Abstract
Controlling foodborne pathogens in buffalo milk is crucial for ensuring food safety. This study estimated the prevalence of nine target genes representing seven critical foodborne bacteria in milk and milk products, and identified factors associated with their presence in buffalo milk chain nodes in Bangladesh. One hundred and forty-three milk samples from bulk tank milk (n = 34), middlemen (n = 37), milk collection centers (n = 37), and milk product shops (n = 35) were collected and analyzed using RT-PCR. Escherichia (E.) coli, represented through yccT genes, was the most prevalent throughout the milk chain (81–97%). Chi-squared tests were performed to identify the potential risk factors associated with the presence of foodborne bacteria encoded for different genes. At the middleman level, the prevalence of E. coli was associated with the Mymensingh, Noakhali, and Bhola districts (P = 0.01). The prevalence of Listeria monocytogenes, represented through inlA genes, and Yersinia (Y.) enterocolitica, represented through yst genes, were the highest at the farm level (65–79%). The prevalence of both bacteria in bulk milk was associated with the Noakhali and Bhola districts (P < 0.05). The prevalence of Y. enterocolitica in bulk milk was also associated with late autumn and spring (P = 0.01) and was higher in buffalo-cow mixed milk than in pure buffalo milk at the milk collection center level (P < 0.01). The gene stx2 encoding for Shiga toxin-producing (STEC) E. coli was detected in 74% of the milk products. At the middleman level, the prevalence of STEC E. coli was associated with the use of cloths or tissues when drying milk containers (P = 0.01). Salmonella enterica, represented through the presence of invA gene, was most commonly detected (14%) at the milk collection center. The use of plastic milk containers was associated with a higher prevalence of Staphylococcus aureus, represented through htrA genes, at milk product shops (P < 0.05). These results suggest that raw milk consumers in Bangladesh are at risk if they purchase and consume unpasteurized milk.
Similar content being viewed by others
Introduction
Foodborne diseases affect about 600 million people annually, resulting in 0.4 million deaths yearly, including 0.1 million children under five1. Food-producing animals may act as a reservoir for many foodborne pathogens, and food products serve as vehicles for transmitting these pathogens to humans2,3. Human infections primarily result from ingesting foodstuffs either contaminated with pathogenic microorganisms or intoxicated by microbial toxins 4. Bacteria are responsible for two-thirds of human foodborne diseases, with a relatively heavy burden affecting low and middle-income countries (LMIC)5,6,7. Foodborne diseases also have economic consequences for healthcare systems, food producers, and distributors, and require specific attention from regulatory authorities5,8. Despite the increased global awareness of foodborne infections as a threat to public health and socio-economic development, food safety requires further attention, specifically focusing on reducing pathogen spillover in LMIC.
Milk and milk products are nutritionally rich and are considered to be an important component of many healthy diets. However, if contaminated, they can be a source of pathogenic microorganisms9. Milk is a suitable growth medium for many microorganisms due to its high nutritional value stemming from its proteins, sugars, and lipid content10,11. Buffalo milk is rich in fat and protein. It is, therefore, used for ghee and cheese preparation and is well accepted by consumers12,13,14. Buffalo milk in Bangladesh has been reported to harbour many microbes, including lactic acid bacteria, spoilage, and pathogenic organisms15,16,17. Previous studies in Iran, Sweden, and Brazil have evidenced the presence of foodborne bacteria in milk from cows, sheep, and goats18,19,20. Although buffalo milk accounts for 35% of the total milk production of Asian countries21, there are limited reports22,23 estimating the prevalence of foodborne pathogens from buffalo milk in LMIC.
Bangladesh's water buffalo rearing system primarily includes free-range systems on coastal or semi-coastal islands, and a semi-intensive or intensive buffalo rearing system in the inlands. Buffalo milk trading also includes different levels of handlers, such as middlemen, milk collection centers, and milk product shops24,25. The buffalo milk chain in Bangladesh is a supply chain consisting of activities and processes including the production, processing, trading, and consumption of milk and milk products26,27. Farms are typically situated far from the milk processing centers and hygienic practices in milk handling are minimal. Consequently, when local transportation is prolonged and labor-intensive measures are required, the absence of milk cooling facilities can compromise milk safety due to potential contamination by foodborne pathogens28. Previous studies have identified zoonotic microorganisms, including Staphylococcus (S.) aureus, Escherichia (E.) coli, and enteropathogenic E. coli O157:H7 from bovine bulk milk and cheese samples29,30,31. Staphylococcus spp. are the most prevalent mastitis-causing pathogens isolated from water buffalo milk samples32,33. The enteropathogenic properties of E. coli O157:H7 are associated with enterohemorrhagic diseases in humans. Enteropathogenicity from E. coli is exhibited as Shiga toxin-producing E. coli (STEC), which corresponds mainly to the genes stx1 and stx234. Shiga toxin-producing E. coli has been identified in children, likely through household livestock fecal contamination through foodborne routes35. Campylobacter (C.) jejuni, Listeria (L.) monocytogenes, Salmonella spp., and Yersinia (Y.) enterocolitica were also previously identified in cow bulk milk and milk products30,36,37,38. Thus, water buffalo milk and milk products may be a source for transmitting foodborne pathogens to humans. Guaranteeing an adequate hygienic status at the farms and during milk handling along the stages of production is required to achieve better quality and safety in milk and milk-derived products. A considerable obstacle to adequately addressing food safety concerns is the lack of data. For example, data on the prevalence of foodborne pathogen contamination in buffalo milk and milk products, enabling policymakers to set public health priorities and allocate resources, is needed. Knowing the risk factors associated with the prevalence of foodborne pathogens may help identify effective control measures to reduce the introduction of such pathogens into the food chain and ensure the public health safety of buffalo milk consumers in Bangladesh. To meet this need, the present study aims to estimate the prevalence of nine target genes belonging to seven critical foodborne bacteria, S. aureus, E. coli, Shiga toxin-producing E. coli, C. jejuni, L. monocytogenes, Salmonella (S.) enterica, and Y. enterocolitica, using molecular methods and to identify the factors associated with these bacteria in milk and milk products along the buffalo milk chain in Bangladesh.
Results
Prevalence of foodborne bacteria along the buffalo milk chain
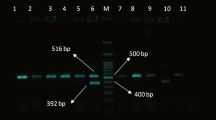
The overall prevalence of RT-PCR identified foodborne bacteria in milk and milk products was very high. Figure 1 shows that E. coli, represented through the presence of yccT genes, was the most prevalent (81–97%) pathogen in the buffalo milk chain and had an exceptionally high prevalence in farm bulk milk. The presence of STEC E. coli virulence-specific genes significantly differed (P < 0.001) along the milk chain and was higher in milk products than at the farm level. The prevalence of S. aureus, represented through htrA genes, increased along the milk chain (P = 0.08), but L. monocytogenes, represented through inlA genes, (P < 0.001) and Y. enterocolitica represented through yst genes, (P < 0.001) decreased along the milk chain and were extremely high in farm bulk milk. The prevalence of S. enterica, represented through invA genes, was low at the farm and middleman levels (0–3%) but higher at the milk collection center level (14%). C. jejuni, represented through cadF genes, was absent in all samples.
The prevalence of target genes for most of the foodborne bacteria was very high in the buffalo milk chain in Bangladesh. Figures show the prevalence of the RT-PCR identified target genes for foodborne bacteria from the milk and milk product samples (N = 143) collected from six districts in Bangladesh with a high density of buffalo. The P value was obtained from a chi-squared test by comparing each pathogen prevalence from the samples from four buffalo milk chain nodes (farm bulk milk, middleman, milk collection center, and milk product).
Factors associated with the prevalence of foodborne bacteria in the buffalo milk chain
Several factors were associated with the higher prevalence of foodborne bacteria at buffalo milk chain nodes. Importantly, bulk milk from the buffalo farms in the Noakhali and Bhola districts had a higher prevalence of genes for L. monocytogenes and Y. enterocolitica than in the other districts (P < 0.05). The prevalence of yst genes for Y. enterocolitica was higher in late autumn and spring compared to winter (P = 0.01). One variable, “Keep bulk milk containers open” had a single missing value (Table 1). At the middleman level, three variables, “Type of container”, “Type of trader”, and “How the container is dried,” had missing values ranging between 3 and 16%. The prevalence of yccT genes for E. coli was higher in the Mymensingh, Noakhali, and Bhola districts than in Rajshahi and Jamalpur. The milk containers that were dried using cloths or tissues had a higher prevalence of genes for STEC E. coli than for sun-dried containers (Table 2). At the milk collection center level, one variable, “Nature of milk,” had a single missing value. The prevalence of yst genes for Y. enterocolitica was higher in buffalo-cow mixed milk than in homogeneous buffalo milk. In the milk products, plastic milk containers had a higher prevalence of htrA genes for S. aureus than earthenware and glass-made containers (Table 3).
Discussion
Our study aimed to estimate the prevalence of and identify the risk factors associated with the presence of RT-PCR identified foodborne bacteria, namely S. aureus, E. coli, STEC E. coli, L. monocytogenes, Y. enterocolitica, S. enterica, and C. jejuni, in the water buffalo milk chain in Bangladesh. The prevalence of yccT genes for E. coli was high in farm bulk milk and decreased very little over the buffalo milk chains in our study. This is consistent with our previous study, which demonstrated the progressive increase of overall Enterobacteriaceae count in the water buffalo milk chain in Bangladesh25. E. coli is often used as an indicator of fecal contamination and is often regarded as commensal rather than pathogenic. However, high contamination levels of pathogenic E. coli can also influence pathogen colonization, leading to an increase in disease severity39,40, and may disseminate antimicrobial resistance genes41,42; thus, it should be considered a health hazard when consuming raw milk or milk products. The prevalence of E. coli in composite buffalo milk was shown to vary between 33 to 67% in earlier studies in Iraq43, Egypt44, and Indonesia45, which is comparatively lower than in our study. These studies used bacterial culture to represent the proportion of live bacteria, and the prevalence may be relatively lower than when detected using RT-PCR without culture. Sample type may be another source of variation for the relatively lower prevalence of E. coli in these studies, as bulk milk could be more likely to be contaminated by external contaminants from the environment than composite milk; however, no information was found on the minorly decreasing prevalence of E. coli in the buffalo milk chain, e.g., at the middleman or milk collection centre levels. This can partly be explained by the fact that previous studies in Italy showed that the freezing of raw milk and the heat treatment applied during stretching for Mozzarella cheese preparation may reduce E. coli contamination in milk products46,47. We, therefore, suggest that enforcing rules to maintain the cold chain could help reduce E. coli contamination in the buffalo milk chain.
In this study, the prevalence of STEC E. coli virulence genes eae, stx1, and stx2 increased along the buffalo milk chain; the prevalence of stx2 was especially high in farms (50%) and milk products (74%). However, the prevalence of STEC E. coli was reasonably low in studies of water buffalo quarter milk in Turkey (1.4%) and Italy (0.6%)48,49. No previous study has evidenced the prevalence of STEC E. coli virulence genes in bulk milk in water buffalo. A recent survey in Bangladesh demonstrated a higher prevalence of stx1, stx2, and eae (40–57%) in cattle, poultry, and diarrheal human patients50. The present study found that the prevalence of STEC E. coli was higher in Noakhali and Bhola districts, where free-range buffalo rearing is more common. In buffalo farms in a free-ranging system, buffalo, cattle, sheep, and sometimes chickens and ducks are often reared in the same farm area. Moreover, buffalo farm workers mostly live close to the farm boundary. Therefore, there may be a risk of the spillover of foodborne bacteria carrying these virulence genes when humans have close interactions with livestock species. Plastic milk containers and milk handling at the middleman level were associated with a higher prevalence of E. coli O157:H7 in dairy cows51, confirming our findings. Plastic milk containers are more challenging to clean than glass or stainless-steel ones, and spoilt milk from the day before can easily be contaminated with pathogenic microorganisms. Using cloths or tissues to dry containers was more often related to a higher prevalence of STEC E. coli than sun-drying. The cloths used to clean and wipe the containers were unclean and frequently used without washing the containers in between. Occasionally, the staff used the cloths for their own personal use, meaning that they could contaminate milk during shipment if overused.
The prevalence of htrA genes of S. aureus in our study ranged between 9 and 31%, increasing along the buffalo milk chain. A recent study in Bangladesh has also reported an increasing level of S. aureus along the water buffalo milk chain15,25. In dairy cows, previous studies have shown that the prevalence of S. aureus was higher in cheese (33–40%) than in bulk milk (13–25%)52,53. The presence of S. aureus in bulk milk might be due to clinical or subclinical mastitis or unhygienic handling and milk processing54. Milk container material and drying methods were found to be risk factors for the presence of htrA genes of S. aureus at the middleman and milk product shop levels. The increasing S. aureus contamination levels at the middleman and milk product shop levels in the current study may be the outcome of the poor hygiene conditions practiced by middlemen and at collection centers during the handling of milk, as well as an insufficient cold chain that supports the exponential growth of previously introduced microorganisms at the milk producer level.
The prevalence of inlA genes of L. monocytogenes and yst genes of Y. enterocolitica was high in the buffalo farms but lower later in the milk chain. The prevalence of inlA genes for L. monocytogenes in this study (65%) is much higher than in water buffalo bulk milk in Pakistan, Egypt, and Brazil (0–8%)22,55,56. There were no reports on prevalence along the milk chain for these countries. However, this finding is consistent with the previous studies in dairy cows, which demonstrated that the prevalence of L. monocytogenes was higher in raw bulk milk (19–40%) than in traditional milk products, such as, yogurt, butter, and cheese (1–8%)57,58. Unlike many bacteria, Listeria may survive with exponential growth rates in low temperatures, ranging from 0 to 5 °C, but will start decreasing at 13 °C59. Therefore, the absence of a cold chain seems beneficial for reducing the prevalence of L. monocytogenes later in the milk chain in water buffalo in Bangladesh. Listeria may also survive in the natural environment, can be widely distributed in soil, and can contaminate roughage60,61. Water buffalo in Bangladesh primarily rely on grazing and often consume green roughage, which may be contaminated by soil. Thus, contamination might potentially occur in the bulk tank if the container is left open, contributing to the elevated prevalence of L. monocytogenes in the farm's bulk milk. In previous studies, the prevalence of Y. enterocolitica was also higher in the bulk milk from water buffalo (25%) than in milk products, such as commercial or traditional cheese and yogurt (0–12%)62,63, which is consistent with our study. We found that the prevalence of yst genes in Y. enterocolitica in bulk milk was higher in late autumn and spring. This may be linked to contamination during manual milk handling on farms in combination with favourable environmental conditions for the pathogen, given that the ambient temperature during late autumn and spring remains above 20 °C. An earlier study reported that Y. enterocolitica did not grow at a low pH (< 4.5) or in temperatures ranging from 5 to 19 °C64. Processing traditional buffalo milk products likely increases the acidity of the milk products, which may reduce the contamination level of Y. enterocolitica in buffalo milk products62,63.
S. enterica, represented through invA genes, was incredibly low (0–3%) at the farm and middleman level, and C. jejuni, represented through cadF genes, was absent in all the samples throughout the buffalo milk chain. It may be suggested that raw milk and milk production from the water buffalo milk chain is safe from contamination by C. jejuni in Bangladesh. These findings are consistent with a previous study of Bangladesh's dairy cow milk chain, which showed no evidence of Salmonella spp. or C. jejuni65. However, another recent study conducted in Ethiopia by Geletu et al.66 revealed that the prevalence of Salmonella spp. in bulk milk and milk collection centers ranged from 10 to 20% for dairy cows. This prevalence was higher than Brazil and India's 0% to 4% in buffalo milk22,23 and was comparable with our study. The prevalence of C. jejuni was mainly reported in bulk milk from dairy cows, ranging from 3 to 20% in different countries, including Italy, Tanzania, and Egypt67,68,69. However, there are limited studies for water buffalo, although Serraino et al.69 reported the absence of C. jejuni in water buffalo farms in Italy. No significant risk factors were identified for this study's higher prevalence of invA genes of S. enterica. However, a higher prevalence of Y. enterocolitica at the milk collection center level was more associated with cow-buffalo mixed milk than with pure buffalo milk. This finding is also consistent with a previous study25, indicating that combining milk from different sources may increase bacterial contamination in water buffalo milk in Bangladesh. Researchers have attempted to explore the implications of contamination for food safety. A study in South Korea describes an awareness survey and demonstrates that bacterial contamination and somatic cell counts were lower and milk solids, such as protein and fat content, were significantly higher in HACCP-certified farms than in non-certified farms70. Therefore, attention payed to the HACCP certification of farmers could help identify barriers to milk quality and contribute to a more sustainable and hygienic milk supply chain.
Our study found that the district of origin could be a risk factor, with the bulk milk samples collected from the Bhola district having a high prevalence of STEC, Y. enterocolitica, and L. monocytogenes (80–100%). This may be because free-range rearing relies primarily on grazing, which contaminates soil, and the farms in this district’s inferior transport facilities and remote locations require longer transportation time. Furthermore, milk handling hygiene was often poor. However, only a univariable analysis could be performed in this study because of the small number of samples analyzed for each sample type. Therefore, a further large-scale study is necessary to assess a more comprehensive number of variables to identify the most effective management practices for reducing foodborne pathogen contamination in Bangladesh's water buffalo milk chain.
This study estimated the prevalence of foodborne bacteria by detecting the selected genes which indicate the presence of various bacteria. However, confirmation by bacteriological culture is required to confirm the presence of viable bacteria in the samples. This is a limitation of our work, and studies using bacteriological culture are needed to overcome this limitation. Still, we feel that the variation in the prevalence of bacteria based on the detection of DNA through PCR is informative of which nodes in the dairy chain are most crucial. In addition, a negative PCR is likely to reflect the absence of viable bacteria, as the sensitivity of PCR is generally higher than for bacteriological culture71,72. The use of direct DNA extraction followed by PCR allows for a more rapid identification of targeted bacteria than bacteriological culture and is thus valuable for the almost real-time monitoring of the presence of bacteria in samples, but culture data is needed to confirm the actual human health hazards.
Conclusions
Our findings give an indication that several potential human pathogenic bacteria, including STEC and S. aureus, are circulating throughout the buffalo milk chain in Bangladesh. This creates a major risk to public health and necessitates the establishment of suitable interventions in future studies. Targeted genes for foodborne bacteria are present at higher levels, starting at the farm level and increasing in the milk collection centers in the buffalo milk chain. Therefore, pathogenic bacteria in milk can be reduced by employing hygienic milking practices, replacing plastic milk containers with glass or stainless steel, and halting the use of dirty cloths when cleaning containers. Temperature-controlled milk containers could be introduced to reduce bacterial multiplication during transportation by middlemen. A small-scale pasteurization and chilling plant could be established at the milk collector level; this would effectively destroy pathogenic organisms that survive at low temperatures, such as L. monocytogenes and Y. enterocolitica. Finally, regular monitoring is required for the presence of foodborne bacteria. Pasteurization is recommended for raw milk to ensure the milk products are of better quality and to ensure the safety of consumers.
Materials and methods
Study design
This cross-sectional study was conducted between February 2020 and April 2021 at four buffalo milk chain nodes (farm, middleman, milk collection center, and milk product shop) in six districts in Bangladesh (Noakhali, Bhola, Moulvibazar, Mymensingh, Jamalpur, and Rajshahi). The list of farmers was created with the help of the Upazilla Veterinary Hospital (UVH) and a non-governmental organization named the Palli Karma-Sahayak Foundation working with buffalo farmers in Bangladesh. The study was approved by the Sylhet Agricultural University Research System (SAU/Ethical Committee/AUP/21/06) at the Sylhet Agricultural University, Bangladesh, and all methods were performed following the relevant guidelines and regulations. The buffalo farmers gave written informed consent, and middlemen, the managers of milk collection centers, and milk product shop owners gave oral consent before participating in this study. A list was created by collecting data on the numbers of buffalo farmers and local buffalo milk product shops at each study location, described in two previous studies in this project25,73. From there, the farms, middlemen, milk collection centers, and milk product shops were randomly recruited for this study based on the sample size estimation. The sample size was calculated at a 50% prevalence with a 95% confidence and an absolute margin of error of 0.1074. This required 35 samples, including 10 additional samples for each type of milk chain sample. Table 4 shows how 143 samples were collected, comprising 108 milk samples from three different milk chain nodes (farm, middleman, and milk collection center) and 35 milk products (yogurt, cheese, and buttermilk) from the milk product shops.
Questionnaire data collection
A questionnaire was developed and divided into four subsections to determine the risk factors associated with the foodborne bacteria related to the buffalo milk chain nodes. Section A captured data at the farm level and included 45 questions. Sections B and C contained 20 questions and collected information from the middlemen and collection centers. Section D included eight questions aimed at gathering information about the milk products, such as the origin of milk, storage time, and the type of containers used. The questionnaire has been detailed in a previous study in this project25 and is given as a supplementary file (S1).
Collection of samples
One hundred and forty-three milk samples were used in this study, where each bulk milk sample was comprised of milk from all the lactating cows in each buffalo farm (n = 34). Two milk samples were collected aseptically at each milk collection center, one before mixing (middleman) (n = 37) and another one after mixing (n = 37). Milk product samples, such as yogurt, cheese, and buttermilk (n = 35), were also collected from the study areas. Samples from the middlemen, milk collection centers, and milk product shops were taken on the same date but were not linked with the source buffalo farm. From each milk sample (bulk milk from farms, middlemen, and milk collection centers), an aliquot of 10 mL and 30–35 g of milk product were aseptically collected in 15 mL and 50 mL falcon tubes, respectively. The sample collection procedure has been described in an earlier study25. Upon arrival at the laboratory, the samples were stored on ice immediately and then at − 20 °C.
Genomic DNA extraction and purification
The milk and milk product samples were subjected to DNA extraction in the Microbial Genetics and Bioinformatics Laboratory, Department of Microbiology, University of Dhaka, Dhaka 1000, Bangladesh. Genomic DNA (gDNA) extraction was performed using a Maxwell® 16 Cell DNA Purification Kit (Promega, UK) with the Maxwell® 16 Instrument platform (Promega, UK). One mL milk sample was centrifuged at 16,000 rcf for 10 min75,76. Then, the 200µL of pellet was used for DNA extraction according to the manufacturer’s instructions. For milk products, a 200 mg sample was used for the DNA extraction, following manufacturer instructions as previously described16,75. The DNA samples were eluted in a 200 μL elution buffer (Promega, UK) and were stored at − 20 °C until further processing. DNA concentration and purity were analyzed using a NanoDrop 2000 Spectrophotometer (Thermo Fisher Scientific, Waltham, Massachusetts, USA) at a wavelength of 260 nm and A260/A280, respectively. DNA samples were considered appropriate for downstreaming if the DNA concentration was ≥ 9 ng/ µL and they had a 260/280 absorbance ratio (> 1.6 to ≤ 2). Then, the DNA samples were delivered to the Molecular Pathology Laboratory, Department of Veterinary and Animal Sciences (DIVAS), Università degli Studi di Milano (UNIMI), Italy.
Real-time polymerase chain reaction
Quantitative real-time PCR was carried out using gene-specific primers targeting the examined microbes (Table 5). These primers were selected due to their specificity as described in previous publications77,78. Quantitative PCR followed MIQE guidelines79 in a final reaction volume of 15 µL using the CFX 96 System (Bio-Rad Laboratories, USA). Each reaction volume contained 7.5µL of 2× Mix EVA Green (SsoFast EvaGreen® Supermix, Bio-Rad Laboratories, USA) and primers specific to the target genes. The PCR reaction was carried out using the same thermal profile for all targets (2 min at 50 °C, 3 min at 95 °C, and 39 cycles of 10 s at 95 °C and 30 s at 60 °C). To assess melting curves, PCR products were incubated at 55 °C for 60 s, and then the temperature was increased to 95 °C at 0.5 °C increments every 10 s. The PCR efficiencies were determined using four-fold serial dilutions of DNA prepared from ATCC strains of the bacteria of interest, such as S. aureus ATCC 19048, E. coli ATCC 11229, E. coli O157:H7 ATCC 35150 (positive for eae (Intimin); stx1 (Shiga toxin 1) positive; stx2 (Shiga toxin 2) positive), L. monocytogenes ATCC 13932, Y. enterocolitica DSM 4780, S. enterica ATCC 13076, and C. jejuni ATCC 33291. ATCC and DSM bacterial strains were obtained from the American-type culture collection (MD, USA) and the German collection of microorganisms and cell cultures (Braunschweig, Germany). No template controls were included in the assays. The results were analyzed using Bio-Rad CFX Maestro 1.0 software (Bio-Rad Laboratories, USA), and the samples with a threshold of CT < 35 cycles were considered positive for the presence of the targeted genes.
Statistical analysis
Data analysis was performed using R (version 4.3.1; R Foundation for Statistical Computing, Vienna, Austria). The presence of the targeted genes (htrA/ yccT/ eae/ stx1/ stx2/ inlA/ yst/ invA/ cadF) was a binary outcome variable (yes or no). The prevalence of STEC E. coli was calculated based on whether at least one of the entero- and shiga-toxin genes (eae/ stx1/ stx2) was present. The prevalence of each pathogen was calculated for each of the milk chain nodes, namely bulk milk, middlemen, milk collection centers, and milk products, by dividing the total number of positives by the total number of samples tested. A chi-squared test was performed to analyse the difference in the prevalence of each pathogen between the four different milk chain nodes. For categorical questionnaire variables, a Fisher’s exact test was performed to compare the difference between the categories of a variable for each RT-PCR positive pathogen. Variables with a P ≤ 0.1 were presented with a prevalence of RT-PCR positive foodborne bacteria and corresponding P-values.
Data availability
The dataset used or analyzed in this study will be made available through github link https://github.com/shuvosingha/water-buffalo-foodborne-pathogens-in-Bangladesh upon publication.
References
WHO. (World Health Organization, 2022).
Heredia, N. & García, S. Animals as sources of food-borne pathogens: A review. Anim. Nutr. 4, 250–255. https://doi.org/10.1016/j.aninu.2018.04.006 (2018).
Qiu, Y. et al. Global prioritization of endemic zoonotic diseases for conducting surveillance in domestic animals to protect public health. Philos. Trans. Biol. Sci. 378, 20220407. https://doi.org/10.1098/rstb.2022.0407 (2023).
Addis, M. & Sisay, D. A review on major food borne bacterial illnesses. J. Trop. Dis. Public Health 3, 1–7 (2015).
Abebe, E., Gugsa, G. & Ahmed, M. Review on major food-borne zoonotic bacterial pathogens. J. Trop. Med. 2020, 4674235. https://doi.org/10.1155/2020/4674235 (2020).
Singha, S., Thomas, R., Viswakarma, J. N. & Gupta, V. K. Foodborne illnesses of Escherichia coli O157origin and its control measures. J. Food Sci. Technol. 60, 1274–1283. https://doi.org/10.1007/s13197-022-05381-9 (2023).
Sirimanapong, W., Phước, N. N., Crestani, C., Chen, S. & Zadoks, R. N. Geographical, temporal and host-species distribution of potentially human-pathogenic group B Streptococcus in aquaculture species in southeast Asia. Pathogens https://doi.org/10.3390/pathogens12040525 (2023).
CDC. (National center for emerging and zoonotic infectious diseases (NCEZID), Division of foodborne, waterborne, and environmental diseases (DFWED), Centers for Disease Control and Phererevention, 2021).
Sonnier, J. L. et al. Prevalence of Salmonella enterica, Listeria monocytogenes, and pathogenic Escherichia coli in bulk tank milk and milk filters from US dairy operations in the National Animal Health Monitoring System Dairy 2014 study. J. Dairy Sci. 101, 1943–1956. https://doi.org/10.3168/jds.2017-13546 (2018).
Monnet, C., Landaud, S., Bonnarme, P. & Swennen, D. Growth and adaptation of microorganisms on the cheese surface. FEMS Microbiol. Lett. 362, 1–9. https://doi.org/10.1093/femsle/fnu025 (2015).
Yuan, L., Sadiq, F. A., Burmølle, M., Wang, N. & He, G. Insights into psychrotrophic bacteria in raw milk: A review. J. Food Prot. 82, 1148–1159. https://doi.org/10.4315/0362-028X.JFP-19-032 (2019).
Vasile, F. E. et al. Exploring the sensory properties of buffalo (Bubalus bubalis) milk custards through a consumer-based study performed with children. Int. J. Dairy Technol. 76, 252–260. https://doi.org/10.1111/1471-0307.12916 (2023).
Pathania, P., Sharma, V., Rao, P. S., Arora, S. & Panjagari, N. R. A distinction of cow and buffalo ghee using principal component analysis of triglyceride composition. Int. J. Dairy Technol. 74, 352–358. https://doi.org/10.1111/1471-0307.12768 (2021).
Gawande, H., Arora, S., Sharma, V., Meena, G. S. & Singh, A. K. Effect of milk protein standardisation using buffalo milk protein co-precipitates on the texture, composition and yield of paneer. Int. J. Dairy Technol. 76, 650–658. https://doi.org/10.1111/1471-0307.12975 (2023).
Hoque, M. N. et al. Antibiogram and virulence profiling reveals multidrug resistant Staphylococcus aureus as the predominant aetiology of subclinical mastitis in riverine buffalo. Vet. Med. Sci. https://doi.org/10.1002/vms3.942 (2022).
Islam, S. M. R. et al. Insights into the nutritional properties and microbiome diversity in sweet and sour yogurt manufactured in Bangladesh. Sci. Rep. 11, 22667. https://doi.org/10.1038/s41598-021-01852-9 (2021).
Tanzina, A. Y. et al. Investigating the nutritional profile and bacteriome diversity in Bangladeshi sour yogurt. Biocatal. Agric. Biotechnol. 44, 102451. https://doi.org/10.1016/j.bcab.2022.102451 (2022).
Artursson, K., Schelin, J., Thisted Lambertz, S., Hansson, I. & Olsson Engvall, E. Foodborne pathogens in unpasteurized milk in Sweden. Int. J. Food Microbiol. 284, 120–127. https://doi.org/10.1016/j.ijfoodmicro.2018.05.015 (2018).
Aragão, B. B. et al. Multiresistant zoonotic pathogens isolated from goat milk in Northeastern Brazil. Compar. Immunol. Microbiol. Infect. Dis. 79, 101701. https://doi.org/10.1016/j.cimid.2021.101701 (2021).
Rahimi, E., Doosti, A., Ameri, M., Kabiri, E. & Sharifian, B. Detection of Coxiella burnetii by nested PCR in bulk milk samples from dairy bovine, ovine, and caprine herds in Iran. Zoonoses Public Health 57, e38-41. https://doi.org/10.1111/j.1863-2378.2009.01289.x (2010).
Minervino, A. H., Zava, M., Vecchio, D. & Borghese, A. Bubalus bubalis: A short story. Front. Vet. Sci. 7, 570413. https://doi.org/10.3389/fvets.2020.570413 (2020).
Godinho, F. M. S. et al. Microbiological and physicochemical characteristics of buffalo milk used for dairy products in southern Brazil. J. Dairy Res. 87, 463–468. https://doi.org/10.1017/s002202992000093x (2020).
Khan, J. A. et al. Assessment of foodborne bacterial pathogens in buffalo raw milk using polymerase chain reaction based assay. Foodborne Pathog. Dis. 19, 750–757. https://doi.org/10.1089/fpd.2022.0044 (2022).
Hamid, M. A., Ahmed, S., Rahman, M. A. & Hossain, K. M. Status of buffalo production in Bangladesh compared to SAARC countries. Asian J. Anim. Sci. 10, 313–329. https://doi.org/10.3923/ajas.2016.313.329 (2016).
Singha, S. et al. Factors influencing somatic cell counts and bacterial contamination in unpasteurized milk obtained from water buffalo in Bangladesh. Trop. Anim. Health Prod. 55, 242. https://doi.org/10.1007/s11250-023-03644-x (2023).
Habib, M. R. et al. Status of the buffalo milk trade and dairy manufacturing business at Bhola district of Bangladesh, and opportunities for buffalo milk products branding. Res. Agric. Livestock Fish. 8, 301–310 (2021).
Samad, M. A systematic review of research findings on buffalo health and production published during the last six decades in Bangladesh. J. Vet. Med. One Health Res. 2, 1–62. https://doi.org/10.36111/jvmohr.2020.2(1).0016 (2020).
Habib, M. R. et al. Dairy buffalo production scenario in Bangladesh: A review. Asian J. Med. Biol. Res. 3, 305–316. https://doi.org/10.3329/ajmbr.v3i3.34518 (2017).
Boss, R. et al. Bovine Staphylococcus aureus: Subtyping, evolution, and zoonotic transfer. J. Dairy Sci. 99, 515–528. https://doi.org/10.3168/jds.2015-9589 (2016).
Jaakkonen, A. et al. Longitudinal study of Shiga toxin-producing Escherichia coli and Campylobacter jejuni on Finnish Dairy Farms and in Raw Milk. Appl. Environ. Microbiol. https://doi.org/10.1128/aem.02910-18 (2019).
Guzman-Hernandez, R. et al. Mexican unpasteurised fresh cheeses are contaminated with Salmonella spp., non-O157 Shiga toxin producing Escherichia coli and potential uropathogenic E. coli strains: A public health risk. Int. J. Food Microbiol. 237, 10–16. https://doi.org/10.1016/j.ijfoodmicro.2016.08.018 (2016).
Patel, R., Kunjadia, P., Koringa, P., Joshi, C. & Kunjadiya, A. Microbiological profiles in clinical and subclinical cases of mastitis in milking Jafarabadi buffalo. Res. Vet. Sci. 125, 94–99. https://doi.org/10.1016/j.rvsc.2019.05.012 (2019).
Dhakal, I. P., Dhakal, P., Koshihara, T. & Nagahata, H. Epidemiological and bacteriological survey of buffalo mastitis in Nepal. J. Vet. Med. Sci. 69, 1241–1245. https://doi.org/10.1292/jvms.69.1241 (2007).
Desmarchelier, P. & Fegan, N. Reference Module in Food Science (Elsevier Health Sciences, 2016).
Lambrecht, N. J. et al. Ruminant-related risk factors are associated with shiga toxin-producing Escherichia coli infection in children in southern Ghana. Am. J. Trop. Med. Hyg. 106, 513–522. https://doi.org/10.4269/ajtmh.21-0550 (2021).
Raeisi, M. et al. Antimicrobial resistance and virulence-associated genes of Campylobacter spp. isolated from raw milk, fish, poultry, and red meat. Microb. Drug Resist. 23, 925–933. https://doi.org/10.1089/mdr.2016.0183 (2017).
Diriba, K., Awulachew, E. & Diribsa, K. The prevalence of Listeria species in different food items of animal and plant origin in Ethiopia: A systematic review and meta-analysis. Eur. J. Med. Res. 26, 60. https://doi.org/10.1186/s40001-021-00532-8 (2021).
Gebeyehu, A., Taye, M. & Abebe, R. Isolation, molecular detection and antimicrobial susceptibility profile of Salmonella from raw cow milk collected from dairy farms and households in southern Ethiopia. BMC Microbiol. 22, 84. https://doi.org/10.1186/s12866-022-02504-2 (2022).
Richter, T. K. S. et al. Responses of the human gut Escherichia coli population to pathogen and antibiotic disturbances. Microb. Syst. https://doi.org/10.1128/mSystems.00047-18 (2018).
Mohamed, M. et al. Extraintestinal pathogenic and antimicrobial-resistant Escherichia coli contamination of 56 public restrooms in the greater Minneapolis-St. Paul Metropolitan Area. Appl. Environ. Microbiol. 81, 4498–4506. https://doi.org/10.1128/aem.00638-15 (2015).
Bachmann, L. et al. Colostrum as a source of ESBL-Escherichia coli in feces of newborn calves. Sci. Rep. 14, 9929. https://doi.org/10.1038/s41598-024-60461-4 (2024).
Mendonça, R. et al. Raw milk cheeses from Beira Baixa, Portugal—A contributive study for the microbiological hygiene and safety assessment. Brazil. J. Microbiol. https://doi.org/10.1007/s42770-024-01332-y (2024).
Sadeq, J. N., Fahed, K. H. & Hassan, H. J. Detection of Escherichia coli hlyA gene and Staphylococcus aureus Sea gene in raw milk of buffaloes using RT-PCR technique in AL- Qadisiyah province. Iraqi J. Vet. Sci. 32, 87–91. https://doi.org/10.33899/ijvs.2018.153815 (2018).
Fahim, K. M., Ismael, E., Khalefa, H. S., Farag, H. S. & Hamza, D. A. Isolation and characterization of E. coli strains causing intramammary infections from dairy animals and wild birds. Int. J. Vet. Sci. Med. 7, 61–70. https://doi.org/10.1080/23144599.2019.1691378 (2019).
Bauzad, M., Yuliati, F. N., Prahesti, K. I. & Malaka, R. IOP Conference Series: Earth and Environmental Science. 012027 (IOP Publishing).
Trevisani, M., Mancusi, R. & Valero, A. Thermal inactivation kinetics of Shiga toxin-producing Escherichia coli in buffalo Mozzarella curd. J. Dairy Sci. 97, 642–650. https://doi.org/10.3168/jds.2013-7150 (2014).
Biondi, L. et al. Impact of freezing on the microbiological quality and physical characteristics of buffalo mozzarella cheese. Animals https://doi.org/10.3390/ani11123502 (2021).
Lorusso, V. et al. Verocytotoxin-producing Escherichia coli O26 in raw water buffalo (Bubalus bubalis) milk products in Italy. J. Food Prot. 72, 1705–1708. https://doi.org/10.4315/0362-028x-72.8.1705 (2009).
Seker, E. & Yardimci, H. First isolation of Escherichia coli O157:H7 from faecal and milk specimens from anatolian water buffaloes (Bubalus bubalus) in Turkey. J. S. Afr. Vet. Assoc. 79, 167–170. https://doi.org/10.4102/jsava.v79i4.267 (2008).
Parvej, M. S. et al. Prevalence of virulence genes of diarrheagenic Escherichia coli in fecal samples obtained from cattle, poultry and diarrheic patients in Bangladesh. Jpn. J. Infect. Dis. 73, 76–82. https://doi.org/10.7883/yoken.JJID.2019.016 (2020).
Disassa, N., Sibhat, B., Mengistu, S., Muktar, Y. & Belina, D. Prevalence and antimicrobial susceptibility pattern of E. coli O157:H7 isolated from traditionally marketed raw cow milk in and around Asosa town, western Ethiopia. Vet. Med. Int. 2017, 7581531. https://doi.org/10.1155/2017/7581531 (2017).
Alghizzi, M. & Shami, A. The prevalence of Staphylococcus aureus and methicillin resistant Staphylococcus aureus in milk and dairy products in Riyadh, Saudi Arabia. Saudi J. Biol. Sci. 28, 7098–7104. https://doi.org/10.1016/j.sjbs.2021.08.004 (2021).
Lemma, F., Alemayehu, H., Stringer, A. & Eguale, T. Prevalence and antimicrobial susceptibility profile of Staphylococcus aureus in milk and traditionally processed dairy products in Addis Ababa, Ethiopia. BioMed Res. Int. 2021, 5576873. https://doi.org/10.1155/2021/5576873 (2021).
Pyz-Łukasik, R., Paszkiewicz, W., Tatara, M. R., Brodzki, P. & Bełkot, Z. Microbiological quality of milk sold directly from producers to consumers. J. Dairy Sci. 98, 4294–4301. https://doi.org/10.3168/jds.2014-9187 (2015).
Munir, M. Z., Khan, J. A., Ijaz, M. & Akhtar, F. First substantiation of clinico-molecular investigation of pathogenic Listeria monocytogenes in Nili-Ravi buffaloes. Iran. J. Vet. Res. 23, 120–127. https://doi.org/10.22099/ijvr.2022.41671.6062 (2022).
Osman, K. M. et al. Determination of virulence and antibiotic resistance pattern of biofilm producing Listeria species isolated from retail raw milk. BMC Microbiol. 16, 263. https://doi.org/10.1186/s12866-016-0880-7 (2016).
Seyoum, E. T., Woldetsadik, D. A., Mekonen, T. K., Gezahegn, H. A. & Gebreyes, W. A. Prevalence of Listeria monocytogenes in raw bovine milk and milk products from central highlands of Ethiopia. J. Infect. Dev. Ctries. 9, 1204–1209. https://doi.org/10.3855/jidc.6211 (2015).
Akrami-Mohajeri, F. et al. The prevalence and antimicrobial resistance of Listeria spp in raw milk and traditional dairy products delivered in Yazd, central Iran (2016). Food Chem. Toxicol. 114, 141–144. https://doi.org/10.1016/j.fct.2018.02.006 (2018).
Buchanan, R. L. & Klawitter, L. A. Effect of temperature history on the growth of Listeria monocytogenes Scott A at refrigeration temperatures. Int. J. Food Microbiol. 12, 235–245. https://doi.org/10.1016/0168-1605(91)90074-y (1991).
Liu, D., Lawrence, M. L., Ainsworth, A. J. & Austin, F. W. Comparative assessment of acid, alkali and salt tolerance in Listeria monocytogenes virulent and avirulent strains. FEMS Microbiol. Lett. 243, 373–378. https://doi.org/10.1016/j.femsle.2004.12.025 (2005).
Waak, E., Tham, W. & Danielsson-Tham, M. L. Prevalence and fingerprinting of Listeria monocytogenes strains isolated from raw whole milk in farm bulk tanks and in dairy plant receiving tanks. Appl. Environ. Microbiol. 68, 3366–3370. https://doi.org/10.1128/aem.68.7.3366-3370.2002 (2002).
Rahimi, E., Sepehri, S., Dehkordi, F. S., Shaygan, S. & Momtaz, H. Prevalence of Yersinia species in traditional and commercial dairy products in Isfahan province, Iran. Jundishapur J. Microbiol. https://doi.org/10.5812/jjm.9249 (2014).
Darwish, S. F., Asfour, H. A. & Allam, H. A. Incidence of Yersinia enterocolitica and Yersinia pseudotuberculosis in raw milk samples of different animal species using conventional and molecular methods. Alex. J. Vet. Sci. 44, 174–185. https://doi.org/10.5455/ajvs.176360 (2015).
Bhaduri, S., Buchanan, R. L. & Phillips, J. G. Expanded response surface model for predicting the effects of temperatures, pH, sodium chloride contents and sodium nitrite concentrations on the growth rate of Yersinia enterocolitica. J. Appl. Bacteriol. 79, 163–170. https://doi.org/10.1111/j.1365-2672.1995.tb00930.x (1995).
Islam, M. A. et al. Microbiological quality assessment of milk at different stages of the dairy value chain in a developing country setting. Int. J. Food Microbiol. 278, 11–19. https://doi.org/10.1016/j.ijfoodmicro.2018.04.028 (2018).
Geletu, U. S., Usmael, M. A. & Ibrahim, A. M. Isolation, identification, and susceptibility profile of E. coli, Salmonella, and S. aureus in dairy farm and their public health implication in Central Ethiopia. Vet. Med. Int. 2022, 1887977. https://doi.org/10.1155/2022/1887977 (2022).
Kashoma, I. P. et al. Prevalence and antimicrobial resistance of campylobacter isolated from dressed beef carcasses and raw milk in Tanzania. Microb. Drug Resist. 22, 40–52. https://doi.org/10.1089/mdr.2015.0079 (2016).
El-Zamkan, M. A. & Hameed, K. G. Prevalence of Campylobacter jejuni and Campylobacter coli in raw milk and some dairy products. Vet. World 9, 1147–1151. https://doi.org/10.14202/vetworld.2016.1147-1151 (2016).
Serraino, A. et al. Presence of Campylobacter and Arcobacter species in in-line milk filters of farms authorized to produce and sell raw milk and of a water buffalo dairy farm in Italy. J. Dairy Sci. 96, 2801–2807. https://doi.org/10.3168/jds.2012-6249 (2013).
Chon, J.-W. et al. Strategies for expanding HACCP certification rate using an awareness survey of dairy farmers. Int. J. Dairy Technol. 74, 453–461. https://doi.org/10.1111/1471-0307.12786 (2021).
Hiitiö, H. et al. Performance of a real-time PCR assay in routine bovine mastitis diagnostics compared with in-depth conventional culture. J. Dairy Res. 82, 200–208. https://doi.org/10.1017/s0022029915000084 (2015).
Zadoks, R. N. et al. Comparison of bacteriological culture and PCR for detection of bacteria in ovine milk–sheep are not small cows. J. Dairy Sci. 97, 6326–6333. https://doi.org/10.3168/jds.2014-8351 (2014).
Singha, S. et al. The prevalence and risk factors of subclinical mastitis in water buffalo (Bubalis bubalis) in Bangladesh. Res. Vet. Sci. 158, 17–25. https://doi.org/10.1016/j.rvsc.2023.03.004 (2023).
Dhand, N. K. & Khatkar, M. S. Statulator (2014).
Hoque, M. N. et al. Metagenomic deep sequencing reveals association of microbiome signature with functional biases in bovine mastitis. Sci. Rep. 9, 13536. https://doi.org/10.1038/s41598-019-49468-4 (2019).
Hoque, M. N. et al. Microbiome dynamics and genomic determinants of bovine mastitis. Genomics 112, 5188–5203. https://doi.org/10.1016/j.ygeno.2020.09.039 (2020).
Cremonesi, P. et al. Development of a droplet digital polymerase chain reaction for rapid and simultaneous identification of common foodborne pathogens in soft cheese. Front. Microbiol. https://doi.org/10.3389/fmicb.2016.01725 (2016).
Cremonesi, P. et al. Development of 23 individual TaqMan® real-time PCR assays for identifying common foodborne pathogens using a single set of amplification conditions. Food Microbiol. 43, 35–40. https://doi.org/10.1016/j.fm.2014.04.007 (2014).
Bustin, S. A. et al. The MIQE guidelines: Minimum information for publication of quantitative real-time PCR experiments. Clin. Chem. 55, 611–622. https://doi.org/10.1373/clinchem.2008.112797 (2009).
Acknowledgements
We gratefully acknowledge the Swedish Research Council for funding this research project, and we thank the participating buffalo farmers for their cooperation. We also thank the UHB bacteriology laboratory of Chattogram Veterinary and Animal Sciences University for their technical support. Finally, we thank the Department of Livestock Services, Bangladesh, and a non-governmental organization named the Palli Karma-Sahayak Foundation, who work with buffalo in Bangladesh, for sharing buffalo distribution data with the research team during field visits.
Funding
Open access funding provided by Swedish University of Agricultural Sciences. This research was funded by the Swedish Research Council (Grant numbers 2018-03583).
Author information
Authors and Affiliations
Contributions
GK, FC, SB, YP, CL, MNH, PC, MMR, and MMRH contributed in the design of work and data acquisition; GK, SB, and CL guided the statistical analysis; GK, SB, CL, PC, MMR, and MNH helped with the interpretation of data; SS drafted the work and performed the laboratory and statistical analysis; all the authors made substantial contributions to revise the drafted work and approved the final version of the manuscript to be submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Singha, S., Koop, G., Rahman, M.M. et al. Foodborne bacteria in milk and milk products along the water buffalo milk chain in Bangladesh. Sci Rep 14, 16708 (2024). https://doi.org/10.1038/s41598-024-67705-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-67705-3