Abstract
Synthesis, solubility and cytotoxicity evaluation of anionic phosphonates derived from betulin, betulinic acid, oleanolic acid and ursolic acid is reported. Phosphonate moieties were successfully installed at terpenoid C28 by carboxylic acid deprotonation/alkylation sequence using (dimethoxyphosphoryl)methyl trifluoromethanesulfonate as alkylation reagent. Also, betulin-derived and ether-linked bis-phosphonate is obtained and characterized. After demethylation in the presence of TMSI the resulting phosphonic acids were transformed into their disodium salts. All target compounds display excellent water solubility, which was determined by qNMR in D2O. Cytotoxicity tests were performed in different concentrations of each compound (10–50 µM) against human osteosarcoma cell line MG-63 and osteoblast precursor cell line MC3T3-E1. Improved aqueous solubility and low cytotoxicity profile of the newly designed triterpenoid phosphonates reveal high potential for various medicinal chemistry and pharmacological applications in the future.
Similar content being viewed by others
Introduction
People have used various plant-derived products as remedies for illnesses since prehistoric times. Also, in the modern era, approximately a quarter of drugs are inspired by or derived from natural products. This is particularly pronounced in anticancer and anti-infective areas, where during the past four decades, more than half of drugs are either natural products or natural product derivatives, mimics of natural products, or compounds bearing natural product pharmacophore1. The use of naturally abundant agents can help to reduce toxic and side effects due to low toxicity profile in normal cells2. Enhanced safety and cost-effectivity promote natural products to great multitarget drug candidates3.
Pentacyclic triterpenoids (PCTs) belong to a widespread family of natural isoprene-derived secondary metabolites, which exhibit a broad spectrum of biological properties4,5,6,7,8. PCTs can be classified into three major groups: lupane (betulin, betulinic acid, and lupeol), oleanane (oleanolic acid, maslinic acid, erythrodiol, and β-amyrin) and ursane (ursolic acid, uvaol, and α-amyrin)9. The ubiquity of PCTs in nature, renewability and their facile isolation process have resulted in numerous studies that have explored potential therapeutic applications of these terpenoids. Among them, the most promising PCTs applications are in the anticancer and antiviral domains10,11,12,13,14,15,16. Emerging application fields of PCTs and their semi-synthetic derivatives include the search for antibacterial8,17 and antifungal agents18,19, and compounds that can treat diabetes20,21 and inflammatory conditions22,23.
However, the development of PCTs drugs is often jeopardized by their physicochemical properties that are characteristic of natural plant compounds – poor solubility in physiological media and low bioavailability24,25,26,27,28,29.The latter can be explained by the high lipophilicity of the steroidal core30, which leads to extremely low aqueous solubility. For example, the solubility of betulinic acid in distilled water is 21 ng/mL and 40.1 µg/mL at pH 11.4 in sodium phosphate solution31. Improvement of aqueous solubility is a possible option to overcome this limitation32, and it can be achieved by chemical modifications of the terpenoid structure33,34,35.One of the approaches is to decorate the lipophilic carbon skeleton either with heteroatoms36,37,38 or with polar ionogenic groups39.
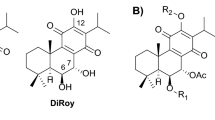
PCTs such as betulinic, ursolic and oleanolic acids possess intrinsic polar ionogenic carboxylate group at C(28), which can be easily transformed into different anionic salts by treatment with alkali and quaternary ammonia hydroxides (Fig. 1). As an example, choline oleanolate displayed the best solubility (81.7 µg/mL) in a simulated gastric juice (aqueous solution of NaCl and sodium dodecyl sulfate, which was adjusted to pH 1.2 by HCl solution)40,41. However, solubility studies of potassium and sodium PCT carboxylates did not show satisfactory results, due to the formation of colloids at concentrations above 0.02 mg/g, which significantly complicated the solubility determination.
On the other hand, various semi-synthetic cationic PCT conjugates were reported during the past decade. Various ammonium42,43, guanidinium44 and imidazolium45 moieties possessing diverse counterions were attached to PCTs cores through different type and size linkers. Similarly, C(2), C(28) and C(30) PCT triphenylphosphonium salts have been synthesized and biologically evaluated46,47. Unfortunately, solubility data of these cationic PCTs were not reported.
Speaking about alternative semi-synthetic anionic PCT derivatives, sulfate48,49,50 and phosphate51,52,53,54,55,56,57,58,59,60 groups have been added to the PCTs cores by corresponding sulfation or phosphorylation of C(3)-OH or/and C(28)-OH groups. PCT-derived mono and diphosphates provide a wide range of biological applications. However, detailed aqueous solubility studies thereof are not available. Even if O-phosphorylation and O-sulfatation of terpenoids may improve their biological activity properties by making structural and spatial changes61, the use of such modified compounds can be hampered by low hydrolytic stability62,63.
The latter issue can be overcome by replacing the phosphates with isosteric and isoelectronic, yet more stable phosphonates. This approach has made phosphonate derivatives a prominent class of biologically active compounds that have been developed particularly well in the area of antiviral nucleotide drugs64,65,66,67. Phosphonates as phosphate mimics have also been studied in the triterpenoid series, but the reported examples are quite scarce. Thus, phosphonate moieties have been attached to the PCT core by an amide bond68 or C-C bond (Fig. 1)69,70. To the best of our knowledge, there is only one example of PCT-phosphonate connected by C(28) carboxylic ester71. Nevertheless, the conversion of the reported phosphonates to phosphonic acids or their salts is still unexplored, and the water solubility of such ionogenic species has not been described.
Herein, we report the design and synthesis of novel pentacyclic triterpenoid – phosphonate conjugates of type C(17)-COO-CH2-P and C(3/28)-O-CH2-P, where the phosphonate moiety is attached to the terpenoid core by the simplest possible methylene linker and chemically bound by ester or ether moiety (Fig. 1). It is important to note, that the PCT’s C(28) esters are hydrolytically stable and can resist basic and acidic treatment72,73,74. Thus, we demonstrate with the present report that such phosphonate esters and phosphonate sodium salts are straightforward to achieve and the latter are very soluble in aqueous solutions, which is often a delicate task to achieve in the field of triterpenoid chemistry.
Results and discussion
Synthesis
Initially, we speculated that the incorporation of methylene phosphonate moiety can be achieved through the ester bond formation between the triterpenic acid C28 carboxylate group and dialkyl (hydroxymethyl) phosphonate via activation of carboxylic acid. For this purpose, we have prepared a series of 3-oxo PCT carboxylic acids 2a-c starting from commercially available betulin 1a, oleanolic acid 1b and ursolic acid 1c. 3-Oxo triterpenic acids 2a-c were successfully converted into corresponding acyl chlorides by SOCl2 treatment, but further reaction with dimethyl (hydroxymethyl)phosphonate was found to be inefficient, due to low conversion of the chloride into the desired product. Following screening of the reaction conditions did not bring the desired result, and the best yield that we reached was 30%. The weak reactivity of triterpenic acid chlorides can be explained by the steric hindrance at C(28) position. Some sources demonstrate that PCT acid halides are capable of reacting with amines75 and phenols76, but insufficient nucleophilicity of alcohols, together with the electron withdrawing effect of phosphonate moiety, makes it even more complicated.
Therefore, we decided to switch reactivity and explore a possible carboxylate alkylation reaction77, in which the reaction site is one atom further from the C(17) quaternary center.
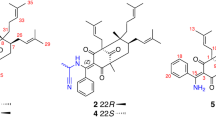
We discovered that 3-oxo triterpenic acids 2a-c underwent rapid deprotonation followed by alkylation with (dimethoxyphosphoryl)methyl trifluoromethanesulfonate in the presence of t-BuOK in anhydrous THF (Fig. 2). The used triflate is readily available from the previously mentioned alcohol78. The desired esters 3a-c were obtained in good yields. Next, 3-hydroxy triterpenic phosphonates 4a-c were obtained by diastereoselective reduction of C(3) ketones. A similar approach using (dimethoxyphosphoryl)methyl trifluoromethanesulfonate in a combination with 3-hydroxy triterpenic acids 1b, c provided a direct access to compounds 4b, c (process 1b, c → 4b, c Fig. 2), yet with a lower yield due to side reactions that implied laborious purification of the products. For the transformation 1b, c → 4b, c K2CO3 was used as a weaker base to achieve a better selectivity between C(17)-COOH and C(3)-OH alkylation, but this required a solvent change to DMF for a better solubility if the base. The latter protocol resulted also in transesterification between C(17)-COOH and phosphonic acid methyl ester moiety of the alkylation reagent yielding C(17)-COOMe side product accompanied by TfOCH2P(O)(OH)(OMe), the separation of which required additional reverse phase chromatography on C18-silica. Therefore, the developed sequence 2 → 3 → 4 is optimal, as it provides clean transformations and ensures access to both C(3)-OH and C(3) = O series of triterpenoids.
With the whole series of the desired phosphonates in hand, next we examined the transformation of phosphonates into sodium phosphonates 7a-c and 8a-c employing TMSI assisted demethylation followed by the conversion of phosphonic acids 5a-c and 6a-c into their salts (Table 1; Fig. 3). Starting with the betulonic acid derived phosphonate 3a (Table 1), we found that the demethylation must be carried out at -40 °C. At higher temperatures betulinic acid olefin moiety underwent cationic rearrangements79 and cleavage of the previously installed ester was observed (Table 1, entries 1, 2). We supposed that the methanolysis of the intermediate O-TMS-phosphonates could also be accomplished at a lowered temperature, but the undesired side product was still formed during the evaporation of the solvent (Table 1, entry 3). Neutralization of HI before warming up the reaction mixture was found to be crucial (Table 1, entry 4). Therefore, sodium bicarbonate aqueous solution must be added subsequently at a lowered temperature, ensuring neutralization of HI and formation of sodium salt 7a.
The developed demethylation conditions for the transformation 3a → 7a were successfully applied on all other compound series consisting of betulinic acid derivative 4a with free C(3)-OH group, 3-oxo-series of oleanolic and ursolic acid-derived phosphonates 3b, c and their corresponding C(3)-OH derivatives 4b, c (Fig. 3). The target products 7a-c and 8a-c were obtained in good to excellent yields and isolated by a simple precipitation/centrifugation approach.
As expected, the obtained products 7a-c and 8a-c were hydrolytically very stable and an eventual cleavage of the carboxylate ester bond was not observed even after heating under two different basic conditions: (1) 60 °C in 1.5 M NaOH/MeOH solution for 6 h; (2) 100 °C in the presence of 4 equiv. NaOH in H2O for 24 h. The obtained ionogenic derivatives revealed excellent water solubility, which can be nicely demonstrated by the acquisition of their 1H NMR spectra in D2O (Fig. 4).
Next, we investigated the installation of phosphonate moiety via an ether bond (Table 2). Starting with betulin, the most abundant natural PCT-3,28-diol, we examined a one-pot double alkylation possibility involving both hydroxyl groups. Application of such strong bases as NaH, t-BuOK, n-BuLi and MeMgBr in combination with (dimethoxyphosphoryl)methyl trifluoromethanesulfonate or tosylate were found to be ineffective (Table 2, entries 1–6). On many occasions we detected the degradation of alkylating reagent. To our delight, we have finally found that combining triflate alkylation reagent (2.2 equiv.) and betulin Li-dialkoxide arising from LDA (lithium diisopropylamide) (2.1 equiv.) provided the expected product 9 in 29% isolated yield (Table 2, entry 9). The desired product 9 was accompanied by the C(28)-O-monoalkylation product 10 and C(28)-O-phosphonylation product 11 in the 9:10:11 ratio 51:20:29 (by NMR). The latter arises from the alkoxide attack on the phosphorous center due to the presence of two competing electrophilic reaction centers in (dimethoxyphosphoryl)methyl trifluoromethanesulfonate. The obtained tetramethyl bis-phosphonate 9 was converted to tetrasodium salt (78%) using the previously developed TMSI conditions (Fig. 5).
Compound solubility and cytotoxicity evaluation
The obtained PCT-derived sodium phosphonates were subjected to water solubility tests (Table 3). For this purpose, we used a quantitative 1H-NMR approach in D2O, using potassium hydrogen phthalate as an external standard (for experimental details see Supporting Information). The presence of the basic forms of phosphonates80 was ensured by the careful addition of NaOD, maintaining pH 8.0–8.5 during the quantification, which is 2–3 units higher than the pKa of phosphonic acid disalt81. As expected, our newly designed phosphonates 7a-c, 8a-c and 12 exhibited excellent aqueous solubility in a range from 3 to 26 mg/mL (pH 8.0–8.5). This is by at least two to three orders of magnitude higher than the reported solubilities of the parent natural triterpenic acids. For example, aqueous solubility of oleanolic and betulinic acids are < 0.1 µg/mL at neutral pH and can be increased to 42.1 µg/mL for betulinic acid and 99.5 µg/mL for oleanolic acid at pH 11.831. Also, parent ursolic acid exhibits a similarly low aqueous solubility29, which can be enhanced to some extent by various modern drug delivery systems26,27,28. Indeed, phosphonic acids are more acidic and easier ionizable than carboxylic acids. This ionic character helps to increase the aqueous solubility as exemplified by here described compounds. On the other hand, a direct numerical comparison of the aqueous solubility of compounds 7a-c, 8a-c and 12 with the reported triterpenoid phosphate/phosphonate analogs51,52,53,54,55,56,57,58,59,60 is burdened as most of the previous reports describe the obtained enhanced solubility in a qualitative manner.
All target compounds were studied to determine their cytotoxic activity at various concentrations of each compound (10–50 µM) against human-derived osteosarcoma cell line MG-63 (ATCC, CRL-1427) and mouse-derived preosteoblast cell line MC3T3-E1 (ATCC, CRL-2593) (Table 4 and Figures S1-S4 in the Supporting Information). For the comparison, naturally occurring betulinic, oleanolic (1b) and ursolic (1c) acids as well as their 3-oxo analogs 2a-c and doxorubicin, were also subjected to the cytotoxicity tests. As expected, the designed water-soluble PCT-derived phosphonates and the natural triterpenic acids, including their 3-oxo-analogs, were harmless to the MC3T3-E1 cells. As an interesting observation and exception should be mentioned the concentration-dependent cell viability drop of MC3T3-E1 cells in the presence of oleanonic acid (0.49 ± 0.12 relative metabolic activity at 50 µM of 2b). To a lesser extent, ursonic acid affected the metabolic activity of MC3T3-E1 cells (0.72 ± 0.09 relative metabolic activity at 50 µM of 2c).
Nevertheless, in the presence of oleanonic acid-derived phosphonate 8b the MG-63 cell line revealed somewhat lower metabolic activity (0.73 ± 0.05 relative metabolic activity at 50 µM of 8b) than in the presence of its parental oleanonic acid (1.03 ± 0.18 for 2b). It is interesting to note that ursolic acid (1c) and ursonic acid (2c) showed a cytotoxic effect towards MG-63 cell line in the cell viability tests (0.28 ± 0.04 and 0.67 ± 0.04 relative metabolic activity at 50 µM of 1c and 2c, respectively).
In summary, we have developed a practical synthetic approach for introduction of the simplest phosphonate moiety, containing only single methylene group, into the PCT core via an ester and an ether bond. The corresponding TMSI induced phosphonate demethylation, which provided the target sodium phosphonates, was optimized for a preparative application avoiding acid promoted cationic rearrangements of the triterpenic core. Phosphonate disodium salts were obtained and characterized for the pentacyclic triterpenoids in the betulinic, oleanolic and ursolic acid series, including their 3-oxo-derivatives. All target compounds possess excellent aqueous solubility (3–26 mg/mL at pH 8.0–8.5), which was properly quantified by qNMR. Thus, this report stands out with the sample 1H NMR spectra of pentacyclic triterpenoid derivatives acquired in D2O. The preliminary cytotoxicity evaluation of the target products revealed that the obtained PCT-derived sodium phosphonates do not possess significant cytotoxicity profile towards normal cells. This fact provides a promising possibility for future studies of these and similar phosphonate derivatives in those biological activity domains that require high selectivity between normal mammalian cells and external factors, such as viral, bacterial and fungal pathogens. Due to their non-toxic nature the title compounds classify also for further studies in the field of antidiabetic and anti-inflammatory agents.
Methods
Synthesis: general information
Solvents for the reactions were dried over standard drying agents and freshly distilled prior to use. All purchased chemicals (Fluka, Aldrich) were used as received. All reactions were followed by TLC on E. Merck Kieselgel 60 F254 and visualized by using UV lamp. Column chromatography was performed on silica gel (60 Å, 40–63 μm, ROCC). Flash column chromatography was performed on a Büchi Sepacore system (Büchi-Labortechnik GmbH, Essen, Germany) with a Büchi Control Unit C-620, an UV detector Büchi UV photometer C-635, Büchi fraction collector C-660 and two Pump Modules C-605. 1H and 13C NMR spectra were recorded on a Bruker 300 and 500 MHz, in CDCl3 or [D4]MeOD at 25 °C. Chemical shifts (δ) values are reported in ppm. The residual solvent peaks are used as internal reference (CDCl3) 7.26 ppm, [D4]MeOD 3.31 ppm for 1H NMR, CDCl3 77.16 ppm, [D4]MeOD 49.00 ppm for 13C NMR), s (singlet), d (doublet), t (triplet), q (quartet), m (multiplet); J in hertz. 1H and 13C NMR peaks were assigned by analysis of multidimensional NMR (COSY, HSQC, HMBC). For 31P NMR calibration, Ph3P was used as external reference (-6.00 ppm in MeODd4) in a coaxially inserted tube. High-resolution massspectra (ESI) were performed on Agilent 1290 Infinity series UPLC connected to Agilent 6230 TOF mass spectrometer (calibration at m/z 121.050873 and m/z 922.009798). Optical rotation was measured at 20 °C on Anton Paar MCP 500 polarimeter (1-cm cell) using multi-wavelength analysis (589 nm, 546 nm, 436 nm, 405 nm, 365 nm).
General procedure I for the synthesis of 3-oxo-triterpenic acid esters, process 2a-c → 3a-c
To solution of 3-oxo-triterpenic acid 2a-c (500 mg, 1.099 mmol, 1 eq.) in anhydrous THF (5 mL) tBuOK (185 mg, 1.649 mmol, 1 eq.) is added portion wise at -5 °C. The resulting reaction mixture is stirred in ambient temperature for 30 min, then warmed up to room temperature and stirred for additional 60 min. The obtained mixture is re-cooled to -5 °C and a solution of previously prepared (dimethoxyphosphoryl)methyl trifluoromethanesulfonate (629 mg, 2.198 mmol, 2 eq.) in anhydrous THF (5 mL) is added dropwise. Then the resulting reaction mixture is warmed up to room temperature and stirred for 12 h. The reaction mixture is evaporated to dryness, redissolved in EtOAc (70 mL) and washed with brine (3 × 10 mL). Separated organic layer is dried over anhydrous Na2SO4. After filtration, the filtrate is concentrated in vacuo and purified by silica column chromatography (Hexanes-EtOAc 9:1 → 1:1) to yield carboxylic ester as a white amorphous solid: 3a (78%, 495 mg); 3b (61%, 387 mg), 3c (71%, 450 mg).
3-oxo-(17 S)-17-(((dimethoxyphosphoryl)methoxy)carbonyl)-28-norlup-20(29)-ene 3a
1H NMR (500 MHz, CDCl3) δ 4.73 (s, 1H, Ha-C(29)), 4.60 (s, 1H, Hb-C(29)), 4.48 (dd, 2J = 14.6, 8.3 Hz, 1H, Ha-C(28’)), 4.39 (dd, 2J = 14.6, 8.2 Hz, 1H, Hb-C(28’)), 3.81 (d, 3J = 10.9, 6 H, (OMe)2), 2.98 (td, 3J = 11.1, 4.8 Hz, 1H, H−C(19)), 2.48 (ddd, 2J = 15.5 Hz, 3J = 9.8, 7.5 Hz, 1H, Ha-C(2)), 2.39 (ddd, 2J = 15.5 Hz, 3J = 7.6, 4.4 Hz, 1H, Hb-C(2)), 2.31–2.19 (m, 2H, Ha-C(16), H-C(13)), 1.96–1.82 (m, 4 H, Ha-C(15), Ha-C(21), Ha-C(22), Ha-C(1)), 1.76–1.69 (m, 1H, Ha-C(12)), 1.68 (s, 3H, H3-C(30)), 1.62 (t, 3J = 11.4 Hz, 1H, H-C(18)), 1.54–1.34 (m, 9 H, H2-C(6), Ha-C(11), H2-C(7), Hb-C(21), Hb-C(1), H-C(9), Hb-C(16)), 1.34–1.14 (m, 4 H, Hb-C(11), Hb-C(15), Hb-C(22), H-C(5)), 1.06 (s, 3H, H3-C(23)), 1.06–1.01 (m, 1H, Hb-C(12)), 1.01 (s, 3H, H3-C(24)), 0.97 (s, 3H, H3-C(27)), 0.96 (s, 3H, H3-C(26)), 0.92 (s, 3H, H3-C(25)). 13C NMR (126 MHz, CDCl3) δ 218.25 (C3), 174.91 (d, 3J = 6.4 Hz, (C28)), 150.34 (C20), 109.96 (C29), 56.90 (C17), 55.18 (d, 1J = 167.4 Hz), 55.10 (C5), 53.20 (d, 2J = 6.2 Hz, MeO), 53.18 (d, 2J = 6.2 Hz, MeO), 50.04 (C9), 49.49 (C18), 47.46 (C4), 46.90 (C19), 42.61 (C14), 40.77 (C10), 39.77 (C1), 38.44 (C13), 37.04 (C21), 37.00 (C10), 34.26 (C2), 33.75 (C7), 32.03 (C16), 30.53 (C22), 29.65 (C15), 26.74 (C23), 25.65 (C12), 21.54 (C11), 21.15 (C24), 19.76 (C30), 19.47 (C6), 16.10 (C25), 15.85 (C26), 14.74 (C27). 31P NMR (121 MHz, CDCl3) δ 21.77. HRMS: [C33H53O6P + H+] 577.3653; found 577.3626 (4.7 ppm). \(\:[{\alpha]}_{D}^{20}=\:+0.19\); \(\:[{\alpha]}_{546}^{20}=\:+0.23\); [\(\:{\alpha]}_{436}^{20}=\:+0.50\); \(\:[{\alpha]}_{405}^{20}=\:+0.66\); \(\:{[\alpha]}_{365}^{20}=\:+1.02\) (c = 1.00, MeOH).
3-oxo-(17 S)-17-(((dimethoxyphosphoryl)methoxy)carbonyl)-28-norolean-12(13)-ene 3b
1H NMR (500 MHz, CDCl3): δ 5.32 (t, 3J = 3.6 Hz, 1H, H-C(12)), 4.42 (dd, 2J = 14.0, 8.6 Hz, 1H, Ha-C(28`)), 4.32 (dd, 2J = 14.0, 8.6 Hz, 1H, Hb-C(28`)), 3.81 (d, 2J = 10.8 Hz, 6 H, (MeO)2), 2.88 (dd, 3J = 14.0, 4.3 Hz, 1H, H-C(18)), 2.55 (ddd, 2J = 15.9 Hz, 3J = 11.2, 7.2 Hz, 1H, Ha-C(2)), 2.36 (ddd, 2J = 15.9 Hz, 3J = 6.8, 3.6 Hz, 1H, Hb-C(2)), 2.01 (dt, 2J = 14.0 Hz, 3J = 4.3 Hz, 1H, Ha-C(16)), 2.00–1.90 (m, 2H, H2-C(11)), 1.88 (ddd, 2J = 13.2 Hz, 3J = 7, 3.6 Hz, 1H, Ha-C(1)), 1.72 (dt, 1H, 2J = 13.6 Hz, 3J = 4.1 Hz, Ha-C(22)), 1.69–1.53 (m, 5 H, Hb-C(16), Ha-C(19), H-C(9), Ha-C(7), Ha-C(15)), 1.52–1.47 (m, 3H, H2-C(6), Hb-C(7)), 1.40 (dt, 2J = 12.3 Hz, 3J = 6.0 Hz, 1H, Hb-C(1)), 1.35–1.28 (m, 4 H, Hb-C(22), Ha-C(21), H-C(5), Hb-C(6)), 1.26–1.08 (m, 3H, Hb-C(21), Hb-C(19), Hb-C(15)), 1.14 (s, 3H, H3-C(27)), 1.08 (s, 3H, H3-C(23)), 1.04 (s, 6 H, H3-C(24), H3-C(25)), 0.92 (s, 3H, H3-C(29)), 0.90 (s, 3H, H3-C(30)), 0.78 (s, 3H, H3-C(26)). 13C NMR (126 MHz, CDCl3): δ 217.90 (C(3)), 176.77 (d, 3J= 8.0 Hz, (C28)), 143.55 (C13), 122.65 (C12), 55.82 (d, 1J = 168.7 Hz, (C28`)), 55.47 (C5), 53.24 (d, 2J= 6.4 Hz, (MeO)2), 47.60 (C4), 47.25 (C17), 46.98 (C9), 45.90 (C19), 41.96 (C14), 41.54 (C18), 39.40 (C8), 39.29 (C1), 36.89 (C10), 34.31 (C2), 33.91 (C21), 33.16 (C30), 32.37 (C7), 32.32 (C22), 30.81 (C20), 27.75 (C15), 26.56 (C23), 25.87 (C27), 23.66 (C29), 23.65 (C11), 23.19 (C16), 21.63 (C24), 19.72 (C6), 16.95 (C26), 15.18 (C25). 31P NMR (121 MHz, CDCl3) δ 21.74. HRMS: [C33H53O6P + H+] 577.3653; found 577.3626 (4.7 ppm). \(\:[{\alpha]}_{D}^{20}=\:+0.66\); \(\:[{\alpha]}_{546}^{20}=\:+0.79\); [\(\:{[\alpha]}_{436}^{20}=\:+1.38\); \(\:[{\alpha]}_{405}^{20}=\:+1.70\); \(\:{[\alpha]}_{365}^{20}=\:+2.28\) (c = 1.00, MeOH).
3-oxo-(17 S)-17-(((dimethoxyphosphoryl)methoxy)carbonyl)-28-norurs-12(13)-ene 3c
1H NMR (500 MHz, CDCl3) δ 5.29 (d, 3J = 3.8 Hz, 1H, H-C(12)), 4.33 (d, 2J = 8.5 Hz, 2H, H2-C(28’)), 3.80 (d, 3J = 10.8 Hz, 6 H, (OMe)2), 2.55 (ddd, 2J = 16.0 Hz, 3J = 10.8, 7.5 Hz, 1H, Ha-C(2)), 2.37 (ddd, 2J = 16.0 Hz, 3J = 6.9, 3.6 Hz, 1H, Hb-C(2)), 2.25 (d, 3J = 11.3 Hz, 1H, H-C(18)), 2.04 (td, 2J = 14.4, 3J = 6.5 Hz, 1H, Ha-C(16)), 1.99–1.92 (m, 2H, H2-C(11)), 1.90 (ddd, 2J = 12.0 Hz, 3J = 7.4, 3.6 Hz, 1H, Ha-C(1)), 1.80–1.68 (m, 3H, Hb-C(16), Ha-C(15), Ha-C(21)), 1.65–1.55 (m, 2H, Hb-C(21), H-C(9)), 1.55–1.39 (m, 5 H, H2-C(6), Ha-C(15), Ha-C(7), Hb-C(1)), 1.39–1.23 (m, 4 H, Hb-C(22), Hb-C(7), H-C(19, H-C(5)), 1.17–1.11 (m, 1H, Hb-C(15)), 1.09 (s, 3H, H3-C(27)), 1.08 (s, 3H, H3-C(28)), 1.04 (s, 6 H, H3-C(24), H3-C(25)), 1.04–0.98 (m, 1H, H-C(20)), 0.94 (d, 3J = 6.3 Hz, 3H, H3-C(30)), 0.86 (d, 3J = 6.4 Hz, 3H, H3-C(29)), 0.79 (s, 3H, H3-C(26)). 13C NMR (126 MHz, CDCl3) δ 217.95 (C3), 176.62 (d, 3J = 8.2 Hz, (C28)), 138.02 (C13), 125.83 (C12), 55.81 (d, 1J = 168.9 Hz, (C28’)), 55.13 (C5), 53,24 (d, 2J = 6.1 Hz, (OMe)), 53.21 (d, 2J = 6.1 Hz, (OMe)), 53.07 (C18), 48.64 (C17), 47.55 (C4), 46.86 (C9), 42.28 (C14), 39.60 (C8), 39.44 (C1), 39.17 (C19), 38.91 (C20), 36.79 (C10), 36.58 (C21), 34.31 (C2), 32.65 (C7), 30.68 (C22), 28.08 (C15), 26.67 (C23), 24.32 (C16), 23.59 (C27), 23.58 (C11), 21.63 (C24), 21.24 (C30), 19.71 (C6), 17.12 (C29), 17.05 (C26), 15.37 (C25). 31P NMR (121 MHz, CDCl3) δ 21.85. HRMS: [C33H53O6P + H+] 577.3653; found 577.3623 (5.2 ppm). \(\:[{\alpha]}_{D}^{20}=\:+0.50\); \(\:[{\alpha]}_{546}^{20}=\:+0.58\); [\(\:{[\alpha]}_{436}^{20}=\:+0.97\); \(\:[{\alpha]}_{405}^{20}=\:+1.23\); \(\:{[\alpha]}_{365}^{20}=\:+1.62\) (c = 1.00, MeOH).
General procedure II for synthesis of 3-hydroxy-triterpenic acid esters, process 3a-c → 4a-c
To solution of 3-oxo-triterpenoic acid ester 3a-c (200 mg, 0.347, 1 eq.) in MeOH (4 mL) NaBH4 (53 mg, 1.388 mmol, 4 eq.) is added portion wise at 0 °C. The resulting reaction mixture is stirred at ambient temperature for 5 h. Then the reaction mixture is quenched by NH4Cl saturated aqueous solution (2 mL), evaporated to dryness, redissolved in EtOAc (25 mL) and washed with brine (3 × 10 mL). The combined organic layer is dried over anhydrous Na2SO4. After filtration, the filtrate is concentrated in vacuo and purified by silica column chromatography (Hexanes-EtOAc 9:1 → 1:1) to yield product as a white amorphous solid: 4a (99%, 198 mg); 4b (96%, 193 mg); 4c (92%, 185 mg).
(17 S)-17-(((dimethoxyphosphoryl)methoxy)carbonyl)-3β-hydroxy-28-norlup-20(29)-ene 4a
1H NMR (500 MHz, CDCl3) δ 6.02 (bs, 1H, OH), 4.73 (s, 1H, Ha-C(29)), 4.61 (s, 1H, Hb-C(29)), 4.48 (dd, 2J = 14.7, 8.2 Hz, 1H, Ha-C(28’), 4.39 (dd, 2J = 14.7, 8.2 Hz, 1H, Hb-C(28’), 3.81 (d, 3J = 10.8 Hz, 6 H, (OMe)2), 3.18 (dd, 3J = 11.4, 4.7 Hz, 1H, H-C(3)), 2.98 (td, 3J = 11.2, 4.7 Hz, 1H, H-C(19)), 2.30–2.34 (m, 1H, Ha-C(16)), 2.24–2.15 (m, 1H, H-C(13)), 1.98–1.83 (m, 2H, Ha-C(21), Ha-C(22)), 1.74–1.31 (m, 17 H, Ha-C(15), H3-C(C30), Ha-C(12), H-C(18), H2-C(6), Ha-C(11), H2-C(7), Hb-C(21), Ha-C(1), H-C(9), Hb-C(16), H2-C(2)), 1.31–1.13 (m, 3H, Hb-C(11), Hb-C(15), Hb-C(22)), 1.08–0.99 (m, 1H, Hb-C(12)), 0.96 (s, 6 H, H3-C(27), H3-C(26)), 0.92 (s, 3H, H3-C(23)), 0.90–0.85 (m, 1H, Hb-C(1)), 0.82 (s, 3H, H3-C(25)), 0.75 (s, 3H, H3-C(24)), 0.68 (d, 3J = 9,4 Hz, 1H, H-C(5)). 13C NMR (126 MHz, CDCl3) δ 174.97 (d, 3J = 6.4 Hz, (C28)), 150.46 (C20), 109.91 (C29), 79.12 (C3), 56.96 (C17), 55.0 (C5), 55.17 (d, 1J = 167.4 Hz, C(28’)), 53.20 (d, 2J = 6.1 Hz, (MeO)), 53.17 (d, 2J = 6.1 Hz, (MeO)), 50.70 (C9), 49.58 (C18), 46.96 (C19), 42.58 (C14), 40.85 (C8), 39.01 (C4), 38.88 (C1), 38.39 (C13), 37.35 (10), 37.05 (C21), 34.48 (C7), 32.12 (C16), 30.57 (C22), 29.70 (C15), 28.13 (C23), 27.55 (C2), 25.67 (C12), 21.03 (C11), 19.49 (C30), 18.44 (C6), 16.30 (C25), 16.07 (C26), 15.50 (C24), 14.85 (C27). 31P NMR (121 MHz, CDCl3) δ 21.88. HRMS: [C33H55O6P + H+] 579.3809; found 579.3782 (4.7 ppm). \(\:[{\alpha]}_{D}^{20}=\:-0.01\); \(\:[{\alpha]}_{546}^{20}=\:-0.01\); [\(\:{\alpha]}_{436}^{20}=\:+0.01\); \(\:[{\alpha]}_{405}^{20}=\:+0.02\); \(\:{[\alpha]}_{365}^{20}=\:+0.02\) (c = 1.00, MeOH).
(17 S)-17-(((dimethoxyphosphoryl)methoxy)carbonyl)-3β-hydroxy − 28-norolean-12(13)-ene 4b
1H NMR (500 MHz, CDCl3) δ 5.30 (t, 3J = 3.6 Hz, 1H, H-C(13)), 4.41 (dd, 2J = 14.6, 8.7 Hz, 1H, Ha-C(28’)), 4.31 (dd, 2J = 14.6, 8.3 Hz, 1H, Hb-C(28’)), 3.80 (d, 3J = 10.9 Hz, 6 H, (OMe)2), 3.25–3.17 (m, 1H, H-C(3)), 2.90–2.81 (m, 1H, H-C(18)), 2.07–1.95 (m, 1H, Ha-C(16)), 1.91–1.85 (m, 2H, H2-C(11)), 1.77–1.16 (m, 16 H, H2-C(6), Hb-C(16), H2-C(2), Ha-C(15), H2-C(22), H2-C(7), H2-C(21), H-C(9), Ha-C(1), H2-C(19)), 1.13 (s, 3H, H3-C(27)), 1.09 (d, 2J = 14.0 Hz, 1H, Hb-C(15)), 0.98 (s, 3H, H3-C(23)), 0.98–0.92 (m, 1H, Hb-C(1)), 0.92 (s, 3H, H3-C(29)), 0.90 (s, 6 H, H3-C(30), H3-C(25)), 0.78 (s, 3H, H3-C(24)), 0.77–0.72 (m, 1H, H-C(5)), 0.72 (s, 3H, H3-C(26)). 13C NMR (126 MHz, CDCl3) δ 176.81 (d, 3J = 7.8 Hz, (C28)), 143.49 (C12), 122.89 (C12), 79.16 (C3), 55.92 (d, 1J = 169.5 Hz, (C28’)), 55.13 (C5)), 53.23 (d, 2J = 6.3 Hz, (OMe)), 53.23 (d, 2J = 6.3 Hz, (OMe)), 47.73 (C9), 47.24 (C17), 45.97 (C19), 41.85 (C14), 41.48 (C18), 39.43 (C8), 38.90 (C4), 38.60 (C1), 37.18 (C10), 33.93 (C21), 33.18 (C30), 32.86 (C7), 32.38 (C22), 30.81 (C20), 28.25 (C23), 27.77 (C15), 27.34 (C2), 25.99 (C27), 23.69 (C29), 23.57 (C11), 23.21 (C16), 18.48 (C6), 17.02 (C26), 15.72 (C24), 15.48 (C25). 31P NMR (121 MHz, CDCl3) δ 21.77. HRMS: [C33H55O6P + NH4+] 596.4075; found 596.4042 (5.5 ppm). \(\:[{\alpha]}_{D}^{20}=\:+0.38\); \(\:[{\alpha]}_{546}^{20}=\:+0.46\); [\(\:[{\alpha]}_{436}^{20}=\:+0.79\); \(\:[{\alpha]}_{405}^{20}=\:+0.97\); \(\:[{\alpha]}_{365}^{20}=\:+1.27\) (c = 1.00, MeOH).
(17 S)-17-(((dimethoxyphosphoryl)methoxy)carbonyl)-3β-hydroxy-28-norurs-12(13)-ene 4c
1H NMR (500 MHz, CDCl3) δ 5.26 (bs, 1H, H-C(13)), 4.33 (d, 2J = 8.4 Hz, 2H, H2-C(28’)), 3.80 (d, 3J = 10.8 Hz, 6 H, (OMe)2), 3.21 (dd, 3J = 11.3, 4.6 Hz, 1H, H-C(3)), 2.23 (d, 3J = 11.3 Hz, 1H, H-C(18)), 2.10–1.99 (m, 1H, Ha-C(16)), 1.95–1.84 (m, 2H, H2-C(11)), 1.79–1.68 (m, 3H, Hb-C(16), Ha-C(15), Ha-C(21)), 1.67–1.22 (m, 12 H, Hb-C(21), Ha-C(1), H2-C(2), H2-C(6), H2-C(7), H2-C(22), H-C(9), H-C(19)), 1.13–1.08 (m, 1H, Hb-C(15)), 1.08 (s, 3H, H3-C(27)), 1.04–0.99 (m, 1H, H-C(20)), 0.99 (s, 3H, H3-C(23)), 0.99–0.94 (m, 1H, Hb-C(1)), 0.94 (d, 3J = 6,3 Hz, 3H, H3-C(30)), 0.92 (s, 3H, H3-C(25)), 0.86 (d, 3J = 6.6 Hz, 3H, H3-C(29)), 0.78 (s, 3H, H3-C(24)), 0.73 (s, 3H, H3-C(26)), 0.73–0.69 (m, 1H, H-C(5)). 13C NMR (126 MHz, CDCl3) δ 176.66 (d, 3J = 8.3 Hz, (C28)), 137.93 (C12), 126.08 (C13), 79.18 (C3), 55.81 (d, 1J = 168.9 Hz, (C28’)), 55.36 (C5), 53.25 (d, 2J = 6.4 Hz, (MeO)), 53.25 (d, 2J = 6.4 Hz, (MeO)), 53.03 (C18), 48.63 (C17), 47.67 (C9), 42.18 (C14), 39.65 (C8), 39.19 (C19), 38.95 (C20), 38.90 (C4), 38.77 (C1), 37.11 (C10), 36.64 (C21), 33.15 (C7), 30.72 (C22), 28.28 (C23), 28.12 (C25), 27.37 (C2), 24.37 (C16), 23.70 (C27), 23.45 (C11), 21.28 (C30), 18.46 (C6), 17.13 (C26), 17.09 (C29), 15.76 (C24), 15.62 (C25). 31P NMR (121 MHz, CDCl3) δ 21.77. HRMS: [C33H55O6P + H+] 579.3809; found 579.3781 (4.8 ppm). \(\:[{\alpha]}_{D}^{20}=\:+0.36\); \(\:[{\alpha]}_{546}^{20}=\:+0.43\); [\(\:[{\alpha]}_{436}^{20}=\:+0.76\); \(\:[{\alpha]}_{405}^{20}=\:+0.92\); \(\:[{\alpha]}_{365}^{20}=\:+1.20\) (c = 1.00, MeOH).
General procedure III for demethylation of phosphonic esters, processes 3a-b → 7a-c and 4a-c → 8a-c
To solution of 3-oxo-triterpenic acid ester 3a-c or 3-hydroxy-triterpenoic acid ester 4a-c (0.4 mmol, 1 eq.) in anhydrous DCM (5 mL) TMSI (171 µL 1.2 mmol, 3 eq.) is added dropwise at -40 °C and the resulting reaction mixture is stirred at -40 °C for 5 h. Then MeOH (2.5 mL) is added dropwise at -40 °C. The obtained mixture is stirred for additional 30 min at the same temperature and solution of NaHCO3 (101 mg, 1.2 mmol, 3 eq.) in H2O (4 mL) is added dropwise at -40 °C. The resulting reaction mixture is warmed up to room temperature and the organic solvents are evaporated in vacuo. The obtained aqueous suspension is centrifuged and the supernatant is removed and discarded. The precipitate is re-suspended in deionized water (1 mL) and the centrifugation – supernatant removal procedure is repeated additional two times (in total: washing with water 3 × 1mL). The obtained precipitated is dried at ambient temperature in vacuo: 7a ( 97%, 230 mg); 7b (90%, 214 mg); 7c (51%, 121 mg); 8a (91%, 217 mg); 8b (78%, 186 mg); 8c (93%, 222 mg).
Sodium (3-oxo-(17R)-17-28-norlup-20(29)-en)-2-oxoethyl-phosphonate 7a
1H NMR (500 MHz, MeODd4) δ 4.72 (s, 1H, Ha-C(29)), 4.58 (s, 1H, Hb-C(29)), 4.16 (dd, 2J = 13.1, 8.7 Hz, 1H, Ha-C(28’)), 3.90 (dd, 2J = 13.1, 8.4 Hz, 1H, Hb-C(29)), 3.02 (td, 3J = 11.2, 4.4 Hz, 1H, H-C(19)), 2.58–2.36 (m, 4 H, H2-C(2), H-C(13), Ha-C(16)), 2.24 (dd, 3J = 11.7, 8.1 Hz, 1H, Ha-C(21)), 2.00–1.86 (m, 2H, Ha-C(21), Hb-C(22)), 1.76 (d, 3J = 13.0 Hz, 1H, Ha-C(12)), 1.69 (s, 3H, H3-C(30)), 1.63 (t, 3J = 11.3 Hz, 1H, H-C(18)), 1.57–1.27 (m, 13H, H2-C(6), H2-C(11), H2-C(7), Ha-C(15), Hb-C(22), Hb-C(16), Hb-C(1), H-C(9), Hb-C(21), H-C(5)), 1.23–1.15 (m, 1H, Hb-C(22)), 1.13–1.06 (m, 1H, Hb-C(12)), 1.06 (s, 3H, H3-C(23)), 1.02 (s, 3H, H3-C(24)), 1.01 (s, 3H, H3-C(27)), 1.00 (s, 3H, H3-C(26)), 0.95 (s, 3H, H3-C(25)). 13C NMR (126 MHz, MeODd4) δ 221.02 (C3), 176.99 (d, 3J = 8.4 Hz, (C28)), 151.94 (C20), 110.22 (C29), 59.92 (d, 1J = 162.6 Hz, (C28’)), 57.99 (C17), 56.11 (C5), 51.23 (C9), 50.68 (C18), 48.31 (C19), 43.61 (C14), 41.87 (C8), 40.70 (C4), 39.60 (C11), 38.06 (C13), 37.79 (C10), 35.05 (C21), 34.74 (C7), 34.72 (C16), 32.92 (C2), 31.61 (C22), 30.88 (C15), 27.17 (C23), 26.89 (C12), 22.62 (C11), 21.43 (C24), 20.76 (C6), 19.55 (C30), 16.54 (C26), 16.35 (C25), 15.03 (C27). 31P NMR (121 MHz, MeODd4) δ 14.20. HRMS: [C31H49O6P-H+] 547.3194; found 547.3198 (0.7 ppm). \(\:[{\alpha]}_{D}^{20}=\:+0.16\); \(\:[{\alpha]}_{546}^{20}=\:+0.19\); [\(\:[{\alpha]}_{436}^{20}=\:+0.38\); \(\:[{\alpha]}_{405}^{20}=\:+0.51\); \(\:[{\alpha]}_{365}^{20}=\:+0.80\) (c = 1.00, MeOH).
Sodium (3-oxo-(17R)-17-28-norolean-12(13)-en)-2-oxoethyl-phosphonate 7b
1H NMR (500 MHz, MeODd4) δ 5.30 (d, 3J = 3.7 Hz, 1H, H-C(13)), 4.21–4.09 (m, 2H, H2-C(28’)), 2.92 (dd, 3J = 14.1, 4.5 Hz, 1H, H-C(18)), 2.57 (ddd, 2J = 16.1 Hz, 3J = 10.8, 7.4 Hz, 1H, Ha-C(2)), 2.37 (ddd, 2J = 16.1 Hz, 3J = 7.1, 3.6 Hz, 1H, Hb-C(2)), 2.09–1.86 (m, 4 H, Ha-C(16), H2-C(11), Ha-C(1)), 1.84–1.60 (m, 6 H, Hb-C(16), Ha-C(15), H2-C(22), Ha-C(19), H-C(9)), 1.59–1.32 (m, 7 H, H2-C(6), H2-C(7), Ha-C(21), Hb-C(1), H-C(5)), 1.21 (d, 2J = 13.2 Hz, 1H, Hb-C(21)), 1.18 (s, 3H, H3-C(27)), 1.16–1.09 (m, 2H, Hb-C(15), Hb-C(19)), 1.08 (s, 6 H, H3-C(23), H3-C(25)), 1.05 (s, 3H, H3-C(24)), 0.95 (s, 3H, H3-C(29)), 0.91 (s, 3H, H3-C(30)), 0.83 (s, 3H, H3-C(25)). 13C NMR (126 MHz, MeODd4) δ 220.52 (C3), 180.23 (d, 3J = 9.0 Hz, (C28)), 145.38 (C12), 123.35 (C13), 60.43 (d, 1J = 162.8 Hz, (C28’)), 56.60 (C5), 48.83 (C4), 48.53 (C17), 48.26 (C9), 47.32 (C19), 42.98 (C14), 42.93 (C18), 40.56 (C8), 40.27 (C1), 37.92 (C10), 35.11 (C2), 35.00 (C21), 33.64 (C30), 33.38 (C7), 33.10 (C22), 31.58 (C20), 29.14 (C15), 26.96 (C23), 26.30 (C27), 24.59 (C11), 24.15 (C29), 23.78 (C16), 21.90 (C24), 20.73 (C6), 17.54 (C26), 15.53 (C25). 31P NMR (121 MHz, MeODd4) δ 11.54. HRMS: [C31H49O6P-H+] 547.3194; found 547.3194 (0 ppm). \(\:[{\alpha]}_{D}^{20}=\:+0.47\); \(\:[{\alpha]}_{546}^{20}=\:+0.56\); [\(\:[{\alpha]}_{436}^{20}=\:+0.98\); \(\:[{\alpha]}_{405}^{20}=\:+1.22\); \(\:[{\alpha]}_{365}^{20}=\:+1.65\) (c = 1.00, MeOH).
Sodium (3-oxo-(17R)-17-28-norurs-12(13)-en)-2-oxoethyl-phosphonate 7c
1H NMR (500 MHz, MeODd4) δ 5.30 (d, 3J = 3.7 Hz, 1H, H-C(12)), 4.08 (d, 2J = 13.2 Hz, 1H, Ha-C(28’)), 4.00 (d, 2J = 13.2 Hz, 1H, Hb-C(28’)), 2.57 (ddd, 2J = 16.0 Hz, 3J = 10.7, 7.4 Hz, 1H, Ha-C(2)), 2.39 (ddd, 2J = 16.0 Hz, 3J = 7.1, 3.7 Hz, 1H, Hb-C(2)), 2.32 (d, 3J = 11,3 Hz, 1H, H-C(18)), 2.10–1.90 (m, 5 H, H2-C(11), Ha-C(16), Ha-C(15), Ha-C(1)), 1.90–1.81 (m, 2H, Hb-C(16), Ha-C(21)), 1.72 (dt, 2J = 13.8 Hz, 3J = 4.0 Hz, 1H, Hb-C(21)), 1.67 (dd, 3J = 11.0, 5.7 Hz, 1H, H-C(9)), 1.62–1.44 (m, 5 H, H2-C(6), Ha-C(22), Ha-C(7), Hb-C(1)), 1.44–1.28 (m, 4 H, Hb-C(22), Hb-C(7), H-C(5), H-C(19)), 1.12 (s, 3H, H3-C(27)), 1.12–1.08 (m, 1H, Hb-C(15)), 1.08 (s, 6 H, H3-C(23), H3-C(25)), 1.05 (s, 3H, H3-C(24)), 1.03–0.99 (m, 1H, H-C(20)), 0.95 (d, 3J = 6.2 Hz, 3H, H3-C(30)), 0.89 (d, 3J = 6.4 Hz, 3H, H3-C(29)), 0.86 (s, 3H, H3-C(26)). 13C NMR (126 MHz, MeODd4) δ 220.64 (C3), 179.92 (d, 3J = 8.8 Hz, (C28)), 139.68 (C13), 126.80 (C12), 62.93 (d, 1J = 153.5 Hz, (C28’)), 56.50 (C5), 54.32 (C18), 49.49 (C17), 48.15 (C9), 43.30 (C14), 40.80 (C8), 40.46 (C19), 40.41 (C1), 40.23 (C20), 37.82 (C10), 37.44 (C21), 35.14 (C7), 33.68 (C2), 31.84 (C22), 29.39 (C15), 27.07 (C23), 25.07 (C16), 24.51 (C11), 24.07 (C27), 21.92 (C24), 21.60 (C30), 20.72 (C6), 17.67 (C29), 17.63 (C26), 15.72 (C25). 31P NMR (121 MHz, MeODd4) δ 11.53. HRMS: [C31H49O6P-H+] 547.3194; found 547.3195 (0.2 ppm). \(\:[{\alpha]}_{D}^{20}=\:+0.49\); \(\:[{\alpha]}_{546}^{20}=\:+0.58\); [\(\:[{\alpha]}_{436}^{20}=\:+0.97\); \(\:[{\alpha]}_{405}^{20}=\:+1.23\); \(\:[{\alpha]}_{365}^{20}=\:+1.62\) (c = 1.00, MeOH).
Sodium (3β-hydroxy-(17R)-17-28-norlup-20(29)-en)-2-oxoethyl-phosphonate 8a
1H NMR (500 MHz, MeODd4) δ 4.62 (s, 1H, Ha-C(29)), 4.48 (s, 1H, Hb-C(29)), 4.08 (dd, 2J = 13.5, 8.9 Hz, 1H, Ha-C(28’)), 3.95 (dd, 2J = 13.5, 8.9 Hz, 1H, Hb-C(28’)), 3.02 (dd, 3J = 11.4, 4.6 Hz, 1H, H-C(3)), 2.93 (td, 3J = 11.3, 4.5 Hz, 1H, H-C(19)), 2.32 (d, 2J = 12.3 Hz, 1H, Ha-C(16)), 2.27–2.19 (m, 1H, H-C(13)), 1.99 (dd, 2J = 12.1 Hz, 3J = 8.1 Hz, 1H, Ha-C(21)), 1.88–1.80 (m, 1H, Ha-C(22)), 1.66–1.57 (m, 1H, Ha-C(12)), 1.59 (s, 3H, H3-C(30)), 1.57–1.11 (m, 15 H, H2-C(6), H2-C(11), H2-C(7), H2-C(2), Hb-C(22), Hb-C(21), Hb-C(16), Ha-C(1), H-C(9), H-C(18), Ha-C(15)), 1.11–0.91 (m, 2H, Hb-C(15), Hb-C(12)), 0.89 (s, 3H, H3-C(27)), 0.87–0.82 (m, 7 H, H3-C(23), H-C(1), H3-C(26)), 0.76 (s, 3H, H3-C(25)), 0.65 (s, 3H, H3-C(24)), 0.63–0.57 (m, 1H, H-C(5)). 13C NMR (126 MHz, MeODd4) δ 177.50 (d, 3J = 8.8 Hz, (C28)), 152.07 (C20), 110.11 (C29), 79.69 (C3), 61,13 (d, 1J = 159.5 Hz, (C28’)), 57.95 (C17), 56.90 (C5), 52.05 (C9), 50.81 (C18), 48.32 (C19), 43.52 (C14), 41.95 (C8), 40.11 (C4), 39.96 (C1), 39.42 (C13), 38.33 (C10), 37.83 (C21), 35.55 (C7), 32.99 (C16), 31.67 (C22), 30.95 (C15), 28.61 (C23), 28.05 (C2), 26.90 (C12), 22.08 (C11), 19.57 (C30), 19.45 (C6), 16.74 (C25), 16.62 (C26), 16.11 (C24), 15.11 (C27). 31P NMR (121 MHz, MeODd4) δ 11.47. HRMS: [C31H51O6P-H+] 549.3350; found 549.3351 (0.2 ppm). \(\:[{\alpha]}_{D}^{20}=\:-0.07\); \(\:[{\alpha]}_{546}^{20}=\:-0.08\); [\(\:[{\alpha]}_{436}^{20}=\:-0.10\); \(\:[{\alpha]}_{405}^{20}=\:-0.10\); \(\:[{\alpha]}_{365}^{20}=\:-0.11\) (c = 1.00, MeOH).
Sodium (3β-hydroxy-(17R)-17-28-norurs-12(13)-en)-2-oxoethyl-phosphonate 8b
1H NMR (500 MHz, MeODd4) δ 5.27 (d, 3J = 3.9 Hz, 1H, H-C(13)), 4.06 (dd, 2J = 10.3, 5.1 Hz, 1H, Ha-C(28’)), 4.02 (dd, 2J = 10.3, 5.1 Hz, 1H, Hb-C(28’)), 3.15 (dd, 3J = 11.4, 4.6 Hz, 1H, H, H-C(3)), 2.31 (d, 3J = 11.3 Hz, 1H, H-C(18)), 2.04 (td, 2J = 13.3 Hz, 3J = 4.3 Hz, 1H, Ha-C(16)), 1.96–1.85 (m, 3H, H2-C(11), Ha-C(15)), 1.84–1.73 (m, 2H, Hb-C(16), Ha-C(21)), 1.73–1.61 (m, 3H, Ha-C(2), Hb-C(21), Ha-C(1)), 1.61–1.46 (m, 5 H, Ha-C(6), Hb-C(2), Ha-C(22), Ha-C(7), H-C(9)), 1.45–1.26 (m, 4 H, Hb-C(6), Hb-C(22), Hb-C(7), H-C(19)), 1.11 (s, 3H, H3-C(27)), 1.07 (d, 2J = 13.4 Hz, 1H, Hb-C(15)), 1.04–0.98 (m, 2H, H-C(20), Hb-C(1)), 0.97 (s, 3H, H3-C(23)), 0.96 (d, 3J = 6.3 Hz, 3H, H3-C(30)), 0.95 (s, 3H, H3-C(25)), 0.89 (d, 3J = 6.4 Hz, 3H, H3-C(25)), 0.79 (s, 3H, H3-C(24)), 0.78 (s, 3H, H3-C(26)), 0.74 (d, 3J = 11.4 Hz, 1H, H-C(5)). 13C NMR (126 MHz, MeODd4) δ 179.47 (d, 3J = 9.2 Hz, C(28)), 139.44 (C13), 127.13 (C12), 79.72 (C3), 61.63 (d, 1J = 158.8 Hz, C(28’)), 56.75 (C5), 54.19 (C18), 49.49 (C17), 49.03 (C9), 43.12 (C14), 40.83 (C8), 40.39 (C19), 40.21 (C20), 40.01 (C1), 39.84 (C4), 38.09 (C10), 37.51 (C21), 34.20 (C7), 31.77 (C22), 29.29 (C15), 28.76 (C23), 27.90 (C2), 25.09 (C16), 24.36 (C11), 24.18 (C27), 21.59 (C30), 19.47 (C6), 17.70 (C24), 17.62 (C29), 16.37 (C26), 16.03 (C25). 31P NMR (121 MHz, MeODd4) δ 12.17. HRMS: [C31H51O6P-H+] 549.3350; found 549.3349 (0.2 ppm). \(\:[{\alpha]}_{D}^{20}=\:+0.33\); \(\:[{\alpha]}_{546}^{20}=\:+0.40\); [\(\:[{\alpha]}_{436}^{20}=\:+0.71\); \(\:[{\alpha]}_{405}^{20}=\:+0.88\); \(\:[{\alpha]}_{365}^{20}=\:+1.12\) (c = 1.00, MeOH).
Sodium (3β-hydroxy-(17R)-17-28-norolean-12(13)-en)-2-oxoethyl-phosphonate 8c
1H NMR (500 MHz, MeODd4) δ 5.25 (t, 3J = 3.6 Hz, 1H, H-C(13)), 4.16 (dd, 2J = 13.2, 8.8 Hz, 1H, Ha-C(28’)), 3.96 (dd, 2J = 13.3, 8.6 Hz, 1H, Hb-C(28’)), 3.14 (dd, 3J = 11.4, 4.5 Hz, 1H, C(3)), 2.88 (dd, 3J = 14.2, 4.4 Hz, 1H, H-C(18)), 1.99 (dt, 2J = 13.8 Hz, 3J = 7,7 Hz, 1H, Ha-C(16)), 1.96–1.79 (m, 3H, Hb-C(16), H-C(11)), 1.79–1.27 (m, 13H, H2-C(6), H2-C(2), Ha-C(15), H2-C(22), H2-C(7), Ha-C(21), Ha-C(1), Ha-C(19), H-C(9)), 1.19 (d, 2J = 14.9 Hz, 1H, Hb-C(21)), 1.15 (s, 3H, H3-C(27)), 1.13–1.00 (m, 2H, Hb-C(19), Hb-C(15)), 1.00–0.95 (m, 4 H, H3-C(23), Hb-C(1)), 0.94 (s, 6 H, H3-C(29), H3-C(25)), 0.90 (s, 3H, H3-C(30)), 0.78 (s, 6 H, H3-C(26), H3-C(24)), 0.77–0.72 (m, 1H, H-C(5)). 13C NMR (126 MHz, MeODd4) δ 180.03 (d, 3J = 8.9 Hz, C(C28)), 145.27 (C12), 123.59 (C13), 79.77 (C3), 62.76 (d, 1J = 154.7 Hz, (C28’)), 56.80 (C5), 49.17 (C9), 48.11 (C17), 47.34 (C19), 42.85 (C18), 40.60 (C14), 39.88 (C8), 39.85 (C1), 38.17 (C4), 38.17 (C10), 34.99 (C21), 33.94 (C7), 33.64 (C30), 33.17 (C22), 31.58 (C20), 29.11 (C15), 28.74 (C23), 27.88 (C2), 26.41 (C27), 24.53 (C11), 24.16 (C29), 23.80 (C16), 19.50 (C6), 17.67 (C26), 16.30 (C24), 15.91 (C25). 31P NMR (121 MHz, MeODd4) δ 11.59. HRMS: [C31H51O6P-H+] 549.3350; found 549.3348 (0.4 ppm). \(\:[{\alpha]}_{D}^{20}=\:+0.31\); \(\:[{\alpha]}_{546}^{20}=\:+0.43\); [\(\:[{\alpha]}_{436}^{20}=\:+0.76\); \(\:[{\alpha]}_{405}^{20}=\:+0.91\); \(\:[{\alpha]}_{365}^{20}=\:+1.21\) (c = 1.00, MeOH).
Synthesis of a mixture of products 9, 10 and 11
To solution of betulin (1a) (500 mg, 1.131 mmol, 1 eq.) in anhydrous THF (5mL) freshly prepared 1 M LDA solution in THF (2.37 mL, 2.37 mmol, 2.1 eq.) is added dropwise at -78 °C. The resulting reaction mixture is warmed up to 0 °C and stirred at ambient temperature for 40 min. Then the solution of previously prepared (dimethoxyphosphoryl)methyl trifluoromethanesulfonate (712 mg, 2.49 mmol, 2.2 eq.) in anhydrous THF (3 mL) is added dropwise to the suspension of lithium alkoxide at 0 °C. The obtained reaction mixture is warmed up to room temperature and stirred for 3 h. Then the reaction mixture is quenched by MeOH (2 mL ), evaporated to dryness, redissolved in EtOAc (50 mL) and subsequently washed with H2O (30 mL) and brine (2 × 30 mL). The combined organic layer is dried over anhydrous Na2SO4. After filtration, the filtrate is concentrated in vacuo and purified by silica column chromatography (Hexanes-EtOAc 4:1–1:9) to yield bis-ether 9 as a white amorphous solid (29%, 226 mg). Rf = 0.31 (100% EtOAc). Side product 11 was isolated with preparative HPLC on C18 reverse phase column by gradient A/B (60/40) → A/B 0/100)*. However, the presence of monoester 10 was detected by HPLC and NMR, yet the product 10 was not isolated in pure form.
* A: 95 parts of 0.1% aqueous solution of trifluoroacetic acid and 5 parts of acetonitrile;
B: acetonitrile.
(3 S)-3,28-di((dimethoxyphosphoryl)methyloxy)-lup-20(29)ene 9
1H NMR (500 MHz, CDCl3) δ 4.67 (s, 1H, Ha-C(29)), 4.57 (s, 1H, Hb-C(29)), 3.99 (dd, 2J = 13.6 Hz, 3J = 8.7 Hz, 1H, Ha-C(28’)), 3.87–3.76 (m, 14 H, H2-C(3’), (H3-CO)4), 3.70 (d, 2J = 8.7 Hz, 1H, Ha-C(28)), 3.68 (dd, 2J = 13.6 Hz, 3J = 9.7 Hz, 1H, Hb-C(28’)), 3.24 (d, 2J = 8.7 Hz, 1H, Hb-C(28)), 2.83 (dd, 3J = 11.8, 4.3 Hz, 1H, H-C(3)), 2.38 (td, 3J = 10.8, 5.5 Hz, 1H, H-C(19)), 2.01–1.86 (m, 3H, Ha-C(16), Ha-C(21), Ha-C(22)), 1.78–1.68 (m, 3H, Ha-C(1), Ha-C(15), Ha-C(2)), 1.67 (s, 3H, H3-C(30)), 1.65–1.57 (m, 2H, Ha-C(12), H-C(13)), 1.56–1.43 (m, 3H, Ha-C(6), Hb-C(2), H-C(18)), 1.43–1.33 (m, 5 H, Ha-C(11), Hb-C(6), Hb-C(16), H2-C(7)), 1.28–1.13 (m, 3H, Hb-C(11), Hb-C(22), H-C(9)), 1.08–0.99 (m, 6 H, H3-C(26), Hb-C(12), Hb-C(15), Hb-C(21)), 0.98 (s, 3H, H3-C(23)), 0.95 (s, 3H, H3-C(27)), 0.85–0.78 (m, 4 H, H3-C(25)), 0.76 (s, 3H, H3-C(26)), 0.67 (d, 3J = 9.5 Hz, 1H, H-C(5)). 13C NMR (126 MHz, CDCl3) δ 150.61 (C20), 109.82 (C29), 90.08 (d, 3J = 12.2 Hz, (C3)), 72.41 (d, 3J = 9.5 Hz (C28)), 65.40 (d, 1J = 164.5 Hz, (C3’)), 63.18 (d, 1J = 166.5 Hz, (C28’)), 55.81 (C5), 53.29 (d, 2J = 6.6 Hz, (MeO)) 53.14 (d, 2J = 6.8 Hz, (MeO)), 53.12 (d, 2J = 6.5 Hz, (MeO)), 53.09 (d, 2J = 6.9 Hz, (MeO)), 50.46 (C9), 48.98 (C18), 48.03 (C19), 47.56 (C17), 42.81 (C14), 41.06 (C8), 39.10 (C4), 38.52 (C1), 37.66 (C13), 37.26 (C10), 34.65 (C21), 34.31 (C7), 29.96 (C22), 29.86 (C16), 28.15 (C23), 27.20 (C15), 25.30 (C12), 22.35 (C2), 20.97 (C11), 19.25 (C30), 18.27 (C6), 16.25 (C24), 16.20 (C25), 16.10 (C26), 14.89 (C27). 31P NMR (121 MHz, CDCl3) δ 23.96, 23.73. HRMS: [C36H64O8P2 + H+] 687.4149; found 687.4141 (1.1 ppm). \(\:[{\alpha]}_{D}^{20}=\:+0.21\); \(\:[{\alpha]}_{546}^{20}=\:+0.26\); [\(\:[{\alpha]}_{436}^{20}=\:+0.47\); \(\:[{\alpha]}_{405}^{20}=\:+0.57\); \(\:[{\alpha]}_{365}^{20}=\:+0.74\) (c = 1.00, MeOH).
(((3 S)-3-((dimethoxyphosphoryl)methyloxy)-28-lup-20(29)enyloxy)(methoxy)phosphoryl)methyl trifluoromethanesulfonate 11
1H NMR (500 MHz, CDCl3) δ 4.68 (s, 1H, Ha-C(29)), 4.59 (s, 1H, Hb-C(29)), 4.27 (dd, 2J = 9.3 Hz, 3J = 5.2 Hz, 1H, Ha-C(28)), 4.00 (dd, 2J = 13.7 Hz, 3J = 8.8 Hz, 1H, H-C(3)), 3.88–3.78 (m, 9H, (H3-COP)2, H2-C(28’), Hb-C(28)), 3.70 (dd, 2J = 13.7 Hz, 3J = 9.7 Hz, 1H, H-C(3’)), 3.47 (m, 3H, OMe), 2.83 (dd, 3J = 11.8, 4.3 Hz, 1H, H-C(3)), 2.38 (ddd, 3J = 10.6, 10.1, 5.6 Hz, 1H, H-C(19)), 2.01–1.86 (m, 3H, Ha-C(16), Ha-C(21), Ha-C(22)), 1.80–1.69 (m, 3H, Ha-C(2), Ha-C(15), Ha-C(1)), 1.66 (s, 3H, H3-C(30)), 1.66–1.57 (m, 3H, Ha-C(12), H-C(13), H-C(18)), 1.57–1.32 (m, 7 H, H2-C(6), Ha-C(11), Hb-C(2), Hb-C(22), H-C(7)), 1.32–1.13 (m, 3H, Hb-C(11), Hb-C(16)), 1.13–1.03 (m, 3H, Hb-C(12), Hb-C(15), Hb-C(22)), 1.02 (s, 3H, H3-C(26)), 0.98 (s, 3H, H3-C(23)), 0.96 (s, 3H, H3-C(27)), 0.82 (s, 3H, H3-C(25)), 0.82–0.75 (m, 1H, Hb-C(1)), 0.75 (s, 3H, H3-C(24)), 0.67 (d, 3J = 9.6 Hz, 1H, H-C(5)). 13C NMR (126 MHz, CDCl3) δ 150.13 (C20), 110.09 (C29), 90.11 (d, 3J = 12.4 Hz, (H-C(3)), 66.33 (d, 1J = 166.44, H-C(3’)), 65.34 (d,2J = 7.6 Hz, C(28)), 63.10 (d, 1J = 167.3 Hz, H-C(28’)), 61.56 (d, 2J = 13.1 Hz, MeO-P(H2C(28))), 55.81 (C5), 53.40 (d, 2J = 6.5 Hz, (MeO)), 53.37 (d, 2J = 6.6 Hz, (MeO)), 50.44 (C9), 48.76 (C18), 47.82 (C19), 47.37 (d, 3J = 6.6 Hz, (C17)), 42.84 (C14), 41.04 (C8), 39.10 (C4), 38.52 (C1), 37.75 (C13), 37.26 (C10), 34.27 (C21), 34.20 (C7), 29.59 (C22), 29.30 (C16), 28.13 (C23), 26.95 (C15), 25.30 (C12), 22.33 (C2), 20.94 (C11), 19.24 (C30), 18.25 (C6), 16.23 (C24), 16.19 (C25), 16.08 (C26), 14.87 (C27). 31P NMR (121 MHz, CDCl3) δ 24.02, 22.69. Rf = 0.43 (100% EtOAc).
Sodium (lup-20(29)-en-(3 S)-3,28-diylbis(oxymethylene))bis(phosphonate) 12, demethylation process 9 → 12
To a solution of compound 9 (275 mg, 0.4 mmol, 1 eq.) in anhydrous DCM (5 mL) TMSI (342 µL 2.4 mmol, 6 eq.) is added dropwise at -40 °C and the resulting reaction mixture is stirred at -40 °C for 5 h. Then MeOH (2 mL) is added dropwise at -40 °C. The obtained reaction mixture is stirred for additional 30 min and solution of NaHCO3 (202 mg, 2.4 mmol, 6 eq.) in H2O (6 mL) is added dropwise at -40 °C, and the resulting mixture is warmed up to room temperature. The resulting reaction mixture is warmed up to room temperature and the organic solvents are evaporated in vacuo. The obtained aqueous suspension is centrifuged and the supernatant is removed and discarded. The precipitate is re-suspended in deionized water (1 mL) and the centrifugation – supernatant removal procedure is repeated additional two times (in total: washing with water 3 × 1mL). The obtained precipitate is then dried in vacuo to yield product 12 as a yellowish amorphous solid (78%, 225 mg).
1H NMR (500 MHz, MeOD) δ 4.69 (s, 1H, Ha-C(29)), 4.57 (s, 1H, Hb-C(29)), 3.85 (dd, 2J = 13.3, 9.1 Hz, 1H, Ha-C(28’), 3.74–3.68 (m, 3H, Ha-C(28), H2-C(3’)), 3.55 (dd, 2J = 13.3, 10.2 Hz, 1H, Hb-C(28’)), 3.32(d, 2J = 11.4 Hz, 1H, Hb-C(28)), 2.89 (dd, 3J = 11.7, 4.3 Hz, 1H, H-C(3)), 2.46 (td, 3J = 11.0, 5.9 Hz, 1H, H-C(19)), 2.08–1.98 (m, 3H, H, Ha-C(16), Ha-C(21), Ha-C(22)), 1.90–1.70 (m, 5 H, Ha-C(15), Ha-C(1), H-C(13), Ha-C(12), Ha-C(2)), 1.69 (s, 3H, H3-C(30)), 1.62–1.39 (m, 7 H, H2-C(6), Ha-C(11), Hb-C(2), H-C(18), H2-C(7)), 1.39–1.10 (m, 4 H, Hb-C(11), Hb-C(22), Hb-C(16), H-C(9)), 1.09 (s, 3H, H3-C(26)), 1.09–1.03 (m, 1H, Hb-C(12)), 1.03 (s, 3H, H3-C(23)), 1.02–0.95 (m, 5 H, H3-C(27), Hb-C(21), Hb-C(15)), 0.95–0.89 (m, 1H, Hb-C(1)), 0.88 (s, 3H, H3-C(25)), 0.80 (s, 3H, H3-C(24)), 0.74 (d, 3J = 9.6 Hz, 1H, H-C(5)). 13C NMR (126 MHz, MeOD) δ 150.51 (C20), 108.83 (C10), 89.45 (d,3J = 12.1 Hz, C(3)), 71.56 (d, 3J = 10.6 Hz, (C28)), 66.93 (d, 1J = 162.8 Hz, (C3’)), 64.67 (d, 1J = 164.8 Hz, C(28’)), 55.77 (C5), 50.41 (C9), 48.79 (C18), 48.01 (C19), 42.40 (C14), 40.77 (C8), 38.69 (C1), 38.33 (C4), 37.51 (C13), 36.90 (C10), 34.30 (C21), 34.05 (C7), 29.58 (C22), 29.49 (C16), 27.19 (C23), 26.97 (C15), 25.20 (C12), 21.92 (C2), 20.60 (C11), 17.98 (C30), 17.89 (C6), 15.34 (C25), 15.32 (C24), 15.22 (C26), 13.85 (C27). 31P NMR (121 MHz, MeOD) δ 19.72, 19.07. \(\:[{\alpha]}_{D}^{20}=\:+0.11\); \(\:[{\alpha]}_{546}^{20}=\:+0.17\); [\(\:[{\alpha]}_{436}^{20}=\:+0.33\); \(\:[{\alpha]}_{405}^{20}=\:+0.37\); \(\:[{\alpha]}_{365}^{20}=\:+0.46\) (c = 1.00, MeOH).
Cytotoxicity evaluation
Cytotoxicity of betulinic acid, ursolic acid and oleanolic acid derivatives was evaluated using human-derived osteosarcoma cell line MG63 (ATCC, CRL-1427) and mouse-derived preosteoblast cell line MC3T3-E1 (ATCC CRL-2593). Before conducting the experiments, both cell lines were continuously cultured according to the ATCC product sheet instructions. Briefly, both cell lines were expanded in α-MEM medium supplemented with 10% FBS and 1% pen-strep and maintained at 37 °C in a humidified atmosphere with 5% CO2.
Each cell line was plated at a concentration of 1 × 104 cells/well in 96-well plate. The plates were incubated for 24 h to allow cell attachment and growth. Bioactive substances were solubilized in methanol prior further dilution in cell culture media. Following the cell incubation period, the culture media was removed and the dilutions of active substance (10, 25 and 50 µM) in cell culture media were added. The culture medium only and its dilutions with methanol solution respective to the bioactive substance concentrations were used as the controls. The final concentration of methanol did not exceed 1%. Cells were treated with bioactive substance solutions for 24 h. After 24 h incubation, relative cell metabolic activity was assessed using CellTiter-Blue® (CTB) analysis (Promega, JAV). Absorbance was measured at 590 nm using microplate reader (Infinite® 200 PRO, Tecan, USA). The relative cell metabolic activity was calculated for each bioactive substance concentration as well as for the controls. All results were presented as the mean ± standard deviation of at least 5 replicates. Statistically significant differences between sample groups are assessed using a one-way ANOVA test and then corrected using the Šídák multiple comparison test. Statistically significant differences were considered to be those with a P-values less than 0.05 (p < 0.05). Numerical values of the cell relative metabolic activity are summarized in Table 4 and the corresponding graphical representation can be found in supporting information (Figures S1-S4).
Data availability
All data generated or analysed during this study are included in this published article (and its Supplementary Information files).
References
Newman, D. J. & Cragg, G. M. Natural products as sources of New drugs over the nearly four decades from 01/1981 to 09/2019. J. Nat. Prod. 83, 770–803. https://doi.org/10.1021/acs.jnatprod.9b01285 (2020).
Safarzadeh, E., Shotorbani, S. S. & Baradaran, B. Herbal Medicine as inducers of apoptosis in Cancer Treatment. Adv. Pharm. Bull. 4, 421–427. https://doi.org/10.5681/apb.2014.062 (2014).
Pezzuto, J. M. Plant-derived anticancer agents. Biochem. Pharmacol. 53, 121–133. https://doi.org/10.1016/s0006-2952(96)00654-5 (1997).
Ghante, M. H. & Jamkhande, P. G. Role of Pentacyclic triterpenoids in Chemoprevention and Anticancer Treatment: an overview on targets and underling mechanisms. J. Pharmacopunct. 22, 55–67. https://doi.org/10.3831/KPI.201.22.007 (2019).
Xiao, S. et al. Synthesis and anti-HCV entry activity studies of beta-cyclodextrin-pentacyclic triterpene conjugates. ChemMedChem. 9, 1060–1070. https://doi.org/10.1002/cmdc.201300545 (2014).
Sathya, S., Sudhagar, S., Sarathkumar, B. & Lakshmi, B. S. EGFR inhibition by pentacyclic triterpenes exhibit cell cycle and growth arrest in breast cancer cells. Life Sci. 95, 53–62. https://doi.org/10.1016/j.lfs.2013.11.019 (2014).
Safayhi, H. & Sailer, E. R. Anti-inflammatory actions of pentacyclic triterpenes. Planta Med. 64, 487–493. https://doi.org/10.1055/s-2006-957748 (1997).
Wu, P. et al. Synthesis and biological evaluation of pentacyclic triterpenoid derivatives as potential novel antibacterial agents. Bioorg. Chem. 109, 104692–104706. https://doi.org/10.1016/j.bioorg.2021.104692 (2021).
Jager, S., Trojan, H., Kopp, T., Laszczyk N, M. & Scheffler, A. Pentacyclic triterpene distribution in various plants—Rich sources for a new group of multi-potent plant extracts. Molecules. 14, 2016. https://doi.org/10.3390/molecules14062016 (2009).
Amiri, S. et al. Betulin and its derivatives as novel compounds with different pharmacological effects. Biotechnol. Adv. 38, 107409–107448. https://doi.org/10.1016/j.biotechadv.2019.06.008 (2009).
Lombrea, A. et al. Anticancer potential of Betulonic acid derivatives. Int. J. Mol. Sci. 22, 3676. https://doi.org/10.3390/ijms22073676 (2021).
Lombrea, A. et al. Comparison of in Vitro Antimelanoma and Antimicrobial Activity of 2,3-Indolo-betulinic acid and its Glycine conjugates. Plants. 12, 1253. https://doi.org/10.3390/plants12061253 (2023).
Popov, S. A. et al. Synthesis and cytotoxicity of hybrids of 1,3,4- or 1,2,5-oxadiazoles tethered from ursane and lupane core with 1,2,3-triazole. Steroids. 162, 108698. https://doi.org/10.1016/j.steroids.2020.108698.( (2020).
Wang, X. et al. Inhibitory effect of oleanolic acid on hepatocellular carcinoma via ERK-p53-mediated cell cycle arrest and mitochondrial-dependent apoptosis. Carcinogenesis. 34, 1323–1330. https://doi.org/10.1093/carcin/bgt058 (2013).
Lewinska, A., Adamczyk-Grochala, J., Kwasniewicz, E., Deregowska, A. & Wnuk, M. Ursolic acid-mediated changes in glycolytic pathway promote cytotoxic autophagy and apoptosis in phenotypically different breast cancer cells. Apoptosis. 22, 800–815. https://doi.org/10.1007/s10495-017-1353-7 (2017).
Similie, D. et al. An update on Pentacyclic triterpenoids Ursolic and oleanolic acids and related derivatives as Anticancer candidates. Antioxidants. 13, 952. https://doi.org/10.3390/antiox13080952 (2024).
Wang, C. M. et al. Antibacterial and synergistic activity of Pentacyclic triterpenoids isolated from Alstonia scholaris. Molecules. 21, 139. https://doi.org/10.3390/molecules21020139 (2016).
Shai, L. J., McGaw, L. J., Aderogba, M. A., Mdee, L. K. & Eloff, J. N. Four pentacyclic triterpenoids with antifungal and antibacterial activity from Curtisia dentata (Burm.f) C.A. Sm. Leaves. J. Ethnopharmacol. 119, 238–244. https://doi.org/10.1016/j.jep.2008.06.036 (2008).
Shu, C. et al. Antifungal efficacy of ursolic acid in control of Alternaria alternata causing black spot rot on apple fruit and possible mechanisms involved. Sci. Hortic. 256, 108636. https://doi.org/10.1016/j.scienta.2019.108636 (2019).
Oboh, M., Govender, L., Siwela, M. & Mkhwanazi, B. N. Anti-diabetic potential of plant-based Pentacyclic triterpene derivatives: Progress made to Improve Efficacy and Bioavailability. Molecules. 26, 7243. https://doi.org/10.3390/molecules26237243 (2021).
Roy, S. et al. Terpenoids as potential phytoconstituent in the treatment of diabetes: from preclinical to clinical advancement. Phytomedicine. 129, 155638. https://doi.org/10.1016/j.phymed.2024.155638 (2024).
Costa, J. F. O., Meira, C. S., Neves, Reis, M. V. G. & Soares, B. Anti-inflammatory activities of Betulinic Acid: a review. Front. Pharmacol. 13, 883857. https://doi.org/10.3389/fphar.2022.883857 (2022).
Jannus, F. et al. Efficient in Vitro and in vivo anti-inflammatory activity of a Diamine-PEGylated oleanolic Acid Derivative. Int. J. Mol. Sci. 22, 8158. https://doi.org/10.3390/ijms22158158 (2021).
Huang, L., Luo, S., Tong, S., Lv, Z. & Wu, J. The development of nanocarriers for natural products. Wiley Interdiscip. Rev.: Nanomed. Nanobiotechnol. 16, e (1967). https://doi.org/10.1002/wnan.1967. (2024).
Basu, A., Namporn, T. & Ruenraroengsak, P. Critical review in Designing Plant-based anticancer nanoparticles against Hepatocellular Carcinoma. Pharmaceutics. 15, 1611. https://doi.org/10.3390/pharmaceutics15061611 (2023).
Mierina, I., Vilskersts, R. & Turks, M. Delivery systems for Birch-bark triterpenoids and their derivatives in Anticancer Research. Curr. Med. Chem. 27, 1308–1336. https://doi.org/10.2174/0929867325666180530095657 (2020).
Jaroszewski, B., Jelonek, K. & Kasperczyk, J. Drug Delivery Systems of Betulin and Its Derivatives: An Overview. Biomedicines 12, 1168. (2024). https://doi.org/10.3390/biomedicines12061168
McClements, D. J. Advances in nanoparticle and microparticle delivery systems for increasing the dispersibility, stability, and bioactivity of phytochemicals. Biotechnol. Adv. 38, 107287. https://doi.org/10.1016/j.biotechadv.2018.08.004 (2020).
Liu, J. Oleanolic acid and ursolic acid: Research Perspectives. J. Ethnopharmacol. 100, 92–94. https://doi.org/10.1016/j.jep.2005.05.024 (2005).
Sousa, J. L. C., Freire, C. S. R., Silvestre, A. J. D. & Silva, A. M. S. Recent developments in the functionalization of Betulinic Acid and its natural analogues: a Route to New Bioactive compounds. Molecules. 24, 355. https://doi.org/10.3390/molecules24020355 (2019).
Jäger, S., Winkler, K., Pfüller, U. & Scheffler, A. Solubility studies of oleanolic acid and betulinic acid in aqueous solutions and plant extracts of Viscum album L. Planta Med. 73, 157–162. https://doi.org/10.1055/s-2007-967106 (2007).
Cerreia Vioglio, P., Chierotti, M. R. & Gobetto, R. Pharmaceutical aspects of salt and cocrystal forms of APIs and characterization challenges. Adv. Drug Deliv Rev. 117, 86–110. https://doi.org/10.1016/j.addr.2017.07.001 (2017).
Boryczka, S. et al. Synthesis, structure and cytotoxic activity of New Acetylenic derivatives of Betulin. Molecules. 18, 4526. https://doi.org/10.3390/molecules18044526 (2013).
Zhou, M., Zhang, R. H., Wang, M., Xu, G. B. & Liao, S. G. Prodrugs of triterpenoids and their derivatives. Eur. J. Med. Chem. 131, 222–236. https://doi.org/10.1016/j.ejmech.2017.03.005 (2017).
Salvador, J. A. R. et al. Oleanane-, ursane-, and quinone methide friedelane-type triterpenoid derivatives: recent advances in cancer treatment. Eur. J. Med. Chem. 142, 95–130. https://doi.org/10.1016/j.ejmech.2017.07.013 (2017).
Michaudel, Q. et al. Improving physical properties via C-H oxidation: Chemical and Enzymatic approaches. Angew Chem. 126https://doi.org/10.1002/ange.201407016 (2014). 12287 – 12292.
Berger, M., Knittl-Frank, C., Bauer, S., Winter, G. & Maulide, N. Application of Relay C – H oxidation logic to Polyhydroxylated Oleanane triterpenoids. Chem. 6, 1183–1189. https://doi.org/10.1016/j.chempr.2020.04.007 (2020).
Lugiņina, J. et al. Electrosynthesis of Stable Betulin-Derived Nitrile Oxides and their Application in Synthesis of Cytostatic Lupane-Type Triterpenoid-Isoxazole Conjugates. Eur. J. Org. Chem. 2557–2577. (2021). https://doi.org/10.1002/ejoc.202100293. (2021).
Serajuddin, A. T. M. Salt formation to improve drug solubility. Adv. Drug Delivery Rev. 59, 603–616. https://doi.org/10.1016/j.addr.2007.05.010 (2007).
Fan, J. et al. Synthesis and evaluation of the Cancer Cell Growth Inhibitory activity of the ionic derivatives of oleanolic acid and ursolic acid with improved solubility. J. Mol. Liq. 332, 115837–115848. https://doi.org/10.1016/j.molliq.2021.115837 (2021).
Bag, B. G. & Dash, S. S. Self-assembly of Sodium and Potassium betulinates into Hydro-and Organo-Gels: entrapment and removal studies of fluorophores and synthesis of gel-gold nanoparticle hybrid materials. RSC Adv. 6, 17290–17296. https://doi.org/10.1039/C5RA25167B (2016).
Wolfram, R. K., Heller, L. & Csuk, R. Targeting mitochondria: esters of rhodamine B with triterpenoids are mitocanic triggers of apoptosis. Eur. J. Med. Chem. 152, 21–30. https://doi.org/10.1016/j.ejmech.2018.04.031 (2018).
Wolfram, R. K. et al. Homo-piperazine-rhodamine B adducts of triterpenoic acids are strong mitocans. Eur. J. Med. Chem. 155, 869–879. https://doi.org/10.1016/j.ejmech.2018.06.051 (2018).
Spivak, A. Y. et al. Synthesis and evaluation of Anticancer activities of Novel C-28 Guanidine-Functionalized Triterpene acid derivatives. Molecules. 23, 3000. https://doi.org/10.3390/molecules23113000 (2018).
Dzhemileva, L. U., Tuktarova, R. A., Dzhemilev, U. M. & D’yakonov, V. A. Pentacyclic Triterpenoids-Based Ionic Compounds: Synthesis, Study of Structure-Antitumor Activity Relationship, Effects on Mitochondria and Activation of Signaling Pathways of Proliferation, Genome Reparation and Early Apoptosis. Cancers 15, 756. (2023). https://doi.org/10.3390/cancers15030756
Spivak, A. Y. et al. Synthesis of lupane triterpenoids with triphenylphosphonium substituents and studies of their antitumor activity. Russ Chem. Bull. 62, 188–198. https://doi.org/10.1007/s11172-013-0028-y (2013).
Spivak, A. Y. et al. Triphenylphosphonium cations of betulinic acid derivatives: synthesis and antitumor activity. Med. Chem. Res. 26, 518e531. https://doi.org/10.1007/s00044-016-1771-z (2017).
Levdanskii, V. A., Levdanskii, A. V. & Kuznetsov, B. N. Sulfation of Betulin by Sulfamic Acid in DMF and Dioxane, Chem. Nat. Compd. 50, 1029–1031. https://doi.org/10.1007/s10600-014-1152-0 (2014).
Bureeva, S. et al. Selective inhibition of the interaction of C1q with immunoglobulins and the classical pathway of complement activation by steroids and triterpenoids sulfates. Bioor Med. Chem. 15, 3489–3498. https://doi.org/10.1016/j.bmc.2007.03.002 (2007).
Kazachenko, A. S. et al. Catalytic Sulfation of Betulin with Sulfamic Acid: experiment and DFT calculation. Int. J. Mol. Sci. 23, 1602. https://doi.org/10.3390/ijms23031602 (2022).
Melnikova, N. B. et al. Betulin-3,28-diphosphate. Physico-Chemical properties and in Vitro Biological Activity experiments. Molecules. 23, 1175. https://doi.org/10.3390/molecules23051175 (2018).
Yu, Z. et al. Pharmacokinetics in Vitro and in vivo of two Novel prodrugs of oleanolic acid in rats and its Hepatoprotective effects against Liver Injury Induced by CCl4. Mol. Pharm. 13, 1699–1710. https://doi.org/10.1021/acs.molpharmaceut.6b00129 (2016).
Krasutsky, P. & Carlson, R. Triterpenes having antibacterial activity. World Patent Appl. WO0226762A1, April 4, 2002.
Krasutsky, P. & Carlson, R. Triterpenes having fungicidal activity against yeast. World Patent Appl. WO0226761A1, April 4, 2002.
Ochiai, M., Goto, K., Tokudome, Y. & Hirokawa, S. Novel triterpenic acid derivative and preparation for external application for skin comprising the same. World Patent Appl. WO2006132033A1, December 14, 2006.
Chrobak, E. et al. New phosphate derivatives of betulin as anticancer agents: synthesis, crystal structure, and molecular docking study. Bioorg. Chem. 87, 613–628. https://doi.org/10.1016/j.bioorg.2019.03.060 (2019).
Orchel, A. et al. Anticancer activity of the Acetylenic Derivative of Betulin Phosphate involves induction of necrotic-like death in breast Cancer cells in Vitro. Molecules. 26, 615. https://doi.org/10.3390/molecules26030615 (2021).
Chrobak, E. et al. Molecular structure, in Vitro Anticancer Study and Molecular Docking of New phosphate derivatives of Betulin. Molecules. 26, 737. https://doi.org/10.3390/molecules26030737 (2021).
Tubek, B., Smuga, D., Smuga, M. & Wawrzeńczyk, C. Synthesis of 28-O-(1,2- diacyl-sn-glycero-3-phospho)-betulin. Synth. Commun. 42, 3648–3654. https://doi.org/10.1080/00397911.2011.588817 (2012).
Petrova, A. V., Poptsov, A. I., Heise, N. V., Csuk, R. & Kazakova, O. B. Diethoxyphosphoryloxy-oleanolic acid is a nanomolar- inhibitor of butyrylcholinesterase. Chem. Biol. Drug Des. 103, e14506. https://doi.org/10.1111/cbdd.14506 (2024).
Mao, X. et al. Progress in phosphorylation of natural products. Mol. Biol. Rep. 51, 697. https://doi.org/10.1007/s11033-024-09596-1 (2024).
Hu, K. S., Darer, A. I. & Elrod, M. J. Thermodynamics and kinetics of the hydrolysis of atmospherically relevant organonitrates and organosulfates. Atmos. Chem. Phys. 11, 8307–8320. https://doi.org/10.5194/acp-11-8307-2011 (2011).
Aly, O. A. & Badawy, M. I. Hydrolysis of organophosphate insecticides in aqueous media. Environ. Int. 7, 373–377. https://doi.org/10.1016/0160-4120(82)90152-0 (1982).
Krečmerová, M., Majer, P., Rais, R. & Slusher, B. S. Phosphonates and phosphonate prodrugs in Medicinal Chemistry: past successes and future prospects. Front. Chem. 10, 889737. https://doi.org/10.3389/fchem.2022.889737 (2022).
Pertusat, F., Serpi, M. & McGuigan, C. Medicinal Chemistry of Nucleoside Phosphonate Prodrugs for antiviral therapy. Antiviral Chem. Chemother. 22, 181–203. https://doi.org/10.3851/IMP2012 (2012).
Pradere, U., Garnier-Amblard, E. C., Coats, S. J., Amblard, F. & Schinazi, R. F. Synthesis of nucleoside phosphate and phosphonate prodrugs. Chem. Rev. 114, 9154–9218. https://doi.org/10.1021/cr5002035 (2014).
Dang, Q. Organophosphonic acids as drug candidates. Expert Opin. Ther. Pat. 16, 343–348. https://doi.org/10.1517/13543776.16.3.343 (2006).
Deng, S. L. et al. Synthesis of Ursolic Phosphonate Derivatives as potential Anti-HIV agents. Phosphorus Sulfur Silicon Relat. Elem. 182, 951–967. https://doi.org/10.1080/10426500601088838 (2007).
Chrobak, E. et al. Betulin Phosphonates; synthesis, structure, and cytotoxic activity. Molecules. 21, 1123. https://doi.org/10.3390/molecules21091123 (2016).
Chodurek, E. et al. Antiproliferative and cytotoxic properties of Propynoyl Betulin derivatives against human ovarian Cancer cells: in Vitro studies. Int. J. Mol. Sci. 24, 16487. https://doi.org/10.3390/ijms242216487 (2023).
Tsepaeva, O. V., Nemtarev, A. V., Grigoreva, L. R. & Mironov, V. F. Synthesis of C(28)-linker derivatives of betulinic acid bearing phosphonate group. Russ Chem. Bull. 70, 179–182. https://doi.org/10.1007/s11172-021-3074-x (2021).
Meksuriyen, D., Nanayakkara, N. P. D., Phoebe, C. H. Jr. & Cordell, G. A. Two triterpenes from Davidsonia Pruriens. Phytochemistry. 25, 1685–1689. https://doi.org/10.1016/S0031-9422(00)81236-4 (1986).
Lee, E. H. et al. Inhibitory effect of Ursolic acid derivatives on recombinant human Aldose Reductase. Russ J. Bioorgan Chem. 37, 637–644. https://doi.org/10.1134/S1068162011050050 (2011).
Popov, S. A., Wang, C., Qi, Z., Shults, E. E. & Turks, M. Synthesis of water-soluble ester-linked ursolic acid–gallic acid hybrids with various hydrolytic stabilities. Synth. Commun. 51, 2466–2477. https://doi.org/10.1080/00397911.2021.1939057 (2021).
Flekhter, O. B. et al. Synthesis and antiviral activity of Betulonic Acid amides and conjugates with amino acids. Russ J. Bioorg. Chem. 30, 89–98. https://doi.org/10.1023/b:rubi.0000015778.77887.f1 (2004).
Yli-Kauhaluoma, J. et al. Betulin Derived Compounds Useful as Antiprotozoal Agents. World Patent Appl. WO2007141391A1, December 13, 2007.
Fu, L. & Gribble, G. W. Efficient and scalable synthesis of Bardoxolone Methyl (CDDO-methyl Ester). Org. Lett. 15, 1622–1625. https://doi.org/10.1021/ol400399x (2013).
Xu, Y. et al. Chemical Synthesis and Molecular Recognition of Phosphatase-Resistant Analogues of Phosphatidylinositol-3-phosphate. J. Am. Chem. Soc. 128, 885–897. https://doi.org/10.1021/ja0554716 (2006).
Dehaem, W., Mashentseva, A. A. & Seitembetov, T. S. Allobetulin and its derivatives: synthesis and Biological Activity. Molecules. 16, 2443–2466. https://doi.org/10.3390/molecules16032443 (2011).
Cruz-Cabeza, A. J. Acid-base crystalline complexes and the pka rule. CrystEngComm. 14, 6362–6365. https://doi.org/10.1039/C2CE26055G (2012).
Franz, R. G. Comparisons of pKa and log P values of some carboxylic and phosphonic acids: synthesis and measurement. AAPS PharmSci. 3, 1–13. https://doi.org/10.1208/ps030210 (2001).
Acknowledgements
The authors acknowledge financial support from the Ministry of Economics Republic of Latvia project “State research project in the field of biomedicine, medical technologies and pharmacy”, project No. VPP-EM-BIOMEDICINA-2022/1–0001 (BioMedPharm). D.L., A.D. and Ö.D. acknowledge the financial support, access to the infrastructure and expertise of the BBCE – Baltic Biomaterials Centre of Excellence (European Union’s Horizon 2020 research and innovation programme under the grant agreement No. 857287).
Author information
Authors and Affiliations
Contributions
Concept, study design, data analysis (J.L, M.T.). Manuscript preparation (V.K., A.D., M.T.) and revison (M.T., D.L.). Chemical synthesis and purification (J.L., V.K., R.L., E.F.). Solubility tests (V.K.). Cytotoxicity tests and evaluation (Ö.D., A.D., D.L.). NMR, quality control and characterization (V.K., J.L.). All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lugiņina, J., Kroškins, V., Lācis, R. et al. Synthesis and preliminary cytotoxicity evaluation of water soluble pentacyclic triterpenoid phosphonates. Sci Rep 14, 28031 (2024). https://doi.org/10.1038/s41598-024-76816-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-76816-w