Abstract
Microvascular complications, affecting small blood vessels, can lead to serious conditions such as kidney failure, painful nerve damage, and vision loss. Early detection and effective treatment of these issues are vital for improving patient outcomes and reducing healthcare expenses. Thus, this study aimed to assess diabetic microvascular complications among adults with type 2 diabetes in Adama, central Ethiopia. An institutional-based cross-sectional study was conducted among 381 adult type 2 diabetes patients. A computer-generated simple random sampling method was used to select study participants. Data were collected using a structured data extraction checklist. The collected data were entered into Epi info version 7.2 and exported to SPSS version 27 for processing and analysis. Binary logistic regression was employed to model the association between diabetic microvascular complications and explanatory variables. An adjusted odds ratio (AOR) with a 95% confidence interval (CI) was used to estimate the strength of association, and statistical significance was proclaimed at a p-value < 0.05. The prevalence of diabetic microvascular complications was 21.8% (95% CI: 17.8–25.6) with diabetic neuropathy being the most common (16.8%), followed by diabetic retinopathy (4.2%), and diabetic nephropathy (2.9%). Poor glycemic control (AOR = 2.00, 95% CI: 1.01–3.98), and a history of hypertension (AOR = 2.36, 95% CI: 1.39-4.00) were positively associated with the development of diabetic microvascular complications. Conversely, being aged 41–60 years (AOR = 0.35, 95% CI: 0.18–0.68) was negatively associated with the development of these complications. About one in five patients developed at least one diabetic microvascular complication. Age, poor glycemic control, and a history of hypertension were associated with the development of these complications. Therefore, intervening to improve glycemic control and manage hypertension is crucial in preventing the onset of diabetic microvascular complications.
Similar content being viewed by others
Introduction
Diabetes mellitus (DM) is a widely prevalent non-communicable disease characterized by hyperglycemia, affecting populations globally with increasing prevalence1,2. Type 2 diabetes mellitus (T2DM) is the most common subtype, distinguished from type 1 diabetes (T1DM) by factors such as age at onset, insulin resistance, and varying need for insulin therapy3,4. Projections indicate a significant rise in global diabetes cases, particularly in developing countries like those in Africa, where urbanization and lifestyle changes contribute to its occurrence5,6. By 2030, the World Health Organization (WHO) estimates more than half a million people will have diabetes worldwide, with substantial implications for public health and national economies, particularly in low-resource settings7,8,9.
T2DM is linked with disabling and potentially fatal microvascular and macrovascular complications10,11. Microvascular complications, which affect small blood vessels, are major contributors to end-stage renal disease, various painful neuropathies, and blindness12. Due to genetic predisposition and chronic hyperglycemia, the microvasculature in diabetics is particularly vulnerable to damage in vital organs such as the kidneys, eyes, and nervous system. Diabetic nephropathy is the most common cause of severe renal disease, diabetic retinopathy is a leading cause of blindness in the diabetic population, and diabetic neuropathy is the primary contributing factor to diabetic foot ulcers and amputations13,14.
The prevalence of microvascular complications ranged from 18.0 to 57.5% in Asia15,16, from 34.3 to 48.4% in the Middle East17,18,19, Ghana 35.3%20and 47.8% in Nigeria21. The increase in the prevalence of DM and its complications has also been noted in Ethiopia, with the prevalence of diabetic complications ranging from 20.4–61%22,23,24,25,26. The lowest reported rate of microvascular complications of T2DM was from Gondar25while the highest rate was reported from the Gurage Zone at 61%23.
Previous studies have shown that factors like age, sex, duration of diabetes, history of hypertension, triglycerides, hypercholesterolemia, dyslipidemia, poor glycemic control, physical inactivity, and positive proteinuria all influence the development of diabetic microvascular complications in T2DM patients14,27,28,29,30,31,32.
Early detection and effective treatment of diabetic microvascular complications are critical for improving patient outcomes and reducing healthcare costs33,34,35. These complications significantly impact morbidity and mortality associated with diabetes globally, placing substantial economic burdens on healthcare systems36,37. Timely interventions not only prolong life expectancy and enhance quality of life but also mitigate the need for costly treatments and hospitalizations. However, there is a dearth of evidence particularly within the study area, to demonstrate the prevalence and factors associated with diabetic microvascular complications. Our study aimed to provide insights into diabetic microvascular complications within our local context, aiming to guide targeted interventions, enhance patient care, and contribute valuable perspectives to the broader discourse on effective diabetes management. Thus, this study aimed to determine the prevalence and associated factors of diabetic microvascular complications among adults with T2DM in Adama, central Ethiopia.
Methods
Study design, setting, and population
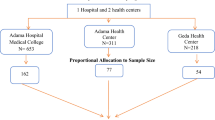
An institutional-based cross-sectional study was conducted at Adama Hospital Medical College (AHMC) in Ethiopia, covering a period of ten years from January 2012 to December 2022. AHMC is located in Adama town, approximately 99 km southeast of Addis Ababa in the Great Rift Valley of East Africa. It is one of the largest public teaching hospitals in the Oromia region, serving a catchment area of over five million people and acting as a referral hub for surrounding zones and regions. All adult T2DM patients who were on follow-up at AHMC constituted the source population, while all newly diagnosed adult T2DM patients who were on follow-up at AHMC from January 2012 to December 2022 were considered the study population.
Sample size determination and sampling procedure
The sample size was determined using a formula tailored for estimating a single population proportion. The calculation was based on specific statistical assumptions, including:
-
A cross-sectional study design to achieve the study objective.
-
A prevalence of DM microvascular complications (P) of 33.2%, derived from a previous study on DM microvascular complications38.
-
A confidence level of 95%, corresponding to a standard value (Z) of 1.96 and.
-
A calculated margin of error (d) of 0.048.
Thus, by inserting these parameters into the formula:
Finally, after adding a 5% adjustment for incomplete data, the final sample size for the study becomes 389.
The study participants were identified using their medical record numbers from individuals who had been under follow-up between January 2012 and December 2022, forming the initial sampling frame. From this group, participants were selected by a simple random sampling technique using computer-generated random numbers. This method ensured that each eligible individual had an equal opportunity to be included, minimizing potential biases and ensuring the sample’s representativeness of the broader population under study.
Study variables
Outcome variable
Microvascular complications (yes/no).
Independent variables
Socio-demographic variables (age, sex, place of residence, marital status), Clinical and comorbidity-related characteristics (type of treatment, proteinuria, triglyceride, total cholesterol, high-density lipoprotein, low-density lipoprotein, glycemic control, family history of T2DM, duration of DM, history of smoking, history of chronic heart disease, history of chronic kidney disease, history of stroke, history of hypertension).
Operational definitions
Microvascular complications
The presence of at least one of the following conditions associated with diabetes: diabetic neuropathy, diabetic nephropathy, or diabetic retinopathy, documented in the patient’s hospital record14,31,39.
Glycemic control
Hemoglobin A1C (HgA1C) below 7%, or the last fasting blood sugar (FBS) level 130 mg/dl or lower in the absence of documented HgA1C determined in less than three months, was considered as good glycemic control. Otherwise, it was classified as poor glycemic control40.
Data collection procedure and quality control
Data were gathered using a structured and pretested data extraction checklist developed after a comprehensive review of patient medical records, follow-up cards, diabetes registration logs, electronic information databases, and relevant prior studies. The checklist encompassed socio-demographic, clinical, and comorbidity-related characteristics. The data collection process was conducted by three trained nurses under the supervision of two public health professionals.
All data collectors and supervisors received one day of training focused on the study objectives, record retrieval procedures, and the overall data collection process. A pretest using 5% of the sample size (n = 19) was performed on records predating January 2012. Based on the pretest results, adjustments and corrections were made to the data extraction checklist. Throughout the data collection phase, supervisors and the principal investigator closely monitored the completeness and consistency of the data. In addition, all gathered data underwent thorough cross-checking during data entry to address any missing information.
Data processing and statistical analysis
The collected data were entered into Epi-Info version 7.2 software, and then exported to Statistical Package for the Social Sciences (SPSS) version 27 for processing and analysis. Before commencing analysis, data processing operations including data cleaning, computing, transforming, coding, recoding, and variable grouping were performed. Descriptive statistics were used to examine and summarize the characteristics of the study population across all variables. Frequency distributions were calculated for categorical variables, while appropriate numerical summary measures were employed to summarize continuous variables after checking for data normality using the Shapiro-Wilk test. The prevalence of diabetic microvascular complications was estimated using proportions and a 95% confidence interval (CI).
To model the association between diabetic microvascular complications and explanatory variables, binary logistic regression was employed. Hence, a bivariable logistic regression model was fitted to assess the crude associations between diabetic microvascular complications and each explanatory variable. At this stage, a p-value of 0.25 was chosen as the cut-off to select variables for multivariable logistic regression analysis, in which the associations were adjusted for potential confounders. Then all candidate variables were included in the multivariable regression analysis to pinpoint factors significantly associated with diabetic microvascular complications. A standard model-building approach was used to develop the model.
Before examining the association between diabetic microvascular complications and the independent variables, the model’s suitability was assessed using diagnostic tests. Specifically, Hosmer and Lemeshow’s test was conducted to evaluate the model’s goodness of fit. The diagnostic results indicated the model fit the data well (p = 0.252). To assess the proportion of variation in diabetic microvascular complications accounted for by the combined influence of explanatory variables, Nagelkerke R-square was calculated. The findings indicated that 15.9% of the variation in diabetic microvascular complications is explained by the collective effects of the variables included in the model. Multicollinearity among the explanatory variables was examined using the variance inflation factor (VIF), which was found to be in the range of 1.015 to 1.269, indicating no collinearity among the covariates. In the final model, an adjusted odds ratio (AOR) with a 95% CI was used to estimate the strength of association, and statistical significance was proclaimed at a p-value < 0.05.
Results
Socio-demographic characteristics
A total of 381 records of patients with T2DM were reviewed and included in the final analysis. The median age of the participants was 49 years (IQR = 38–60). Among the participants, 208 (54.6%) were male. The majority, 281 (73.8%), resided in Adama, and 283 (74.3%) were married (Table 1).
Clinical and comorbidity-related characteristics
In this study, 172 participants (45.1%) were on oral hypoglycemic agents, while 343 (90%) had HDL levels under 40 mg/dL. The majority of DM patients, 331 (86.9%), had good glycemic control, 248 (63.8%) had been living with DM for less than 5 years, and 161 (42.3%) had a history of hypertension (Table 2).
The prevalence of diabetic microvascular complications
The overall prevalence of diabetic microvascular complications among T2DM patients was 21.8% (95% CI: 17.8–25.6). Among these complications, diabetic neuropathy was the most common at 16.8% (95% CI: 13.5–21.5), followed by diabetic retinopathy at 4.2% (95% CI: 2.4–6.3), and diabetic nephropathy at 2.9% (95% CI: 1.2–4.7). Additionally, 19.7% of the participants had only one microvascular complication, while 2.1% had more than one complication.
Factors associated with diabetic microvascular complications
In the bivariable logistic regression analysis, age, type of treatment, high-density lipoprotein level, glycemic control, family history of T2DM, duration of DM, and history of hypertension were found to have a crude association with diabetic microvascular complications at a p-value of < 0.25. After adjusting for all potential confounders in a multivariable logistic regression analysis, age, glycemic control, and history of hypertension remained statistically significant factors, each with a p-value of less than 0.05.
Consequently, this study found that T2DM patients aged 41–60 had 65% lower odds of developing diabetic microvascular complications compared to those aged over 60 years (AOR = 0.35, 95% CI: 0.18–0.68). The odds of developing diabetic microvascular complications were two-fold greater among T2DM patients with poor glycemic control compared to those with good glycemic control (AOR = 2.00, 95% CI: 1.01–3.98). Similarly, in contrast to T2DM patients without a history of hypertension, those with a history of hypertension exhibited 2.4 times higher odds of developing diabetic microvascular complications (AOR = 2.36, 95% CI: 1.39–4.00) (Table 3).
Discussion
This study revealed that the prevalence of diabetic microvascular complications was 21.8% (95% CI: 17.8–25.6). This is comparable to findings from studies conducted in Northern Ethiopia (19.5%)41and India (18.04%)28. Conversely, the prevalence found in this study is lower than that reported in studies from Northwest Ethiopia (26.3%)42, Southern Ethiopia (26.5%)31, Northeast, Ethiopia (33.2%)38, Southwest Ethiopia (41.5%)43, Dessie town hospitals, Ethiopia (37.9%)14, Ayder Referral Hospital, Ethiopia (42.6%)44, Sudan (45.9%)45, Tanzania (57.6%)46, Nigeria (69.3%)47, Saudi Arabia (55.1%)48, Qatar (48.4%)49, South India (52.1%)50, China (57.5%, 34.5%)32,51. Additionally, the prevalence of diabetic microvascular complications in this study is higher than the figure reported in a systematic review and meta-analysis conducted in low and middle-income countries (12%)52. These discrepancies could be attributed to variations in the diagnostic and screening methods or criteria for diabetic-related microvascular complications, as well as differences in access to healthcare services and the quality of diabetes management. Additionally, variations in the demographic and clinical characteristics of the study populations, differences in sample sizes, socio-demographic factors, and disparities in study periods might also explain the observed variations.
In the current study, T2DM patients aged 41–60 had lower odds of developing diabetic microvascular complications compared to those over 60 years old. This finding aligns with previous studies in Southern Ethiopia31, Saudi Arabia53, and China51, which showed that increasing age is associated with higher odds of developing diabetic microvascular complications. Additionally, studies from Dessie town hospitals14and Ayder Referral Hospital44in Ethiopia, as well as from India28, also indicated that older age is associated with the development of these complications. Aging is associated with structural and functional changes in the vascular system, including increased arterial stiffness and endothelial dysfunction, vascular calcification, reduced baroreceptor sensitivity, increased oxidative stress, and chronic inflammation, which collectively contribute to the heightened risk of microvascular complications in older adults with diabetes. These changes impair the ability of blood vessels to respond to metabolic demands and exacerbate the damage caused by hyperglycemia, making the management of diabetes in older populations particularly crucial29,54,55,56.
In agreement with previous studies done in Saudi Arabia27,17, Pakistan57, Turkey58, and Southern Ethiopia31. This study revealed that the odds of developing diabetic microvascular complications were two-fold greater among T2DM patients with poor glycemic control compared to those with good glycemic control. This can be justified by the fact that poor glycemic control leads to the formation of advanced glycation end products (AGEs), increased oxidative stress, chronic inflammation, endothelial dysfunction, activation of protein kinase C, and alterations in the polyol pathway. These biochemical changes collectively damage small blood vessels, causing microvascular complications. The thickening of basement membranes, increased vascular permeability, and endothelial cell dysfunction contribute to vision loss, kidney dysfunction, and nerve damage, highlighting the critical importance of maintaining optimal blood glucose levels to prevent these serious complications59,61,62,62.
Hypertension was another significant factor associated with the development of diabetic microvascular disorders. Compared to T2DM patients without a history of hypertension, those with a history of hypertension had greater odds of developing diabetic microvascular complications. This finding was supported by studies done in Ireland63, Spain64, Romania65,China32,51, Thailand30,Qatar49, Tanzania46,Dessie town hospitals, Ethiopia14and Southern Ethiopia31. Hypertension accelerates microvascular complications in diabetic patients by increasing intracellular hyperglycemia, which leads to oxidative stress, inflammation, and endothelial dysfunction. The heightened vascular pressure from hypertension further damages small blood vessels, leading to more rapid progression and increased severity of these complications66,67.
When interpreting the study’s findings, it is essential to consider certain limitations. Because of the study’s retrospective nature, we were unable to explore the effects of certain sociodemographic, clinical, and behavioral factors. Exploring these factors could have enriched the study by providing a more comprehensive understanding of how different aspects of a person’s background, medical history and current health status and behavior may influence the development of diabetic complications. Moreover, given the cross-sectional design of the study, establishing causal relationships between dependent and independent variables is difficult.
Conclusion
This study revealed that 1 in 5 patients with T2DM experienced at least one diabetic microvascular complication. Poor glycemic control and a history of hypertension were found to have a positive association with the development of these complications, while, being aged between 41 and 60 years showed a negative association. Early detection of these complications is crucial, highlighting the need for proactive interventions to manage modifiable risk factors such as poor glycemic control and hypertension that contribute to the onset of diabetic microvascular issues in individuals with T2DM.
Data availability
All data and materials are available from the corresponding author without undue reservation.
References
Lovic, D. et al. The growing epidemic of diabetes Mellitus. CVP. 18 (2), 104–109 (2020).
Cheran, K. et al. The Growing Epidemic of Diabetes Among the Indigenous Population of Canada: A Systematic Review. Cureus [Internet]. 2023 Mar 15 [cited 2024 Jul 16]; https://www.cureus.com/articles/126446-the-growing-epidemic-of-diabetes-among-the-indigenous-population-of-canada-a-systematic-review
World Health Organization. Classification of diabetes mellitus. ; (2019).
Leslie, R. D., Palmer, J., Schloot, N. C. & Lernmark, A. Diabetes at the crossroads: relevance of disease classification to pathophysiology and treatment. Diabetologia. 59 (1), 13–20 (2016).
Animaw, W. & Seyoum, Y. Increasing prevalence of diabetes mellitus in a developing country and its related factors. PLoS One. 12 (11), e0187670 (2017).
Gassasse, Z., Smith, D., Finer, S. & Gallo, V. Association between urbanisation and type 2 diabetes: an ecological study. BMJ Glob Health. 2 (4), e000473 (2017).
Cho, N. H. et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 138, 271–281 (2018).
Sun, H. et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 183, 109119 (2022).
Hossain, M. J., Al-Mamun, M. & Islam, M. R. Diabetes mellitus, the fastest growing global public health concern: early detection should be focused. Health Sci. Rep. 7 (3), e2004 (2024).
American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 40, S1–129 (2017).
Fowler, M. J. Microvascular and macrovascular complications of diabetes. Clin. Diabetes. 3, 116–122 (2011).
Merid, F., Getahun, F., Esubalew, H. & Gezahegn, T. Diabetic microvascular complications and associated factors in patients with type 2 diabetes in Southern Ethiopia. Front Endocrinol [Internet]. 2024 Jul 4 [cited 2024 Jul 9];15. https://www.frontiersin.org/journals/endocrinology/articles/https://doi.org/10.3389/fendo.2024.1342680/full
Stolar, M. Glycemic Control and complications in type 2 diabetes Mellitus. Am. J. Med. 123 (3, Supplement), S3–11 (2010).
Seid, M. A. et al. Microvascular complications and its predictors among type 2 diabetes mellitus patients at Dessie town hospitals, Ethiopia. Diabetol. Metab. Syndr. 13 (1), 86 (2021).
Bui, H. D. T. et al. Prevalence of and factors related to microvascular complications in patients with type 2 diabetes mellitus in Tianjin, China: a cross-sectional study. Ann. Trans. Med. 7, 325. https://doi.org/10.21037/atm (2019).
Bansal, D. et al. Microvascular complications and their associated risk factors in newly diagnosed type 2 diabetes mellitus patients. Int. J. Chronic Dis. 2014, 201423. https://doi.org/10.1155/2014/201423 (2014).
Saiyed, N. S. et al. Risk factors of microvascular complications among type 2 diabetic patients using cox proportional hazards models: a cohort study in tabuk Saudi Arabia. J. Multidiscip Healthc. 15, 1619–1632. https://doi.org/10.2147/JMDH.S367241 (2022).
Dweib, M. & El Sharif, N. Diabetes-related microvascular complications in primary health care settings in the West Bank, Palestine. J. Clin. Med. 12, 6719. https://doi.org/10.3390/jcm12216719 (2023).
Cheema, S. et al. Risk factors for microvascular complications of diabetes in a high-risk middle east population. J. Diabetes Res. 2018, 7. https://doi.org/10.1155/2018/8964027 (2018).
Annani-akollor, M. E. et al. Predominant complications of type 2 diabetes in Kumasi: a 4-year retrospective cross-sectional study at a teaching hospi_tal in Ghana. Med. (B Aires). 55 (125), 1–11 (2019).
Jasper, U., Opara, M. & Pyiki, E. Prevalence and clinical pattern of acute and chronic complications in African diabetic patients. Br. J. Med. Med. Res. 4, 4908. https://doi.org/10.9734/BJMMR (2014).
Korsa, A. T., Genemo, E. S., Bayisa, H. G. & Dedefo, M. G. Diabetes mellitus complica_tions and associated factors among adult diabetic patients in selected hospitals of west Ethiopia diabetes mellitus complications and associated factors among adult diabetic patients in selected hospitals of West Ethio_pia. Open. Cardiovasc. Med. J. 13, 41–48 (2019).
Gebre, B. B. & Assefa, Z. M. Magnitude and associated factors of diabetic complication among diabetic patients attending gurage zone hospitals. South. West. BMC Res. Notes. 12 (780), 1–6. https://doi.org/10.1186/s13104-019-4808-9 (2019).
Sheleme, T., Mamo, G., Melaku, T. & Sahilu, T. Prevalence, patterns and predic_tors of chronic complications of diabetes mellitus at a large referral hospital in Ethiopia: a prospective observational study. Diabetes Metab. Syndr. Obes. Targets Ther. 13, 4909–4918 (2020).
Fasil, A. B. & Belete, A. M. Glycemic control and diabetes complications among diabetes mellitus patients attending at University of Gondar Hospital, Northwest Ethiopia. Diabetes Metab. Syndr. Obes. Targets Ther. 12, 75–83 (2019).
An, T. Major microvascular complications and associated risk factors among endocrinology & metabolic syndrome major microvascular complications and associated risk factors among diabetic outpatients in Southwest Ethiopia. Endocrinol. Metab. Syndr. 6 (4), 1–10 (2017).
Al-Shehri, F. S. Glycemic Control and Microvascular complications of type 2 diabetes among saudis. JDM. 09 (04), 167–175 (2019).
Bansal, D. et al. Microvascular complications and their Associated Risk factors in newly diagnosed type 2 diabetes Mellitus patients. Int. J. Chronic Dis. 2014, 1–7 (2014).
for the ADVANCE Collaborative group et al. Impact of age, age at diagnosis and duration of diabetes on the risk of macrovascular and microvascular complications and death in type 2 diabetes. Diabetologia. 57 (12), 2465–2474 (2014).
Hurst, C., Thinkhamrop, B. & Tran, H. T. The Association between Hypertension Comorbidity and Microvascular complications in type 2 diabetes patients: a nationwide cross-sectional study in Thailand. Diabetes Metab. J. 39 (5), 395 (2015).
Merid, F., Getahun, F., Esubalew, H. & Gezahegn, T. Diabetic microvascular complications and associated factors in patients with type 2 diabetes in Southern Ethiopia. Front. Endocrinol. 15, 1342680 (2024).
Thi Bui, H. D. et al. Prevalence of and factors related to microvascular complications in patients with type 2 diabetes mellitus in Tianjin, China: a cross-sectional study. Annals of Translational Medicine; Vol 7, No 14 (July 31, 2019): Annals of Translational Medicine [Internet]. [cited 2019 Jan 1]; (2019). https://atm.amegroups.org/article/view/26961
Ekoru, K. et al. Type 2 diabetes complications and comorbidity in Sub-saharan africans. EClinicalMedicine. 16, 30–41 (2019).
Crasto, W., Patel, V., Davies, M. J. & Khunti, K. Prevention of Microvascular complications of Diabetes. Endocrinol. Metab. Clin. North Am. 50 (3), 431–455 (2021).
Marshall, S. M. & Flyvbjerg, A. Prevention and early detection of vascular complications of diabetes. BMJ. 333 (7566), 475–480 (2006).
Zheng, Y., Ley, S. H. & Hu, F. B. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat. Rev. Endocrinol. 14 (2), 88–98 (2018).
Federation, I. D. IDF Diabetes Atlas, tenth. Int. Diabetes ; (2021).
Taderegew, M. M. et al. Platelet Indices and Its Association with Microvascular complications among type 2 diabetes Mellitus patients in Northeast Ethiopia: a cross-sectional study. DMSO. 14, 865–874 (2021).
Kosiborod, M. et al. Vascular complications in patients with type 2 diabetes: prevalence and associated factors in 38 countries (the DISCOVER study program). Cardiovasc. Diabetol. 17 (1), 150 (2018).
Care, D. Standards of medical care in diabetes 2019. Diabetes Care. 42 (Suppl 1), S124–S138 (2019).
Gebremedhin, H. & Aregawi, B. G. Micro Vascular complications and Associated factors among type two Diabetic patients in Adigrat and Wkuro General hospitals, Northern Ethiopia: a retrospective cross-sectional study. J. Diabetes Metabolism. 11, 1–7 (2020).
Shita, N. G. & Isayu, A. S. Predictors of blood glucose change and microvascular complications of type 2 diabetes mellitus patients in Felege Hiwot and Debre Markos referral hospital, North West Ethiopia. BMC Endocr. Disord. 22 (1), 136 (2022).
An, T. et al. Major Micro vascular Complications and Associated Risk Factors among Diabetic Outpatients in Southwest Ethiopia. Endocrinol Metab Syndr [Internet]. 2017 [cited 2024 Jul 13];06(04). https://www.omicsonline.org/open-access/major-micro-vascular-complications-and-associated-risk-factors-amongdiabetic-outpatients-in-southwest-ethiopia-2161-1017-1000272.php?aid=92151
Berihun, L. & Muluneh, E. K. Correlates of time to microvascular complications among diabetes mellitus patients using parametric and non-parametric approaches: a case study of Ayder referral hospital, Ethiopia. Eth J. Sci. Technol. 10 (1), 65 (2017).
Hussein, M. & Menasri, S. Prevalence of Microvascular complications in type 2 diabetics attending a primary Healthcare Centre in Sudan. Dubai Diabetes Endocrinol. J. 25 (3–4), 127–133 (2019).
Shillah, W. B., Yahaya, J. J., Morgan, E. D. & Bintabara, D. Predictors of microvascular complications in patients with type 2 diabetes mellitus at regional referral hospitals in the central zone, Tanzania: a cross-sectional study. Sci. Rep. 14 (1), 5035 (2024).
Ikem, R. T., Enikuomehin, A. C., Soyoye, D. O. & Kolawole, B. A. The burden of diabetic complications in subjects with type 2 diabetes attending the diabetes clinic of the Obafemi Awolowo University Teaching Hospital, Ile-Ife, Nigeria - a cross-sectional study. Pan Afr Med J [Internet]. [cited 2024 Jul 13];43. (2022). https://www.panafrican-med-journal.com/content/article/43/148/full
Alnaim, M. M., Alrasheed, A., Alkhateeb, A. A., Aljaafari, M. M. & Alismail, A. Prevalence of microvascular complications among patients with type 2 diabetes mellitus who visited diabetes clinics in Saudi Arabia. Saudi Med. J. 44 (2), 211 (2023).
Cheema, S. et al. Risk factors for Microvascular Complications of Diabetes in a high-risk Middle East Population. J. Diabetes Res. 2018, 1–7 (2018).
Govindarajan Venguidesvarane, A. et al. Prevalence of vascular complications among type 2 Diabetic patients in a Rural Health Center in South India. J. Prim. Care Community Health. 11, 215013272095996 (2020).
Li, J. et al. Prevalence and associated factors of vascular complications among inpatients with type 2 diabetes: a retrospective database study at a tertiary care department, Ningbo, China. PLoS One. 15 (6), e0235161 (2020).
Aikaeli, F. et al. Prevalence of microvascular and macrovascular complications of diabetes in newly diagnosed type 2 diabetes in low-and-middle-income countries: A systematic review and meta-analysis. Asweto CO, editor. PLOS Glob Public Health. ;2(6):e0000599. (2022).
Alaboud, A. F. et al. Microvascular and macrovascular complications of type 2 diabetic mellitus in Central, Kingdom of Saudi Arabia. SMJ. 37 (12), 1408–1411 (2016).
Ungvari, Z., Kaley, G., De Cabo, R., Sonntag, W. E. & Csiszar, A. Mechanisms of vascular aging: New perspectives. Journals Gerontol. Ser. A: Biol. Sci. Med. Sci. 65A (10), 1028–1041 (2010).
Seals, D. R., Jablonski, K. L. & Donato, A. J. Aging and vascular endothelial function in humans. Clin. Sci. 120 (9), 357–375 (2011).
Strait, J. B. & Lakatta, E. G. Aging-associated cardiovascular changes and their relationship to heart failure. Heart Fail. Clin. 8 (1), 143–164 (2012).
Ali, A. et al. Prevalence of microvascular complications in newly diagnosed patients with Type 2 diabetes. Pak J Med Sci [Internet]. Jun 10 [cited 2024 Jul 15];29(4). (2013). http://pjms.com.pk/index.php/pjms/article/view/3704
Kayar, Y. et al. Relationship between the poor glycemic control and risk factors, life style and complications. Biomed. Res. 28 (4), 1581–1586 (2017).
Oguntibeju, O. O. Type 2 diabetes mellitus, oxidative stress and inflammation: examining the links. Int. J. Physiol. Pathophysiol Pharmacol. 11 (3), 45–63 (2019).
Nakamura, A. & Kawaharada, R. Advanced Glycation End Products and Oxidative Stress in a Hyperglycaemic Environment. In: Alok Raghav, Jamal Ahmad, editors. Fundamentals of Glycosylation [Internet]. Rijeka: IntechOpen; 2021 [cited 2024 Jul 16]. p. Ch. 2. https://doi.org/10.5772/intechopen.97234
Mauricio, D., Gratacòs, M. & Franch-Nadal, J. Diabetic microvascular disease in non-classical beds: the hidden impact beyond the retina, the kidney, and the peripheral nerves. Cardiovasc. Diabetol. 22 (1), 314 (2023).
Mengstie, M. A. et al. Endogenous advanced glycation end products in the pathogenesis of chronic diabetic complications. Front. Mol. Biosci. 9, 1002710 (2022).
Tracey, M. L. et al. Risk factors for macro- and microvascular complications among older adults with diagnosed type 2 diabetes: findings from the Irish longitudinal study on Ageing. J. Diabetes Res. 2016, 1–9 (2016).
Del Cañizo Gómez FJ et al. Microvascular complications and risk factors in patients with type 2 diabetes. Endocrinología Y Nutrición. 58 (4), 163–168 (2011).
Dobrica, E. et al. Journal of Hypertension [Internet]. ;37. (2019). https://journals.lww.com/jhypertension/fulltext/2019/07001/macrovascular_and_microvascular_complications_in.391.aspx
Petrie, J. R., Guzik, T. J. & Touyz, R. M. Diabetes, hypertension, and Cardiovascular Disease: clinical insights and vascular mechanisms. Can. J. Cardiol. 34 (5), 575–584 (2018).
Lastra, G., Syed, S., Kurukulasuriya, L. R., Manrique, C. & Sowers, J. R. Type 2 diabetes Mellitus and Hypertension. Endocrinol. Metab. Clin. North Am. 43 (1), 103–122 (2014).
Acknowledgements
The authors express their gratitude to the officials of the Adama town public health facility for their invaluable support throughout this study. Special thanks are also extended to our dedicated team of data collectors and supervisors, whose meticulous efforts ensured the smooth execution of this study. Lastly, heartfelt appreciation goes to all study participants for their essential contributions to advancing our understanding in this field.
Author information
Authors and Affiliations
Contributions
YMN conceived the study idea, conducted data extraction, performed statistical analysis, interpreted the findings. YMN, MS and NMF critically reviewed, and finalized the version for submission. All authors thoroughly read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
Ethical approval was obtained from the Institutional Ethical Review Board of Adama Hospital Medical College. Permission to access medical records was granted by the hospital’s medical director. Since the study involved secondary data analysis of existing medical records, the Institutional Ethical Review Board of Adama Hospital Medical College waived the requirement for obtaining informed consent. Throughout the study, strict confidentiality of data was maintained, and data was stored on a secure, password-protected system. The study’s procedures were all conducted in accordance with the principles of the Helsinki Declaration.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Negussie, Y.M., Sento, M. & Fati, N.M. Diabetic microvascular complications among adults with type 2 diabetes in Adama, central Ethiopia. Sci Rep 14, 24910 (2024). https://doi.org/10.1038/s41598-024-77183-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-77183-2