020, the WHO and VRBPAC have recommended the use of trivalent vaccines without the B/Yamagata component for the 2024–2025 northern hemisphere influenza season6,7. To assess if a trivalent (tIRV) modRNA vaccine could perform as well as a qIRV modRNA vaccine for the three shared vaccine strains, we compared the immunogenicity of tIRV and qIRV to one another and to licensed adjuvanted QIV in mice. mIRVs targeting the individual vaccine strains were evaluated in parallel to assess any possible interference between IAV and IBV components of the multivalent IRVs that could result in lower immunogenicity. In this study, the modRNA-HA vaccines encoded HAs from the WHO-recommended influenza strains for cell culture- or recombinant-based vaccines for use in the 2022–2023 northern hemisphere influenza season: A/Wisconsin/588/2019 (H1N1), A/Darwin/6/2021 (H3N2), B/Austria/1359417/2021 (B/Victoria), B/Phuket/3073/2013 (B/Yamagata)27. Two weeks after the second immunization, virus neutralization titers against the vaccine-matched strains were measured by MNT (Fig. 4). Neutralization titers elicited by mIRV, tIRV, or qIRV against the shared vaccine strains (H1N1, H3N2, and B/Vic) were not statistically different (Fig. 4a–c) indicating an absence of interference. Neutralization titers against B/Yamagata elicited by mIRV and qIRV were also not statistically different (Fig. 4d). Notably, all three modRNA-HA vaccine formulations induced statistically significantly higher virus neutralizing titers against H1N1 (Fig. 4a) and B/Victoria (Fig. 4c) than the licensed QIV comparator. Neutralization titers against H3N2 (Fig. 4b) and B/Yamagata (Fig. 4d) were similar between the modRNA-HA vaccine formulations and the QIV control.
Female naïve BALB/c mice were immunized IM with two doses (prime + boost) of a monovalent (mIRV; 0.2 μg; 10/group), trivalent (tIRV; 0.6 μg (0.2 μg/HA); 10/group), or quadrivalent (qIRV; 0.8 μg (0.2 μg/HA); 10/group) modRNA-HA vaccine, a QIV comparator (Fluad; 2.4 μg; 10/group), or saline (10/group). Virus neutralization responses against each of the IRV-targeted strains (a) A/Wisconsin/588/2019 (H1N1), (b) A/Darwin/6/2021 (H3N2), (c) B/Austria/1359417/2021 (B/Victoria), and (d) B/Phuket/3073/2013 (B/Yamagata), were measured by 50% MNT on Day 42 (2 weeks post-boost). All titers are reported as GMT with 95% CI. Each data point represents one animal. Statistical comparisons were performed using an ANOVA and Tukey’s multiple comparisons test, ***, p ≤ 0.0001; ns not significant. IM intramuscular, QIV quadrivalent influenza vaccine, MNT microneutralization assay, GMT geometric mean titer, LOD limit of detection for MNT assay.
Toxicological evaluation of mIRV and qIRV in Wistar Han rats
To evaluate the nonclinical safety of modRNA-HA influenza vaccines, repeat-dose toxicity studies were conducted with mIRV encoding the HA antigen from A/Wisconsin/588/2019 (H1N1) and qIRV encoding HA antigens from the WHO-recommended influenza strains for cell culture- or recombinant-based vaccines for use in the 2021–2022 northern hemisphere influenza season26. Briefly, male and female Wistar Han rats were administered 2 doses of mIRV or qIRV two weeks apart (Days 1 and 15). Dosing phase animals were euthanized two days after the second dose (Day 17) while recovery phase animals were euthanized approximately three weeks following the second dose (Day 38–39).
In-life findings
In the repeat-dose toxicity studies, administration of mIRV and qIRV was tolerated without evidence of systemic toxicity. There were no vaccine-related mortalities, clinical signs, or effects on injection site dermal scores or ophthalmoscopic parameters. Transiently higher mean body temperature was observed for both mIRV (both sexes) (Supplementary Fig. 2A) and qIRV (males only) (Supplementary Fig. 2B) on Days 1 (1.01x–1.03x controls; 38.65 °C: p < 0.01 and 37.75 °C: p < 0.05, respectively) and 15 (1.01–1.02x controls; 38.71 °C: p = 0.05 females and 37.15 °C–38.14 °C: p < 0.01 males). Vaccine-related transiently lower mean body weight was observed for both mIRV and qIRV in males only on Day 4 (0.96x control; p < 0.05) (Supplementary Fig. 2C, D) due to body weight loss and an associated decrease in mean food consumption (0.85x–0.84x controls; p < 0.01) and recovered by Day 8. Transiently lower mean food consumption was also observed on Day 4 (0.89x control; p < 0.01) in the female group administered qIRV, with recovery by Day 8 (Supplementary Fig. 2D). Transient slightly lower mean body weight and food consumption effects were associated with the observed acute phase protein response (higher A2M and A1AGP). There was no effect on mean body weight or food consumption in the recovery phase for either vaccine. The effects on body weight and body temperature were similar to findings reported with COVID-19 modRNA vaccines28.
Serology
To confirm immunogenicity of both vaccine formulations administered in rats, functional antibodies titers were measured by HAI. An HAI response was detected in rats at the end of the dosing and recovery phases for all strains encoded by mIRV (Supplementary Fig. 3) and qIRV (Supplementary Fig. 4). Hemagglutinin inhibition was not observed in the saline control animals.
Clinical pathology
Key clinical pathology observations in rats were similar for both mIRV and qIRV and reflected the expected immune response following vaccination. Hematology findings were consistent with an inflammatory leukogram and included higher neutrophil counts on Days 3 and 17; a higher incidence of hyper-segmented neutrophils on Day 17; and higher monocytes, eosinophils, and/or large unstained cells on Days 3 and 17 (Fig. 5a, Supplementary Table 1). Findings consistent with an acute phase response were also noted for both vaccines and included higher fibrinogen on Day 17; higher globulin and/or lower albumin on Days 3 and 17; and higher alpha-2 macroglobulin (A2M) and alpha-1-acid glycoprotein (A1AGP) on Days 3 and 17 (Fig. 5b–d, Supplementary Table 1). All clinical pathology changes recovered by the end of the recovery phase except for higher globulin and/or lower albumin (Supplementary Table 1). In addition, transient, slightly lower reticulocyte and/or platelet counts on Day 3 and a nominal prolongation in prothrombin time (PT) on Day 17 were observed for both vaccines (Supplementary Table 1), a spectrum of findings consistent with immune activation29,30,31 and similar to observations with COVID-19 modRNA vaccines28.
Neutrophil counts (a), fibrinogen concentrations (b), A2M concentrations (c), and A1AGP concentrations (d) in male (M) and female (F) Wistar Han rats immunized IM with two doses of mIRV (34 μg; 15/sex/group), qIRV (30 μg; 7.5 μg/HA; 15/sex/group), or saline (control). Blood samples were collected on Dosing Phase Days 3 and/or 17 and/or 39 (D3, D17, and D39, respectively). Box-and-whisker plots represent group medians (middle line), 25th and 75th percentiles (box), and min and max (lower and upper whiskers). All saline groups depicted in (a–d) are shown in black. A2M, alpha-2 macroglobulin; A1AGP, alpha-1-acid glycoprotein; IM, intramuscular.
Anatomic pathology
Histopathologic features were comparable between mIRV and qIRV vaccines, with similar non-adverse vaccine-related microscopic findings at the injection site and in the draining (iliac) and inguinal lymph nodes, spleen, bone marrow, thymus, and liver. Vaccine-related cell inflammation and edema ranging from minimal to mild were observed at the injection site (Fig. 6a, b). These findings are typically associated with the IM administration of LNP-encapsulated mRNA vaccines28,32 and correlated with macroscopic observations of abnormal color (dark). At the end of the recovery phase, full recovery of edema and dark injection site and partial recovery of inflammation (minimal) at the injection site was observed (Fig. 6c, d).
a Injection site section of mIRV (H1) immunized animals euthanized 2 days after the third dose (Day 17) showing inflammatory cells (arrows) admixed with pale eosinophilic fluid (edema) (black asterisk) infiltrating and expanding subcutaneous tissue and connective tissue of skeletal muscle. b 20x magnification of (a) showing inflammatory cells (mainly neutrophils with fewer plasma cells, macrophages, and lymphocytes) (arrows) and edema fluid (asterisk) surrounding myofibers. c Injection site section of mIRV immunized animals euthanized after a 3-week recovery showing fewer inflammatory cells infiltrating and expanding subcutaneous tissue and spaces around skeletal myofibers (arrows). d 20x magnification of (c) showing inflammatory cells (fewer plasma cells and lymphocytes) surrounding myofibers (arrows). e Lymph node sections of mIRV immunized animals showing prominent germinal centers (GC) and inflammatory cells (predominantly plasma cells) expanding sinuses (inset). f Liver sections of mIRV immunized animals euthanized 2 days after the third dose (Day 17) showing hepatocytes containing small clear round membrane bound structures within cytoplasm (black arrowheads).
Vaccine-related findings in the draining lymph nodes (increased cellularity of plasma cells and germinal centers) (Fig. 6e), spleen (increased cellularity of hematopoietic cells and germinal centers) (Supplementary Fig. 5A), and bone marrow (increased cellularity of hematopoietic cells) (Supplementary Fig. 5B) were secondary to immune activation and/or inflammation at the injection site, as reported previously for the COVID-19 modRNA vaccine28. The presence of plasma cells in the draining and inguinal lymph nodes was interpreted to reflect a robust immunological response to the vaccines and correlated with enlarged draining lymph nodes after vaccine administration. Microscopic observations in the spleen correlated with increased splenic weights (Supplementary Table 2) and macroscopically enlarged spleens. At the end of the recovery phase, full recovery occurred for enlarged spleen, higher spleen weights, increased cellularity of hematopoietic cells in the spleen and bone marrow, and increased cellularity of germinal centers in the spleen. Partial recovery occurred for enlarged draining lymph nodes and increased cellularity of plasma cells and germinal centers in the draining and inguinal lymph nodes. An infiltration of macrophages in the draining and inguinal lymph nodes was observed with mIRV at the end of the recovery phase and was considered indicative of a reparative process (phagocytosis of material draining to the lymph node from the injection site).
A microscopic finding of minimal decreased lymphocyte cellularity in the thymus was observed for mIRV and was considered secondary to stress (indicated by a slight decrease in body weight or food consumption or a slight increase in body temperature) and not directly related to the vaccine33. Decreased lymphocyte cellularity correlated with lower thymic weights (Supplementary Table 2). At the end of recovery phase, these findings were completely recovered.
Microscopic findings of minimal periportal hepatocyte vacuolation were observed for both vaccines at the end of the dosing phase (Fig. 6f). This was not associated with microscopic or biochemical evidence of hepatocyte damage (no increases in ALT or AST) and was interpreted to reflect hepatocyte uptake of the LNP lipids, as observed previously28,34. At the end of the recovery phase, this finding was completely recovered.
Discussion
Egg-based influenza vaccines comprise the majority of the influenza vaccine global market16. While egg-based manufacturing can support the production of large volumes at a low cost, the process takes approximately six months and can be impacted by egg supply shortages. Furthermore, passaging influenza viruses in eggs during manufacturing can introduce egg-specific mutations that alter the antigenicity of the virus leading to mismatch between the vaccine strain and circulating viruses that may reduce vaccine efficacy as was seen for the H3N2 vaccine strain in the 2012–2013 influenza season35.
Alternatively, modRNA vaccines have emerged as a powerful tool for the prevention of infectious diseases as evidenced by the critical role they played in the COVID-19 pandemic response. modRNA vaccine technologies offer the ability to rapidly produce large numbers of vaccine doses without the risk of mismatch associated with egg-based manufacturing, and at a lower cost than cell-based influenza vaccines13. The shorter production time can also help to mitigate impacts of viral evolution and antigenic drift on vaccine efficacy. In preclinical studies, influenza mRNA-LNP vaccines targeting HA have demonstrated robust antibody induction and T cell responses36,37, as well as protective efficacy against influenza virus challenge in multiple animal models38,39,40,41,42,43. Our studies described here support these prior preclinical observations and provide further evidence that modRNA-HA vaccines targeting seasonal influenza strains are immunogenic.
Here, a modRNA-LNP platform16,17,18,19 was leveraged to develop seasonal influenza vaccines. HA antigens administered in monovalent and multivalent (tIRV, qIRV) formulations in equal doses per antigen exhibited consistent antibody responses specific to each HA subtype in mice, demonstrating that potency of modRNA-HA vaccines is preserved when multiple antigens are targeted. Studies in both mice and NHPs demonstrated that influenza modRNA-HA vaccines elicit a multi-faceted immune response characterized by strong HA-specific functional and neutralizing antibody responses as well as cell-mediated immune responses. Unadjuvanted monovalent and quadrivalent modRNA-HA vaccines induced similar or better HAI titers compared to an adjuvanted licensed QIV vaccine. An HAI titer of ≥1:40 is an accepted immunological correlate of protection against influenza infection in humans44,45.
Influenza modRNA-HA vaccines induced robust T cell responses in mice and NHPs. In mice, modRNA-HA vaccination induced Th1-type CD4+ and IFN-γ+ CD8+ T cell responses, whereas vaccination with the licensed QIV comparator induced a Th2-type CD4+ T cell response and a minimal IFN-γ+ CD8+ T cell response. modRNA-HA vaccination also induced a Th1-type CD4+ T cell response in NHPs. Though a licensed inactivated influenza vaccine comparator was not evaluated in the NHP study, a prior study by Carroll et. al. evaluated the T cell response in rhesus macaques following vaccination with a licensed inactivated influenza vaccine (Fluzone®)22. Fluzone®-vaccinated NHPs mounted a CD4+ T cell response consisting of a higher proportion of influenza-specific IL-2- and TNF-secreting CD4+ T cells and a smaller proportion of influenza-specific IFN-γ-secreting CD4+ T cells; however, animals failed to retain the IFN-γ+ CD4+ T cells two weeks post-boost22. In contrast, in our study, modRNA-HA induced IFN-γ-expressing CD4+ T cells that peaked one week post-boost with measurable responses detected until Day 105 when levels returned to baseline.
In the study by Carroll et al., influenza-specific IFN-γ+ CD8+ T cells were detectable in Fluzone®-vaccinated macaques, but only in a subset of animals22. In our study, IFNγ+ CD8+ T cell responses were observed in mice but not NHPs following modRNA-HA vaccination. The lack of CD8+ T cell activity observed in modRNA-HA-vaccinated NHPs is similar to observations from NHP studies of a COVID-19 mRNA vaccine46; however, vaccination of humans with COVID-19 mRNA vaccines has been shown to elicit durable CD8+ T cell responses47,48. In summary, T cell responses to influenza vaccines in NHPs may vary based on vaccine platform, use of adjuvant, route of administration, and animal species, and may not be fully predictive of responses in humans.
The immune response elicited by the influenza modRNA-HA vaccines in preclinical animal studies aligns with clinical data from both SARS-CoV-2 and influenza modRNA vaccines. Data from a Phase 1/2 clinical trial of the BNT162b2 COVID-19 modRNA vaccine (NCT04368728) demonstrated that vaccination induced high levels of SARS-CoV-2 neutralizing antibody titers as well as antigen-specific CD8+ and Th1-type CD4+ T cell responses19. Preliminary data from a Phase 2 trial of a quadrivalent influenza modRNA-HA vaccine (NCT05052697) also demonstrated the ability of modRNA vaccines to induce both neutralizing antibody responses and strain-specific CD4+ and CD8+ T cell responses49. The induction of influenza-specific T cell immunity has been associated with reduced disease severity and viral shedding as well as broadly protective heterosubtypic immunity50. Thus, the modRNA platform may provide benefits over currently licensed seasonal influenza vaccines which induce limited T cell immunity51,52,53. Studies to investigate the HA trimers produced from modRNA-HA and to further characterize the types of antibodies elicited following vaccination are ongoing or planned, and are beyond the scope of the current manuscript.
Nonclinical toxicity of the modRNA-LNP platform has previously been assessed in rats using the BNT162 vaccine candidates BNT162b1, BNT162b2, and BNT162b3 which were tolerated at doses up to 100 µg without any evidence of systemic toxicity28. As demonstrated here, both monovalent and quadrivalent modRNA-HA influenza vaccines using the same LNP platform were also well tolerated and shared similar non-adverse findings and expected inflammatory responses to those seen after administration of the BNT162 modRNA vaccine candidates28. The reproducible, consistent toxicology findings observed between the COVID-19 and influenza modRNA vaccines support the consideration of modRNA-LNP as a safe and tolerable vaccine platform technology that could be utilized to target a new viral variant or pathogen by changing the RNA-encoded target antigen.
Altogether, the data presented here demonstrate the ability of modRNA vaccines to induce robust, balanced humoral and cellular immune responses to influenza with a tolerable nonclinical safety profile. This data, along with platform biodistribution data from the COVID-19 vaccine program, were used to support a first-in-human (FIH) Phase 1 trial of Pfizer’s modRNA influenza vaccines (NCT05052697) which have since advanced to Phase 3 testing (NCT05540522). modRNA vaccines represent a promising approach for improving influenza vaccine efficacy to reduce morbidity and mortality associated with seasonal influenza epidemics.
Methods
Formulation of the monovalent, trivalent, and quadrivalent modRNA-HA vaccines
ModRNA-HA vaccines encoding full-length HA proteins of WHO-recommended strains for cell culture- or recombinant-based vaccines for use in either the 2021–2022 (A/Wisconsin/588/2019 (H1N1), A/Cambodia/e0826360/2020 (H3N2), B/Washington/02/2019 (B/Victoria), and B/Phuket/3073/2013 (B/Yamagata))26 or 2022–2023 (A/Wisconsin/588/2019 (H1N1), A/Darwin/6/2021 (H3N2), B/Austria/1359417/2021 (B/Victoria), and B/Phuket/3073/2013 (B/Yamagata))27 northern hemisphere influenza seasons were individually formulated and prepared as either monovalent, trivalent, or quadrivalent formulations as previously described for the BNT162b2 modRNA vaccine17. Stock concentrations of modRNA-HA were diluted in saline to achieve the desired dose for vaccine administration in animals.
In vitro expression of HA from the influenza modRNA-HA vaccine
Individually LNP-formulated modRNAs encoding full-length HA from H1N1, H3N2, B/Victoria, or B/Yamagata strains were diluted in Opti-MEM (Thermo Fisher, Cat #31985062) and directly added to a HEK-293T (CRL-3216, ATCC) cell monolayer at four RNA dose levels (62.5, 31.1, 15.6, and 7.8 ng/well). The input amount of mRNA encoding the strain-specific HA was the same between modRNA formulations (e.g., different amounts of mIRV and qIRV were applied to cells to achieve a final concentration of 62.5 ng/well of mRNA encoding the B/Phuket/3073/2013 HA). Opti-MEM media alone was used as a negative control. Protein expression was measured with a flow cytometer (BD FACS Fortessa) using in-house generated rabbit polyclonal antibodies raised against each of the following strains: A/Wisconsin/588/2019 (H1N1), A/Darwin/6/2021 (H3N2), B/Austria/1359417/2021 (B/Victoria), or B/Phuket/3073/2013 (B/Yamagata), followed by a secondary anti-rabbit antibody conjugated to Alexa-Fluor 488 (Invitrogen, Cat # A-11008). The percentage of live cells expressing the strain-specific HA protein was enumerated and expression was measured by quantifying the number of live cells that had a positive signal for bound anti-HA antibody.
Animals
Mouse immunogenicity studies utilized female BALB/c mice (The Jackson Laboratory) that were first immunized between 7-13 weeks of age. NHP immunization studies utilized female rhesus macaques (Macaca mulatta) and cynomolgus macaques (Macaca fasicularis) from the Pfizer colony at Pearl River, NY that were co-housed in standard quad caging. Rhesus and cynomolgus macaques were immunized at 5.5 and 13.5–15.5 years of age, respectively. Animal studies were performed at Pfizer, Pearl River, NY, which is accredited by the Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC).
For mIRV and qIRV toxicology studies, male and female Wistar Han rats, 11 weeks of age at the dosing study start, were supplied by Charles River Laboratories. Toxicology studies were conducted at Pfizer, Groton, CT according to GLP and OECD guidelines. Animals were offered Certified Irradiated Rodent Diet 2916 C (Envigo Teklad Global Diet) and locally sourced water ad libitum, except when fasting was conducted prior to clinical pathology collections or euthanasia. Animals were socially housed throughout the study in ventilated Tecniplast double decker polyphenylsulfone cages with Enrich-n’Pure® (The AndersonsP, Inc.). Environmental conditions across studies were set to maintain relative humidity ranging from 30% to 70% and temperature ranging from 68 °F to 79 °F with room lighting set to provide a 12-h light/dark cycle.
All procedures performed on animals were in accordance with regulations and established guidelines and were reviewed and approved by an Institutional Animal Care and Use Committee.
Mouse immunization study design
Experimental vaccine groups each contained 10 female BALB/c mice. Control groups consisted of 5 or 10 female BALB/c mice that were administered 50 µL of saline intramuscularly (IM). For all studies, mice were immunized IM twice, on Days 0 and 28. Groups receiving modRNA-HA vaccines received 0.2 µg of each mRNA HA construct. Thus, mIRV vaccines were administered at a 0.2 µg dose in a 50 µL volume; tIRV was administered at a 0.6 µg dose (0.2 µg/HA) in a 50 µL volume; and qIRV vaccines were administered at a 0.8 µg dose (0.2 µg /HA) in a 50 µL volume. An undiluted comparator QIV (Fluad®) was administered IM at a final concentration of 2.4 µg in a 20 µL dose volume (1/25th of the human dose), also on Days 0 and 28. Whole blood was collected on Day 21 (3 weeks post-dose 1) and Day 42 (2 weeks post-dose 2) and evaluated for levels of functional anti-HA antibodies by serology. Splenocytes were isolated on Day 42 (study end) to measure the T cell-mediated immune response following immunization.
NHP immunization study design
Rhesus and cynomolgus macaques (3 animals/group) were each immunized IM with a 30 µg dose of mIRV (A/Wisconsin/588/2019) in a 0.5 mL total volume. Whole blood was collected on Days -7 (pre-vaccination), 7, 21, 28, 35, 42, 77, 105, 133, and 168 and evaluated for levels of functional anti-HA antibodies by serology. PBMCs were isolated on Days -7 (pre-vaccination), 7, 35, 42, 77, 105, 133 and 168 to measure T cell responses following immunization.
Toxicology study design
For both toxicology studies, male and female Wistar Han rats (15/sex/group) were randomly assigned to Groups 1 or 2, and doses were administered IM by 2 separate injections on Days 1 and 15. Group 1 was administered sterile saline. Group 2 was administered with either 34 µg mIRV or 30 µg qIRV (7.5 µg/HA). A subset of animals (10/sex/group) was euthanized 2 days after the second dose (Day 17), while the remaining animals (5/sex/group) underwent an approximate 3-week recovery and then were euthanized (Day 38–39). Serum samples were collected from each animal prior to dose initiation and on Day 17 (dosing phase) and Day 21 (recovery phase) for analysis of hemagglutination inhibition, to confirm in parallel functional immunogenicity of the mIRV and qIRV under toxicological observation.
Samples for clinical pathology analysis in toxicology studies (hematology, coagulation, clinical chemistry, acute phase proteins and urinalysis) were collected on Days 3 (nonterminal; hematology, clinical chemistry, and acute phase proteins A1AGP and A2M only), 17 (terminal), and 39 (terminal), from overnight fasted animals. For non-terminal collections, hematology was assessed in the first 7 animals/sex/group and clinical chemistry was assessed in the last 8 animals/sex/group. Phlebotomy sites included the jugular vein (non-terminal bleed) or aorta under isoflurane anesthesia followed by exsanguination (terminal bleed). Blood samples were collected into appropriate tubes (K2EDTA for hematology, 3.2% sodium citrate for coagulation, serum separator for clinical chemistry and acute phase proteins).
Animal blood collection and splenocyte isolation
For mouse immunization studies, the interim bleed was conducted using a submandibular bleeding technique. At the study end, blood was collected via cardiac puncture (terminal bleed). Whole blood tubes remained at room temperature (RT) for at least 30 min prior to centrifuging at 10,000 RPM for 3 min for sera collection. Samples for HAI and MNT assays were treated using a receptor destroying enzyme (RDE) kit (Accurate Chemical), heat inactivated and pre-adsorbed with turkey red blood cells (RBCs). Samples were stored at −80 °C until testing. At the study end, spleens were collected from 5 mice per group and separately placed in a 70 µm cell strainer (Fisher) immersed in 7 mL of complete RPMI (cRPMI: 10% FBS/RPMI; Pen-Strep; Sodium pyruvate; HEPES; MEM-NEAA; Amphotericin B) per well of a 6-well plate. Plates were maintained on ice during transit and before processing for single cell suspension. Spleens were homogenized, subjected to RBC lysis, and passed through a cell strainer to remove RBCs and clumps.
For NHP immunization studies, blood for serum and PBMC isolation was collected in BD Vacutainer® SST™ tubes and K2 EDTA 5.4 mg tubes, respectively, while animals were safely restrained. Whole blood samples were centrifuged at 3000 RPM for 10 min and sera were collected and stored at −80 °C until testing. Blood for PBMC isolation were retained at RT until processed. Diluted whole blood was layered on 90% Ficoll (GE Healthcare) to isolate PBMCs via density gradient centrifugation at 800 × g. PBMCs were then frozen in Gibco Recovery™ Cell Culture Freezing Medium at 5 × 106 cells/vial and stored in liquid nitrogen until analysis.
Viruses
All viruses used for testing were rescued using a reverse genetics system similar to one previously described54. In brief, an eight-plasmid system was applied for virus rescue. Each bidirectional plasmid encoded one of the eight segmented genes of influenza virus. The sequences for HA and NA genes were strain-specific and the six influenza backbone genes were subtype-specific (IAV or IBV). For IAV, sequences for the backbone genes of PA, PB2, NP, NS, and M were from the A/Puerto Rico/8/1934 (H1N1) (PR8) strain while PB1 sequence was from the A/California/07/2009 (H1N1) strain. For IBV, all six backbone genes were from B/Brisbane/60/2008 (B/Vic). The pool of 2 µg of each plasmid in OptiMEM medium (Gibco # 31985) was co-transfected into a co-culture of HEK-293T and MDCK cells (1:1 ratio) with Lipofectamine 2000 (Invitrogen) for 4 h at 37 °C followed by replacement of media with OptiMEM supplemented with 1 µg/mL of TPCK-treated trypsin. The viruses were harvested at 72-h post-transfection and propagated twice in MDCK cells with multiplicity of infection (MOI) of 0.001–0.01 for passage 1 and MOI of 0.0001–0.001 for passage 2. Passage 1 viruses served as virus seeds and passage 2 viruses served as viral stocks for HAI and MNT assay testing, described below.
Hemagglutination inhibition assay (HAI)
modRNA-HA vaccine-induced functional anti-HA antibodies that prevent HA-mediated agglutination of RBCs were measured using the hemagglutination inhibition assay (HAI). All sera were pre-treated with RDE, heat-inactivated, and then pre-adsorbed with appropriate RBCs to remove any non-specific agglutinins. 2-fold serial dilutions of mouse or NHP sera, tested in duplicate, in PBS were mixed with the vaccine matched influenza virus strain on a shaker for 5 min then left to incubate for 30 min at RT. The neutralization reaction was then mixed with either turkey or guinea pig RBCs (Lampire Biological Laboratories) and incubated an additional 30 or 60 min, respectively, at RT. Assay plates were imaged on a FluHema (SciRobotics). The HAI titer was reported as the reciprocal of the highest serum dilution resulting in loss of HA activity, visualized as a full smear reaching the bottom of the well with substantial footing when the microtiter plate was tilted 60° for 30 s, when using turkey RBCs. If guinea pig RBCs were used, loss of HA activity was observed as a pellet on the microtiter plate without tilting. All samples were run in duplicate.
For the toxicity studies, the HAI assay was conducted by VisMederi (Siena, Italy). In the VisMederi HAI assay, sera collected from mIRV and qIRV immunized rats were pre-treated with RDE, heat-inactivated and then pre-adsorbed with appropriate RBCs to remove any non-specific agglutinins. The treated serum, tested in duplicate per sample, was serially titrated two-fold in a dilution plate starting at a 1:10 dilution. An equal volume of standardized influenza antigen, obtained from Francis Crick Institute (London, UK) and propagated by VisMederi Research (Siena, Italy), was added to the serum samples and the plates were incubated 60 min at RT. RBCs were then added to all wells, and plates were incubated further for 60 min at RT. Following the last incubation, the plates were tilted, and the titer was determined as the reciprocal of the highest serum dilution in which agglutination was still completely inhibited. The geometric mean of four titers per sample (two analysts + two readers) was reported for each influenza vaccine antigen.
Microneutralization test (MNT)
Anti-HA neutralizing antibody responses following vaccination were measured using a 1-day microneutralization assay (MNT). Sera were pre-treated with RDE and heat-activated prior to use in the MNT assay. Serial dilutions of either mouse or NHP sera were incubated in a flat bottom 96-well plate with the vaccine matched influenza virus strain for 1 h at 37 °C/5% CO2. Adherent MDCK cells (MDCK NBL-2, ATCC CCL-34) were added in suspension on top of the neutralization reaction and incubated at 37 °C/5% CO2 for 18–20 h. Cells were then fixed with methanol and stained with either Polyclonal Rabbit IgG Anti-Influenza A NP or Anti-Influenza B NP (Invitrogen) primary antibody followed by AlexaFluor 488 goat anti-rabbit IgG H + L (Life Technologies) secondary antibody. Infected cells were counted using a CTL ImmunoSpot S6 Universal-V Analyzer with ImmunoCapture Software (Cellular Technology Ltd). MNT titers were reported as the reciprocal of the dilution that resulted in 50% reduction in infection when compared to a no serum control. All samples were run in duplicate.
Intracellular cytokine staining assay
Vaccine-induced T cell responses to influenza were measured by flow cytometry-based intracellular cytokine staining assay (ICS). In mouse studies, freshly-isolated splenocytes (2 × 106 cells/well) were cultured in cRPMI with media containing DMSO only (unstimulated) or a specific peptide pool representing HA sequences of the A/Wisconsin/588/2019 (H1N1) influenza virus strain (Mimotopes) for 5 h at 37 °C in the presence of protein transport inhibitors, GolgiPlug and GolgiStop. Following stimulation, cells were stained for surface and intracellular markers to identify activated and/or cytokine-expressing T cell types (CD3+ cells for CD4 vs CD8), activation markers (CD154/CD40L), and cytokines (IFN-γ, IL-2, IL-4, TNF-α, CD154, and CD107a). The eBioscience™ fixable viability dye eFluor 506 (Invitrogen) was used prior to surface staining, per manufacturer’s instructions, to exclude dead cells. After staining, the cells were washed and resuspended in flow cytometry buffer (2% FBS/PBS). Cells were acquired on a BD LSR Fortessa and data were analyzed using BD FlowJo™ software. Results are background (media - DMSO) subtracted and shown as a percentage of CD4+ T cells or CD8+ T cells.
In NHP studies, the ex vivo stimulation with HA peptides was performed as described above, using PBMCs collected at different timepoints in place of splenocytes. Frozen PBMCs were thawed and rested for the ICS assay. Following stimulation, PBMCs were stained for surface and intracellular markers to identify IFN-γ-expressing T cells for both species (rhesus and cynomolgus macaques). Acquired data were analyzed as described above. The T cell gating strategy used for all species is shown in Supplementary Fig. 6A, B.
Toxicology observations and measurements
For in-life assessments, during the Dosing Phase all animals were weighed twice prior to the initiation of dosing (PID) on Days 1 and 7, prior to dosing on Days 1 and 15, and on non-dosing Days 4, 8, and 11, and a fasted weight was collected just prior to scheduled necropsy. Body weights were collected on Recovery Phase Days 1, 8, 15, and 21. Clinical observations occurred at least once daily prior to the initiation of dosing, at least twice daily on non-dosing days and during the recovery phase, and prior to and after each dose on dosing days. Body temperatures were collected on all animals on Dosing Phase Days 1 and 15 prior to dosing and at approximately 4- and 24-h post-dose. Injection sites were observed on Dosing Phase Days 1 and 15 prior to dosing and approximately 4- and 24-h post-dose on all animals.
Hematology was evaluated using a Siemens Advia 2120i analyzer (Siemens Healthineers Tarrytown, NY, USA). Fibrinogen activated partial thromboplastin time, and prothrombin time was evaluated on the Diagnostic Stago STA-R evaluation coagulation analyzer (Diagnostic Stago, Parsippany, NJ, USA). Blood smears were prepared for the first 7 animals on Day 3 and all animals on Day 17 and Day 39. Blood cell morphology was evaluated microscopically on 5 animals of each sex from all groups at both scheduled necropsies (i.e., at dosing and recovery phases). Routine clinical chemistry parameters were evaluated using a Siemens Advia 1800 clinical chemistry analyzer (Siemens Healthineers, Tarrytown, NY, USA). Acute phase proteins alpha-2 macroglobulin (A2M) and alpha-1-acid glycoprotein (A1AGP) were measured using the rat MSD Acute Phase Protein Panel 1 on the MSD SECTOR S 600 Analyzer (Meso Scale Design). Routine urinalysis parameters were measured, and a microscopic examination of sediment for formed elements was performed on 5 animals of each sex from all dose groups at both scheduled necropsies (i.e., dosing and recovery phases).
For post-mortem analysis, complete necropsies, tissue collection, organ weights, and macroscopic tissue evaluation were performed on all animals. Animals were euthanized by gas anesthesia (isoflurane) followed by exsanguination on Dosing Phase Day 17 (2 days after the last dose) or on Recovery Phase Day 22, the last day of the Recovery Phase (surviving animals). Necropsy, tissue collection, organ weights, macroscopic tissue evaluation, and microscopic examination were performed. Anatomic pathology analysis was completed at Pfizer DSRD, Groton, CT, and microscopic examination and peer review were completed at Pfizer DSRD, Pearl River, NY.
Statistical analysis
Animal immunogenicity data was analyzed using GraphPad PRISM software. GMTs of the immune responses for vaccine groups and strains were calculated and are displayed in each bar chart. An independent two sample t-test was performed to compare immune responses of two groups between mIRV or qIRV and QIV (Fluad®). An analysis of variance (ANOVA) was conducted to compare immune responses among mIRV, tIRV, qIRV, and QIV (Fluad®). All pairwise comparisons of the four groups were performed and Tukey’s test was applied to adjust for multiple comparisons. All tests were two-tailed. A p value less than 0.01 was considered statistically significant and is marked with asterisk(s) in the bar charts.
Statistical analysis of body weight, body weight change, food consumption, and body temperature were conducted. Descriptive statistics were generated for each parameter and group at each scheduled sampling time or each time interval. Analysis of body temperature was based on the maximum body temperature post injection for each animal. A nonparametric (rank-transform) one-way ANOVA was conducted, with a 2-sided pairwise comparison of each dose group to the reference group (saline control) using Dunnett’s test. Average ranks were assigned to ties. A p value of less than 0.05 was considered statistically significant and is marked with asterisk(s) in the bar charts.
Data availability
All data generated or analyzed during this study are included in the published article and its supplementary information file. Primary data sets may be made available upon reasonable request and with the permission of Pfizer Inc.
References
Paget, J. et al. Global and national influenza-associated hospitalisation rates: estimates for 40 countries and administrative regions. J. Glob. Health 13, 04003 (2023).
Iuliano, A. D. et al. Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. Lancet 391, 1285–1300 (2018).
CDC. Disease Burden of Flu, https://www.cdc.gov/flu/about/burden/ (2023).
Kostova, D. et al. Influenza illness and hospitalizations averted by influenza vaccination in the United States, 2005-2011. PLoS ONE 8, e66312 (2013).
Carias, C. et al. Net Costs Due to Seasonal Influenza Vaccination-United States, 2005-2009. PLoS ONE 10, e0132922 (2015).
FDA. Use of Trivalent Influenza Vaccines for the 2024-2025 U.S. Influenza Season, https://www.fda.gov/vaccines-blood-biologics/lot-release/use-trivalent-influenza-vaccines-2024-2025-us-influenza (2024).
WHO. Recommended composition of influenza virus vaccines for use in the 2024-2025 northern hemisphere influenza season, https://www.who.int/publications/m/item/recommended-composition-of-influenza-virus-vaccines-for-use-in-the-2024-2025-northern-hemisphere-influenza-season (2024).
Dou, D., Revol, R., Ostbye, H., Wang, H. & Daniels, R. Influenza A virus cell entry, replication, virion assembly and movement. Front. Immunol. 9, 1581 (2018).
Russell, C. A. et al. Influenza vaccine strain selection and recent studies on the global migration of seasonal influenza viruses. Vaccine 26, D31–D34 (2008).
Zost, S. J. et al. Contemporary H3N2 influenza viruses have a glycosylation site that alters binding of antibodies elicited by egg-adapted vaccine strains. Proc. Natl Acad. Sci. USA 114, 12578–12583 (2017).
USDA. Avian influenza outbreaks reduced egg production, driving prices to record highs in 2022, https://www.ers.usda.gov/data-products/chart-gallery/gallery/chart-detail/?chartId=105576 (2022).
Chen, J. R., Liu, Y. M., Tseng, Y. C. & Ma, C. Better influenza vaccines: an industry perspective. J. Biomed. Sci. 27, 33 (2020).
CDC. CDC Vaccine Price List, https://www.cdc.gov/vaccines/programs/vfc/awardees/vaccine-management/price-list/index.html (2024).
Scorza, F. B. & Pardi, N. New Kids on the Block: RNA-Based Influenza Virus Vaccines. Vaccines (Basel) 6 https://doi.org/10.3390/vaccines6020020 (2018).
NIH. COVID-19 Vaccine Development: Behind the Scenes, https://covid19.nih.gov/news-and-stories/vaccine-development (2020).
Walsh, E. E. et al. Safety and immunogenicity of two RNA-Based Covid-19 vaccine candidates. N Engl. J. Med. 383, 2439–2450 (2020).
Vogel, A. B. et al. BNT162b vaccines protect rhesus macaques from SARS-CoV-2. Nature 592, 283–289 (2021).
Polack, F. P. et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J. Med. 383, 2603–2615 (2020).
Sahin, U. et al. BNT162b2 vaccine induces neutralizing antibodies and poly-specific T cells in humans. Nature 595, 572–577 (2021).
Chen, D. et al. Epidermal powder immunization of mice and monkeys with an influenza vaccine. Vaccine 21, 2830–2836 (2003).
Carroll, T. D. et al. Efficacy of influenza vaccination of elderly rhesus macaques is dramatically improved by addition of a cationic lipid/DNA adjuvant. J. Infect. Dis. 209, 24–33 (2014).
Carroll, T. D. et al. Alphavirus replicon-based adjuvants enhance the immunogenicity and effectiveness of Fluzone (R) in rhesus macaques. Vaccine 29, 931–940 (2011).
Coe, C. L., Lubach, G. R. & Kinnard, J. Immune senescence in old and very old rhesus monkeys: reduced antibody response to influenza vaccination. Age 34, 1169–1177 (2012).
Liu, M. A., McClements, W., Ulmer, J. B., Shiver, J. & Donnelly, J. Immunization of non-human primates with DNA vaccines. Vaccine 15, 909–912 (1997).
Davis, A. S., Taubenberger, J. K. & Bray, M. The use of nonhuman primates in research on seasonal, pandemic and avian influenza, 1893-2014. Antiviral Res. 117, 75–98 (2015).
WHO. Recommended composition of influenza virus vaccines for use in the 2021-2022 northern hemisphere influenza season, https://www.who.int/publications/m/item/recommended-composition-of-influenza-virus-vaccines-for-use-in-the-2021-2022-northern-hemisphere-influenza-season (2021).
WHO. Recommended composition of influenza virus vaccines for use in the 2022-2023 northern hemisphere influenza season, https://www.who.int/publications/m/item/recommended-composition-of-influenza-virus-vaccines-for-use-in-the-2022-2023-northern-hemisphere-influenza-season (2022).
Rohde, C. M. et al. Toxicological Assessments of a Pandemic COVID-19 Vaccine-Demonstrating the Suitability of a Platform Approach for mRNA Vaccines. Vaccines 11 https://doi.org/10.3390/vaccines11020417 (2023).
Kim, A. et al. Isocitrate treatment of acute anemia of inflammation in a mouse model. Blood Cells Mol. Dis 56, 31–36 (2016).
Kim, A. et al. A mouse model of anemia of inflammation: complex pathogenesis with partial dependence on hepcidin. Blood 123, 1129–1136 (2014).
Brooks, M. B. et al. Non-lethal endotoxin injection: a rat model of hypercoagulability. PLoS ONE 12, e0169976 (2017).
Hassett, K. J. et al. Optimization of Lipid Nanoparticles for Intramuscular Administration of mRNA Vaccines. Mol. Ther. Nucleic Acids 15, 1–11 (2019).
Everds, N. E. et al. Interpreting stress responses during routine toxicity studies: a review of the biology, impact, and assessment. Toxicol Pathol. 41, 560–614 (2013).
EMA. Comirnaty EPAR Public Assessment Report, https://www.ema.europa.eu/en/documents/assessment-report/comirnaty-epar-public-assessment-report_en.pdf (2021).
Skowronski, D. M. et al. Low 2012-13 influenza vaccine effectiveness associated with mutation in the egg-adapted H3N2 vaccine strain not antigenic drift in circulating viruses. PLoS ONE 9, e92153 (2014).
Bahl, K. et al. Preclinical and clinical demonstration of immunogenicity by mRNA vaccines against H10N8 and H7N9 influenza viruses. Mol. Ther. 25, 1316–1327 (2017).
Pardi, N. et al. Nucleoside-modified mRNA immunization elicits influenza virus hemagglutinin stalk-specific antibodies. Nat. Commun. 9, 3361 (2018).
Kackos, C. M. et al. Seasonal quadrivalent mRNA vaccine prevents and mitigates influenza infection. NPJ Vaccines 8, 157 (2023).
Chivukula, S. et al. Development of multivalent mRNA vaccine candidates for seasonal or pandemic influenza. NPJ Vaccines 6, 153 (2021).
Flynn, J. A. et al. Characterization of humoral and cell-mediated immunity induced by mRNA vaccines expressing influenza hemagglutinin stem and nucleoprotein in mice and nonhuman primates. Vaccine 40, 4412–4423 (2022).
Zhuang, X. et al. mRNA Vaccines Encoding the HA Protein of Influenza A H1N1 Virus Delivered by Cationic Lipid Nanoparticles Induce Protective Immune Responses in Mice. Vaccines 8, https://doi.org/10.3390/vaccines8010123 (2020).
Xiong, F. et al. An mRNA-based broad-spectrum vaccine candidate confers cross-protection against heterosubtypic influenza A viruses. Emerg. Microbes Infect. 12, 2256422 (2023).
Petsch, B. et al. Protective efficacy of in vitro synthesized, specific mRNA vaccines against influenza A virus infection. Nat. Biotechnol. 30, 1210–1216 (2012).
Hobson, D., Curry, R. L., Beare, A. S. & Ward-Gardner, A. The role of serum haemagglutination-inhibiting antibody in protection against challenge infection with influenza A2 and B viruses. J. Hyg. 70, 767–777 (1972).
Al-Khayatt, R., Jennings, R. & Potter, C. W. Interpretation of responses and protective levels of antibody against attenuated influenza A viruses using single radial haemolysis. J. Hyg. 93, 301–312 (1984).
Corbett, K. S. et al. Evaluation of the mRNA-1273 Vaccine against SARS-CoV-2 in Nonhuman Primates. N Engl. J. Med. 383, 1544–1555 (2020).
Zhang, Z. et al. Humoral and cellular immune memory to four COVID-19 vaccines. Cell 185, 2434–2451.e2417 (2022).
Mateus, J. et al. Low-dose mRNA-1273 COVID-19 vaccine generates durable memory enhanced by cross-reactive T cells. Science 374, eabj9853 (2021).
Stevo, C. Second Quarter 2022 Earnings Teleconference, https://s28.q4cdn.com/781576035/files/doc_financials/2022/q2/Q2-2022-Earnings-Charts-FINAL.pdf (2022).
Jansen, J. M., Gerlach, T., Elbahesh, H., Rimmelzwaan, G. F. & Saletti, G. Influenza virus-specific CD4+ and CD8+ T cell-mediated immunity induced by infection and vaccination. J. Clin. Virol. 119, 44–52 (2019).
He, X. S. et al. Cellular immune responses in children and adults receiving inactivated or live attenuated influenza vaccines. J. Virol. 80, 11756–11766 (2006).
Hoft, D. F. et al. Comparisons of the humoral and cellular immune responses induced by live attenuated influenza vaccine and inactivated influenza vaccine in adults. Clin. Vaccine Immunol. 24, https://doi.org/10.1128/CVI.00414-16 (2017).
Lobby, J. L., Danzy, S., Holmes, K. E., Lowen, A. C. & Kohlmeier, J. E. Both humoral and cellular immunity limit the ability of live attenuated influenza vaccines to promote T Cell responses. J. Immunol. 212, 107–116 (2024).
Hoffmann, E., Neumann, G., Kawaoka, Y., Hobom, G. & Webster, R. G. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl Acad. Sci. USA 97, 6108–6113 (2000).
Acknowledgements
The authors would like to thank Miguel Garcia, Cindy Yang, Lei Zhang, Fanrong Kong, Shilong Li, Pengbo Guo, Adam Campbell, Lynn Phelan, Qianjing He, Herg Zhang, Sarah Cui, Ksenia Krylova, Kimberly Fernando, Patty Gu, Bhunal Patel, Bilal Aldoori, Yordin Caceres, Douglas Spraul, Amanda Wimbish, Jingrun Fan, Sandra Zeller, Patrick Findley, and Alicia Solorzano for manufacturing high quality material for use in preclinical studies. The authors would like to thank Ann Healy, Kristianne Dizon, Tara Ciolino, Arthur Illenberger, Anderson Watson, Paula Corts, Kathryn McGovern, Theresa Campbell, and Melanie Blanco who participated in dose preparation, syringe filling for dose administration, dosage instruction review, and/or sample preparation for the in vivo immunogenicity studies. The authors would like to thank Carles Martinez-Romero for contributions to HAI assay development and support. For the toxicology portions, the authors would like to thank Lila Ramaiah for clinical pathology work, Alessandro Torelli and Martina Monti at Vismederi for serology work, Lindsay Tomlinson and Rani Sellers for pathology assistance, and Gabe Webb for assistance in graphing serology data. The authors also thank Pfizer colleagues Christina D’Arco for writing and editorial support and Kayvon Modjarrad for critical review of the manuscript. The study was funded by Pfizer Inc.
Author information
Authors and Affiliations
Contributions
T.H., A.S., C.M.R., and P.S.A. wrote the manuscript. E.M., S.L., M.S.M., C.H.H., S.R., I.D., and L.F. contributed to immunogenicity study methodology and investigation. R.M.M. developed methods essential to generation of mRNA constructs and W.C., I.S., and C.U. contributed to serological assay methodologies. C.A., K.T., D.I., R.S., F.M., S.S., and K.S.E. contributed to study investigation. W.C., E.M., I.D., and L.F. contributed to immunological data curation. J.H. performed formal statistical analysis of immunological data. V.M. contributed to the analysis, curation, and investigation of toxicity data. A.V., B.M., and S.C. contributed to the analysis, curation, and visualization of toxicity data. Y.C. contributed to data visualization. A.S., P.S.A., and C.M.R. were involved in original study conceptualization, and A.S.A., P.S.A., C.M.R., V.M., W.C., I.S., K.S.E., and K.T. contributed to project supervision. All authors reviewed the work, contributed to manuscript development, and have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
All authors are current or former employees of Pfizer Inc., and may, as a consequence, be shareholders. Pfizer was involved in the design, analysis, and interpretation of the data in this research study, the writing of this report, and the decision to publish. PSA is an inventor on a patent application related to nucleoside-modified RNA LNP vaccines encoding influenza hemagglutinin.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hauguel, T., Sharma, A., Mastrocola, E. et al. Preclinical immunogenicity and safety of hemagglutinin-encoding modRNA influenza vaccines. npj Vaccines 9, 183 (2024). https://doi.org/10.1038/s41541-024-00980-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41541-024-00980-3