Abstract
Flooding exacerbates health challenges by spreading waterborne diseases like diarrhea through the destruction of sanitation infrastructure and contamination of drinking water sources. However, evidence on the prevalence and contributing factors of diarrheal diseases among under-five children in the Dasenech district is limited. This study aimed to assess the prevalence of acute diarrhea and its determinants among under-five children in flood-affected areas of the South Ethiopia region. A community-based cross-sectional study was conducted from July 1 to July 15, 2024, in flood-affected areas of the Dasenech district, involving 696 under-five children. Five kebeles were purposively selected, followed by the proportional allocation of households, after which a systematic sampling technique was applied to identify study participants. Data were collected using a pretested and structured questionnaire administered by trained interviewers. Multivariable logistic regression analysis was performed to identify factors associated with acute diarrhea, with statistical significance set at p < 0.05 and a 95% confidence interval (CI). The prevalence of acute diarrhea was 31.6% (95% CI: 28.7–34.3%). Significant predictors of acute diarrhea included non-adherence to exclusive breastfeeding (AOR: 2.14, 95% CI: 1.65–3.98), lack of latrines (AOR: 12.08, 95% CI: 9.77–13.13), unsafe disposal of child excreta (AOR: 3.86, 95% CI: 2.38–6.26), home delivery (AOR: 6.02, 95% CI: 5.53–8.82), and a recent history of diarrhea among mothers or caregivers (AOR: 3.14, 95% CI: 1.33–5.66). Acute diarrhea is highly prevalent among under-five children in the Dasenech district. The findings underscore the need for targeted public health measures, such as improving waste management, promoting exclusive breastfeeding, constructing and utilizing latrines, and addressing maternal and caregiver health, to mitigate the burden of diarrheal diseases in this vulnerable population.
Similar content being viewed by others
Introduction
Diarrhea is defined as an increase in bowel movement frequency or a change in stool consistency, commonly identified as the passage of three or more loose or watery stools within a 24-h period1. This condition often results from intestinal infections caused by bacteria, viruses, or parasites, which are closely associated with limited access to safe water and inadequate sanitation facilities2. Inadequate water and sanitation contribute to over 94% of the four billion annual cases of diarrhea worldwide3,4. This condition claims approximately two million lives each year, representing 4% of global mortality. Alarmingly, 1.3 million of these deaths occur among children annually5.
Children in low- and middle-income countries (LMICs) disproportionately bear the burden of diarrheal diseases, with South Asia and sub-Saharan Africa accounting for 88% of global childhood deaths due to diarrhea6,7. Children under the age of five in developing nations experience an average of three episodes of diarrhea each year, underscoring the high prevalence of this disease in these regions8,9. Notably, diarrhea has a strong association with poverty, disproportionately affecting marginalized and impoverished populations9. Among under-five children, diarrhea is the most common illness and the second leading cause of death, following respiratory infections10,11. In 2016, approximately 829,000 deaths were attributed to inadequate water, sanitation, and hygiene (WASH) conditions, with 297,000 occurring in children under-five. This represented 60% of all diarrhea-related deaths globally and 5.3% of deaths in this age group in LMICs12. These statistics emphasize the critical need for targeted interventions to address WASH deficiencies and reduce the burden of diarrheal diseases in vulnerable populations.
Tropical infectious diseases, including diarrheal illnesses, pose significant challenges to global health and economic development. Among these, diarrhea is particularly detrimental to children, especially during the first two years of life, a vital period for growth and development13. Recent national statistics indicate that approximately 13% of children experienced diarrhea within a two-week period14. Additionally, local studies reveal that the prevalence of diarrhea among children under-five varies across different regions of the country, ranging from 12 to 31%15,16,17,18,19,20,21,22,23. Beyond the immediate health implications, early childhood diarrhea has far-reaching consequences, including impaired growth, delayed physical development, and reduced cognitive function, all of which can diminish human potential and productivity. Moreover, severe cases increase the risk of life-threatening complications such as dehydration, electrolyte imbalances, kidney failure, and organ damage13,24.
The high prevalence and severity of diarrhea are driven by multiple factors, including inadequate access to clean water, poor sanitation, improper disposal of human waste25, insufficient feeding and hygiene practices26, substandard living conditions, and limited availability of affordable and effective healthcare services27,28. Environmental factors also play a significant role. For instance, a study conducted in flood-affected districts of the South Gondar Zone reported a high prevalence of diarrhea (29.0%), largely attributed to poor sanitation, hygiene practices, and low community awareness18.
The Dasenech district, located in the South Ethiopia region and recognized at the national level, is particularly prone to recurrent flooding due to its flat terrain. These flooding events significantly worsen public health challenges by promoting the spread of waterborne diseases, such as diarrhea29. As a result, the district provides a vital case study for understanding the effects of persistent flooding on communities and the resulting burden of diarrheal diseases.
Numerous studies have explored diarrhea among children under-five in Ethiopia11,15,16,17,18,19,20,21,22,23,30,31. For instance a systematic review and meta-analysis study conducted in Ethiopia shows that the pooled prevalence of diarrhea among under-five children are 22.0% and 20.8%30,31. However, insufficient attention has been given to the burden of diarrhea in flood-affected areas, where the issue is often more severe. Despite its significance, research in this area remains limited, with only one notable study conducted in the Fogera and Libo Kemkem districts of Northwest Ethiopia18. Furthermore, there is a lack of comprehensive data from other regions, including the Southern region, highlighting the need for broader investigation. This gap in research hinders efforts to generate current data on diarrheal disease in flood-affected areas, which is essential for guiding decision-makers in prioritizing interventions. This study, therefore, aimed to assess the prevalence and predictors of diarrheal disease among under-five children living in flood-affected areas of Southern Ethiopia. The findings are expected to support the development of proactive preventive measures, reduce the incidence of acute diarrhea in the Dasenech district, and offer insights that could benefit similar communities.
Methods and materials
Study area, design, and period
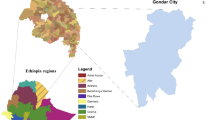
A community-based cross-sectional study was conducted in the flood-affected areas of Dasenech district from July 1 to July 15, 2024. Located in the South Ethiopia Region within the South Omo Zone, Dasenech district lies in the Omo River and Lake Turkana watershed at an altitude of 350–370 m above sea level. The district’s terrain is predominantly flat (99.83%), with only 0.17% consisting of plateau land. It comprises 39 rural kebeles (small administrative unit in Ethiopia) and one urban administrative center, Omo Rate Town, which serves as the district capital. Omo Rate is situated 932 km southwest of Addis Ababa and 712 km south of Hawassa. The district shares borders with Hammer District to the north, Kenya to the south, Hammer District to the east, and Gnangatom District to the west.
As per data from the Dasenech district vital registration office, the district’s 2024 projected population was 136,933. During the study period, the district had three health centers and 21 health posts. In the past three years, Dasenech has experienced recurrent flooding caused by excessive or sudden water releases from the nearby Gibe 3 hydroelectric dam, as well as overflow and directional changes of the Omo River and Lake Turkana. These floods frequently damage sanitation facilities and water supply systems, compromising water quality and sanitation and increasing the community’s vulnerability to waterborne diseases. For instance, the 2024 joint report by the United Nations Office for the Coordination of Humanitarian Affairs (OCHA) revealed that flooding in November 2023 displaced 79,828 people and affected 62,793 individuals, leading to heightened risks of physical injuries and communicable diseases. Additionally, in May 2024, an overflow of the Omo River impacted 12,247 individuals, many of whom faced the risk of displacement32,33.
Study and source population
In this study, the source population included all households residing in flood-affected areas of the Dasenech District. The study population comprised households specifically located in purposively selected kebeles within the district. Data were collected through interviews with either the household head or a family member who had at least one child under the age of five and was present during the data collection period.
Eligibility criteria
Mothers or caregivers with at least one child under-five years of age who had resided in the Dasenech district for a minimum of six months were included in the study. However, those who were unable to provide information due to illness or hearing impairments were excluded.
Sample size determination
The total sample size was determined using the single population proportion formula, based on the following parameters: a prevalence rate of 29.0% from a prior study18, a 5% margin of error, and a 95% confidence level. This yielded an initial sample size of 316. To account for the clustering effect in the sampling design, a design effect of 2 was applied, increasing the sample size to 632. Additionally, to accommodate potential non-responses, a 10% non-response rate was considered, resulting in a final sample size of 696.
Sampling technique and sampling procedure
From the 40 kebeles (the smallest administrative units) in the district, five were purposively chosen based on their proximity to significant geographic features, including the Omo River, Gibe 3 Hydroelectric Dam, and Lake Turkana. These selected kebeles; Toltena (952 households), Hado (669 households), Fejejena Ocholoch (772 households), Karaw (906 households), and Akudengulo (822 households) together comprised a total of 4,121 households with at least one child under the age of five. To ensure representative sampling, proportional allocation was conducted according to the population sizes of the selected kebeles. Households with under-five children were identified using a sampling frame provided by health extension workers, and a simple random sampling technique was applied to select the participating households. In instances where a household had more than one child under the age of five, one child was randomly chosen for the study using the lottery method. This systematic approach ensured fairness and balanced representation in the sampling process. The sampling technique was described in detail (see Fig. 1).
Sampling and study unit
In this study, households with at least one child under the age of five were considered the sampling unit, while mothers or caregivers who provided information about these children were identified as the study unit. The target population was under-five children.
Study variables and measurements
In this study, the dependent variable is the prevalence of diarrheal disease among children under the age of five in flood-affected areas, which was determined by mothers/caregiver-reported occurrences of diarrhea in the past two weeks. The study’s predictor variables were categorized into three main groups: socio-demographic factors, environmental factors, and knowledge and practices of mothers/caregivers.
The socio-demographic factors include the sex and age of the child, the relationship of the interviewee to the child, family size, and the education level and occupation of both the mother/caregiver and father. Additional socio-demographic variables include monthly income, ethnicity, marital status, and religion. These variables are important as they may influence access to healthcare, living conditions, and the overall well-being of the child. Environmental factors encompass the type of floor material in the household, latrine availability and ownership, method of refuse disposal, types of water sources, and the type of water storage container. These factors directly relate to the sanitation and hygiene practices within the household, which can significantly impact the prevalence of diarrheal disease. Finally, the knowledge and practices of mothers/caregivers were assessed based on several aspects, including whether the child consumes food other than breast milk, whether a separate material is used for food preparation, and the method of child feeding (such as exclusive breastfeeding). Additional practices included ensuring that drinking water storage containers are covered and properly used, awareness of fly-borne disease transmission, and the safe disposal of child excreta. Information was also gathered on the place of birth, birth order of the child, history of diarrhea in the past two weeks, vaccination status, and whether the child was exclusively breastfed. These variables are crucial as they directly reflect the caregivers’ role in preventing diarrhea and promoting the health of the child.
Data collection method and tool
Data was collected through face-to-face interviews using a structured questionnaire. The data collection team consisted of five diploma nurses and one bachelor’s degree environmental health professional, who were involved in both data collection and supervision. All supervisors and data collectors received training on the study’s objectives, data collection methods, proper completion of the questionnaire, and the ethical considerations of engaging with participants in a respectful and courteous manner. In our study, if a household had two or more children under the age of five, one child was randomly selected for inclusion. This approach was implemented to avoid bias and ensure equal representation from each household, regardless of the number of children.
Operational definitions
Acute diarrhea: Children who had loose or watery stools than normal (three or more times) within 24 h, in the past 2 weeks before data collection34.
Safe child faeces disposal: Disposing of the stool of the child using either defecation into a latrine, putting or rinsing into a latrine, or disposed of by burial35.
Kebele: A small administrative unit in Ethiopia.
Data quality assurance
The socio-demographic, environmental, knowledge and practice, and diarrheal disease information were gathered through a pretested structured questionnaire, which was developed by reviewing relevant literature11,15,16,17,18,19,20,21,22,23,30,31 and adapting the WHO core questionnaire (WHO, 2006)36. This adaptation allowed for the inclusion of variables pertinent to the local context and study objectives. The questionnaire was pretested to ensure clarity, relevance, and cultural appropriateness before being used for data collection. It was first translated into Amharic, the local official language of the study area, and then back-translated into English to ensure the accuracy and consistency of the translation. To maintain data quality, training was provided to both data collectors and supervisors. Additionally, the questionnaire was pretested among 5% of the sample size in a nearby kebele in the Gnangatom district prior to the actual data collection. The Cronbach’s alpha value for the questionnaire was 0.73, which is above the acceptable threshold of 0.60, indicating that the questionnaire’s reliability was deemed satisfactory for use in this study37.
Statistical analysis
The data was coded and entered into EpiInfo™ 7.2 and subsequently exported to SPSS 25.0 for analysis. Descriptive analysis was conducted to summarize the socio-demographic characteristics of the research participants. Bivariable and multivariable logistic regression analyses were performed to identify potential predictive factors. In the bivariable logistic regression, variables with a p-value of 0.25 or less38, were considered as candidate variables and included in the multivariable regression model. In the final multivariable model, variables with a p-value of less than 0.05 at a 95% confidence interval (CI) were considered statistically significant predictors associated with the prevalence of acute diarrhea.
Result
All 690 filled-out questionnaires were returned and analyzed, yielding a 99.13% response rate.
Socio-demographic characteristics of study participants
Among the 690 mothers and caregivers who participated in the study, the mean age was 34.5 ± 6.2 years, with half (345, 50.0%) falling within the age range of 32–38 years. The mean age of under-five children was 27.6 ± 4.5 months, with over half (56.6%) aged between 25–36 months, and 53.9% were male. The majority of respondents, 640 (92.8%), reported a family size of five or fewer members. Regarding the relationship to the child, most participants (89.8%) were the child’s mother. Among the respondents, 592 (85.9%) were married, and 413 (59.9%) identified farming as their primary occupation. In terms of religion, 520 participants (75.3%) identified as Catholic. Additionally, more than half of the respondents (378, 54.8%) were illiterate, indicating they were unable to read or write. These findings provide valuable demographic and socioeconomic insights into the study population (see Table 1).
Environmental factors
Among the participants, 430 (62.3%) reported living in homes with wood-based floors, and 586 (85.0%) had access to a latrine. Regarding waste disposal practices, 424 (61.4%) disposed of waste in open fields, 189 (27.4%) used pit holes, 44 (6.3%) used garbage cans, and 33 (4.8%) burned their rubbish. The study also revealed that a majority of respondents, 484 (70.0%), relied on unprotected wells or springs as their primary source of drinking water. Furthermore, over three-quarters of the participants, 459 (78.3%), reported having privately owned latrines. These findings highlight significant gaps in safe waste disposal and access to protected water sources, which are critical for improving sanitation and reducing health risks (see Table 2).
Practice and knowledge of mother/caregiver of under-five children
Among the 690 mothers and caregivers surveyed, 648 (94.0%) reported that their child had consumed food or drink other than breast milk. Of these, 628 (91.0%) prepared the child’s food separately using designated utensils. Supplementary feeding with gruel was reported for 308 (44.6%) children, and 339 (49.1%) of them were fed using a bottle.
Regarding water storage practices, 617 (89.7%) participants reported that their drinking water storage containers were covered, 630 (91.3%) accessed water by dipping into the storage container, and 584 (92.7%) used a separate can for retrieving water. The survey also examined awareness of disease transmission and sanitation practices. A total of 619 (89.8%) participants recognized flies as disease carriers, while 376 (54.5%) safely managed their child’s excreta. Additionally, 596 (86.4%) acknowledged that children’s excreta could contribute to disease transmission. Most of the children, 474 (68.7%), were born in a health facility, and 438 (63.4%) were vaccinated against measles. However, 289 (41.9%) of mothers or caregivers reported experiencing diarrhea within the two weeks preceding the interview. These findings emphasize the need for improved hygiene practices and health education to reduce the risk of disease transmission (see Table 3).
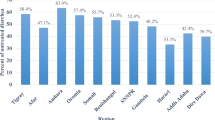
Prevalence of acute diarrheal disease among under-five children
The prevalence of diarrheal disease among children under the age of five was 31.6% (95% CI: 28.7–34.3%) in the two weeks preceding the study (see Fig. 2). Of the 218 children who experienced diarrhea during this period, 146 (67.0%) were reported to have had watery diarrhea, as indicated by their mothers or caregivers. Additionally, 92 children (42.0% of those with diarrhea) were taken to a health facility for treatment.
Factors associated with the prevalence of acute diarrheal disease
After adjusting for potential confounders in the multivariable binary logistic regression analysis, several factors were identified as significant predictors of diarrheal diseases among under-five children. These included non-adherence to exclusive breastfeeding, lack of latrine facilities, unsafe disposal of child excreta, home delivery, and a recent history of diarrhea in mothers or caregivers.
The regression analysis identified several significant risk factors for childhood diarrhea. Exclusive breastfeeding played a crucial protective role, as children whose mothers did not exclusively breastfeed were more than twice as likely to develop diarrhea compared to those who received exclusive breastfeeding [AOR = 2.14, 95% CI: 1.65–3.98]. Sanitation factors were strongly associated with diarrheal disease prevalence. Households lacking latrine facilities had a 12-fold higher risk of childhood diarrhea compared to those with access to latrines [AOR = 12.08, 95% CI: 9.77–13.13]. Likewise, improper child excreta disposal significantly increased the risk, with children in households practicing unsafe disposal being nearly four times more likely to experience diarrhea than those in households using safe disposal methods [AOR = 3.86, 95% CI: 2.38–6.26]. Place of birth was another significant factor, as children born at home had a six fold higher likelihood of developing diarrhea compared to those delivered in health facilities [AOR = 6.02, 95% CI: 5.53–8.82]. Additionally, a recent history of diarrhea in mothers or caregivers within the past two weeks was associated with a threefold increase in the risk of childhood diarrhea [AOR = 3.14, 95% CI: 1.33–5.66].
These findings highlight the urgent need for interventions aimed at promoting exclusive breastfeeding, improving access to latrines, ensuring safe disposal of child excreta, encouraging facility-based deliveries, and addressing household-level transmission risks to reduce the burden of diarrheal diseases among children under-five. Further public health efforts should focus on these modifiable risk factors to mitigate the occurrence of childhood diarrhea in flood-prone and resource-limited settings (See Table 4).
Discussion
This community-based cross-sectional study aimed to assess the prevalence and factors associated with diarrhea among under-five children living in flood-affected regions of Dasenech district. The findings showed that the prevalence of acute diarrheal disease among under-five children was 31.6% (95% CI: 28.7–34.3%). The study identified several significant predictors of diarrhea, including non-adherence to exclusive breastfeeding, lack of access to latrine facilities, unsafe disposal of child excreta, home delivery, and a history of diarrhea in mothers or caregivers.
The 31.6% prevalence of diarrhea observed in this study is similar to findings from other regions, such as Wonago District (30.9%)39, Northern Kenya (32.1%)40, and rural Burundi (32.6%)41. These results align with previous studies conducted in Arba-Minch District (30.5%)42, Uganda (29.1%)19, Yemen (29.07%)43, Fogera and Libo Kemkem (29.0%)18, and Nekemte Town (28.9%)20. The similarity in findings may be attributed to comparable water, sanitation, and hygiene practices, as well as socioeconomic conditions across these study areas. Poor hygiene and limited access to sanitation in economically disadvantaged areas are significant contributing factors to the high prevalence of diarrhea44.
The findings of the current study show a higher prevalence of acute diarrheal disease among under-five children compared to other studies. For instance, the Ethiopian Demographic and Health Survey reported a prevalence of 12.0%16, while Debre Berhan town had a rate of 16.4%45, and Kamashi District in the Benishangul Gumuz Region reported 14.5%15. Additionally, Goba District reported 17.2%46, Bahir Dar City 14.5%47, Gelsha 11.0%48, Sheka Zone 21.8%22, North Gondar Zone 22.1%21, Gondar town 24.64%17, and Harena Buluk Woreda 28.4%23. Other comparative studies show rates such as Tiko-Cameroon at 23.8%28, Senegal at 26.0%49, and Mecha District at 22.1%50. Furthermore, Kersa District and Jabi Tehinan District reported 22.5% and 21.5%, respectively51,52. The higher prevalence observed in the current study is attributed to the unique context of the flood-affected areas, where flooding significantly exacerbates public health challenges, such as the spread of waterborne communicable diseases like diarrhea. Flood-affected regions often lack sufficient water, sanitation, and hygiene infrastructure, which contribute to the high rates of diarrheal disease. This may also be related to the destruction of existing water and sanitation facilities by seasonal floods, particularly during the summer, and the lack of proper health extension program implementation.
The prevalence of diarrhea among under-five children observed in this study (31.6%) is lower compared to reports from Enderta Woreda (35.6%), non-open-defecation-free residents of Farta District (40.5%) in Ethiopia, as well as slum areas in Kenya (37.3%)53,54,55. This lower prevalence might be attributed to heightened awareness and targeted health interventions in flood-affected areas. These regions are often identified as high-risk zones for waterborne diseases, leading to prioritization by government and non-governmental organizations for public health initiatives, including clean water provision and improved sanitation infrastructure. Moreover, communities in flood-affected areas may adopt better hygiene practices, such as proper water storage and treatment, driven by the necessity to address the risks associated with frequent flooding. These proactive measures could contribute to the reduced prevalence of diarrhea in such settings.
The current findings reveal that the prevalence of acute diarrheal disease was significantly associated with the availability of latrines. Children from households without latrines were twelve times more likely to develop acute diarrhea compared to those from households with latrine facilities. This observation is supported by findings from a cross-sectional study conducted in Ethiopia30, Jama district56, Benna Tsemay district57, Dabat district58, Farta district54, North Gondar zone59, Idiofa, Democratic Republic of the Congo41, and in Indonesia42. Proper use of latrines, regardless of whether they are renovated, has been shown to provide health benefits and reduce the risk of diarrheal diseases41. However, beyond latrine availability, the structural integrity of these facilities in flood-prone areas is a critical concern. Floodwaters can submerge and erode latrine walls, leading to fecal contamination of the environment and water sources, thereby exacerbating the spread of diarrheal diseases. Therefore, the construction of flood-resilient latrines, along with improved drainage systems and safe water access, is essential in mitigating the health risks associated with flooding. Investing in sustainable water, sanitation, and hygiene (WASH) infrastructure tailored to flood-prone settings is crucial for long-term disease prevention and public health protection.
The odds of developing acute diarrhea were twice as high among under-five children whose mothers or caregivers did not practice exclusive breastfeeding compared to their counterparts. This finding aligns with a previous study conducted in Bereh district60, Rural Areas of North Gondar Zone21, Bahir Dar city47, Kenya55, Robe Didea General Hospital, Ethiopia61, and Bangladesh40. Furthermore, it supports the recommendations of the World Health Organization (WHO), the United Nations International Children’s Emergency Fund (UNICEF), the American Academy of Pediatrics (AAP), the American Academy of Family Physicians (AAFP), and the National Nutrition Programme of Ethiopia (NNPE), which emphasize that exclusive breastfeeding (EBF) is an effective, cost-efficient, and long-lasting natural strategy for reducing child morbidity and mortality associated with infectious diseases.
Children from households with improper disposal of child feces were approximately four times more likely to experience diarrhea compared to those from households with proper child feces disposal practices. This finding is supported by a study conducted in Horo Guduru Wollega Zone62, Farta district54, Jamma district56, Welkite Town63, Pawi64, and India43. Although it may seem that children’s feces are less hazardous than adult feces, evidence indicates that they pose a greater health risk due to the higher prevalence of viruses such as hepatitis A, rotavirus, and other infectious diseases43,44. This study highlights the critical need for safe disposal of juvenile excreta to achieve the Sustainable Development Goals (SDGs) and reduce preventable deaths.
Children delivered at home were approximately six times more likely to experience diarrhea compared to those delivered in health institutions. Mothers who deliver in health facilities are more likely to adopt recommended practices, including immunization, exclusive breastfeeding, participation in child growth monitoring programs, and maintaining proper hygiene and sanitation for both the child and household. These practices significantly contribute to improved health outcomes for their children. Similar findings have been reported in previous studies conducted in Awi zone65. These practices play a vital role in reducing the risk of diarrheal diseases and promoting the overall well-being of the child.
This study found that a maternal or caregiver history of diarrhea was significantly associated with an increased risk of acute diarrhea in children. Children whose mothers or caregivers had experienced diarrhea within the two weeks prior to the study were three times more likely to develop diarrhea compared to those whose mothers or caregivers had no such history. Similar findings have been reported in previous studies conducted in Jawi zone66, Pawi64 and other parts of Ethiopia37,45,46. Diarrhea often spreads from person to person due to poor hygiene practices or through contaminated food or drinking water via the fecal–oral route. Consequently, mothers and caregivers responsible for food preparation and child handling may inadvertently transmit the disease. Additionally, if the mother or caregiver is unwell, their ability to properly care for the child may be compromised, further increasing the risk of transmission.
Policy implications from these findings suggest the urgent need for comprehensive health strategies focusing on water, sanitation, and hygiene (WASH) in flood-prone areas. Governments and Non-governmental organizations (NGOs) should prioritize the construction of flood-resilient infrastructure and promote safe water handling and hygiene practices. Additionally, maternal and child health programs must advocate for exclusive breastfeeding and safe fecal disposal practices to reduce the risk of diarrheal diseases. By addressing these issues, particularly in high-risk, flood-affected areas, long-term improvements in child health and reductions in diarrhea-related morbidity and mortality can be achieved.
In general, the findings of this study not only underscore the critical link between flood-related environmental factors and diarrhea prevalence but also highlight the need for targeted policy and community-based interventions to reduce the burden of waterborne diseases among under-five children. Ensuring access to proper sanitation, promoting exclusive breastfeeding, and improving hygiene practices are key to breaking the cycle of diarrhea in flood-affected regions.
Conclusion
The study revealed a high prevalence of diarrheal disease among under-five children in the study area, at 31.6% (95% CI: 28.7–34.3%). Independent predictors of acute diarrhea among under-five children included non-adherence to exclusive breastfeeding, lack of latrine facilities, unsafe disposal of child excreta, home delivery, and mothers’ or caregivers’ histories of diarrhea. To break the chain of transmission and reduce the burden of diarrheal diseases, efforts should focus on improving latrine coverage, promoting maternal education, and adopting safe child excreta disposal practices. These interventions are essential and should be prioritized for effective public health action.
Strength and limitations of the study
One of the key strengths of this study is its focus on assessing the burden of diarrheal disease among under-five children in a marginalized and disadvantaged group located in the Southern region. This group is particularly vulnerable due to its border location, limited access to education, technological resources, and healthcare services, as well as susceptibility to flooding disasters. The study was conducted during the season when such floods commonly occur, providing an accurate reflection of the real prevalence and incidence of the disease in the aftermath of these events. This research is among the few to examine diarrheal disease in flood-affected areas after a flood season, offering valuable insights for governmental and non-governmental organizations involved in emergency response and disaster relief efforts.
However, the study has certain limitations. Being cross-sectional in design, it cannot establish causality. Additionally, there is a possibility of social desirability bias and recall bias, which could lead to inaccurate reporting. The study was also constrained by limited resources, preventing the inclusion of a control group (households located far from river areas) for comparison. Furthermore, the study did not perform seasonal adjustments, which may have limited the ability to assess the long-term prevalence of the disease comprehensively.
Data availability
Data will be made available upon a reasonable request to the corresponding author gech23man@gmail.com.
References
Sokic-Milutinovic, A. et al. Diarrhea as a clinical challenge: General practitioner approach. Dig. Dis. 40(3), 282–289 (2022).
DuPont, H. L. Persistent diarrhea: A clinical review. JAMA 315(24), 2712–2723 (2016).
World Health Organization and UNICEF. Progress on sanitation and drinking-water: 2010 update, in Progress on sanitation and drinking-water: 2010 update (2010).
Abu, M. & Codjoe, S. N. A. Experience and future perceived risk of floods and diarrheal disease in urban poor communities in Accra, Ghana. Int. J. Environ. Res. Public Health 15(12), 2830 (2018).
Black, R. E. et al. Global, regional, and national causes of child mortality in 2008: A systematic analysis. Lancet 375(9730), 1969–1987 (2010).
Mekonnen, W. et al. Under five causes of death in Ethiopia between 1990 and 2016: Systematic review with meta-analysis. Ethiop. J. Health Dev. 34(2) (2020).
Demissie, G. D. et al. Diarrhea and associated factors among under five children in sub-Saharan Africa: Evidence from demographic and health surveys of 34 sub-Saharan countries. PLoS ONE 16(9), e0257522 (2021).
Kosek, M., Bern, C. & Guerrant, R. L. The global burden of diarrhoeal disease, as estimated from studies published between 1992 and 2000. Bull. World Health Organ. 81, 197–204 (2003).
World Health Organization. Meeting the MDG drinking water and sanitation target: The urban and rural challenge of the decade (World Health Organization, 2006).
Ugboko, H. U. et al. Childhood diarrhoeal diseases in developing countries. Heliyon 6(4), e03690 (2020).
Fetensa, G. et al. Diarrhea and associated factors among under-5 children in Ethiopia: A secondary data analysis. SAGE open medicine 8, 2050312120944201 (2020).
Prüss-Ustün, A. et al. Burden of disease from inadequate water, sanitation and hygiene for selected adverse health outcomes: An updated analysis with a focus on low-and middle-income countries. Int. J. Hyg. Environ. Health 222(5), 765–777 (2019).
Guerrant, R. L. et al. Magnitude and impact of diarrheal diseases. Arch. Med. Res. 33(4), 351–355 (2002).
Li, H. et al. 2-week prevalence and associated factors of fever, diarrhea, and coexisting fever and diarrhea among children aged 6–23 months in rural Hunan Province. Sci. Rep. 14(1), 13867 (2024).
Fenta, A., Alemu, K. & Angaw, D. A. Prevalence and associated factors of acute diarrhea among under-five children in Kamashi district, western Ethiopia: Community-based study. BMC Pediatr. 20, 1–7 (2020).
Central statistical agency [Ethiopia] and ICF International: Ethiopia demographic and health survey. Central Statistical Agency [Ethiopia] and ICF International (2011).
Demoze, L. et al. Under five children diarrhea prevalence and associated factors in slum areas of Gondar City Northwest Ethiopia: A community based cross-sectional study. Sci. Rep. 14(1), 19095 (2024).
Birhan, T. A. et al. Prevalence of diarrheal disease and associated factors among under-five children in flood-prone settlements of Northwest Ethiopia: A cross-sectional community-based study. Front. Pediatr. 11, 1056129 (2023).
Omona, S. et al. Prevalence of diarrhoea and associated risk factors among children under five years old in Pader District, northern Uganda. BMC Infect. Dis. 20, 1–9 (2020).
Regassa, G. et al. Environmental determinants of diarrhea among under-five children in Nekemte town, western Ethiopia. Ethiop. J. Health Sci. 18(2) (2008).
Getachew, A. et al. Diarrhea prevalence and sociodemographic factors among under-five children in rural areas of North Gondar Zone, Northwest Ethiopia. Int. J. Pediatr. 2018(1), 6031594 (2018).
Gashaw, T. A. & Walie, Y. M. Prevalence and determinate factors of diarrhea morbidity among under five children in shake zone, Southwest Ethiopia, a community based cross-sectional study. Arch. Community Med. Public Health 5(1), 008–014 (2019).
Beyene, S. G. & Melku, A. T. Prevalence of diarrhea and associated factors among under five years children in Harena Buluk Woreda Oromia region, south East Ethiopia, 2018. J. Public Health Int. 1(2), 9–26 (2018).
Ogbo, F. A. et al. Infant feeding practices and diarrhoea in sub-Saharan African countries with high diarrhoea mortality. PLoS ONE 12(2), e0171792 (2017).
Tarekegn, M. & Enquselassie, F. A case control study on determinants of diarrheal morbidity among under-five children in Wolaita Soddo Town, Southern Ethiopia. Ethiop. J. Health Dev. 26(2), 78–85 (2012).
Shati, A. A. et al. Occurrence of diarrhea and feeding practices among children below two years of age in southwestern Saudi Arabia. Int. J. Environ. Res. Public Health 17(3), 722 (2020).
Unicef and Unicef. Strategy for water, sanitation and hygiene 2016–2030 (2016).
Tambe, A. B., Nzefa, D. L. & Nicoline, N. A. Childhood diarrhea determinants in sub-Saharan Africa: A cross sectional study of Tiko-Cameroon. Challenges 6(2), 229–243 (2015).
Watson, J. T., Gayer, M. & Connolly, M. A. Epidemics after natural disasters. Emerg. Infect. Dis. 13(1), 1 (2007).
Alebel, A. et al. Prevalence and determinants of diarrhea among under-five children in Ethiopia: A systematic review and meta-analysis. PLoS ONE 13(6), e0199684 (2018).
Sahiledengle, B. et al. Burden of childhood diarrhea and its associated factors in Ethiopia: A review of observational studies. Int. J. Public Health 69, 1606399 (2024).
(OCHA), U.N.O.f.t.C.o.H.A. ETHIOPIA Several regions are reeling from the impact of floods that occurred July and August (2024). https://www.unocha.org/publications/report/ethiopia/ethiopia-situation-report-23-august-2024.
(OCHA), U.N.O.f.t.C.o.H.A. Joint Mission Report- flood affected Area, South Ethiopia Region—South Omo Zone, Dasenech Woreda, May 2024 (2024). https://fscluster.org/sites/default/files/2024-06/Joint%20mission%20report%20for%20Dasenech_%20May%202024.pdf.
Jaffaar, M. M., Al-Khafaji, K. A. & Khalid, S. K. Identification of Shigella sp. causing children bloody diarrhea in Baghdad. J. Genet. Environ. Resour. Conserv. 6(1), 14–17 (2018).
Waddington, H. et al. Water, sanitation and hygiene interventions to combat childhood diarrhoea in developing countries. International Initiative for Impact Evaluation (2009).
World Health Organization. Core questions on drinking water and sanitation for household surveys (World Health Organization, 2006).
Bujang, M. A., Omar, E. D. & Baharum, N. A. A review on sample size determination for Cronbach’s alpha test: A simple guide for researchers. Malays. J. Med. Sci. MJMS 25(6), 85 (2018).
Bursac, Z. et al. Purposeful selection of variables in logistic regression. Source Code Biol. Med. 3, 1–8 (2008).
Tesfaye, T. S., Magarsa, A. U. & Zeleke, T. M. Moderate to severe diarrhea and associated factors among under-five children in Wonago District, South Ethiopia: A cross-sectional study. Pediatr. Health Med. Ther. 11, 437–443 (2020).
Mwangi, B. et al., Prevalence and Risk Factors of Diarrhea Among Children Under Five Years in Northern Kenya’s Drylands: A Longitudinal Study. medRxiv https://doi.org/10.1101/2024.11.13.24317266v1 (2024).
Diouf, K. et al. Diarrhoea prevalence in children under five years of age in rural Burundi: An assessment of social and behavioural factors at the household level. Glob. Health Action 7(1), 24895 (2014).
Mohammed, S., Tilahun, M. & Tamiru, D. Morbidity and associated factors of diarrheal diseases among under five children in Arba-Minch district, Southern Ethiopia, 2012. Sci. J. Public Health 1(2), 102–106 (2013).
Mohanna, M. A. B. & Al-Sonboli, N. Prevalence of diarrhoea and related risk factors among children aged under 5 years in Sana’a, Yemen. Hamdan Med. J. 11(1), 29–33 (2018).
Mebrahtom, S., Worku, A. & Gage, D. J. The risk of water, sanitation and hygiene on diarrhea-related infant mortality in eastern Ethiopia: A population-based nested case-control. BMC Public Health 22(1), 343 (2022).
Shine, S. et al. Prevalence and associated factors of diarrhea among under-five children in Debre Berhan town, Ethiopia 2018: A cross sectional study. BMC Infect. Dis. 20, 1–6 (2020).
Megersa, S., Benti, T. & Sahiledengle, B. Prevalence of diarrhea and its associated factors among under-five children in open defecation free and non-open defecation free households in Goba District Southeast Ethiopia: A comparative cross-sectional study. Clin. Mother Child Health 16, 324 (2019).
Dagnew, A. B. et al. Prevalence of diarrhea and associated factors among under-five children in Bahir Dar city, Northwest Ethiopia, 2016: A cross-sectional study. BMC Infect. Dis. 19, 1–7 (2019).
Natnael, T., Lingerew, M. & Adane, M. Prevalence of acute diarrhea and associated factors among children under five in semi-urban areas of northeastern Ethiopia. BMC Pediatr. 21(1), 290 (2021).
Thiam, S. et al. Prevalence of diarrhoea and risk factors among children under five years old in Mbour, Senegal: A cross-sectional study. Infect. Dis. Poverty 6(04), 43–54 (2017).
Dessalegn, M., Kumie, A. & Tefera, W. Predictors of under-five childhood diarrhea: Mecha District, west Gojam, Ethiopia. Ethiop. J. Health Dev. 25(3), 192–200 (2011).
Mengistie, B., Berhane, Y. & Worku, A. Prevalence of diarrhea and associated risk factors among children under-five years of age in Eastern Ethiopia: A cross-sectional study. Open J. Prev. Med. 3(07), 446 (2013).
Anteneh, Z. A., Andargie, K. & Tarekegn, M. Prevalence and determinants of acute diarrhea among children younger than five years old in Jabithennan District, Northwest Ethiopia, 2014. BMC Public Health 17, 1–8 (2017).
Berhe, H., Mihret, A. & Yitayih, G. Prevalence of diarrhea and associated factors among children under-five years of age in enderta woreda, Tigray, northern Ethiopia, 2014. Int. J. Ther. Appl. 31, 32–37 (2016).
Tafere, Y. et al. Diarrheal diseases in under-five children and associated factors among Farta District Rural Community, Amhara Regional State, North Central Ethiopia: A comparative cross-sectional study. J. Environ. Public Health 2020(1), 6027079 (2020).
Mutama, R., Mokaya, D. & Wakibia, J. Risk factors associated with diarrhea disease among children under-five years of age in Kawangware slum in Nairobi County, Kenya. Food Public Health 9(1), 1–6 (2019).
Workie, G. Y., Akalu, T. Y. & Baraki, A. G. Environmental factors affecting childhood diarrheal disease among under-five children in Jamma district, South Wello zone, Northeast Ethiopia. BMC Infect. Dis. 19, 1–7 (2019).
Alemayehu, M., Alemu, T. & Astatkie, A. Prevalence and determinants of diarrhea among under-five children in Benna Tsemay District, South Omo Zone, Southern Ethiopia: A community-based cross-sectional study in pastoralist and agropastoralist context. Adv. Public Health 2020(1), 4237368 (2020).
Melese, M. et al. Prevalence of diarrhea, intestinal parasites, and associated factors among under-five children in Dabat District, Northwest Ethiopia: multicenter cross-sectional study. Environ. Health Insights 17, 11786302231174744 (2023).
Getachew, A. et al. Environmental factors of diarrhea prevalence among under five children in rural area of North Gondar zone, Ethiopia. Ital. J. Pediatr. 44, 1–7 (2018).
Feleke, Y., Legesse, A. & Abebe, M. Prevalence of diarrhea, feeding practice, and associated factors among children under five years in Bereh District, Oromia, Ethiopia. Infect. Dis. Obstet. Gynecol. 2022(1), 4139648 (2022).
Debebe, S., Kloos, H. & Assefa, A. Diarrheal prevalence and associated risk factors among under-five children attending Robe Didea General Hospital, Arsi Robe Town, Oromia Regional State, Ethiopia: A cross-sectional study. Alex. J. Med. 60(1), 65–75 (2024).
Alemayehu, K. et al. Prevalence and determinants of diarrheal diseases among under-five children in Horo Guduru Wollega Zone, Oromia Region, Western Ethiopia: A community-based cross-sectional study. Can. J. Infect. Dis. Med. Microbiol. 2021(1), 5547742 (2021).
Wolde, D. et al. The burden of diarrheal diseases and its associated factors among under-five children in Welkite Town: A community based cross-sectional study. Int. J. Public Health 67, 1604960 (2022).
Brhanu, H., Negese, D. & Gebrehiwot, M. Determinants of acute diarrheal disease among under-five children in Pawi Hospital, Northwest Ethiopia. Am. J. Pediatr. 2(2), 29–36 (2017).
Adam Birhan, N. et al. Prevalence of diarrhea and its associated factors among children under five years in Awi Zone, Northwest Ethiopia. BMC Pediatr. 24(1), 701 (2024).
Gessesse, D. N. & Tarekegn, A. A. Prevalence and associated factors of diarrhea among under-five children in the Jawi district, Awi Zone Ethiopia. Community based comparative cross-sectional study, 2019. Front. Pediatr. 10, 890304 (2022).
Acknowledgements
The researchers extend their deepest gratitude to the administration of Dasenech District, the Dasenech District Health Office, the heads of the respective health centers, and the health extension workers in Ethiopia for their invaluable support, guidance, and insights throughout the research process. Our heartfelt thanks also go to Debre Markos University for their support and for granting study leave, which was instrumental in facilitating this study. Finally, we sincerely acknowledge the unwavering dedication and cooperation of the data collectors, supervisors, and respondents, whose contributions were indispensable to the successful completion of this research.
Author information
Authors and Affiliations
Contributions
G.Y.: study conception and design, data collection, analysis, and interpretation of results, reviewed the results, drafted manuscript preparation, and approved the final version of the manuscript; H.M., B.T., G.A.A., & C.Y.: data collection, reviewed the results, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
Ethical approval for this study was obtained from the Research and Ethical Review Committee of Debre Markos University, under approval number CMHS/R/C/Ser/No/413/16. Participants were provided with comprehensive information about the study’s purpose, methods, and confidentiality measures. Privacy was safeguarded by anonymizing the data and removing any personal identifiers from the questionnaire. Participants were also informed of their right to withdraw their consent at any time without consequence. All participants were provided written informed consent during the study. The Research and Ethical Review Committee verified and confirmed the adherence to ethical standards throughout the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yirdaw, G., Mekonen, H., Assaye, B.T. et al. Prevalence of acute diarrhea and its risk factors among under five children in flood affected Dasenech District, Southern Ethiopia: a cross-sectional study. Sci Rep 15, 16980 (2025). https://doi.org/10.1038/s41598-025-02120-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-02120-w