Abstract
This study aimed to investigate the effects of chronic sympathoinhibition on glucose uptake by the myocardium and by the skeletal muscle in an animal model of obesity associated with leptin signaling deficiency. 6 obese Zucker rats (OZR) and 6 control Lean Zucker rats (LZR) were studied during basal conditions, chronic clonidine administration (30 days, 300 µg/kg), and washout recovery period. Glucose uptake in the myocardium and in the skeletal muscle was measured using positron emission tomography (PET) and 2-[18F] fluoro-2-deoxy-D-glucose ([18F]FDG). The standardized uptake value (SUV) corrected for blood glucose was used for the semi-quantitative analysis. Body weight, food and water intake, blood glucose concentration, blood pressure variability as an index of sympathetic activity and hemodynamic parameters such as mean arterial blood pressure (MAP), systolic blood pressure (SBP), diastolic blood pressure (DBP) and heart rate (HR) were analyzed. Myocardial glucose uptake was significantly lower during basal conditions in OZR versus LZR. In both OZR and LZR, chronic clonidine significantly reduced myocardial glucose uptake and hemodynamic variables (such as MAP, SBP, DBP, HR), and sympathetic activity (SA). [18F]FDG skeletal muscle uptake did not significantly differ in OZR versus LZR. Our findings indicate that cardiac glucose metabolism is reduced in obesity presumably in relation with the level of sympathetic activation.
Similar content being viewed by others
Introduction
Obesity is a major public health issue in both industrialized and developing nations and has been recently classified as the new major global epidemic1. Predictive studies conclude that > 50% of the world’s population will be overweight or obese by 2030 2,3,4. This epidemic is linked to a higher prevalence of comorbidities such as arterial hypertension, diabetes, insulin resistance, and dyslipidemia, which collectively form the metabolic syndrome and lead to a poor long-term prognosis5,6,7.
Recent studies suggest that pathological activation of the sympathetic nervous system (SNS) plays a crucial role in the development of metabolic syndrome. Various mediators, including hyperinsulinemia, angiotensin II, and adipokines like leptin, tumor necrosis factor-alpha, and interleukin-6, contribute to excessive SNS activation in obesity8,9. Leptin, a peptide hormone secreted by adipocytes in proportion to body fat, is particularly important in obesity-associated SNS activation and related conditions such as arterial hypertension10,11.
Leptin receptors are not only present in adipose tissue but also in peripheral organs like the heart, where they influence cardiac metabolism12. In obesity and diabetes, the heart’s mechanical efficiency is reduced due to metabolic remodeling, characterized by increased fatty acid uptake and oxidation and decreased glucose metabolism13,14. This shift leads to lipid accumulation, promoting cardiomyocyte apoptosis and contributing to cardiac dysfunction15.
The Obese Zucker Rat (fa/fa) (OZR) model, which mirrors human metabolic syndrome, demonstrates features such as obesity, hyperlipidemia, insulin resistance, and hypertension due to a genetic loss of leptin receptor function15,16,17,18,19. Previous studies have shown that increased sympathetic drive in obesity exacerbates metabolic alterations in the heart, reducing the efficiency of mechanical work and depleting key myocardial energy stores20,21. Clonidine, a sympatholytic agent, effectively reduces both systemic and cardiac sympathetic outflow, suggesting potential benefits for cardiac metabolism and function in obesity22,23,24,25.
The present study aimed to investigate the effects of sustained sympathoinhibition on cardiac glucose uptake in OZR and Lean Zucker Rats (LZR), thereby also exploring the role of central leptin signaling and its impact on cardiac metabolism. We hypothesize that clonidine -induced sympathoinhibition decreases myocardial glucose uptake and modulates systemic glucose levels, reflecting thus an improvement of the metabolic regulation in obesity. Positron emission tomography (PET) with (18)F-labeled glucose analog, 2-[18F] fluoro-2-deoxy-D-glucose ([18F] FDG) was used in our study to noninvasively and longitudinally quantify the glucose metabolism in the myocardium and skeletal muscle: before, during, and after central sympathoinhibition with clonidine.
Materials and methods
Study protocol
All experiments were performed in accordance with the European Directive 2010/63/EU on the Protection of Animals Used for Scientific Purposes, the European Convention for the Protection of Vertebrate Animals used for Experimental and other Scientific Purposes (Council of Europe No. 123, Strasbourg, 1985) and the National Institutes of Health Guide for the Care and Use of Laboratory Animals. The study was approved by the Research Ethics Committee of the “Grigore T. Popa” University of Medicine and Pharmacy, Iaşi. All experiments were conducted in accordance with the aforementioned guidelines and regulations, and in particular in accordance with the ARRIVE guidelines.
Male OZR (fa/fa) and their lean (fa/− and −/−) littermates (LZR) (36 weeks of age, Charles River Laboratories - Wilmington, MA, USA) were used to assess the effects of clonidine-induced sympathoinhibition on myocardial and skeletal muscle glucose metabolism. 6 OZR and 6 LZR were investigated during basal conditions, long-term clonidine administration, and a recovery period. Clonidine (300 µg/kg/day; Sintofarm S.A., Bucharest, Romania) was administered in the drinking water for 30 days in doses reported to induce sympathoinhibition as previously described25, while normal water was administered during basal conditions and the recovery period. The water intake was measured daily at 8 a.m. to ensure the appropriate administration, and the clonidine dosage was modified accordingly when necessary. Blood pressure and heart rate were continuously measured. Weekly measurements of body weight, food and water intake, and blood glucose were also recorded. Metabolic parameters from both OZR and LZR were averaged as follows: basal conditions - day 1 to day 6; clonidine administration - day 7 to day 33; recovery period - day 34 to day 46. The animals were fed a standard rodent diet. [18F] FDG (Monrol Europe S.R.L, București, Romania) was injected in the jugular vein (19–23 MBq in a solution of 0.2 mL) under isoflurane (2% in 100% oxygen) anesthesia.
Animal preparation
Rats were housed in a temperature (21–23 oC) and humidity-controlled environment with a 12-hour light/dark cycle (lights on at 8:00 and off at 20:00) with ad libitum access to food and water. All animals were housed in single cages to allow for precise control over water and food intake and to ensure consistent delivery of the drug during the experimental period. The animals were acclimatized for at least 3 weeks before the experimental protocols.
Continuous blood pressure recording
A telemetric system was used for continuous measurement of blood pressure as previously described25. Briefly, rats were anesthetized with a mixture of isoflurane (Anesteran, Rompharm Company, Srl., Otopeni, Romania) and room air (2–3% v/v) and placed on a heating pad to maintain body temperature at 36–37 °C during surgical procedures. The depth of anesthesia was verified by the abolition of tail-pinch and corneal reflexes. All surgical procedures were conducted under aseptic conditions using betadine and alcohol for skin scrubbing. Rats were administered tetracyclin (2 mg/mL in drinking water) for 3 days following surgery.
Placement of telemeters for continuous BP recording.
The implantation procedure for the telemeters involved midline abdominal and left inguinal incisions, as previously described25. The body of the telemetry transmitter (TRM54PB, Millar, Inc., Houston, TX) was sutured to the right flank of the inner abdominal wall with silk sutures (3 − 0, Ethicon, NJ). A 3 cm piece of PE90 polyethilene tubing (Intramedic, Becton Dickinson, MD) was guided from the left iliac fossa through a 1 mm incision of the abdominal muscle layer towards the inguinal area. The solid-state pressure sensor was tunneled through the tubing and advanced ~ 3 cm into the femoral artery with the pressure sensing tip in the aorta below the emergence of the renal arteries. The pressure sensor was secured with silk threads placed on the femoral artery and at the emergence from the abdominal wall. Incisions were closed with non-absorbable sutures (3 − 0 Prolene; Ethicon, NJ, United States) and antibiotic prophylaxis administered intraperitoneally for 72 h.
Continuous recording of BP waveform
Using a PowerLab 16/35 acquisition system (ADInstruments, Bella Vista, NSW, Australia), 24-h blood pressure waveforms from implanted telemeters were acquired continuously at a sampling frequency of 2000 Hz. TR181 smartpads (Millar, Inc., Houston, TX, United States) were used for both blood pressure signal acquisition and wireless charging of the implanted telemeters. Daily systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP) and heart rate (HR) were calculated from all 24-h individual cardiac cycles identified using LabChart built-in BP module (ADInstruments, Bella Vista, NSWLZ, Australia). Hemodynamic parameters from both OZR and LZR were averaged as follows: basal conditions—day 1 to day 6; clonidine administration - day 7 to day 33; recovery period - day 34 to day 46.
Estimation of sympathetic activity
As we previously described25,26,27, the original daily blood pressure (BP) signal sampled at 2000 Hz was analyzed in the frequency domain using the LabChart software based on the Fast Fourier Transform algorithm. Power spectra were calculated for all artifact-free segments ∼1 min in duration, overlapping by 50%, and windowed using a Hamming function, then averaged to generate daily BP spectra. Analysis of the direct BP signal was preferred over the extraction of cardiac cycle-related variables such as SBP, to avoid issues related to resampling for unequally spaced time-series. The frequency band between 0.25 and 0.75 Hz (low frequency, LF) contains BP oscillations originating from sympathetically driven variations in arterial vascular tone28. The power in this band was integrated and expressed as a percentage of the total power below the HR (0.01–3 Hz). BP oscillations from sympathetically driven variations in arterial vascular tone in both OZR and LZR were averaged as follows: basal conditions - day 1 to day 6; clonidine administration - day 7 to day 33; recovery period - day 34 to day 46.
Blood glucose measurements
Blood glucose concentration was measured from lateral tail vein pricks using an Accu-Chek glucose meter and test strips (Roche Diagnostics Corp., Indianapolis, IN) before and after the time of 18 F-FDG injection. Food was withdrawn in both OZR and LZR 18 h preceding the CT scans, which were performed after 15:00. The methodology and infrastructure of the laboratory did not allow the evaluation of various biological parameters such as insulin, fatty acids, and leptin.
Oral glucose tolerance test and Insulin tolerance test
Oral glucose tolerance test (OGTT) was completed by oral administration via gavage of glucose 40% (20 g glucose to 50mL tap water) in doses of 2 g/kg bw and blood glucose levels were measured during the first 120 min after glucose administration using glucose meter and test strips (Fora Diamond Prima, ForaCare Suisse AG) during control (day 5), clonidine administration (day 28) and clonidine washout (day 42).
Insulin tolerance test (ITT) was achieved by 0.75 UI/kg bw insulin (Humalog 100 units/ mL, Lilly) administration followed by seriate glucose measurements during the first 120 min after insulin administration using glucose meter and test strips (Fora Diamond Prima, ForaCare Suisse AG) during control (day 3), clonidine administration (day 25) and clonidine washout (day 40).
Area under the curve (AUC) for the OGTT and ITT
AUC was computed for the OGTT and ITT to assess quantitatively glucose metabolism and insulin sensitivity. This approach allows for the evaluation of dynamic changes over time and offers a more comprehensive perspective on intervention-induced differences between groups.
Rate pressure product (RPP)
RPP, an index of myocardial workload and oxygen demand, was calculated as the product between heart rate (HR) and systolic blood pressure (SBP). Thus, RPP provides a standardized measure of cardiac metabolic demand, allowing us to normalize the glucose uptake values and comparison across experimental conditions. To better interpret myocardial glucose uptake, we have normalized SUVglc values to RPP (Rate Pressure Product), a standard measure of myocardial workload.
Image acquisition
Rats were anesthetized using a mixture of isoflurane (Anesteran, Rompharm Company, Srl., Otopeni, Romania) and room air (2–3% v/v). Body temperature was continuously monitored before, during, and after the CT scan. All images were acquired on a GE Discovery PET/CT 710 scanner (GE Healthcare, Milwaukee,USA) with time-of-flight (TOF) capabilities on day 6 of the basal period, day 30 of the clonidine administration period, and day 43 of the recovery period. CT scans were performed using a standardized protocol involving 120 kV, auto mA, a tube-rotation time of 0.5 s per rotation, a pitch of 0.984, and a section thickness of 3.7 mm, matching the PET image section thickness. Immediately after the CT scan, PET was performed in the identical axial field of view. A single time-point acquisition was completed for 10 min and the images were reconstructed using the vendor-provided reconstruction VUE Point FX incorporating the SharpIR algorithm (3 iterations/24 subsets and a post-filtering of a 4 mm FWHM Gaussian in-plane and a [1:6:1] weighted axial filter). Image matrix was 256 × 256 with a pixel size of 2.73 mm.
Image analysis
The analysis of the PET-CT images was performed using CARIMAS (version 2.10) software published and freely distributed by the Turku PET Center, Finland and available at https://carimas.fi. CT scans were used as anatomical reference. To analyze the myocardial glucose uptake, heart images were reorientated into short-axis images. The polar maps have been generated automatically using short-axis slices of the left ventricle (LV) from PET images and unfolding them into a two-dimensional format. Each segment of the polar map corresponds to a specific region of the left ventricle, with the apex at the center and the base of the ventricle forming the outer edge. The color coding represents the intensity of [18F]FDG uptake, where typically blue areas indicate low glucose uptake and red areas indicate high glucose uptake, as depicted in Fig. 1.
Representative of standard reorientation of the heart into the short-axis images; short axis slices from apex to base and the corresponding polar map of myocardial [18F]FDG uptake. The images were generated and analyzed using Carimas 2.0 software available at https://carimas.fi.
To assess the glucose cardiac metabolism, the standardized uptake value (SUV) was calculated according to the formula:\(\:SUV=\frac{{C}_{t}}{{D}_{inj}\times{BW}^{-1}}\), where Ct = tissue radioactivity concentration; Dinj = injected dose; BW= body weight. Glucose correction was applied to the SUV values by normalizing to a value of 100 mg/dL, i.e. as glucose corrected SUV (SUVglc): SUVglc = SUVx gluc/ 100, where “gluc” is blood glucose concentration. SUVglc is reported only for the left ventricle. To analyze the skeletal muscle glucose uptake, a set of 2D ROIs were drawn on 10 consecutive axial slices at the level of the right tibialis muscles (anterior and posterior) on CT images. The 2D ROI sets were converted in 3D VOIs (237±61 mm3) and applied on all fused PET/CT images.
Statistical analysis
All statistical analyses were performed using IBM SPSS Statistics for Windows, version 26 (IBM Corp., Armonk, N.Y., USA) and R. All data are reported as mean ± standard deviation. Statistical significance between the three conditions was determined by two-way repeated measures ANOVA with post-hoc analyses using the Bonferroni multiple comparison correction. The Wilk’s lambda test was applied to verify if the explanatory variables had different means. Differences between the means were considered statistically significant if p < 0.05. Pearson’s coefficient (r-value) analysis was performed, with differences considered significant at p < 0.05 and − 0.50 > r > 0.50.
Results
Metabolic parameters during basal conditions, clonidine administration and recovery period
During basal conditions, OZR showed significantly higher body weight, food, and water intake (p < 0.05) compared with LZR. During the recovery period, only food and water intake increased significantly over basal values in both OZR and LZR. No statistically significant differences were found in blood glucose levels or skeletal muscle glucose uptake between OZR and LZR. Sympathetic inhibition led to a significant decrease in the body weight, food intake, and global myocardial glucose uptake in both groups as shown in Table 1. Skeletal muscle glucose uptake followed the same tendency but did not reach statistical significance in all experimental settings. Changes in metabolic parameters during different experimental intervals are summarized in Table 1.
Hemodynamic parameters during basal, sympatholytic therapy and recovery periods
During basal conditions, OZR had significantly increased MAP, SBP, DBP, and high levels of estimated sympathetic activity compared with LZR. No significant differences in HR were observed between OZR and LZR. As expected, clonidine administration led to a significant decrease in MAP, SBP, and DBP in both groups. Additionally, clonidine administration led to significant sympathoinhibition, as indicated by the reduction of the sympathetically mediated oscillations of BP in the low-frequency (LF) band and bradycardia in both OZR and LZR. All hemodynamic parameters returned to basal values after the cessation of clonidine. Changes in hemodynamic parameters during experimental settings are summarized in Fig. 2 (Mean Arterial Blood Pressure), Fig. 3 (Heart Rate) and Table 2.
When evaluating heart rate together with cardiac glucose uptake, we found a positive correlation in the LZR group (r = 0.55, p = 0.025), while this was not statistically significant in OZR group (p = 0.122).
Dynamic glucose regulation during basal conditions, clonidine administration and recovery period
Oral glucose tolerance test (OGTT)
The OGTT was used to assess glucose regulation across experimental conditions. This test highlights the differences in glucose uptake and metabolic flexibility between OZR and LZR groups under basal, clonidine induced sympathoinhibition and recovery periods. As shown in Fig. 4, in OZR, the glucose levels are higher at all time points when compared to LZR, indicating impaired glucose tolerance. Between 15 and 45 min, glucose levels increase in all groups, but in the control group a higher peak can be observed compared to clonidine administration and clonidine washout. Between 45 and 120 min, glucose levels return towards baseline levels in all groups with clonidine administration and clonidine washout showing a more rapid decline. In LZR, no significant differences were observed between groups during baseline. At 15 min, significant differences were observed between control, clonidine administration and clonidine washout. Over time, glucose levels decrease, with clonidine administration showing a faster return to baseline. In conclusion, during clonidine administration, OZR demonstrated a more controlled glucose rise and a faster return to baseline compared to basal conditions, indicating improved glucose metabolism. In contrast, LZR showed minimal differences at baseline, but clonidine administration also led to a faster normalization of glucose levels.
Graphical representation of the statistical differences of the OGTT in Obese Zucker rats (OZR – upper panel) and Lean Zucker rats (LZR- lower panel) during basal, clonidine administration and clonidine washout over time; * = p < 0.0001 in OZR Control versus Recovery and Clonidine versus Recovery at 15 min; * = p < 0.0001 in LZR Control versus Recovery at 15 min, Control versus Clonidine at 60 min and Control versus Recovery at 120 min; n = 6.
Insulin tolerance test (ITT)
ITT was performed to evaluate the insulin-mediated glucose disposal measuring thus the rate at which blood glucose levels decrease following insulin administration, providing insights into insulin sensitivity. As depicted in Fig. 5, in OZR, between 15 and 30 min, control groups shows a more significant decrease in glucose levels compared to clonidine administration and clonidine washout. Up to 120 min, glucose levels gradually return, with clonidine administration showing a steadier response. In LZR, in the 15–30 time interval, control groups shows a more significant decrease in glucose levels compared to clonidine administration and clonidine washout. Up to 120 min, glucose levels gradually return and a steadier response as in the case of OZR was observed with clonidine administration. In conclusion, OZR showed a less pronounced glucose reduction during baseline conditions, suggesting a reduced insulin sensitivity. Clonidine induced sympathoinhibition resulted in a steadier decline in glucose levels and a faster return to baseline compared to basal conditions, suggesting improved insulin sensitivity. Similarly, LZR exhibited consistent glucose responses, with clonidine administration leading to a more stable glucose decline.
Graphical representation of the statistical differences of the ITT in Obese Zucker Rats (OZR-upper panel) and Lean Zucker Rats (LZR-lower panel) during basal, clonidine administration and clonidine washout over time. * = p < 0.0001 in OZR Control versus Recovery at 45 min; * = p < 0.0001 in OZR Clonidine versus Recovery at 90 min; * = p < 0.0001 in LZR Control versus Clonidine at 120 min; n = 6.
Area Under the Curve for the OGTT and ITT
AUC for OGTT and ITT showed significant differences in glucose metabolism and insulin sensitivity between OZR and LZR across all experimental phases. As depicted in Figs. 6 and 7 (AUC-OGTT during control) significant differences between OZR and LZR in glucose levels were observed with higher AUC for the OZR. This may suggest impaired glucose tolerance in OZR when compared to LZR. During clonidine treatment, a significant improvement in glucose metabolism is observed with AUC decreasing significantly in OZR which indicate improved glucose tolerance and potentially improved insulin sensitivity, as suggested also by AUC-ITT. During recovery phase, a partial regression toward baseline for both OZR and LZR may be observed. As depicted in Figs. 6 and 7 (lower panel AUC-ITT) during control phase, OZR shows significantly reduced glucose clearance compared to LZR suggesting insulin resistance. Both OZR and LZR improved glucose clearance during clonidine-induced sympathoinhibition with a more substantial improvement in OZR which may indicate an improved insulin sensitivity in this group. During recovery phase, glucose clearance decreased when compared to clonidine-induced sympathoinhibition but remains better than control suggesting some lasting effects of clonidine on insulin sensitivity.
Area Under the Curve for the OGTT (upper panel) and ITT (bottom panel) in Obese Zucker Rats (OZR) versus Lean Zucker Rats (LZR) during basal, clonidine administration and clonidine washout over time. Upper Panel – AUC for OGTT: * = p < 0.0001 OZR versus LZR in Control at 15,30,45,60 and 90 min; * = p < 0.0001 OZR versus LZR in Clonidine at 45, 60, 90 and 120 min; * = p < 0.0001 OZR versus LZR in Recovery; Lower Panel – AUC for ITT: * = p < 0.0001 OZR versus LZR in Control between 15–120 min time interval; * = p < 0.0001 OZR versus LZR in Clonidine at 30, 90, 120 min; * = p < 0.0001 OZR versus LZR in Recovery at 15, 30, 45 min. Values are the mean ± SEM and n = 6.
Graphical representation of the statistical differences of the AUC-OGTT (upper panel) and AUC-ITT (lower panel) in Obese Zucker Rats (OZR) and Lean Zucker Rats (LZR) during control, clonidine administration and clonidine washout over time. Upper panel: AUC-OGTT OZR * = p < 0.0001 in OZR Control versus Recovery at 30 min; * = p < 0.0001 in OZR Clonidine versus Recovery at 60 min; * = p < 0.0001 in OZR Control versus Recovery at 90 min; AUC-OGTT LZR: * = p < 0.0001 in LZR control versus Recovery and Clonidine versus Recovery at 15 min; * = p < 0.0001 in LZR Clonidine versus Recovery at 30 min; * = p < 0.0001 in LZR Control versus Clonidine at 45, 60, 90 and 120 min; n = 6.
Cardiac glucose uptake and RPP normalization during basal, sympatholytic therapy and recovery periods
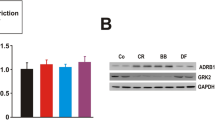
LV whole SUVglc was significantly decreased in OZR compared with LZR at baseline (1.62 ± 0.73 vs. 4.95 ± 2.02 g/ml, p < 0.04). During clonidine administration, a significant reduction of 32.7% in cardiac glucose uptake was observed in OZR (1.62 ± 0.73 vs. 1.09 ± 0.29, p < 0.05) and a 50% reduction in LZR (4.95 ± 2.02 vs. 2.50 ± 1.52, p < 0.05), as shown in the Fig. 8 and Supplementary Fig. 1. Moreover, the calculated RPP (Table 1) support the hypothesis that clonidine administration reduces myocardial workload in both OZR and LZR, reflecting thus a decreased cardiac energy demands.
Global Myocardial SUVglc in OZR and LZR during basal, clonidine administration and clonidine washout * = p < 0.05 in OZR Control versus Clonidine; * = p < 0.05 in OZR Clonidine versus Recovery; * = p < 0.05 in OZR Control versus Recovery; * = p < 0.05 in LZR Control versus Clonidine; * = p < 0.05 in LZR Clonidine versus Recovery; * = p < 0.05 in OZR Control versus Recovery; Values are the mean ± SEM and n = 6; blue colour = basal conditions; red colour= clonidine administration; yellow colour = recovery;
Discussion
Our study aimed to investigate the impact of chronic sympathoinhibition on cardiac glucose uptake in OZR and LZR, focusing on the implications of leptin signaling and sympathetic activity. Our findings provide insights into the metabolic adaptations in obesity and the impact of clonidine-induced sympathoinhibition on myocardial metabolism and dynamics of systemic glucose regulation.
Cardiac metabolism and energy demand
In the normal adult heart, 50–70% of ATP is obtained from fatty acids ß-oxidation while the rest of 10–40% of energy is obtained from the oxidation of pyruvate resulting from glycolysis and lactate oxidation 29,30, –31. The heart fatty acids ß-oxidation is a dynamic process and is under the influence of various factors such as the presence of competing energy substrates, energy demand and fatty acids supply to the heart32. During physiological conditions, the heart can shift its metabolism from fat to carbohydrate utilization in stressful conditions such as hypoxia, increased cardiac workload or after a carbohydrate-rich meal. Our results show that at baseline, OZR exhibited significantly lower myocardial glucose uptake than LZR (1.62 ± 0.73 vs. 4.95 ± 2.02 SUVglc g/mL) although the cardiac workload is significantly increased in OZR compared to LZR as shown by RPP (50,700 bpm*mmHg in OZR vs. 45,560 bpm*mmHg in LZR). This finding highlights the metabolic inflexibility in substrate utilizations in obesity, where the heart relies predominantly on fatty acids. Contributing factors may include elevated serum free fatty acids, impaired insulin signaling, and decreased glucose transporter activity. Our results align with other reports showing that increased serum free fatty acids and fatty acid uptake in OZR result in reduced cardiac glucose utilization14,33.
Chronic administration of clonidine significantly reduced myocardial glucose uptake in both OZR and LZR. In OZR, cardiac glucose uptake decreased by 32.7% (from 1.62 ± 0.73 to 1.09 ± 0.29 SUVglc g/mL), while in LZR, it decreased by 50% (from 4.95 ± 2.02 to 2.50 ± 1.52 SUVglc g/mL). This reduction was accompanied by a significant decrease in body weight and food intake which may indicate a reduced in both systemic and myocardial energy demands rather than an impaired metabolism. Moreover, the reductions in RPP during clonidine administration confirm its role in alleviating myocardial workload in both OZR and LZR. This effect associates with reduced sympathetic drive, as indicated by decreases in heart rate and systolic blood pressure. Notably, RPP remained lower in the recovery phase compared to basal, suggesting thus a sustained effect of clonidine on cardiac energy demands. The normalization of SUVglc to RPP revealed that the reduced myocardial glucose uptake observed during clonidine administration reflects a decrease in cardiac energy demands rather than glucose metabolic impairment. In OZR, normalized SUVglc decreased significantly from basal to clonidine, consistent with the decrease of both heart rate and systolic blood pressure during clonidine treatment. A similar trend was observed in LZR, highlighting the general effect of sympathoinhibition on myocardial workload. These findings underline the adaptive nature of reduced glucose uptake during sympathoinhibition, aligning with the decreased oxygen and energy requirements of the myocardium under reduced sympathetic drive. The partial recovery of normalized SUVglc after clonidine interruption may reflect a dynamic response to changes in sympathetic activity.
On the other hand, the clonidine induced reduction in sympathetic tone can decrease basal metabolic rate and thermogenesis, as well as lower catecholamine-driven lipolysis. Clonidine’s interaction with imidazoline receptors, particularly in the hypothalamus, has been linked to appetite suppression and an improved glucose homeostasis. Activation of these receptors may modulate the autonomic control of feeding behaviors and glucose metabolism, leading to decreased food intake and improved insulin sensitivity, both of which contribute to weight loss. These changes suggest that the combined alpha-adrenergic and imidazoline receptor effects act synergistically to alter energy balance and metabolic regulation. Notably, these findings align with previous studies demonstrating clonidine’s ability to influence central mechanisms governing energy homeostasis8,34.
By reducing sympathetic activity, clonidine decreases cardiac workload and glucose turnover. In LZR, this response likely enhances metabolic efficiency, while in OZR, it exposes the heart’s dependence on fatty acids and limited glycolytic capacity. Our findings suggest that obesity-driven metabolic remodeling shifts cardiac energy reliance from glucose to fatty acids, a process most probably exacerbated by elevated serum free fatty acids and impaired insulin action. Although clonidine reduces myocardial glucose uptake, it simultaneously alleviates metabolic stress by reducing cardiac energy demands. These results may reflect the dual role of clonidine: promoting energy efficiency and revealing underlying metabolic inflexibility in obesity.
Role of skeletal muscles in glucose homeostasis
Interestingly, while clonidine significantly reduced cardiac glucose uptake, it did not significantly alter skeletal muscle glucose uptake in either OZR or LZR. This finding is consistent with prior evidence showing that skeletal muscle glucose uptake is largely determined by insulin-dependent mechanisms, which were not the primary focus of this study35. Clonidine’s effects on systemic glucose levels and myocardial glucose uptake are more likely mediated by reductions in sympathetic activity, rather than direct modulation of skeletal muscle glucose metabolism. The decline in systemic glycemia during sympathoinhibition, despite stable skeletal muscle SUVglc, suggests that skeletal muscle plays a limited role in this reduction.
The impact of sympathoinhibition on glucose regulation
The observed decline in blood glucose levels during clonidine administration, as demonstrated by both basal measurements and dynamic glucose tolerance tests (i.e. OGTT, ITT, AUC-OGTT and AUC-ITT), highlights the impact of sympathoinhibition on systemic glucose regulation. In both OZR and LZR, blood glucose levels decreased significantly during clonidine treatment, with partial recovery observed during recovery phase. This suggests improved glucose tolerance and potentially enhanced insulin sensitivity due to clonidine treatment. Clonidine-induced sympathoinhibition has been shown to enhance systemic insulin sensitivity, likely through reduced adrenergic stimulation of hepatic and peripheral tissues36. This would lead to increased glucose disposal in insulin-sensitive tissues such as adipose tissue and may explain the decline in systemic glucose levels during clonidine treatment. Specifically, OZR exhibited a faster return to baseline glucose levels after glucose administration during clonidine treatment compared to basal conditions, indicating improved glucose disposal dynamics. Similarly, ITT results revealed that clonidine administration enhanced the rate of glucose clearance, particularly in OZR, where insulin resistance is probably more pronounced. When analyzing AUC for OGTT and ITT, significant statistically differences were also found in glucose metabolism and insulin sensitivity between OZR and LZR groups across all experimental phases. During control, OZR exhibited impaired glucose tolerance and reduced glucose clearance compared to LZR, reflecting baseline metabolic dysfunction. During clonidine-induced sympathoinhibition, both groups showed significant improvements in glucose tolerance and insulin sensitivity, as evidenced by reduced AUC values for OGTT and increased glucose clearance during ITT, with a more pronounced effect in OZR. These findings suggest that sympathoinhibition enhances glucose-insulin dynamics by mitigating sympathetic overactivity. Partial regression toward baseline values was observed in both groups during recovery. However, the glucose-insulin dynamics remained significantly improved than in the control phase, indicating some lasting benefits of clonidine treatment. These results underline the potential of targeting the sympathetic nervous system to improve metabolic flexibility and manage glucose-insulin dysregulation, particularly in obesity-related conditions.
Another mechanisms explaining the decline in systemic glucose levels may be suppression of the hepatic gluconeogenesis and glycogenolysis by reducing adrenergic signaling to the liver, a well-documented pathway in metabolic regulation during sympathoinhibition37,38,39. Although not directly explored in this study, clonidine may also modulate pancreatic beta-cell activity, enhancing insulin secretion or suppressing glucagon release and explain thus the reduced systemic glucose levels40. Interestingly, in LZR, although there are no baseline differences, clonidine administration results in a more controlled glucose rise and quicker return to baseline, similar to the fat rats as shown by OGTT. This indicates that clonidine may have a beneficial effect on glucose metabolism regardless of obesity status. Our results suggest that clonidine administration improve glucose tolerance and insulin sensitivity in both OZR and LZR. Taken together, these findings suggest that clonidine may have potential therapeutic benefits for managing glucose metabolism in obesity.
Potential mechanisms related to leptin signaling
Experimental data show that leptin may act as a critical link between obesity and associated comorbidities such as arterial hypertension through the activation of the sympathetic nervous system41,42. In obesity-hypertension, it has been shown that leptin increases the sympathetic outflow to the kidneys, skeletal muscle vasculature and adrenal glands through centrally acting mechanisms via the arcuate nucleus of the hypothalamus43. Animal studies focusing on acute effects of the leptin administration into hypothalamus have showed an increased glucose uptake within skeletal muscle, brown adipose tissue and heart44,45 probably mediated by a beta-adrenergic mechanism for the sympathetic nerves innervating peripheral tissues46. The involvement of the sympathetic nervous system as the modulator of the central leptin effects is still a topic of debate since the central-induced cardioprotective effects are not dependent on intact cardiac sympathetic innervation, as reported by other studies47.
Most of the various differences between LZR and OZR may result from the leptin signaling deficiency in OZR. Leptin deficiency or resistance in OZR is associated with a shift from glucose to fatty acid utilization, contributing to metabolic inflexibility and cardiac dysfunction through various mechanism such as fibrosis, vascular dysfunction, increased inflammation, and impaired heart metabolism48,49. Interestingly, a metabolic switch from glucose to free fatty acids utilization was described in leptin or leptin-receptors deficient rodent models leading to impairment of cardiac function due to cardiac lipotoxicity, but the precise mechanisms responsible for this alterations are still controversial48. Conversely, leptin may decrease the transport of fatty acids across the cardiomyocyte membrane, reducing lipid-mediated apoptosis and protecting cardiac function in obesity51,52. Further studies are necessary to dissect between the central and peripheral effects of leptin signaling on cardiac metabolism.
Conclusions
These results advance current knowledge by elucidating how excessive sympathetic nervous system activity in obesity may impair cardiac glucose utilization and systemic glucose dynamics. The use of clonidine to chronically inhibit sympathetic activity and its subsequent effect in further decreasing cardiac glucose uptake highlights a potential therapeutic avenue for addressing cardiac metabolic dysfunction in obesity. Our results may pave the way to understand the physiopathology of cardiac metabolism in obesity and also offer new therapeutic insights into managing glucose intolerance and insulin resistance, which are known to be critical components of metabolic syndrome and cardiovascular diseases. The significant reduction in myocardial glucose uptake in OZR compared to LZR under basal conditions highlights a critical metabolic inflexibility in the obese state, possible driven by leptin signaling deficiency. As we have discussed right above, leptin signaling may well be the correct molecular key that explains many of the various but correlated differences between OZR and LZR, so that leptin may therefore explain even certain mechanisms of obesity and its comorbidities in humans. The practical value of the present experimental study lies in its potential implications for understanding the interplay between sympathetic activity and cardiac metabolism in obesity. Our results suggest that targeting sympathetic overactivity could provide therapeutic benefits by restoring metabolic flexibility and reducing cardiovascular risks associated with obesity.
Limitations
A limitation of our study consists in the technique used for estimating sympathetic activity in OZR. While the use of low frequency blood pressure oscillations is a validated technique for lean rats, there is no consistent data in literature that confirms that this technique could be applied to obese rats. Nonetheless, the observation of a similar trend in decreased blood pressure variability—used in this study as a surrogate marker for sympathetic activity—following clonidine administration in both OZR and LZR encouraged us to include low-frequency blood pressure oscillation measurements in our study and strengthened our confidence in the results. Another limitation of this study is the absence of an experimental group representing simple obesity without leptin signaling deficiency. This limits our ability to differentiate between the effects of leptin resistance and those of general obesity on cardiac metabolism. Future studies will include such a group to disentangle these mechanisms. Another limitation of the study comes from the lack of data regarding leptin, insulin and fatty acid measurements in both LZR and OZR. Therefore, the complete mechanisms that might influence the glucose uptake were not fully evaluated. Further studies which also integrate metabolic markers as well as evaluating the liver involvement in cardiac glucose metabolism are needed to validate the data found in our research.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Tiwari, A. & Balasundaram, P. In StatPearls (StatPearls Publishing, Treasure Island, 2024).
Sarma, S., Sockalingam, S. & Dash, S. Obesity as a multisystem disease: Trends in obesity rates and obesity-related complications. Diabetes Obes. Metab. 23 (Suppl 1), 3–16 (2021).
Loos, R. J. F. & Yeo, G. S. H. The genetics of obesity: From discovery to biology. Nat. Rev. Genet. 23, 120–133 (2022).
James, W. P. T. & Obesity A global public health challenge. Clin. Chem. 64, 24–29 (2018).
Landsberg, L. et al. Obesity-related hypertension: Pathogenesis, cardiovascular risk, and treatment–a position paper of the the Obesity Society and the American Society of Hypertension. Obes. (Silver Spring). 21, 8–24 (2013).
Grundy, S. M. Metabolic syndrome update. Trends Cardiovasc. Med. 26, 364–373 (2016).
Shariq, O. A. & McKenzie, T. J. Obesity-related hypertension: A review of pathophysiology, management, and the role of metabolic surgery. Gland Surg. 9, 80–93 (2020).
Thorp, A. A. & Schlaich, M. P. Relevance of sympathetic nervous system activation in obesity and metabolic syndrome. J. Diabetes Res. 341583 (2015). (2015).
Mahfoud, F. et al. Effect of renal sympathetic denervation on glucose metabolism in patients with resistant hypertension: A pilot study. Circulation 123, 1940–1946 (2011).
Hall, J. E. et al. Obesity-induced hypertension: Role of sympathetic nervous system, leptin, and melanocortins. J. Biol. Chem. 285, 17271–17276 (2010).
Yu, B. & Cai, D. Neural programmatic role of leptin, TNFα, Melanocortin, and glutamate in blood pressure regulation vs obesity-related hypertension in male C57BL/6 mice. Endocrinology 158, 1766–1775 (2017).
Green, E. D. et al. The human obese (OB) gene: RNA expression pattern and mapping on the physical, cytogenetic, and genetic maps of chromosome 7. Genome Res. 5, 5–12 (1995).
Boudina, S. & Abel, E. D. Diabetic cardiomyopathy revisited. Circulation 115, 3213–3223 (2007).
Lopaschuk, G. D., Folmes, C. D. L. & Stanley, W. C. Cardiac energy metabolism in obesity. Circ. Res. 101, 335–347 (2007).
Sharma, S. et al. Intramyocardial lipid accumulation in the failing human heart resembles the lipotoxic rat heart. FASEB J. 18, 1692–1700 (2004).
Wong, S. K., Chin, K. Y., Suhaimi, F. H., Fairus, A. & Ima-Nirwana Animal models of metabolic syndrome: A review. Nutr. Metab. (Lond). 13, 65 (2016).
Chentouf, M. et al. Excessive food intake, obesity and inflammation process in Zucker fa/fa rat pancreatic islets. PLoS One. 6, e22954 (2011).
Iliescu, R. & Chade, A. R. Progressive renal vascular proliferation and injury in obese Zucker rats. Microcirculation 17, 250–258 (2010).
Chatham, J. C. & Seymour, A. M. L. Cardiac carbohydrate metabolism in Zucker diabetic fatty rats. Cardiovasc. Res. 55, 104–112 (2002).
Bussey, C. T., Thaung, H. P. A., Hughes, G., Bahn, A. & Lamberts, R. R. Cardiac β-adrenergic responsiveness of obese Zucker rats: The role of AMPK. Exp. Physiol. 103, 1067–1075 (2018).
Fragasso, G. Deranged cardiac metabolism and the pathogenesis of heart failure. Card Fail. Rev. 2, 8–13 (2016).
Azevedo, E. R., Newton, G. E. & Parker, J. D. Cardiac and systemic sympathetic activity in response to clonidine in human heart failure. J. Am. Coll. Cardiol. 33, 186–191 (1999).
Chernow, B., Lake, C. R., Zaloga, G. P., Coleman, M. D. & Ziegler, M. G. Effect of clonidine on sympathetic nervous system activity in patients with essential hypertension. Int. J. Clin. Pharmacol. Res. 3, 9–15 (1983).
Aggarwal, A., Esler, M. D., Morris, M. J., Lambert, G. & Kaye, D. M. Regional sympathetic effects of low-dose clonidine in heart failure. Hypertension 41, 553–557 (2003).
Tudorancea, I. et al. Reduced renal Mass, Salt-Sensitive hypertension is resistant to renal denervation. Front. Physiol. 9, 455 (2018).
Iliescu, R., Tudorancea, I., Irwin, E. D. & Lohmeier, T. E. Chronic baroreflex activation restores spontaneous baroreflex control and variability of heart rate in obesity-induced hypertension. Am. J. Physiol. Heart Circ. Physiol. 305, H1080–H1088 (2013).
Tudorancea, I. et al. The impact of renal denervation on the baroreflex control of hert rate in an experimental model of reduced renal mass, salt sensitive hypertension. Med. Surg. J. – Rev. Med. Chir. Soc. Med. Nat. 122, 558–569 (2018).
Oliveira-Sales, E. B., Toward, M. A., Campos, R. R. & Paton, J. F. R. revealing the role of the autonomic nervous system in the development and maintenance of Goldblatt hypertension in rats. Auton. Neurosci. 183, 23–29 (2014).
Karwi, Q. G., Uddin, G. M., Ho, K. L. & Lopaschuk, G. D. loss of metabolic flexibility in the failing heart. Front. Cardiovasc. Med. 5, 68 (2018).
Stanley, W. C., Recchia, F. A. & Lopaschuk, G. D. Myocardial substrate metabolism in the normal and failing heart. Physiol. Rev. 85, 1093–1129 (2005).
Lopaschuk, G. D., Ussher, J. R., Folmes, C. D. L., Jaswal, J. S. & Stanley, W. C. Myocardial fatty acid metabolism in health and disease. Physiol. Rev. 90, 207–258 (2010).
Stanley, W. C. & Chandler, M. P. Energy metabolism in the normal and failing heart: Potential for therapeutic interventions. Heart Fail. Rev. 7, 115–130 (2002).
Young, M. E. et al. Impaired long-chain fatty acid oxidation and contractile dysfunction in the obese Zucker rat heart. Diabetes 51, 2587–2595 (2002).
Tran, L. T. et al. Hypothalamic control of energy expenditure and thermogenesis. Exp. Mol. Med. 54, 358–369 (2022).
Sylow, L., Tokarz, V. L., Richter, E. A. & Klip, A. The many actions of insulin in skeletal muscle, the paramount tissue determining glycemia. Cell. Metab. 33, 758–780 (2021).
Giugliano, D. et al. Hemodynamic and metabolic effects of transdermal clonidine in patients with hypertension and non-insulin-dependent diabetes mellitus. Am. J. Hypertens. 11, 184–189 (1998).
Rui, L. Energy metabolism in the liver. Compr. Physiol. 4, 177–197 (2014).
Püschel, G. P. Control of hepatocyte metabolism by sympathetic and parasympathetic hepatic nerves. Anat. Rec Discov Mol. Cell. Evol. Biol. 280, 854–867 (2004).
Nonogaki, K. New insights into sympathetic regulation of glucose and fat metabolism. Diabetologia 43, 533–549 (2000).
Nilsson, T., Arkhammar, P., Rorsman, P. & Berggren, P. O. Inhibition of glucose-stimulated insulin release by alpha 2-adrenoceptor activation is parallelled by both a repolarization and a reduction in cytoplasmic free Ca2 + concentration. J. Biol. Chem. 263, 1855–1860 (1988).
Bell, B. B. & Rahmouni, K. Leptin as a mediator of obesity-Induced Hypertension. Curr. Obes. Rep. 5, 397–404 (2016).
Kshatriya, S. et al. Obesity hypertension: The regulatory role of leptin. Int J Hypertens 270624 (2011). (2011).
Russo, B., Menduni, M., Borboni, P., Picconi, F. & Frontoni, S. Autonomic nervous system in obesity and insulin-resistance-the Complex interplay between Leptin and Central Nervous System. Int. J. Mol. Sci. 22, (2021).
Kamohara, S., Burcelin, R., Halaas, J. L., Friedman, J. M. & Charron, M. J. Acute stimulation of glucose metabolism in mice by leptin treatment. Nature 389, 374–377 (1997).
Minokoshi, Y., Haque, M. S. & Shimazu, T. Microinjection of leptin into the ventromedial hypothalamus increases glucose uptake in peripheral tissues in rats. Diabetes 48, 287–291 (1999).
Haque, M. S. et al. Role of the sympathetic nervous system and insulin in enhancing glucose uptake in peripheral tissues after intrahypothalamic injection of leptin in rats. Diabetes 48, 1706–1712 (1999).
Omoto, A. C. M. et al. Central nervous system actions of Leptin improve cardiac function after Ischemia-Reperfusion: Roles of sympathetic innervation and sex differences. J. Am. Heart Assoc. 11, e027081 (2022).
Poetsch, M. S., Strano, A. & Guan, K. Role of leptin in cardiovascular diseases. Front. Endocrinol. (Lausanne). 11, 354 (2020).
Vilariño-García, T. et al. Role of leptin in obesity, cardiovascular disease, and type 2 diabetes. Int. J. Mol. Sci. 25, (2024).
Burcelin, R. et al. Acute intravenous leptin infusion increases glucose turnover but not skeletal muscle glucose uptake in ob/ob mice. Diabetes 48, 1264–1269 (1999).
Hall, M. E., Harmancey, R. & Stec, D. E. Lean heart: Role of leptin in cardiac hypertrophy and metabolism. World J. Cardiol. 7, 511–524 (2015).
Unger, R. H. Minireview: Weapons of lean body mass destruction: The role of ectopic lipids in the metabolic syndrome. Endocrinology 144, 5159–5165 (2003).
Author information
Authors and Affiliations
Contributions
Conceptualization: Ionuț Tudorancea and Radu Iliescu; Methodology: Ionuț Tudorancea, Radu Iliescu, Ionela Lăcrămioara Șerban, Dragomir Șerban, Irina-Iuliana Costache-Enache, Alexandru Grațian Naum, Cătălin Caratașu; Software: Alexandru Grațian NaumValidation: Ionuț Tudorancea, Radu Iliescu; Ionela Lăcrămioara Șerban, Dragomir Șerban, Irina-Iuliana Costache-Enache, Alexandru Grațian NaumInvestigation: Ionuț Tudorancea, Radu Iliescu; Data curation: Ionuț Tudorancea, Radu Iliescu; Ionela Lăcrămioara Șerban, Dragomir Șerban, Irina-Iuliana Costache-Enache, Alexandru Grațian Naum, Cătălin Caratașu; Writing—original draft preparation: Ionuț Tudorancea; writing—review and editing: Ionuț Tudorancea, Radu Iliescu; Visualization: Ionuț Tudorancea, Radu Iliescu; Ionela Lăcrămioara Șerban, Dragomir Șerban, Irina-Iuliana Costache-Enache, Alexandru Grațian Naum, Cătălin Caratașu; Project administration: Ionuț Tudorancea, Radu Iliescu.All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Institutional review board statement
The animal study protocol was approved by Ethics Committee of “Grigore T. Popa” University of Medicine and Pharmacy.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tudorancea, I., Șerban, I.L., Șerban, D.N. et al. Sympathetic nervous system inhibition enhances cardiac metabolism and improves hemodynamics and glucose-insulin dynamics in obese and lean rat models. Sci Rep 15, 503 (2025). https://doi.org/10.1038/s41598-024-84218-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-84218-1