Abstract
Ventral curvature (VC), and penile straightening is a key step in severe proximal hypospadias surgery. One of the most important variables in selecting the appropriate technique for primary severe hypospadias repair seems to be the urethral plate transection to achieve penile straightening. In some cases, cutting the urethral plate is not sufficient and VC is corrected with ventral corporotomies. In the presented study, it was aimed to evaluate the early results of patients who underwent urethral plate transsection (UPT). Thirty-two cases with severe proximal hypospadias who underwent chordee correction by transsection of the urethral plate between 2019 and 2022 years were evaluated retrospectively. The patients’ ages varied between 8 months and 16 years, with a mean age of 4.61 ± 4.10 years. Ventral curvature was below 90 degrees in 6 patients and above 90 degrees in 26 patients. Penile curvature was corrected by plate transection in 9 children (28.2%) and plate transection combined with ventral corporotomies in 23 children (71.8%). Bracka operation was performed on 8 cases, Duckett operation on 1 case, STAG operation on 8 cases, and STAC operation on 15 cases. We noted recurrence of curvature in 7 children (Bracka 3, STAG 2, STAC 2) which required dorsal plication during the urethroplasty. Second/third stage was completed in all children. Success, hematoma, fistula, meatal stricture, glanuler dehisence, graft stricture rates determined to be 53.2%, 6.25%, 12.5%, 12.5%, 6.25% and 9.37% respectively. Staged procedures give the oppurtunity to correct the residuel or recurrence curvature before urethroplasty. Follow up is important to address long term functional results of ventral corporotomies.
Similar content being viewed by others
Introduction
Surgical treatment of patients with proximal hypospadias continues to challenge pediatric urologists despite all developments. Although several surgical techniques have been described, there is no consensus on the ideal treatment option. Straightening maneuvers in curvature up to 30 degrees can be corrected by dorsal plication directly opposite the area of greatest bending. Nevertheless, optimal management of VC greater than 30 degrees remains uncertain. Multiple plications using 5 − 0 to 4 − 0 polypropylene are described, although concerns for both recurrent curvature and loss of penile length increase when more than one plication is performed1. Persistent or recurrent VC was found in most patients presenting after failed proximal hypospadias repair, which most often indicated failure of the initial straightening procedure. This was significantly more likely after ’chordee excision’ or dorsal plication than with ventral lenghtening, and when the urethral plate was conserved.
In cases where the chordee persists after excision of all fibrotic structures, the urethral plate is transected. Urethral plate transection could make penile straightening more effective1. In some cases, transection of the urethral plate is not sufficient and the penis is tried to be straightened with ventral corporotomy.
Studies regarding severe proximal hypospadias where the urethral plate has been transected are very limited in the literature. It was aimed to evaluate the surgical complications and early results of the patients with proximal hypospadias requiring urethral plate transection.
Material and method
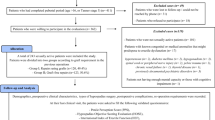
Thirty-two cases with severe proximal hypospadias who underwent VC correction by transection of the urethral plate between 2019 and 2022 years were evaluated. Demographic data of the cases, additional anomalies (Table 1), operation notes, complications were retrospectively analyzed from hospital records. Re-do cases that were operated in different centers were excluded from the study. All hypospadias operations were started by performing the artificial erection test. Midline Heineke and Mikulicz dorsal plication was preferred in cases where VC persisted below 30 degrees after the skin degloving and excision of the fibrotic structures. Urethral plate transection between the glans and the urethral meatus applied in persisted VC larger than 30 degrees. In cases where the VC was corrected after transection, a two-stage intervention was performed by covering the urethral bed with a graft taken from the foreskin or oral mucosa, while a single-stage intervention was performed with a transverse island flap in one case. In cases whose chordee did not improve with the transection of the urethral plate, three ventral corporotomies and staged procedure was performed.
Results
The ages of the patients included in the study ranged between 8 months-16 years with a mean age of 4.61 ± 4.10 years. Ventral curvature was below 90 degrees in 6 patients and above 90 degrees in 26 patients. Bracka operation was performed on 8, Duckett operation on 1, STAG operation on 8, and STAC operation on 15 cases. In 9 (28.2%) of the cases, the chordee totally improved after separation of the urethral plate. Ventral corporatomy was required as additional procedure in remainig 23 cases (71.8%) due to persistent chordee above 30 degrees. Buccal mucosal graft was used in 15 cases and preputium graft in 16 cases. Graft take was successful in 29 cases (90.3%), 3 children required revision of fibrotic graft. In the artificial chordee test performed during the urethroplasty, less than 30 degrees of chordee was detected in seven patients (22.5%), and dorsal plication was added to the procedure. Three of the patients who had plication were in Bracka group. The remaining four patients were in STAG (n = 2) and STAC (n = 2) repair group. Dartos flap was applied to cover the urethroplasty in 25 cases and tunica vaginalis was applied in 4 cases. Second/third stage completed in all children. Success rate detected to be 53.2%. No diverticulum, no urethral dehiscence was encountered. Cosmetic appearance was excellent in follow up. Complications were detected in 15 cases (46.8%) in total. In cases where complications were determined, preputium was used as graft in 8 cases. Complications were as follows: 3 patients (37.5%; fistula + mea stenosis 1, fistula 2) from Bracka group, 7 patients (87.5%; meatal stenosis 2, graft stricture 2, hematoma 1, glanuler dehiscence1, fistula 1) from STAG group, 4 patients (26.6%; meatal stenosis 1, hematoma 1, graft stricture 1, glanuler dehiscence 1) from STAC group and 1 fistula case from Duckett group (Table 2).
Discussion
Especially over the years, paradigm shifts have been observed in proximal hypospadias repair. Today, many surgeons believe that staged procedures offer superior functional and cosmetic results with fewer complications in the treatment of proximal hypospadias. Two-stage repairs permit compartmentalization of the repair, providing the opportunity to reevaluate the situation along the way for complex hypospadias cases. The time interval between the first and second stage allows for growth of the penile structures and reveals complications that relate to recurrent VC or graft contracture.
Insufficient ventral skin, abnormalities in subcutaneous dartos tissue, short urethral plate, corporal disproportion are possible explanations for VC development2,3,4. Correct determination of the cause of development is important in choosing the surgical technique to be applied and therefore in achieving a successful result5. Several surgical techniques have been described for repair of any possible cause of VC. Skin degloving and dartos dissection, urethral mobilization or transsection, ventral lenghtening are VC releasing approaches5. The techniques described can be applied alone or in combination, depending on the degree of VC.
In a proportion of patients with primary severe hypospadias, UPT is deemed necessary for penile straightening5. Accepted surgical approaches for these patients have included preputial island tube urethroplasty or the use of urethral plate substituting techniques5. In the latter, the urethral plate continuity is restored by interposition of preputial skin or oral mucosa in the gap between the ends of the divided urethral plate6,7. Twenty-two of 32 patients included in the presented study required corporotomies for VC relaease in addition to UPT.
In patients undergoing UPT it is still controversial as to whether staging the repair would actually decrease the complication rate and improve outcomes or just increase the number of surgeries8. Current review study conducted by Yadav et al. on 2023 aimed to highlight outcomes of VC surgical techniques in patients with and without hypospadias9. In their review two studies reported comparing UPT with plication. Wang et al. reported overall success rate to be 77.8% and 50% in UPT with dorsal plicaton and UPT group alone respectively10. No significant difference found in study comparing UPT to UPT with dorsal plication group11. In a recent study reported by Hennayake et al., two groups of patients with proximal hypospadias who underwent UPT and those who underwent bulbospongiosus muscle repair in addition to UPT were compared. They concluded that bulbospongiosa muscle repair would contribute significantly to the physiology of micturition and ejaculation by normalizing the anatomy of the penoscrotal junction and bulbar urethra. Also, repair of the bulbospongiosus muscle is reported to cause repositioning of the penile base at the anterior end of the pubic bones which creates cosmetically acceptable appearance, especially in cases with penoscrotal transposition12.
As in the literature we use one stage repair for only selected patients with minimal degree of VC and qualified urethral plate13. The most common used techniques in our clinic for severe hypospadias cases are STAC and STAG repairs. We took the importance of VC (rather than meatal location) into consideration while choosing the surgical intervention. Because VC has been defined as the factor that significantly affects surgical success14.
There are several studies reporting staged proximal hypospadias repair technique results. Some of them argue that multi-stage repair is superior to single-stage repair2,15,16 and vice versa17,18. The results of 2-stage STAG and 3-stage STAC for primary proximal hypospadias were recently compared by Snodgrass also19. As a result with fewer urethroplasty complications, healthier grafts and shaft skins STAC repair reported to be reliable technique for severe hypospadias cases.
Despite the large number of comparative studies, long-term studies reporting the anatomical and functional results of patients together are restricted20,21,22,23,24. Normal anatomical closure is adviced for vetter postpubertal results. Gong et al. in their study reviewed the literature regarding modern proximal hypospadias repair approaches and outcomes20. They reported overall complication rates of currently used techniques to be 4–68%. The point they particularly emphasize is that these rates are reported ignoring functional complications. Andersson et al. reported the urological long-term outcome of proximal hypospadias repair as ‘’good’’. Also, as a result of Penile Perception Score, preservation of penile length and correcting curvature in proximal hypospadias reported to be a priority in this patient group21. Therefore, based on the all evidences, literature still have no answer to ‘’what is the best approach for proximal hypospadias repair?’’ question. The mean age of the patient group included in the study, the ongoing follow-up and small sample size restrict us from reporting functional results for now.
Nearly all patients with VC also had urethroplasty complications in presented study, indicating that surgeons should check AE while operating for fistulas, wound dehiscences, and obstructions. Based on the experience gained as a result of the study authors recommend surgeons objectively measure VC and consider ventral lenghtening when it exceeds 30 degrees.
Conclusion
Urethral plate transection and/or ventral corporotomy achieve proper straightening of the penis and allows for reconstruction of a good urethra, yet urethrocutaneous fistula and meatal stenosis remain the main complications. Even for proximal hypospadias, degloving the penis alone can correct the VC, and transection of the urethral plate should be avoided before repeating an artificial erection. Follow up is important to address long term functional results of ventral corporotomies.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- STAC:
-
Straighten and close hypospadias repair
- STAG:
-
Staged tubularized autograft hypospadias repair
- STAC:
-
Ventral curvature
References
Braga, L. H. et al. Ventral penile lengthening versus dorsal plication for severe ventral curvature in children with proximal hypospadias. J. Urol. 180, 1743–1748. https://doi.org/10.1016/j.juro.2008.03.087 (2008).
Snodgrass, W. & Bush, N. Staged tubularized autograft repair for primary proximal hypospadias with 30-Degree or greater ventral curvature. J. Urol. 198, 680–686. https://doi.org/10.1016/j.juro.2017.04.019 (2017).
Atmoko, W. et al. Abnormal Dartos fascia in buried penis and hypospadias: evidence from histopathology. J. Pediatr. Urol. 14, 536e1. 536.e7 (2018).
Snodgrass, W. & Bush, N. Tubularized incised plate proximal hypospadias repair: continued evolution and extended applications. J. Pediatr. Urol. 7 (1), 2–9. https://doi.org/10.1016/j.jpurol.2010.05.011 (2011).
Castagnetti, M. & El-Ghoneimi, A. Surgical management of primary severe hypospadias in children: systematic 20-year review. J. Urol. 184 (4), 1469–1474. https://doi.org/10.1016/j.juro.2010.06.044 (2010).
Johal, N. S., Nitkunan, T., O’Malley, K. & Cuckow, P. M. The two-stage repair for severe primary hypospadias. Eur. Urol. 50, 366–371. https://doi.org/10.1016/j.eururo.2006.01.002 (2006).
Macedo, A. Jr & Srougi, M. Onlay urethroplasty after sectioning of the urethral plate: early clinical experience with a new approach - the ‘three-in-one’ technique. BJU Int. 93 (7), 1107–1109. https://doi.org/10.1111/j.1464-410X.2003.04789.x (2004).
Shukla, A. R., Patel, R. P. & Canning, D. A. The 2-stage hypospadias repair. Is it a misnomer? J. Urol. 172, 1714–1716. https://doi.org/10.1097/01.ju.0000138926.26530.f9 (2004).
Yadav, P. et al. A scoping review on Chordee correction in boys with ventral congenital penile curvature and hypospadias. Indian J. Urol. 40, 17–24. https://doi.org/10.4103/iju.iju_277_23 (2024).
Wang, C., Zhang, W. & Song, H. Recurrent ventral curvature with Long-Term Follow-up after transverse preputial Island urethroplasty. Eur. J. Pediatr. Surg. 30, 429–433. https://doi.org/10.1055/s-0039-1688479 (2020).
Zhang, Y. et al. Using Buck’s fascia as an integral covering in urethroplasty to restore the anatomical structure of the penis in One-Stage hypospadias repair: A multicenter Chinese study comprising 1,386 surgeries. Front. Pediatr. 9, 695912. https://doi.org/10.3389/fped.2021.695912 (2021).
Hennayake, S. et al. Repair of the bulbospongiosus muscle to suspend the penis to the pubic bones in proximal hypospadias. J. Pediatr. Surg. 60 (2), 162074. https://doi.org/10.1016/j.jpedsurg.2024.162074 (2025).
Snodgrass, W. & Bush, N. Recurrent ventral curvature after proximal TIP hypospadias repair. J. Pediatr. Urol. 17, 222e1–222e5. https://doi.org/10.1016/j.jpurol.2020.11.030 (2020).
Castagnetti, M. & El-Ghoneimi, A. Surgical management of primary severe hypospadias in children: an update focusing on penile curvature. Nat. Rev. Urol. 19, 147–160. https://doi.org/10.1038/s41585-021-00555-0 (2022).
Joshi, R. S. et al. The Bracka two-stage repair for severe proximal hypospadias: A single center experience. J. Indian Assoc. Pediatr. Surg. 20, 72–76. https://doi.org/10.4103/0971-9261.151549 (2015).
Tiryaki, S. et al. Unexpected outcome of a modification of Bracka repair for proximal hypospadias: high incidence of diverticula with flaps. J. Pediatr. Urol. 12, 395. e1-395.e6 (2016).
Pippi Salle, J. L. et al. Proximal hypospadias: A persistent challenge. Single institution outcome analysis of three surgical techniques over a 10-year period. J. Pediatr. Urol. 12, 28e1–28e287. https://doi.org/10.1016/j.jpurol.2015.06.011 (2016).
Castagnetti, M., Zhapa, E. & Rigamonti, W. Primary severe hypospadias: comparison of reoperation rates and parental perception of urinary symptoms and cosmetic outcomes among 4 repairs. J. Urol. 189 (4), 1508–1513. https://doi.org/10.1016/j.juro.2012.11.013 (2013).
Snodgrass, W. & Bush, N. 2-stage STAG vs 3-stage STAC for primary proximal hypospadias repair. J. Pediatr. Urol. 21 (2), 522–525. https://doi.org/10.1016/j.jpurol.2024.10.023 (2025).
Gong, E. M. & Cheng, E. Y. Current challenges with proximal hypospadias: we have a long way to go. J. Pediatr. Urol. 13 (5), 457–467. https://doi.org/10.1016/j.jpurol.2017.03.024 (2017).
Andersson, M. et al. Urological results and patient satisfaction in adolescents after surgery for proximal hypospadias in childhood. J. Pediatr. Urol. 16:660.e1-660.e8. 10.1016/j.jpurol.2020.07.005 22 (2008).
Effect of hypospadias on sexual function and reproduction. Ind. J. Urol. 24(2):249–52. doi: 10.4103/0970-1591.40623. (2023).
Post-pubertal functional outcomes of one-stage anatomical reconstruction of the corpus spongiosum, bulbospongiosus muscle and dartos in 46 children with proximal hypospadias. J. Pediatr. Urol. 19(4):383–390. doi.org/10.1016/j.jpurol.2023.03.024 (2020).
Bracka, A. A long-term view of hypospadias. Br. Jof Plast. Surg. 42, 251–255 (1989).
Author information
Authors and Affiliations
Contributions
Gokhan Demirtas , Tugrul Tiryaki wrote the main manuscript text and Gunay Ekberli contributed to manuscript Figs. 1 and 2 and writing, revision made by Bilge Karabulut and Suleyman Tagci.All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Ankara Bilkent City Hospital (15.05.2024/TABED 2-24-167).
Consent to participate
Written informed consent was obtained from the parents.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Demirtas, G., Ekberli, G., Tagcı, S. et al. Urethral plate transection for chordee release in severe proximal hypospadias cases. Sci Rep 15, 15269 (2025). https://doi.org/10.1038/s41598-025-00079-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-00079-2