Abstract
The transition from radioimmunoassay (RIA) to chemiluminescent enzyme immunoassay (CLEIA) for plasma aldosterone concentration (PAC) assays has raised concerns over its impact on primary aldosteronism (PA) diagnosis. This study investigated the correlation between PAC and renin values using RIA, CLEIA, and liquid chromatography/mass spectrometry/mass spectrometry (LC–MS/MS), established cutoff values for PA diagnosis using the aldosterone-to-renin ratio (ARR) with PAC_CLEIA, and assessed the differences in PAC values by measuring weak mineralocorticoids (WMs). This retrospective study evaluated 312 serum PAC samples using RIA, CLEIA, and LC–MS/MS, and analyzed 315 plasma renin samples. Method correlations were assessed through Passing-Bablok regression. Receiver operating characteristic curves determined ARR cutoffs for PA diagnosis. WMs were quantified to evaluate their impact on ΔPAC (RIA-LC–MS/MS) through multiple regression analysis. PAC_CLEIA and PAC_LC-MS/MS values were highly correlated. ARRs derived from PAC_RIAs demonstrated more false positives and lower specificity than ARRs using PAC_CLEIA or PAC_LC-MS/MS. WMs significantly influenced ΔPAC in both the PA and non-PA groups. ARRs using PAC_CLEIA are valuable for determining PA cutoffs in clinical practice. The transition to PAC using CLEIA may enhance PA detection rates. WMs were found to interfere with PAC measurements in the RIA method, affecting outcomes.
Similar content being viewed by others
Introduction
Primary aldosteronism (PA) is the leading cause of secondary hypertension, characterized by excessive aldosterone production, elevated plasma aldosterone concentrations (PACs), low plasma renin activity (PRA), and increased cardiovascular risks1,2. PA screening in patients with hypertension typically involves determining PACs and the PAC/PRA ratio (aldosterone-to-renin ratio [ARR])3,4. Currently, the estimated prevalence of PA is as high as 4% in primary care, 10% in referred patients, and 20% among those with treatment-resistant hypertension5,6,7. In Japan, PA is estimated to affect between 2 and 4 million people (1–2% of the population; 10–20% of patients with hypertension)8. Cases initially suspected to be essential hypertension are diagnosed as PA upon closer evaluation1,5,9,10,11,12,13.
Given the likelihood of underdiagnosed mild PA cases, there is a need for highly sensitive and specific screening tests. Targeted PA screening in treatment-resistant hypertension is cost-effective8,12,14, necessitating the development of rapid and accurate screening methods15.
Traditionally, PACs are assessed using radioimmunoassay (RIA)16,17, a method burdened by several limitations such as the use and disposal of radioisotopes, manual measurement complexity, low traceability of certified reference materials, low sensitivity at lesser concentrations, and the time needed for measurements8,18. Moreover, the PACs measured by RIA can be affected by cross-reactivity with some weak mineralocorticoids (WMs)19. However, the cross-reactivity of various WMs in different disease states remains unclear. The newer chemiluminescent enzyme immunoassay (CLEIA) offers numerous advantages over the traditional RIA, including greater sensitivity, certified traceability, and expedited, automated testing20,21. CLEIA, principally a sandwich assay (two-step immunoassay with anti-metatype antibody detection) employing more specific monoclonal antibodies, offers quick aldosterone testing (< 30 min). It uses a monoclonal antibody specific for aldosterone, resulting in very low cross-reactivity with other steroids20,21. PAC_CLEIA correlates strongly with PACs measured by liquid chromatography-mass spectrometry/mass spectrometry (LC–MS/MS), the international gold standard22,23. The Japanese Guidelines for Primary Aldosteronism Treatment 2021 define a PAC_CLEIA of 6.0 ng/dL or more and a PAC_CLEIA/PRA ratio of 20 or more as positive for PA. They also categorize a PAC_CLEIA/PRA ratio of between 10 and 20 as borderline, and a PAC of 6.0 ng/dL or more and a PAC_CLEIA/PRA ratio of between 10 and 20 as provisionally positive8. Notably, PAC_CLEIA values are lower than conventional PAC_RIA values, deviating from the PAC_RIA cutoff values19. Current screening criteria are based on evidence from PAC_RIAs, whereas evidence concerning the utility and optimal cutoff values for PAC_CLEIAs is limited.
The ARR is strongly influenced by the denominator, PRA. False positives can occur with low PRA values, which can be as low as 0.1 ng/mL/h24. Older patients with hypertension are particularly likely to have low renin levels. Traditionally, PRA has been used to assess renin levels and can be determined by liquid chromatography coupled with mass spectrometry in the same run as aldosterone25; however, the active renin concentration (ARC) is increasingly being used14,21,26. The ARC is less susceptible to interference by endogenous angiotensinogen and can accurately and rapidly assess renin levels21. The relationship between the ARC to the PRA level, and the cutoff values for PA screening, are unclear.
To address these knowledge gaps, this study aimed to evaluate the accuracy and validity of PAC measurements obtained through RIA, CLEIA, and LC–MS/MS methods, as well as plasma renin levels determined by PRA_RIA, PRA_EIA, and ARC. Moreover, it aimed to establish optimal cutoff values for PA screening, specifically focusing on PAC_CLEIAs and the PAC_CLEIA/PRA ratio. Furthermore, we investigated the impact of WMs on variations in PAC values across these different measurement methods, identifying how these factors differ by disease state.
Results
Participants and samples
This study included PAC and plasma renin samples from 227 and 245 patients, respectively, who underwent PA screening, as well as loading tests and adrenal vein sampling (AVS). The final cohort of 220 patients had an estimated glomerular filtration rate of 70.0 mL/min/1.73 m2 (Table 1). For a broad validation of PAC value conversion, the analysis included AVS-collected samples, which exhibit higher PAC values than those in clinical practice. Out of 312 PAC samples, 242 (77.6%) were screening samples, 30 (9.6%) were used for loading tests, and 40 (12.8%) were AVS samples. Out of 315 renin samples, 264 (83.8%) were for screening, 32 (10.2%) for loading tests, and 19 (6.0%) were AVS samples (Supplemental Fig. 1, Step 1).
The 220 patients were divided into non-PA and PA groups to assess screening parameters (Supplemental Fig. 1, Step 2). The mean age and number of sexes in both groups are listed in Table1. Age, sex, body mass index, serum potassium level, and blood pressure were not significantly different between the two groups. However, the incidence of adrenal nodules was higher in the PA group, which also had smaller tumor sizes than the non-PA group (Table 1).
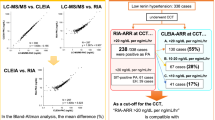
Correlations between PAC methods and bias analysis of PAC values
To explore correlations and conversion (regression) equations between PAC and PRA levels, we first measured PACs (Table 2). The correlation analysis between PAC_LC-MS/MS and PAC_CLEIAs revealed an r of 0.999 across the entire measurement range. The regression equation was: PAC_LC-MS/MS = 0.957 × PAC_CLEIA–0.044 (Fig. 1A). In the Bland‒Altman analysis, the bias between PAC_LC-MS/MS and PAC_CLEIAs was –4.097 ng/dL across the entire measurement range (Fig. 1B). The bias between PAC_LC-MS/MS and PAC_CLEIAs was –0.429 ng/dL within the PAC_CLEIA non-diluted range (Supplemental Fig. 2A). The correlation analysis between PAC_LC-MS/MS and PAC_RIAs indicated an r of 0.992 and a regression equation of: PAC_LC-MS/MS = 0.723 × PAC_RIA–3.487 (Fig. 1C). The bias between the PAC_LC-MS/MS and PAC_RIAs was –64.330 ng/dL across the entire measurement range (Fig. 1D). The bias was –8.014 ng/dL for the PAC_CLEIA non-diluted range (Supplemental Fig. 2B). When correlating PAC_RIAs and PAC_CLEIAs, the r was 0.991 and the equation was: PAC_CLEIA = 0.756 × PAC_RIA–3.458 (Fig. 1E). The bias between the PAC_CLEIAs and PAC_RIAs was –60.233 ng/dL across the whole measurement range (Fig. 1F), and –7.584 ng/dL for the PAC_CLEIA non-diluted range (Supplemental Fig. 2C). The regression analysis revealed a very strong correlation between PAC_LC-MS/MS and PAC_CLEIA, while the PAC_RIA differed from the values obtained by LC–MS/MS and CLEIAs.
Passing-Bablok regression analysis for plasma aldosterone concentration (PAC) (A,C,E) and Bland–Altman analysis (B,D,F), along with comparisons of PAC measurements from identical samples over the full measurement range (G) and in screening samples only (H) (values from the same sample are connected by lines). Values from chemiluminescent enzyme immunoassay (CLEIA) and liquid chromatography/mass spectrometry/mass spectrometry (LC–MS/MS) were highly correlated and nearly identical. In contrast, radioimmunoassay (RIA) values were higher than both CLEIA and LC–MS/MS values. Differences between groups were evaluated using Friedman’s test followed by Dunn’s multiple comparisons test. “Screening”, “loading test”, “AVS”, and “95% LoA” refer to screening, loading test, adrenal venous sampling samples, and 95% limits of agreement, respectively.
Figure 1G is a dot plot showing the different PAC measurements from the same samples. The PAC_RIA values were significantly higher than PAC_LC-MS/MS values (p < 0.0001) within the entire measurement range, while the PAC_CLEIA values closely aligned with those of PAC_LC-MS/MS. Moreover, the PAC_LC-MS/MS and PAC_CLEIA values were lower than the PAC_RIA values in samples collected for screening (p < 0.0001) (Fig. 1H).
Correlations between PAC methods and bias analysis of PAC values in loading test and AVS samples
Additional analyses were performed on each sample type to examine the correlation and bias of PAC values in loading test and AVS samples. For the loading test samples, the correlation analysis between PAC_LC-MS/MS and PAC_CLEIA revealed an r of 0.992 (Supplemental Fig. 3A). The bias between PAC_LC-MS/MS and PAC_CLEIA was 0.322 ng/dL (Supplemental Fig. 3B). The correlation analysis between PAC_LC-MS/MS and PAC_RIA revealed an r of 0.819 (Supplemental Fig. 3C). The bias between PAC_LC-MS/MS and PAC_RIA was −5.476 ng/dL (Supplemental Fig. 3D). The correlation analysis between PAC_CLEIA and PAC_RIA revealed an r of 0.817 (Supplemental Fig. 3E). The bias between PAC_CLEIA and PAC_RIA was -5.153 ng/dL (Supplemental Fig. 3F).
Regarding PAC values, RIA produced significantly higher values compared with LC–MS/MS (p < 0.0001), whereas no significant difference was found between CLEIA and LC–MS/MS (Supplemental Fig. 3G). For the AVS samples, the correlation analysis between PAC_LC-MS/MS and PAC_CLEIA revealed an r of 0.999 (Supplemental Fig. 4A). The bias between PAC_LC-MS/MS and PAC_CLEIA was 28.84 ng/dL (Supplemental Fig. 4B). The correlation analysis between PAC_LC-MS/MS and PAC_RIAs revealed an r of 0.990 (Supplemental Fig. 4C). The bias between PAC_LC-MS/MS and PAC_RIA was -448.1 ng/dL (Supplemental Fig. 4D). The correlation analysis between PAC_CLEIA and PAC_RIA revealed an r of 0.989 (Supplemental Fig. 4E). The bias between PAC_CLEIA and PAC_RIA was -419.2 ng/dL (Supplemental Fig. 4F). Again, RIAs yielded significantly higher PAC values than LC–MS/MS (p < 0.0001), with no significant difference between CLEIAs and LC–MS/MS (Supplemental Fig. 4G).
Correlations between PRA methods
For the 315 total renin samples, the median values are shown in Table 2. The correlation analysis between PRA_RIAs and PRA_EIAs over the entire measurement range yielded an r of 0.975 and a regression equation of: PRA_EIA = 1.692 × PRA_RIA–0.203 (Fig. 2A). For PRA_RIA values of 2 ng/mL/h or less (the most relevant PA diagnostic range), r was 0.896 and the regression equation was: PRA_EIA = 1.6 × PRA_RIA–0.18 (Fig. 2B). The slope was more than 1 for both the full measurement range and the low-PRA_RIA (≤ 2 ng/mL/h) range, indicating that values obtained by EIA were significantly higher than those obtained by RIA across both ranges, as shown in dot plots (Fig. 2C,D).
Passing-Bablok regression analysis for renin measurements over the entire range (A,E,G) and in the low plasma renin activity (PRA) range (B,F,H), in addition to comparisons of PRA measurements from identical samples over the full measurement range (G) and in radioimmunoassay (RIA) values < 2 ng/mL/h (D) (values from the same samples are connected by a line). PRA values from enzyme immunoassay (EIA) were significantly higher than PRA_RIA values. Correlations between PRA and active renin concentration (ARC) values were relatively low, complicating accurate conversion. Notably, in the low-renin range, a broad range of ARC values corresponded to each PRA value, allowing for a more granular assessment of renin values. Inter-group differences were evaluated using Wilcoxon matched-pairs signed rank tests. “Screening,” “loading test”, and “AVS” signify screening, loading test, and adrenal venous sampling samples, respectively.
In the Bland–Altman analysis, the bias between the PRA_EIAs and PRA_RIAs was + 0.732 ng/mL/h across the entire measurement range (Supplemental Fig. 5A).
Correlations between PRA and ARC methods
The correlation analysis between ARCs and PRA_RIAs showed an r of 0.893 across the entire range, with the equation: ARC = 10.193 × PRA_RIA + 0.499 (Fig. 2E). For PRA_RIA values of 2 ng/mL/h or less, the r was 0.766, and the equation was: ARC = 11.356 × PRA_RIA–0.982 (Fig. 2F). Between ARCs and PRA_EIAs, the r was 0.902 across the entire measurement range, and the equation was: ARC = 6.456 × PRA_EIA + 0.365 (Fig. 2G). For PRA_RIA values of less than 2 ng/mL/h, the r was 0.864, and the equation was: ARC = 8.716 × PRA_EIA–0.770 (Fig. 2H).
Although correlations between PRA and ARC values were relatively low, PRA is a discontinuous variable measured in increments of 0.1 ng/mL/h by both RIA and EIA, while ARC is a continuous variable. Hence, a range of ARC values can correspond to a specific PRA value, especially when considering the lower PRA values that are important for PA diagnosis.
Cutoff values for ARR for PA screening
The screening parameters for the 220 eligible patients were compared between non-PA and PA groups (Supplemental Fig. 1; Step 2). In the PA group, ARR values based on PRA_RIA were significantly higher than those is the non-PA group across all three PAC assay methods (p < 0.001) (Table 1, Fig. 3A–C). Most patients in the PA group were taking calcium channel blockers (CCBs) or mineralocorticoid receptor blockers (MRBs) because the cohort was part of a retrospective analysis that included patients without hypertension, patients with other endocrine disorders, and patients taking drugs affecting the renin–angiotensin–aldosterone system (Table 1, Supplemental Table 3).
Distribution of plasma aldosterone concentration (PAC) and plasma renin activity (PRA) in the primary aldosteronism (PA) and non-PA groups according to different aldosterone-to-renin ratio (ARR) methods (A–C) and derivation of ARR cutoff values using receiver operating characteristic curve analysis (D–I). For all PAC assay methods, PAC/PRA_ radioimmunoassay (RIA) was significantly higher in the PA group than in the non-PA group. Cutoff values and specificity are shown, with sensitivity set at 80.6%. The area under the curve (AUC) was greater for the ARR using PAC determined by chemiluminescent enzyme immunoassay (CLEIA) than for the ARR using PAC determined by RIA. Inter-group differences were evaluated using the Mann‒Whitney U test. The letter “a” represents specificity and an ARR threshold at 90.3% sensitivity; “b” represents specificity and an ARR threshold at 80.6% sensitivity; “c” represents sensitivity, specificity, and an ARR threshold at the Youden Index.
ARR values based on ARCs were also compared between the PA and non-PA groups. Using all three methods for measuring PAC, ARR values were higher in the PA group (p < 0.0001) (Table 1, Supplemental Fig. 6A–C). PAC values were plotted against the corresponding PAC/PRA_RIA or PAC/ARC ratios for each of the three PAC methods, showing that the PA and non-PA groups were separable (Supplemental Fig. 6).
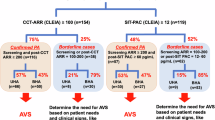
To evaluate the suitability of each method for PA screening, receiver operating characteristic (ROC) curves were created for the PAC/PRA ratio based on PAC values measured by RIA, CLEIA, and LC–MS/MS. The area under the curve (AUC) values were 0.872 for PAC_LC-MS/MS/PRA_RIA, 0.872 for PAC_CLEIA/PRA_RIA, and 0.801 for PAC_RIA/PRA_RIA (Fig. 3D–F). There was no significant difference in AUC between PAC_LC-MS/MS/PRA_RIA and PAC_CLEIA/PRA_RIA. However, the AUC of PAC_RIA/PRA_RIA was significantly different from that of PAC_LC-MS/MS/PRA_RIA (p < 0.05) and PAC_CLEIA/PRA_RIA (p < 0.05). At a sensitivity of 80.6%, the cutoff value was 10.0 ng/dL/ng/mL/h for PAC_LC-MS/MS/PRA_RIA (specificity: 85.7%), 10.5 ng/dL/ng/mL/h for PAC_CLEIA/PRA_RIA (specificity: 84.5%), and 19.1 ng/dL/ng/mL/h for PAC_RIA/PRA_RIA (specificity: 67.9%) (Fig. 3D–F). At a sensitivity of 90.3%, the cutoff value was 4.67 ng/dL/ng/mL/h for PAC_LC-MS/MS/PRA_RIA (specificity: 55%), 5.47 ng/dL/ng/mL/h for PAC_CLEIA/PRA_RIA (specificity: 58%), and 11.6 ng/dL/ng/mL/h for PAC_RIA/PRA_RIA (specificity: 44%) (Supplemental Table 4).
We also created ROC curves for the PAC/ARC ratios corresponding to each PAC assay method. The AUC for PAC_CLEIA/ARC was 0.855. At a sensitivity of 80.6%, the cutoff value was 0.72 ng/dL/pg/mL for PAC_LC-MS/MS/ARC (specificity: 73.8%), 0.77 ng/dL/pg/mL for PAC_CLEIA/ARC (specificity: 73.8%), and 1.60 ng/dL/pg/mL for PAC_RIA/ARC (specificity: 60.7%) (Fig. 3G–I). At a sensitivity of 80.6%, the specificity was lower for the PAC/ARC ratio than for the PAC/PRA ratio using all the PAC methods; however, at a sensitivity of 90.3%, the specificity was similar between ARC-based and PRA-based ratios from all PAC methods (Supplemental Table 4).
Furthermore, we identified the following cutoff values for the combination of ARR and PAC at a sensitivity of 81%: PAC_RIA/PRA_RIA ratio more than 11.6 ng/dL/ng/mL/h and PAC_RIA more than 11.5 ng/dL (specificity: 82%); PAC_CLEIA/PRA_RIA ratio more than 5.47 ng/dL/ng/mL/h and PAC_CLEIA more than 5.4 ng/dL (specificity: 82%); and PAC_LC-MS/MS/PRA_RIA ratio more than 4.66 ng/dL/ng/mL/h and PAC_LC-MS/MS more than 5.8 ng/dL (specificity: 85%) (Supplemental Tables 6, 7).
When we substituted ARCs for PRA levels, the combined ARR and PAC values remained effective screening parameters for PA. We identified the following cutoff values for the combination of ARR (PAC/ARC ratio) and PAC at a sensitivity of 81%: PAC_RIA/ARC ratio more than 1.10 ng/dL/pg/dL and PAC_RIA more than 11.6 ng/dL (specificity: 86%); PAC_CLEIA/ARC ratio more than 0.51 ng/dL/pg/dL and PAC_CLEIA more than 5.5 ng/dL (specificity: 85%); and PAC_LC-MS/MS/ARC ratio more than 0.49 ng/dL/pg/dL and PAC_LC-MS/MS more than 5.8 ng/dL (specificity: 86%). These results were generally similar to the specificity of cutoff values for the PAC/PRA_RIA ratio plus PAC combinations (Supplemental Table 8).
Impact of changes in the ARR screening method on PA diagnosis rates
To clarify the impact of screening method changes on PA diagnostic rates (sensitivity and specificity), we utilized waterfall plots. These plots assessed the concordance between ARRs (PAC/PRA_RIA ratios) computed with three PAC methods using identical samples from both PA and non-PA groups. When comparing LC–MS/MS and RIAs, the first y-axis represented the PAC_LC-MS/MS/PRA_RIA ratio, while the second y-axis showed the PAC_RIA/PRA_RIA ratio. The 80.6%-sensitivity cutoff values, as determined by ROC curve analysis for each ARR, were indicated in each y-axis. Then, ARRs were plotted from left to right in descending order of value. In the PA group, the determinations were almost identical; however, in the non-PA group, divergence occurred in 15 cases, which yielded false-positive PAC_RIA results (Fig. 4A, B). Waterfall plots comparing the PAC_LC-MS/MS/PRA_RIA ratio on the first y-axis and the PAC_CLEIA/PRA_RIA ratio on the second y-axis, indicated closely aligned results in both the PA and non-PA groups (Fig. 4C, D). When the first y-axis was set to PAC_CLEIA/PRA_RIA and the second to PAC_RIA/PRA_RIA, the determinations were nearly identical in the PA group but diverged in 17 cases in the non-PA group, resulting in false-positive PAC_RIA results (Fig. 4E, F).
Waterfall plots evaluating the concordance of aldosterone-to-renin ratios (ARRs) measured by different plasma aldosterone concentration (PAC) assays between primary aldosteronism (PA) and non-PA groups. (A,C,E). ARRs shown on the left y-axis are plotted on the x-axis from left to right in descending order, and the corresponding ARRs on the right y-axis are aligned at the same x-coordinate. Cutoff values for each ARR at a sensitivity of 80.6% are indicated on both the left and right y-axes. (B,D,F) Enlarged views of the dotted line areas in A, C, and E, respectively. Dots in the pink false-positive (FP) zone indicate false positives for ARRs on the right y-axis. The ARRs using PAC values determined by radioimmunoassay (RIA) resulted in more false positives than the ARRs using PAC values determined by chemiluminescent enzyme immunoassay (CLEIA). Units for all y-axis values are ng/dL/ng/mL/h.
Characteristics of false-positive patients by PAC_RIA/PRA_RIA
Further analysis of false-positives identified by PAC_RIA/PRA_RIA, when compared to PAC_LC-MS/MS/PRA_RIA in patients without PA, revealed distinct characteristics (Supplemental Table 9). Compared with true-negatives in patients without PA, the false-positives had significantly lower PAC_CLEIA and PAC_LC-MS/MS values (p = 0.007 and p = 0.010, respectively), as well as lower PRA_RIA and ARC values (both p < 0.0001). These differences resulted in higher ARRs or PAC/ARC ratios. Interestingly, lower levels of corticosterone (B) and 18-oxocortisol (18oxoF) (p = 0.038 and p = 0.041, respectively) were also characteristic of the false-positive group.
WMs cross-react with the PAC measurement system, particularly the RIA method
Lastly, we utilized 150 serum samples to investigate the cause of the significantly higher PAC_RIA values compared with PAC_CLEIA and PAC_ LC–MS/MS values, identifying which WMs contributed more to ΔPAC (PAC_RIA-PAC_LC-MS/MS) through multiple regression analysis (Supplemental Fig. 1, Step 3). 18-hydroxycorticosterone (18OHB), 18-hydroxycortisol (18OHF), and 18oxoF values were significantly higher in the PA group than those in the non-PA group, while deoxycorticosterone (DOC) and B showed no significant differences (Table 1). The multiple regression analysis indicated that the ΔPAC was strongly correlated with B, 18OHB, and DOC across all 150 samples: in the non-PA group, 18OHB, 18oxoF, and B contributed; in the PA group, B, DOC, and 18OHB were significant contributors (Supplemental Table 10).
This data clarifies that the WMs affecting ΔPAC values and PAC_RIAs differ between the non-PA and PA groups. Notably, PAC_RIAs exhibited cross-reactivity not only with PAC but also with certain WMs, particularly DOC, B and 18OHB, resulting in higher values for PAC_RIAs compared with PAC_LC-MS/MS.
Discussion
PAC has traditionally been measured using RIA. However, in recent years, many institutions have transitioned to using CLEIA for PAC measurement due to its potential advantages. Several factors contribute to the superior performance of CLEIA compared with RIA, including the high specificity of the reaction, the use of antibodies with improved selectivity and affinity, and calibrations traceable to Certified Reference Material (CRM)22. Despite this shift, there are few reports that have comprehensively measured and compared PACs of multiple specimens by RIA, CLEIA, and LC–MS/MS in the same specimen22,26,27. Our study addresses this gap by conducting a thorough comparison of these three methods using the same specimens, providing valuable insights into their relative performance and clinical implications.
Our findings corroborate previous studies22,27,28, showing a strong correlation between PAC_CLEIA and PAC_LC-MS/MS values (r = 0.999, p < 0.0001). CLEIA maintains a high correlation with LC–MS/MS across screening, loading test, and AVS samples, with minimal bias in PAC values. This confirms CLEIA as a highly accurate and reliable method for PAC measurement, suitable for PA screening, diagnostic testing, and AVS. The strong correlation with LC–MS/MS, considered the gold standard, further validates the accuracy of CLEIA for PAC measurement.
Additionally, we derived a conversion equation from PAC_RIA to PAC_CLEIA. This equation serves two important purposes: first, it allows for the recalibration of past PAC measurements obtained through RIA, ensuring continuity in patient data interpretation; second, it provides a foundation for optimizing future PA screening cutoff values based on CLEIA measurements. This conversion tool could be particularly beneficial in clinical settings transitioning from RIA to CLEIA, enabling more accurate comparisons of historical and current PAC data.
Our study also investigated renin activity, comparing PRA and ARC measurements. We found that the ARC is particularly suitable for detailed evaluation in patients with PRA values of 2 ng/mL/h or less, which is the range relevant for PA diagnosis. The ARC offers advantages in terms of speed (≤ 30 min) and sensitivity, with a threshold value of 0.04 pg/mL showing excellent sensitivity21. These characteristics make the ARC a promising parameter for PA screening.
However, our analysis revealed a relatively weak correlation between PRA_RIA and the ARC (r = 0.894). The slope of the regression equation was 10.193, which complicates the conversion between PRA and ARC values. This weak correlation likely stems from the fundamental differences in their measurement principles: PRA quantifies angiotensin I production per unit time using angiotensinogen in the blood as a substrate, while the ARC directly measures the ARC using a specific monoclonal antibody21. We also assessed the accuracy of the PAC, PRA, and ARR values for their clinical importance in PA screening. We determined PA screening cutoff values for the ARR with a sensitivity setting at 80%. Previously, a considerable variation in ARR cutoff values has been used for PA screening (Supplemental Table 5). This variability in ARR cutoff values may be due to differences in participant recruitment conditions and patient population characteristics in different study settings. In our study, a PAC_RIA/PRA_RIA ratio cutoff value of more than 19.1 ng/dL/ng/mL/h achieved a sensitivity of 80.6%, consistent with the Nishizaka and Calhoun studies29,30,31.
Previous studies have suggested that combining ARR and PAC values can improve PA screening accuracy by reducing false-positives30,32. These studies found that using combinations of ARR and PAC cutoff values tended to increase specificity at the expense of sensitivity for detecting treatment-resistant hypertension or hypertension in the target population30,32. Our results align with these findings, demonstrating an increase in specificity and improved accuracy of PA screening when using combined criteria (Supplemental Tables 6, 7, 8). We observed a consistent trend across studies evaluating different ARR cutoff values, with higher cutoff values being associated with lower sensitivity and higher specificity. This trend was evident in our own data as well as in the varying ARR sensitivity reported across different studies (Supplemental Table 5). The observed pattern reflects the inherent trade-off between sensitivity and specificity in diagnostic testing.
In terms of PAC measurement, CLEIA demonstrated strong correlations with the gold standard LC–MS/MS, affirming its accuracy. This high correlation, coupled with CLEIA’s ability to provide fast results, suggests it may be particularly useful for rapid testing during AVS. Moreover, our analysis revealed that a PAC_CLEIA/PRA_RIA ratio of 10.5 ng/dL/ng/mL/h achieved a sensitivity of 80.6% with few false-positives (specificity: 84.5%). These performance characteristics suggest that the PAC_CLEIA/PRA_RIA ratio could serve as a valuable parameter for PA screening, offering a good balance between sensitivity and specificity. Recently, Ono et al. reported a PAC_CLEIA/PRA_RIA ratio of 31.5 ng/dL/ng/mL/hr (sensitivity 90.2%, specificity 76.8%) as the cutoff value for aldosterone-producing adenoma (APA) detection28. The variation in these cutoff values is likely attributable to differences in the characteristics of the study populations, the specific patient groups targeted by the cutoff values, and the influence of medications, such as MRBs, that may affect ARR in our cohort.
Although we have presented an ARR screening cutoff using PAC_CLEIA, the current consensus for screening cutoffs still employs PAC_RIA, which generally shows higher values than PAC_CLEIA. In our cohort, the median PAC_RIA was over twice as high as the median PAC_CLEIA. This discrepancy raises questions about the underlying causes of these differences.
Artifactual results in immunoassays can be due to various interferences, including cross-reacting substances, heterophile antibodies, autoantibodies, and the high-dose hook effect33,34. However, the precise reasons for the discrepancies between PAC_RIA and PAC_CLEIA values remain unclear. Nishikawa et al. reported that the addition of 18oxoF to samples led to discrepancies of up to 24% in PAC-RIA measurements19, suggesting the potential influence of WMs on RIA results.
To investigate the degree of WM interference in PAC measurement, we measured WMs in the same samples where PAC was measured. Our multiple regression analysis revealed that the WMs contributing to ΔPAC (PAC_RIA-PAC_LC/MS/MS) varied between the non-PA and PA groups. This variation could be linked to differing expressions of steroid synthases, notably aldosterone synthase, in PA and normal adrenal glands.
In adrenal glands with APAs, tumors with KCNJ5 mutations have been reported to consist of cells expressing only CYP11B2 and cells that co-express CYP11B2 and 17α-hydroxylase, with some cells also co-expressing CYP11B2, 17α-hydroxylase, and CYP11B135. This suggests that the steroid synthase expression profile in the adrenal gland may differ significantly between PA and non-PA groups. Our observations suggested potential differences in the contributions of various steroid metabolites between the PA and non-PA groups. In the PA group, we noted possible influences from DOC and B, which are precursors of aldosterone, as well as 18OHB. In contrast, the non-PA group appeared to show potential contributions from 18OHB, 18oxoF, and B. The PAC_RIA values seemed to exhibit some degree of cross-reactivity with WMs, which appeared to vary depending on the underlying pathology. This variability in cross-reactivity, along with differences in true PAC levels, may contribute to the tendency for PAC_RIA values to be somewhat higher than those obtained through PAC_LC-MS/MS.
This study has a few limitations that may affect the generalizability of its findings. First, is the selection bias inherent in our cohort, which predominantly comprises patients receiving MRBs and CCBs in a university hospital setting. These medications may influence the ARR, which could result in false-negative results in PA screening. Second, additional variables such as the timing of blood sampling, freezing and thawing procedures, salt consumption, potassium levels, and patient posture can also impact the levels of renin and aldosterone. Despite our efforts to mitigate these effects, the retrospective design of our study precluded the evaluation of all patients under optimal conditions.
Ideally, medications that interfere with the renin–angiotensin–aldosterone system, including angiotensin-converting enzyme inhibitors, angiotensin II type 1 receptor blockers, beta-blockers, and diuretics, should be discontinued at least 2 weeks before testing, while MRBs should be withdrawn for 4 weeks36. Despite our efforts to control for these variables, the lack of standardized conditions may have affected the diagnostic performance of the ARR in our cohort. Consequently, future prospective studies with stricter control of these variables—including medication use, patient age, disease duration, and underlying comorbidities—are warranted. Such studies could help establish more accurate cut-off values for the ARR using different measurement methods and contribute to improving the diagnostic accuracy for PA screening.
In conclusion, our study suggests the potential utility of CLEIA as a method for measuring PAC, and proposes PA screening cutoff values based on PAC_CLEIA. Our findings indicate that PAC_RIA, which remains in use in many settings, may yield somewhat higher values compared with the CLEIA method, possibly due to the influence of WMs. This study aims to contribute to the ongoing improvement of hypertension care by potentially enhancing the accuracy of PA screening. By doing so, we hope to support efforts to identify PA cases that may otherwise go undetected, ultimately leading to more targeted and effective patient care. However, further research and clinical validation may be necessary to fully establish the role of CLEIA in PA screening and diagnosis.
Methods
This study was approved by the Ethics Committee of Chiba University Graduate School of Medicine (approval number: 2020-3795). Written informed consent was not required as the study was retrospective and used only surplus blood samples from regular medical care. The requirement for informed consent has been waived by the Ethics Committee of Chiba University Graduate School of Medicine due to the retrospective nature of the study. Details of the study were disclosed in advance on the website, and patients had the option to opt out. This study was designed in accordance with the STARD checklist.
Participants
We retrospectively examined 312 PAC samples from 227 patients and 315 plasma renin samples from 245 patients treated at Chiba University Hospital in Japan between March 31 and May 13, 2021 (Supplemental Fig. 1).
In step 1, we derived conversion equations between the different assays. For aldosterone, the equations were derived between PAC_CLEIA and PAC_LC-MS/MS, PAC_RIA and PAC_LC-MS/MS, and PAC_RIA and PAC_CLEIA. For renin, equations were derived between PRA_RIA and PRA_EIA, PRA_RIA and ARC, and PRA_EIA and ARC. The equations were also derived for samples in the low range (PRA ≤ 2 ng/mL/h). PRA_EIA samples outside the sensitivity range were excluded. Due to the higher PAC values in loading test and AVS samples and the potential for drug interference (e.g., corticotropin, captopril, furosemide), which may lead to PAC and renin differences, separate analyses were performed for each sample type. As the study aimed to reflect clinical practice, loading test and AVS samples were included when deriving conversion equations.
In step 2, we calculated ARR thresholds (PAC/PRA_RIA, PAC/ARC). Medical records were reviewed to include only screening samples, excluding loading test and AVS samples. Only samples with concurrent aldosterone and renin measurements were selected. When multiple samples were taken from a patient, the early morning resting sample was used. For PRA_RIA, the ARR was calculated from the lower detection limit if the observed value was below this limit.
In total, 220 patients were classified into three groups: the PA group, which met the PA diagnostic criteria (n = 72); the non-PA group, which fulfilled the criteria for non-PA diagnostic conditions (n = 84); and the gray group, which did not fit into either of the other two categories (n = 64). The PA diagnostic criteria included: hypertension; 1 or more elevated PAC_RIA (> 12 ng/dL) and PAC_RIA/PRA_RIA ratio (> 20 ng/dL/ng/mL/h); and 1 or more positive functional confirmatory test (saline infusion, captopril loading, or furosemide-upright loading). The 72 patients in the PA group included seven with APAs, 23 with bilateral hyperaldosteronism (BHA), and 42 with no diagnosis of APA or BHA. The non-PA group included patients with: no hypertension or hypoadrenocorticism, those with hypertension with negative screening and functional tests, those who had undergone adrenalectomy for unilateral aldosteronism or unilateral adrenal tumor. The gray group, which included patients who did not fit into the other two groups (positive screening tests but negative or no functional tests; nonfunctioning adrenal tumors; secondary hypertension resulting from non-PA disorders; bilateral aldosteronism and post-unilateral adrenalectomy), was excluded from the analysis.
In step 3, WMs were analyzed in the aldosterone samples utilized in step 2 to explore the factors causing differences between PAC assays. A total of 150 WM samples from the PA (n = 68) and non-PA groups (n = 82) were analyzed, excluding those with insufficient volume. WM types such as DOC, B, 18-OHB, 18-OHF, and 18-oxoF were measured.
Aldosterone, renin and WM measurement methods
For serum PAC, blood samples were first subjected to serum separation, and the serum was stored at − 30 °C for a few days. PAC_RIA measurements were performed using the Spac-S Aldosterone Kit (Fujirebio, Inc., Tokyo, Japan). The remaining serum was returned to − 30 °C storage, and subsequently, PAC_CLEIA was measured using Lumipulse Presto Aldosterone (Fujirebio, Inc., Tokyo, Japan). This refreezing process was repeated before performing PAC_LC-MS/MS (ASKA Pharmaceutical Co., Ltd, Tokyo, Japan). Additionally, some samples were analyzed for DOC, B, 18-OHB, 18-OHF, and 18-oxoF using LC–MS/MS.
Plasma renin was assessed similarly; however, the blood samples underwent plasma separation instead. Regarding our sample handling procedures, samples were maintained in a frozen state throughout transport and were stored at -80 °C. For analysis, frozen samples were thawed in a water bath for 10–15 min. After thawing, samples were vortexed and centrifuged at 3000 rpm for 5 min at room temperature for measurement. PRA_RIA was conducted using the Renin Activity (PRA) “FR” kit (Fujirebio, Inc, Tokyo, Japan), while PRA_EIA was performed with the Renin Activity Kit “Yamasa” (YAMASA CORPORATION, Chiba, Japan). The ARC was assessed using CLEIA (Lumipulse Presto Renin, Fujirebio, Inc, Tokyo, Japan), which is available only in Japan.
PAC_RIA, PRA_RIA, and PRA_EIA were carried out by SRL (Tokyo, Japan). PAC_LC-MS/MS and WMs were assessed at ASKA Pharmaceutical Medical Co., Ltd., and PAC_CLEIA and ARC measurements were conducted at Fujirebio, Inc., using the fully automated CLEIA system, LUMIPULSE L2400. Additional details about the assays are provided in the Supplemental Materials.
Analytical performance and method comparisons
Lumipulse Presto Aldosterone is traceable to NMIJ CRM 6402. This method demonstrated an intra-run coefficient of variation (CV) ranging from 1.0% to 2.4%, an inter-run CV from 0.9% to 1.5%, and a between-day CV from more than 0.0% to 1.7%21. The limit of quantification (LoQ) was 0.4 ng/dL, with a measurement range from 0.4 to 200 ng/dL21. LC–MS/MS is also traceable to NMIJ CRM 6402. It has a quantification range of 0.5 to 1000 ng/dL, with intra-assay precision showing a CV between 2.8% and 3.9% (n = 5), and an inter-assay precision showing a CV between 4.8% and 7.9%19. The Spac-S Aldosterone Kit is traceable to a manufacturer’s in-house standard. This method is a direct aldosterone measurement that does not include processes such as extraction. The limit of detection (LoD), calculated using the 3SD method, is 0.54 ng/dL, with a quantification range of 2.5 to 160 ng/dL. The intra-assay precision shows a CV between 1.8% and 8.3% (n = 10), while the inter-assay precision shows a CV between 2.8% and 4.5%19.
Statistical analysis
Data were analyzed with a combination of software packages: GraphPad Prism v.10.0.3, JMP Pro v.17.1.0, and R v.4.0.4. Data are presented as means ± standard deviations (when normally distributed) or medians (interquartile ranges) (when not normally distributed). Passing-Bablok regression and Pearson’s correlation coefficient were used to compare the two methods. Bland–Altman analysis evaluated mean differences. Differences in values between the two methods were assessed using Wilcoxon matched-pair signed rank tests. Friedman’s test, followed by Dunn’s multiple comparisons test, was used for comparisons between the three methods. For inter-group comparisons, paired t-tests were employed for normally distributed variables and Mann–Whitney U tests for non-normally distributed variables. ROC curve analysis examined the diagnostic abilities of each measurement. AUCs were compared using DeLong’s tests across methods and optimal cutoff values were established. Multiple linear regression analysis identified factors contributing to discrepancies between PAC measurement methods. Multicollinearity was assessed through the variance inflation factor (VIF), ensuring that each variable’s VIF was less than 5. Statistical significance was set at a p-value of 0.05 or less.
Data availability
All data generated and analyzed during this study are included in this article and the supplementary materials.
Abbreviations
- ARC:
-
Active renin concentration
- ARR:
-
Aldosterone-to-renin ratio
- AVS:
-
Adrenal vein sampling
- CLEIA:
-
Chemiluminescent enzyme immunoassay
- EIA:
-
Enzyme immunoassay
- LC–MS/MS:
-
Liquid chromatography/mass spectrometry/mass spectrometry
- PAC:
-
Plasma aldosterone concentration
- PRA:
-
Plasma renin activity
- RIA:
-
Radioimmunoassay
- WM:
-
Weak mineralocorticoid
References
Reincke, M. et al. Diagnosis and treatment of primary aldosteronism. Lancet Diabetes Endocrinol. 9(12), 876–892 (2021).
Ohno, Y. et al. Prevalence of cardiovascular disease and its risk factors in primary aldosteronism: A multicenter study in Japan. Hypertension 71(3), 530–537 (2018).
Yoshida, Y. & Shibata, H. Recent progress in the diagnosis and treatment of primary aldosteronism. Hypertens. Res. 46(7), 1738–1744 (2023).
Meng, X. et al. Evaluation of the saline infusion test and the captopril challenge test in Chinese patients with primary aldosteronism. J. Clin. Endocrinol. Metab. 103(3), 853–860 (2018).
Buffolo, F. et al. Is primary aldosteronism still largely unrecognized?. Horm. Metab. Res. 49(12), 908–914 (2017).
Scholl, U. I. et al. Somatic and germline CACNA1D calcium channel mutations in aldosterone-producing adenomas and primary aldosteronism. Nat. Genet. 45(9), 1050–1054 (2013).
Rossi, G. P. et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J. Am. Coll. Cardiol. 48(11), 2293–2300 (2006).
Naruse, M. et al. Japan Endocrine Society clinical practice guideline for the diagnosis and management of primary aldosteronism 2021. Endocr. J. 69(4), 327–359 (2022).
Burrello, J. et al. Prevalence of hypokalemia and primary aldosteronism in 5100 patients referred to a tertiary hypertension unit. Hypertension 75(4), 1025–1033 (2020).
Mantero, F., Mattarello, M. J. & Albiger, N. M. Detecting and treating primary aldosteronism: Primary aldosteronism. Exp. Clin. Endocrinol. Diabetes 115(3), 171–174 (2007).
Baudrand, R. et al. Continuum of renin-independent aldosteronism in normotension. Hypertension 69(5), 950–956 (2017).
Nishikawa, T., Saito, J. & Omura, M. Prevalence of primary aldosteronism: Should we screen for primary aldosteronism before treating hypertensive patients with medication?. Endocr. J. 54(4), 487–495 (2007).
Chen, S., Liu, H., Luo, P. & Yu, Y. Computed tomography combined with confirmatory tests for the diagnosis of aldosterone-producing adenoma. Endocr. J. 68(3), 299–306 (2021).
Naruse, M. et al. International multicenter survey on screening and confirmatory testing in primary aldosteronism. Eur. J. Endocrinol. 188(1), 125–134 (2023).
Tamura, N. et al. Comparisons of plasma aldosterone and renin data between an automated chemiluminescent immunoanalyzer and conventional radioimmunoassays in the screening and diagnosis of primary aldosteronism. PLoS One 16(7), e0253807 (2021).
Ito, T., Woo, J., Haning, R. & Horton, R. A radioimmunoassay for aldosterone in human peripheral plasma including a comparison of alternate techniques. J. Clin. Endocrinol. Metab. 34(1), 106–112 (1972).
Umemura, S. et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019). Hypertens. Res. 42(9), 1235–1481 (2019).
Pizzolo, F. et al. Fully automated chemiluminescence vs RIA aldosterone assay in primary aldosteronism work-up. J. Hum. Hypertens. 31(12), 826–830 (2017).
Nishikawa, T. et al. Calibration and evaluation of routine methods by serum certified reference material for aldosterone measurement in blood. Endocr. J. 63(12), 1065–1080 (2016).
Kobayashi, H. et al. Impact of a change to a novel chemiluminescent immunoassay for measuring plasma aldosterone on the diagnosis of primary aldosteronism. Endocr. J. 70(5), 489–500 (2023).
Teruyama, K., Naruse, M., Tsuiki, M. & Kobayashi, H. Novel chemiluminescent immunoassay to measure plasma aldosterone and plasma active renin concentrations for the diagnosis of primary aldosteronism. J. Hum. Hypertens. 36(1), 77–85 (2021).
Nishikawa, T. et al. Comparison and commutability study between standardized liquid chromatography-mass spectrometry/mass spectrometry (LC-MS/MS) and chemiluminescent enzyme immunoassay for aldosterone measurement in blood. Endocr. J. 69(1), 45–54 (2022).
Noh, J., Lee, C., Kim, J. H., Myung, S. W. & Choi, M. H. LC-MS based simultaneous profiling of adrenal hormones of steroids, catecholamines, and metanephrines. J. Lipid Res. 6, 100453 (2023).
Ng, E. et al. Aldosterone, renin, and aldosterone-to-renin ratio variability in screening for primary aldosteronism. J. Clin. Endocrinol. Metab. 108(1), 33–41 (2022).
Chen, F. et al. A liquid chromatography-tandem mass spectrometry (LC-MS/MS)-based assay for simultaneous quantification of aldosterone, renin activity, and angiotensin II in human plasma. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 1179, 122740 (2021).
Liu, Z., Jin, L., Zhou, W. & Zhang, C. The spectrum of plasma renin activity and hypertension diseases: Utility, outlook, and suggestions. J. Clin. Lab. Anal. 36(11), e24738 (2022).
Tan, X., Li, F., Wang, X. & Wang, Y. Quantitation and clinical evaluation of plasma aldosterone by ultra-performance liquid chromatography–mass spectrometry. J. Chromatogr. A 1609, 460456 (2020).
Satoh, F. et al. New screening cutoff values for detection of aldosteronoma examined by LC-MS/MS and newly developed non-competitive Cleia. J. Hypertens. 41, e36 (2023).
Ono, Y. et al. Screening cutoff values for the detection of aldosterone-producing adenoma by LC-MS/MS and a novel noncompetitive CLEIA. J. Endocr. Soc. 8(6), bvae080 (2024).
Vorselaars, W. M. C. M., Valk, G. D., Vriens, M. R., Westerink, J. & Spiering, W. Case detection in primary aldosteronism: High-diagnostic value of the aldosterone-to-renin ratio when performed under standardized conditions. J. Hypertens. 36(7), 1585–1591 (2018).
Nishizaka, M. K., Pratt-Ubunama, M., Zaman, M. A., Cofield, S. & Calhoun, D. A. Validity of plasma aldosterone-to-renin activity ratio in African American and white subjects with resistant hypertension”. Am. J. Hypertens. 18(6), 805–812 (2005).
Calhoun, D. A., Nishizaka, M. K., Zaman, M. A., Thakkar, R. B. & Weissmann, P. Hyperaldosteronism among black and white subjects with resistant hypertension. Hypertension 40(6), 892–896 (2002).
Gomez-Sanchez, C. E. et al. Immunohistochemistry of the human adrenal CYP11B2 in normal individuals and in patients with primary aldosteronism. Horm. Metab. Res. 52(6), 421–426 (2020).
Ward, G., Simpson, A., Boscato, L. & Hickman, P. E. The investigation of interferences in immunoassay. Clin. Biochem. 50(18), 1306–1311 (2017).
Seiler, L. et al. Diagnosis of primary aldosteronism: Value of different screening parameters and influence of antihypertensive medication. Eur. J. Endocrinol. 150(3), 329–337 (2004).
Tuhan, H. U. et al. Cross-reactivity of adrenal steroids with aldosterone may prevent the accurate diagnosis of congenital adrenal hyperplasia. J. Pediatr. Endocrinol. Metab. 28(5–6), 701–704 (2015).
Acknowledgements
We extend our sincere appreciation Dr. Hisashi Koide for the valuable discussion and to Yae Sano for technical support. This work was supported by grants from the Ministry of Education, Culture, Sports, Science and Technology (Japan): Grants-in-Aid for Scientific Research (B) #21H02974, #19H03708, and #22300325 and (C) #22K08644, #22K07205, #22K08619, #21K07145, #21K08524, #20K08397, #20K07561, #19K07635, 19K08972, #18K07439, and #18K08464; Challenging Research (Exploratory) #21K19398; Early-Career Scientists #20K17527; and Fund for the Promotion of Joint International Research (Fostering Joint International Research [A]) #19KK04071, #20KK0373, and #22KK0271. T. Tanaka was supported by the Japan Society for the Promotion of Science KAKENHI grant JP19H03708. This work was partly supported by The Uehara Memorial Foundation, Mochida Memorial Foundation for Medical and Pharmaceutical Research, The Naito Foundation, Mitsui Life Social Welfare Foundation, Princes Takamatsu Cancer Research Fund, Takeda Science Foundation, Senshin Medical Research Foundation, Japan Diabetes Foundation, Yamaguchi Endocrine Research Foundation, The Cell Science Research Foundation, The Ichiro Kanehara Foundation for the Promotion of Medical Sciences and Medical Care, the Yasuda Memorial Medical Foundation, MSD Life Science Foundation, The Hamaguchi Foundation for the Advancement of Biochemistry, The Novartis Foundation (Japan) for Promotion of Science, Kose Cosmetology Research Foundation, and the Medical Institute of Bioregulation Kyushu University Cooperative Research Project Program.
Author information
Authors and Affiliations
Contributions
Y.T., T.K., K.T., T.I. and T.T. designed the study. Y.T., T.K., H.M, I.S., S.K., and M.F. collected clinical information and conducted the experiments. Y.T., T.K., S.K., N.H., E.K., and T.M., performed statistical analyses. Y.T., T.K., N.H., M.Y. and T.T. analyzed, discussed. Y.T., T.K. and T.T. interpreted the data, coordinated and directed the project, and wrote the manuscript. All authors All authors reviewed the manuscript and have approved the submitted manuscript.
Corresponding author
Ethics declarations
Competing interests
All authors affiliated with Chiba University and Saiseikai Yokohamashi Tobu Hospital (Yuki Taki, Takashi Kono, Hidekazu Nagano, Hiroka Miyagawa, Satomi Kono, Masanori Fujimoto, Ikki Sakuma, Naoko Hashimoto, Masataka Yokoyama, Eiryo Kawakami, Takashi Miki, Tomoaki Tanaka, and Takamasa Ichijo, respectively) have no competing financial interests. Kyoko Teruyama is a full-time employee of Fujirebio Inc. and has no competing financial interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Taki, Y., Kono, T., Teruyama, K. et al. Comparative analysis of aldosterone and renin assays for primary aldosteronism screening. Sci Rep 14, 26040 (2024). https://doi.org/10.1038/s41598-024-75645-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-75645-1