Abstract
The aim of this study was to investigate the role of platelet indicators in the susceptibility of ABO blood groups to lung adenocarcinoma. This was a multicenter retrospective cohort analysis. The study included 528 patients diagnosed with primary lung adenocarcinoma and 528 randomly selected control group patients who were admitted to the Chengdu Fifth People’s Hospital from January 2021 to September 2023. Additionally, it included 1452 patients diagnosed with primary lung adenocarcinoma and 1452 control group patients who were admitted to the Sichuan Cancer Hospital from November 2013 to May 2021. Platelet indicators were studied using an automated blood counter. ABO blood groups were determined by the gel column method using agglutination techniques. Statistical analysis was performed using Chi-square tests, independent-samples T-tests, ANOVA, and logistic regression. Chi-square analysis showed that there was a difference in ABO blood group composition between the lung adenocarcinoma group and the control group (p < 0.001). Independent-samples T-tests showed that MPV was significantly higher in lung adenocarcinoma than in control group (p = 0.025). The ANOVA of ABO blood groups and platelet indicators in lung adenocarcinoma showed that the average platelet count (PLT) of O group blood was higher than that of B group blood (p = 0.037), while the mean platelet volume (MPV) was significantly lower than that of A group, B group and AB group blood (p = 0.009). After adjusting for gender and age, logistic regression analysis showed that the risk of lung adenocarcinoma in blood groups O and B was higher than that in blood group A (p < 0.05 for each) and blood group AB (p < 0.05 for each), regardless of whether platelet indicators were added. Meanwhile, logistic regression showed that high platelet volume (MPV) was a risk factor for lung adenocarcinoma (p = 0.029). Our findings suggest that platelet indicators are respectively associated with ABO blood groups and lung adenocarcinoma. However, platelet indicators may not influence the ABO blood groups related susceptibility to Lung Adenocarcinoma.
Similar content being viewed by others
Introduction
Cancer is a major public health problem. Some progress has been made in the treatment of cancer. Cancer remains a leading cause of death by disease. Every year, more than 19 million people are diagnosed with cancer and 10 million die of the disease, accounting for one in six deaths globally1. According to the “Cancer Statistics 2023”, lung cancer is the leading cause of death2. Data showed that about 350 people die from lung cancer every day2. Histological classification of lung cancer: squamous cell carcinoma, adenocarcinoma, small cell carcinoma, large cell carcinoma2,3. The most common type of lung cancer is adenocarcinoma, comprising around 40% of all lung cancer cases. In spite of achievements in understanding the pathogenesis of this disease and the development of new approaches, unfortunately, lung adenocarcinoma is still one of the most aggressive and rapidly fatal tumor types with overall survival less than 5 years4.
The relationships between ABO blood groups and risk of cancers have been studied since the 1960’s5. In recent years, more and more studies on ABO blood group and cancer have found that there is a significant correlation between ABO blood group and pancreatic cancer, breast cancer, salivary gland cancer, oral cancer, gastric cancer, chronic lymphocytic leukemia, bladder cancer, pharyngeal cancer, esophageal adenocarcinoma, and small bowel cancer6,7,8. In 2022, A large cohort of 7681 lung cancer patients in Nanchang, China, study showed that the risk of lung adenocarcinoma in blood type O was higher than that in blood type A9. However, a study from Kasairi, Turkey, found no correlation between ABO blood types and various types of lung cancer10. In addition, in 2012, León-Atance et al. observed that Blood group antigen A was closely related to lung adenocarcinoma11. Overall, the relationship between lung adenocarcinoma and ABO blood group remains controversial.
Inflammation and genetic predisposition influence lung cancer risk. Previous studies have suggested that the inflammatory response may depend on the ABO phenotype12. ABO blood groups, first discovered by Landsteiner in the last century, were the polymorphic genetic phenotypes to be revealed13. Due to its stable heritability and correlation with diseases, it has been highly valued by medical researchers. In recent years, more and more reports have been made on the relationship between the ABO blood group and malignant tumors6,7,8,9.
Numerous studies have shown that the hematological components of the systemic inflammatory response are closely related to platelet-related indicators14,15. Platelets are altered by cancer cells, and platelets facilitated the survival and diffusion of cancer cells. Platelets affect several aspects of cancer biology in multiple ways, including cancer growth and metastasis, immune evasion, tumor angiogenesis, and sometimes the slowing of tumor growth16. Platelets are an important part of the tumor microenvironment, and there is a significant cross communication between platelets and cancer cells. Cancer cells alter the activation status of platelets, their RNA spectrum, proteome, and other properties. The “cloaking” of cancer cells by platelets providing physical protection, avoiding destruction from shear stress and the attack of immune cells, promoting tumor cell invasion17. Platelet indicators have been associated with cancer, for example: high platelet count associated with poor survival and worse prognosis for many cancer types, high mean platelet volume (MPV) is a predictor of poor prognosis in various types of cancer17. There have been relatively few studies on the platelet indicators of ABO blood groups. In 2018, there was a study of the relationship between platelet index and ABO blood group in 301 healthy volunteers attending the cardiology clinic of Harran University medical faculty18. Platelets are tightly linked to the ABO blood groups, Platelets express ABO antigens and platelet indicators are related to ABO blood groups. Most of the existing studies have focused on the relationship between platelet indicators and diseases14,15,16,17, explored the risks and benefits of ABO blood group and platelet transfusion19,20, and studied the relationship between ABO blood groups and diseases7,9,10,11,12,21. The lack of linking the three to analyze whether platelet indicators affect the susceptibility of ABO blood group to malignancy. Currently, no studies have investigated the impact of platelet indicators on susceptibility to lung adenocarcinoma across different ABO blood groups.
In this study, we aim to elucidate the relationship between ABO blood group types, platelet indicators, and susceptibility to lung adenocarcinoma. Specifically, we seek to determine whether platelet indicators influence the susceptibility associated with ABO blood group variations in lung adenocarcinoma (Fig. 1). Our findings propose novel insights that could potentially inform innovative approaches in the clinical management of lung adenocarcinoma.
Materials and methods
Patient characteristics
This study was a multicenter retrospective cohort study, Chengdu Fifth People’s Hospital as a general hospital and Sichuan Cancer Hospital as a specialist hospital. Patients were screened according to inclusion and exclusion criteria. Inclusion criteria: 1, All patients had a first diagnosis of lung adenocarcinoma by histopathology or cytology, and no bone marrow infiltration. 2, All patients were Rh(D) positive. 3, Complete ABO blood group results. 4, Complete platelet indicators results. Exclusion criteria: 1, Patients with concurrent tumors at other sites; 2, Patients with repeat admission; 3, without ABO blood group results or RH(D) negative and subtype; 4, without platelet indicators results. This multicenter retrospective study included 528 patients diagnosed with primary lung adenocarcinoma and 528 randomly selected control patients admitted to Chengdu Fifth People’s Hospital from January 2021 to September 2023. Additionally, the study encompassed 1,452 patients diagnosed with primary lung adenocarcinoma and 1,452 control patients admitted to Sichuan Cancer Hospital from November 2013 to May 2021. A total of 1980 patients with lung adenocarcinoma were enrolled. A total of 1980 control group patients were enrolled as a control group.
Data collection
The clinical data included gender, age, ABO blood group, and platelet indicators. Platelet venous blood was collected at the same time as ABO blood group samples. The blood samples were taken in tubes containing ethylene diamine tetraacetic acid. The pathological type was first diagnosed as lung adenocarcinoma. Platelet count (PLT), mean platelet volume (MPV), platelet distribution width (PDW), and plateletcrit (PCT) were studied by an auto-analyzer. Sichuan Cancer Hospital applied BC-6600 (Mindray Medical Electronics Co., Shenzhen, China) hematology analyzer, and Chengdu Fifth People’s Hospitalr used BC-6800 (Mindray Medical Electronics Co., Shenzhen, China). ABO Blood groups were determined by the microcolumn gel immunoassay using agglutination techniques.
Statistical analysis
The statistical IBM SPSS Statistics version 25.0 software (IBM Corp, Armonk, NY, USA) were applied to analyze the date. The Chi square statistics were used to compare ABO blood groups and qualitative data of lung adenocarcinoma between the two groups. Independent sample T test was used to analyze the difference of platelet indicators between lung adenocarcinoma and control group. Multiple comparisons were made for ABO blood group and platelet numerical variables in patients. Statistical analysis was performed with the use of analysis of variance (ANOVA, post hoc multiple comparisons). The quantitative data were described by mean ± standard deviation (X ± S). The relationship between ABO blood group and lung adenocarcinoma was analyzed by logistic regression. The confidence interval was accepted as 95% throughout the analyses. All p-values < 0.05 were considered statistically significant.
Results
Study population summary
After excluding the 12,275 subjects following the criteria outlined in Fig. 2. A total of 1980 patients with lung adenocarcinoma and 1980 controls were selected in this study. The demographic characteristics of the enrolled subjects are summarized in Table 1.
ABO blood groups distribution
We used chi-square analysis to compare ABO blood group between lung adenocarcinoma group and control group. In the Fifth People’s Hospital of Chengdu, the ABO blood group distribution of lung adenocarcinoma patients and controls is shown in Table 2 (p = 0.045). In Sichuan Cancer Hospital, the ABO blood group distribution of lung adenocarcinoma patients and controls is shown in Table 3 (p < 0.001). In total, the ABO blood group distribution of lung adenocarcinoma patients and controls is shown in Table 4 (p < 0.001). The Multicenter results showed that there were significant in ABO blood group composition between lung adenocarcinoma group and control group (p < 0.001).
Correlation analysis of platelet parameters and lung adenocarcinoma
We used an independent sample T test to compare platelet indicators between the lung adenocarcinoma group and the control group. The platelet indicators of lung adenocarcinoma patients and control group are shown in Table 5; Fig. 3. The results showed that MPV was significantly higher in lung adenocarcinoma than in control group (p = 0.025). However, no significant differences were detected in PLT, PCT, and PDW (p > 0.05 for each).
Correlation analysis of platelet parameters and ABO blood group
In the control group, we explored the association between ABO blood group and platelet indicators, and observed that there were no statistical significance between PLT, PCT, MPV, PDW and ABO blood groups (p > 0.05 for each, Table 6).
In lung adenocarcinoma group, The comparison of alterations in platelet indicators among ABO blood group subjects is presented in Table 7 and in Figs. 4 and 5, PLT was found to be significantly higher in O blood group than in B blood group (p = 0.005). MPV was found to be significantly lower in O blood group than in A, B, and AB blood group (p = 0.008, p = 0.006 and p = 0.028, respectively). However, no considerable differences with respect to PCT and PDW among ABO blood group subjects were detected (P > 0.05 for each).
Analysis of correlation between related factors and lung adenocarcinoma
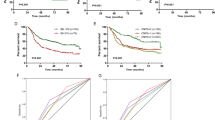
We used logistic regression to calculate odds ratios (OR) and 95% confidence intervals (95% CI) for lung adenocarcinoma by ABO blood groups, adjusted for age, gender, and platelet indicators (MPV). In the logistic regression, we divided gender into two groups: female = 0, male = 1, the odds ratio was calculated based on gender index against female. From Table 4, we found that the proportion of blood group O and blood group B in lung adenocarcinoma were higher than that in the control group. So, we took ABO blood group (O = 0, A = 1, B = 2, AB = 3, the odds ratio was calculated based on each blood group against blood group O) were independent variables, and ABO blood group (B = 0, A = 1, O = 2, AB = 3, the odds ratio was calculated based on each blood group against blood group B) as the independent variable. Then, the logistic regression analysis was performed variables. Figure 6 was a logistic analysis between lung adenocarcinoma group and ABO blood groups. From Fig. 6, this study analyzed the influence of platelet indicators on the susceptibility to lung adenocarcinoma concerning ABO blood groups. The analysis aimed to determine whether the inclusion of platelet indicators alters the risk associated with different ABO blood types. Specifically, the results for each ABO blood group were compared to those of the O blood group. This comparison was conducted in two scenarios: first, without considering the effects of platelet indicators, as shown in Fig. 6A; and second, with the addition of platelet indicators, as illustrated in Fig. 6B. Furthermore, a similar comparative analysis was performed for each ABO blood group against the B blood group. Again, the results were assessed under two conditions: without taking platelet indicators into account, as depicted in Fig. 6C, and with the inclusion of platelet indicators, as shown in Fig. 6D. This comprehensive analysis provides insights into how platelet indicators may modify the relationship between ABO blood group types and the susceptibility to lung adenocarcinoma.
Logistic Regression Analysis of Lung Adenocarcinoma and ABO Blood Group. This study analyzed whether ABO blood group alters the susceptibility to lung adenocarcinoma before and after the inclusion of platelet indicators. The odds ratio was calculated for each blood group relative to blood group O or B. (A-B) The analysis results for each ABO blood group were compared to those of group O, without (A) and with (B) the addition of platelet indicators. (C-D) The analysis results for each ABO blood group were compared to those of group B, without (C) and with (D) the addition of platelet indicators.
The results showed that 6 A, blood group O had a higher risk of lung adenocarcinoma than blood group A (P = 0.001; OR = 0.755; 95% CI: 0.643–0.888) and blood group AB (p = 0.045; OR = 0.780; 95% CI: 0.612–0.994). There was no association between blood group O and blood group B (p = 0.116; OR = 1.143; 95% CI: 0.968–1.350). 6B, blood group O had a higher risk of lung adenocarcinoma than blood group A P = 0.001; OR = 0.752; 95% CI: 0.639–0.884 and blood group AB (p = 0.040; OR = 0.775; 95% CI: 0.608–0.989). There was no association between blood group O and blood group B (p = 0.128; OR = 1.138; 95% CI: 0.963–1.345). 6 C, blood group B had a higher risk of lung adenocarcinoma than blood group A P = 0.000; OR = 0.661; 95% CI: 0.556–0.786 and blood group AB (p = 0.003; OR = 0.682; 95% CI: 0.531–0.877). There was no association between blood group B and blood group O (p = 0.116; OR = 0.875; 95% CI: 0.741–1.033). 6D, blood group B had a higher risk of lung adenocarcinoma than blood group A P = 0.000; OR = 0.661; 95% CI: 0.555–0.786 and blood group AB (p = 0.003; OR = 0.681; 95% CI: 0.530–0.875). There was no association between blood group B and blood group O (p = 0.128; OR = 0.879; 95% CI: 0.744–1.038). All four studies showed that women had a higher risk of lung adenocarcinoma than men (p < 0.001). The elderly was at higher risk of lung adenocarcinoma (p < 0.001; OR = 1.042; 95% CI: 1.036–1.048). High platelet volume (MPV) was a risk factor for lung adenocarcinoma (p = 0.029; OR = 1.041; 95% CI: 1.004–1.080).
Mean platelet volume distribution in blood group O
Logistic regression found that blood groups O and B were more susceptible, we divided mean platelet distribution into two groups: Reference lower limit (≤ 9.84 fl.) and Non-reference lower limit (>9.84 fl.) values based on Chengdu reference intervals22. The distribution is shown in Tables 8 and 9. The results showed that the MPV high value of blood group O and B in lung adenocarcinoma was higher than in control group.
Discussion
The aim of this study was to investigate the impact of platelet indicators on susceptibility to lung adenocarcinoma across ABO blood groups. Our findings reveal that individuals with blood groups O and B are at a higher risk of lung adenocarcinoma compared to those with blood groups A and AB, Whether or not platelet indicators were added. Moreover, we observed a significant correlation between ABO blood groups and platelet indicators in lung adenocarcinoma. Specifically, PLT was significantly elevated in the O blood group compared to the B blood group, while MPV was notably lower in the O blood group than in blood groups A, B, and AB. High MPV values emerged as a risk factor for lung adenocarcinoma, with elevated levels noted in the O and B blood group compared to controls. These findings underscore that platelet indicators influence ABO blood groups and lung adenocarcinoma, respectively. However, platelet indicators had no Influence on ABO blood group-related lung adenocarcinoma susceptibility.
Of course, susceptibility to lung adenocarcinoma is influenced by various factors, including smoking history, alcohol consumption, geographical region, and gender. The role of ABO blood group in susceptibility therefore necessitates consideration of platelet indicators. Our study showed that ABO blood group platelet indicators were not significant in the control group, while ABO platelet indicators were significant in lung adenocarcinoma. Risks associated with smoking, drinking, and gender have been clearly delineated in prior research. Nevertheless, ABO blood group susceptibility to lung adenocarcinoma exhibits variability across different regions. Our study specifically examines the impact of individual platelet indicators on ABO blood group susceptibility to lung adenocarcinoma.
Previous studies have shown that there were significant regional and ABO blood group differences in platelet indicators18,22. And our data are specifically from southwest Sichuan. Studies in healthy Chinese Han adults have reported significant region-based differences for all platelet indicators. For instance, individuals from Chengdu, Sichuan Province, exhibited the lowest mean PLT count and plateletcrit (PCT), yet the highest MPV, platelet distribution width (PDW), and platelet-large cell ratio (P-LCR)22. Studies from Turkey have also demonstrated a relationship between platelet indicators and ABO blood group in healthy adults; MPV was notably lower in subjects with blood groups O and A compared to those with AB and B blood groups. Similarly, PDW was significantly lower in subjects with blood groups O and A compared to those with B blood groups. Additionally, MPV levels were significantly lower in subjects with blood group O compared to non-O blood group subjects18.
The variability in ABO blood group susceptibility to lung adenocarcinoma observed across regions such as Jiangxi, China; Kayseri, Turkey; and Albacete, Spain9,10,11. May be attributed to variations in study population, different races and ABO blood group distribution percentage, thus influencing the heterogeneous susceptibility of ABO blood types to lung adenocarcinoma. Collectively, maybe the variability in study population and race contributes to the heterogeneous susceptibility of ABO blood types to lung adenocarcinoma. Age, sex, and platelet indicators did not affect susceptibility.
In this study, we demonstrated that MPV and PLT vary significantly across ABO blood groups in lung adenocarcinoma, whereas no significant differences were observed in the control group. Importantly, both the case and control groups originate from the same source. Previous Studies have shown that high MPV is of various types of cancer risk indicators17. Our study showed that the difference in MPV between lung adenocarcinoma and controls. And through the final logistic regression analysis also showed that high platelet volume (MPV) was a risk factor for lung adenocarcinoma. Although this difference was small, we think it illustrates the risk of high MPV. At the same time, research showed that the MPV high value of blood group O and B in lung adenocarcinoma was higher than in control group. In addition, there is an increased risk of thromboembolic events, which are the leading cause of death in cancer patients. In our study, blood group O had a higher PLT than the other three blood groups, especially blood group B. High platelets are a risk factor for thrombotic events. Additionally, platelet-VWF interaction is influenced by blood group23. ABO group not only exerts major quantitative and qualitative effects on VWF, but also affect specific aspects of platelet function. In general, VWF levels tend to be lower in patients with blood group O24. The significance of VWF to our research is worth pondering. Unfortunately, due to the retrospective study, VWF detection was not carried out in the laboratory before. We hope to have more research to show the role of VWF in this. In addition, the occurrence of lung adenocarcinoma has a certain relationship with gender, men had a lower risk of lung adenocarcinoma than women9,25, this conclusion is consistent with the results of this study. Our research shows that the elderly was at higher risk of lung adenocarcinoma. This conclusion is also consistent with the results of relevant studies9,25. So we believe these results are reliable.
Our study has several notable strengths. (1) The distribution of ABO blood group in China is characterized. Most southern ethnic groups have a higher O type frequency, except for a few ethnic groups in Yunnan (they have a higher A type frequencies); A majority of northern ethnic groups have a higher B type frequency, and a few of them have a O type frequency. Overall, the blood group distribution in China is O > A > B > AB9,26. This experiment, the ABO blood groups distribution of the control group was O > A > B > AB. The blood group distribution in this study was basically consistent with that in China. (2) Most studies of ABO blood groups and lung adenocarcinoma have included contemporaneous controls from patients without lung cancer, including those with other malignant diseases. A person’s serological ABO blood group may appear to change. For example, the ABO antigens can act as tumor markers27. Therefore, we only used contemporaneous benign patients as controls to minimize the influence of malignant diseases on serological ABO blood groups. And to ensure the control group and the homology of lung adenocarcinoma group. (3) Most experiments were analyzed in a single center, and the results may be biased. In this study, we used multicenter data analysis to avoid incomplete data analysis from a single center, and the results were more reliable with sufficient data sources.
Shortcomings of this study are as follows: (1) No pathological staging analysis was performed for lung adenocarcinoma. (2) The platelet indicators in this study did not include the proportion of large platelets (P-LCR).
We also observed that platelets secrete a lot of chemicals. such as ADP, TXA2, TGF-β, microRNA. For example platelets-derived microRNAs are associated with lung adenocarcinoma17. Here we study the effects of platelets, limited to platelet indicators (PLT, PCT, MPV, PDW), which belong to the physical aspects of platelets. The effect of platelet secreted substances on ABO susceptibility to lung adenocarcinoma deserves further exploration.
In conclusion, these findings suggest that platelet indicators are respectively associated with ABO blood groups and lung adenocarcinoma. However, Platelet Indicators may not influence the ABO blood groups related Susceptibility to Lung Adenocarcinoma. Further elucidation necessitates a larger volume of multicenter data.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Jassim, A., Rahrmann, E. P., Simons, B. D. & Gilbertson, R. J. Cancers make their own luck: Theories of cancer origins. Nat. Rev. Cancer. 23 (10), 710–724 (2023).
Siegel, R. L., Miller, K. D., Wagle, N. S. & Jemal, A. Cancer statistics, 2023. CA-Cancer J. Clin. 73 (1), 17–48 (2023).
Thai, A. A., Solomon, B. J., Sequist, L. V., Gainor, J. F. & Heist, R. S. Lung cancer. Lancet 398 (10299), 535–554 (2021).
Denisenko, T. V., Budkevich, I. N. & Zhivotovsky, B. Cell death-based treatment of lung adenocarcinoma. Cell. Death Dis. 9 (2), 117 (2018).
Aird, I., Lee, D. R. & Roberts, J. A. ABO blood groups and cancer of oesophagus, cancerof pancreas, and pituitary adenoma. Br. Med. J. 1 (5180), 1163–1166 (1960).
Vasan, S. K. et al. ABO blood group and risk of cancer: A register-based cohort study of 1.6 million blood donors. Cancer Epidemiol. 44, 40–43 (2016).
Wolpin, B. M. et al. Pancreatic cancer risk and ABO blood group alleles: Results from the pancreatic cancer cohort consortium. Cancer Res. 70 (3), 1015–1023 (2010).
Groot, H. E. et al. Genetically determined ABO blood group and its associations with Health and Disease. Arterioscl Throm Vas. 40 (3), 830–838 (2020).
Yang, H. et al. Influence of ABO blood group on susceptibility to different pathological types of lung cancer: A retrospective study. World J. Surg. Oncol. 20 (1), 379 (2022).
Unal, D. et al. ABO blood groups are not associated with treatment response and prognosis in patients with local advanced non- small cell lung cancer. Asian Pac. J. Cancer Prev. 14 (6), 3945–3948 (2013).
Leon-Atance, P. et al. Prognostic influence of loss of blood group a antigen expression in pathologic stage I non-small-cell lung cancer. Arch. Bronconeumol. 48 (2), 49–54 (2012).
Suadicani, P., Hein, H. O. & Gyntelberg, F. ABO phenotypes and inflammation-related predictors of lung cancer mortality: The Copenhagen male study - a 16-year follow-up. Eur. Respir J. 30 (1), 13–20 (2007).
Landsteiner, K. [Agglutination phenomena of normal human blood]. Wien Klin. Wochenschr. 113 (20–21), 768–769 (2001).
Dan, J., Tan, J., Huang, J., Yuan, Z. & Guo, Y. Early changes of platelet–lymphocyte ratio correlate with neoadjuvant chemotherapy response and predict pathological complete response in breast cancer. Mol. Clin. Oncol. 19 (5), 90 (2023).
Luo, H. et al. Normal reference intervals of neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, lymphocyte-to-monocyte ratio, and systemic Immune inflammation index in healthy adults: A large Multi-center Study from Western China. Clin. Lab. 65(3), 255–265 (2019).
Lopez, J. A. Introduction to a review series on platelets and cancer. Blood 137 (23), 3151–3152 (2021).
Zhang, X. et al. Research progress on the interaction between oxidative stress and platelets: Another avenue for cancer? Pharmacol. Res. 191, 106777 (2023).
Celik, H. et al. The relationship between platelet indices and ABO blood groups in healthy adults. J. Clin. Lab. Anal. 33 (3), e22720 (2019).
Dunbar, N. M., Ornstein, D. L. & Dumont, L. J. ABO incompatible platelets: Risks versus benefit. Curr. Opin. Hematol. 19 (6), 475–479 (2012).
Han, M. H. & Badami, K. G. ABO non-identical platelet transfusions, immune platelet refractoriness and platelet support. Brit J. Haematol. 204(5), 2097–2102 (2024).
Jacoub, K. & Al-Eisawi, Z. ABO blood group and skin cancers. Clin. Hemorheol. Micro. 81 (4), 359–371 (2022).
Hong, J. et al. Investigation on reference intervals and regional differences of platelet indices in healthy Chinese Han adults. J. Clin. Lab. Anal. 29 (1), 21–27 (2015).
Dunne, E. et al. Blood group alters platelet binding kinetics to Von Willebrand factor and consequently platelet function. Blood 133 (12), 1371–1377 (2019).
Ward, S. E., O’Sullivan, J. M. & O’Donnell, J. S. The relationship between ABO blood group, Von Willebrand factor, and primary hemostasis. Blood 136 (25), 2864–2874 (2020).
de Groot, P. & Munden, R. F. Lung cancer epidemiology, risk factors, and prevention. Radiol. Clin. N Am. 50 (5), 863–876 (2012).
Sun, Y. et al. Distribution of ABO blood groups among the 56 ethnic groups in China. Foreign Med. (Medical Geogr. Branch) 31(01), 22–25 (2010).
Dean, L. ABO Blood Group (Medical Genetics Summaries, 2012).
Acknowledgements
We sincerely acknowledge the dedicated efforts of the clinical department staff and information section personnel in collecting cancer-related data, without whom this research would not have been possible.
Funding
We conducted this research without funding support.
Author information
Authors and Affiliations
Contributions
H.L. and Y.Z. conceived and designed the study. T.Z. wrote this manuscript. T.Z. and H.L. searched database and reviewed studies. T.Z. performed data analysis and prepare the initial draft of the manuscript.H.Land M.X. helped in drafing the manuscript and critically reviewed the manuscript.J.D. and T.Z. participated in interpretation of data. H.Y., R.Z., L.R., P.Z., Y.W. and R.Y. conducted data collection. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The research related to human use has complied with all the relevant national regulations, institutional policies and follows the tenets of the Helsinki Declaration, and has been approved by the Institutional Ethics Committee of The Sichuan Cancer Hospital and Chengdu Fifth People’s Hospital. The Institutional Review Board (IRB) of the Sichuan Cancer Hospital approved this retrospective study (IRB code: SCCHEC-02-2021-064 ). The Institutional Review Board (IRB) of Chengdu Fifth People’s Hospital approved this retrospective study (IRB code: Ethical review 2023-036(science)-01). This retrospective study has been approved to waive informed consent by the Institutional Review Board of the Sichuan Cancer Hospital and Chengdu Fifth People’s Hospital.
Consent to participate
The study was a retrospective analysis and didn’t require the patient’s informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, T., Xiang, M., Yin, H. et al. Platelet indicators do not influence the impact of ABO blood groups on lung adenocarcinoma susceptibility. Sci Rep 15, 1131 (2025). https://doi.org/10.1038/s41598-024-82910-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-82910-w