Abstract
Stress of conscience (SC) in healthcare professionals results from conflicts with ethical beliefs due to work constraints, while moral sensitivity (MS) and a positive ethical climate (EC) are crucial for ethical decision-making and quality patient care. The aim of the study was to assess correlation of the hospital EC, MS and SC among nurses, midwives; to assess psychometric properties of the Polish version of the Stress of Conscience Questionnaire (SCQ). An cross-sectional study was conducted from March 2019 to December 2020 among 683 nurses, midwives working at the hospital. The internal consistency reliability of the SCQ was satisfactory (0.837). A two-factor solution explained 54.26% of the total variance. The intensity of SC among the nurses, midwives increased with the deterioration of selected indicators of the EC of the hospital relationships with managers, the hospital, doctors; deterioration of relationships in these areas increased the subjects’ SC, while the overall indicator of the EC of the hospital remained independent of the intensity of SC. Respondents’ MS were higher the more EC of the hospital in which they worked was. Supporting a culture that values ethics and positive communication among healthcare professionals can create environments that enhance professional satisfaction and prioritize patient-oriented care.
Similar content being viewed by others
Introduction
Stress of conscience (SC) arises when healthcare professionals find themselves unable to act in alignment with their conscience, ethical beliefs due to factors including their work environment1. Conscience, a concept has been approached through various theories. Theological literature often links conscience with an internal or divine voice2,3. Alternatively, some theories suggest that conscience stems from authority figures, family, or society4. Conscience, aids individuals in discerning between right and wrong or in making morally justified decisions5. Acting contrary to conscience can lead to adverse outcomes for healthcare professionals, including feelings of guilt or shame and the need to compromise standards and goals of healthcare services6,7. Moral sensitivity, on the other hand, is defined as the ability of an of an individual to recognise the meaning of a situation in a moral context and the ability to respond to it8. It includes both a person’s emotions, their intention of actions as well as their perception9. It forms part of moral care, is an intuition that stems from a desire to ensure the well-being of another person10. Analysis of the literature shows that the moral sensitivity of nurses and midwives is crucial for holistic patient care, influencing ethical decision-making and the resolution of ethical dilemmas.11. An ethical climate is perceived as the understanding of the colleagues of the ethical behaviour patterns, the capacity to deal with them when they arise. A positive ethical climate supports staff in resolving ethical dilemmas on the basis of developed e.g. standards of practice, guidelines12, and also has a correlation with nurses’ moral sensitivity13 and patient safety culture14. The literature on ethical climate shows that it is not only related to the actions taken by healthcare professionals, but also influences the organisation of clinical work, patient care and thus the quality of services provided by nursing staff15,16.
This study was conducted to investigate the psychometric properties of the Polish version of the Stress of Conscience Questionnaire and to assess the correlation of the level of experienced stress of conscience with the hospital ethical climate and moral sensitivity. A study investigating the above research topic was conducted for the first time in Poland. There have been studies at different settings1,8,16,17 but no research results were found showing the correlation together between selected three factors such as hospital ethical climate, moral sensitivity and stress of conscience. This study can enhance the training of healthcare professionals by improving nurses’ and midwives’ soft and communication skills, emphasizing the importance of effective communication within therapeutic teams, and developing personal ethical decision-making and problem-solving skills needed in clinical practice when interacting with patients, their families, and hospital managers.
Methods
Aim
The objectives of the present study are as follows: (1) to investigate the psychometric properties of the Polish version of the Stress of Conscience Questionnaire; (2) to assess the correlation of the level of experienced stress of conscience with the hospital ethical climate and moral sensitivity.
Two research questions were formulated: (1) What are the psychometric properties of the Polish version of the Stress of Conscience Questionnaire? (2) Is there a correlation between nurses’ and midwives’ stress of conscience their moral sensitivity and the ethical climate of the hospital?
Study design
A descriptive cross-sectional correlational study was carried out in hospitals in eastern Poland, reported according to the guidelines of the Strengthening the Reporting of Observational studies in Epidemiology (STROBE)18. The study was conducted in two adjacent voivodeships (Lubelskie and Podkarpackie) due to the similar state of registered and working nurses, midwives and their age structure19. Raosoft Sample Size Calculator was used to determine the sample size. For a confidence level of 0.95, a margin of error of 0.05, and a response distribution of 0.50, a sample size of 384 respondents was required (based on the report of the Supreme Chamber of Nurses and Midwives in 2019 as a population size indicator19. Data collection for this study occurred from March 2019 to December 2020, encompassing both pre-pandemic and pandemic periods. In Poland the first case of SARS-CoV-2 coronavirus was detected in March 202020. Although our study was initially conceived before the COVID-19 pandemic and not specifically in response to it, we recognize its relevance in understanding stress of conscience amid increased healthcare demands and ethical challenges during crises. Consequently, we conducted an additional analysis to examine the pandemic’s impact on the stress of conscience among nurses and midwives.
Study participants
First, the questionnaire survey was delivered to midwives, nurses (n = 683) working in hospitals in south-eastern Poland. The following inclusion criteria for participation in the study were applied: (1) informed consent to participate in the study, (2) possession of a licence to practice as a midwife and/or nurse, (3) working in a hospital at the time of the survey, as a midwife or nurse, (4) a minimum of two years of clinical practice as a midwife or nurse. The inclusion criterion of a minimum of two years of clinical practice as a nurse or midwife in a hospital setting as used to ensure that participants had sufficient professional experience to assess and reflect on the ethical climate, moral sensitivity, and stress of conscience in their workplace. Additionally, the initial adaptation period is complete and the probability of facing ethical dilemmas during this time increases. Survey questionnaires were distributed to convenience sample of nurses and midwives who volunteered to participate after receiving an explanation of the study’s purpose, details, and data collection process. Respondents were guaranteed anonymity and the option to withdraw at any time. Completed questionnaires were collected confidentially at their stations in sealed envelopes, with collection times arranged in advance with the participants.
Instruments
The following research tools were used:
-
1.
Stress of Conscience Questionnaire (SCQ) (SCQ) developed by Glasberg et al. (2006) to investigate stress of conscience among healthcare professionals1. The SCQ consists of two latent factors: (1) internal demands, and (2) external demands and constraints. Internal demands pertain to individuals’ personal core values and ethical standards, causing stress when their actions or decisions conflict with these principles1. External demands, on the other hand, are influenced by professional or societal values and involve pressures from factors like organizational policies, workload, or societal norms1. The SCQ is composed of 9 two-part items (Part A and Part B) measuring the commonly occurring stressful situations in the clinical setting and the extent to which these situations are perceived as leading to troubled conscience. Part A assesses the frequency of such situations on a 6-point Likert scale, ranging from 0 to 5 (0/never, 1/less than once/6 months, 2/more than once/6 months, 3/every month, 4/every week, and 5/every day). Part B assesses the extent to which they are perceived as leading to troubled conscience, on a visual analogue scale that ranges from 0 (“No, it does not trouble my conscience at all”) to 5 (“Yes, it troubles my conscience greatly”). The SCQ individual item score (the index score) is obtained by multiplying Part A and Part B ratings. The approval for the use of the SCQ was obtained from the author of the tool before conducting the research. The process of translating and adapting the SCQ to Polish conditions was performed with the use of the International Test Commission Guidelines for Translating and Adapting Tests,21. One question was added in the Polish version to the 9-item scale developed by Glasberg et al.1, referring to the provision of services that the nurse or midwife does not accept (question 3A: “Do you sometimes provide services that you do not accept?” and 3B: “Does this give you troubled conscience?”).
-
2.
Hospital Ethical Climate Survey (HECS) was orginally developed by Olson22. In the study the Polish 21-item version of the Hospital Ethical Climate Survey (HECS-Pol) was used23. HECS-Pol is a questionnaire assessed by the respondent on a 5-point Likert scale (from 1 – “almost never true” to 5 – “almost always true”) and consists of 5 subscales examining the relations between the respondent and patients, peers, hospital and managers, physicians. The higher the total result obtained, the more positive the ethical climate of the analyzed organisation. The α-Cronbach’s internal consistency and reliability coefficient for the HESC scale is 0.9323.
-
3.
Moral Sensitivity Questionnaire Revised (MSQ—R) is a nine-item questionnaire developed by Lutzen et al.24 measuring the self-awareness of the moral character of a certain situation. MSQ includes three factors such as: moral burden, moral strength and moral responsibility24. A higher score indicates higher moral sensitivity. In the study the Polish version (MSQ-Pol) was used. The internal consistency of the factors of MSQ-Pol was calculated by means of Cronbach’s alpha (0.827). In the MSQ-Pol a 2-factor solution was used: Factor 1 'moral strength and moral responsibility’ consisted of 5 items, the factor ‘moral burden’ consisted of 4 items.
-
4.
A self-designed questionnaire to collect sociodemographic data such age, sex, education.
Data collection
The study was conducted using Paper-and-Pencil Interviewing method (PAPI) over a 14-month period from March 2019 to December 2020 (the beginning of the COVID-19 pandemic interrupted the collection of surveys, collection resumed in November and December 2020) in hospitals in eastern Poland. A convenience sampling was conducted. The survey questionnaire (n = 683) was delivered to the hospitals after obtaining permission to conduct the study from the hospital management. Respondents who verbally consented to participate and met the inclusion criteria received questionnaires. They were briefed about the study’s purpose and data collection process (test followed by retest). The questionnaires included study details and researcher contact information for queries. First, the questionnaire was delivered to nurses and midwives (n = 683) who agreed to take part in the study and who work in hospitals in the Lubelskie and Podkarpackie voivodeships in Poland. After three weeks the same respondents were invited to take part in the study and 124 retests (of the Polish version of SCQ) were filled and returned correctly. Respondents were assured of the option to withdraw anytime. Completed questionnaires were to be sealed in envelopes and returned to the nurse or midwife in charge, then collected by the researcher on an agreed date. The survey had a return and completion rate of 69.7% (476 respondents), with 97.53% (435) responding before the pandemic and 9.19% (41) during the second wave.
Statistical analysis
The Statistical Package for Social Sciences (SPSS) and AMOS, Version 29.0 was used for statistical analysis of the data (SPSS, Chicago, IL, USA) after the data had been entered into the database created in Microsoft Excel. Descriptive statistics of the collected data were summarized as mean (M), percentages, and standard deviation (SD) values. Statistical significance in the final model was set at p < 0.05. The Pearson’s correlation coefficient (r) test was used to measure the association between the selected variables.
Internal consistency reliability was evaluated by Cronbach’s alpha (> 0.7), item-total correlations (> 0.3) and inter-item correlations (0.2–0.4) Exploratory factor analysis (EFA, PCA method) was used to investigate instrument dimensionality. Kaiser-Meyer Olkin measure of sampling adequacy (KMO) and Bartlett’s test of sphericity were analysed first to determine suitability of the data to undergo factor analysis, the cut of were > 0.6. The varimax orthogonal rotation was performed. Confirmatory factor analysis (CFA) was used to examine the adequacy of the resulting factor model. To evaluate model fit, this study used a range of absolute and incremental model fit indices, including the ratio of chi-square to degrees of freedom (X2/df), comparative fit index (CFI), Tucker Lewis index (TLI); root mean square error of approximation (RMSEA), PCLOSE and SRMR. The Pearson correlation coefficient was computed between the two test/retest sets. Correlations of Stress of Conscience, Moral Sensitivity, and Hospital Ethical Climate are presented with the precise number of the study participants for each item, and only N for the pair of results was considered from the whole study group.
Ethical issues
The research was conducted after obtaining the approval of the Bioethics Committee at the Medical University of Lublin (number: KE-0254/267/2020) and in accordance with the Helsinki Declaration principles. Participants were informed of their right to withdraw at any time. Those who provided written consent took part. Consent and survey responses were collected separately in sealed envelopes to ensure anonymity. Data was entered into a password-protected Excel sheet accessible only to the principal investigator to maintain confidentiality. Informed consent was obtained from all subjects and/or their legal guardian(s).
Results
General characteristics of the participants
The sample consisted 476 of nurses, and midwives, 460 were female (96.6%). The mean age was 36.12 (SD = 10.06) and the average seniority was 14.79 years (SD = 14.66). The detailed results are shown in the Table 1.
Process of validation of the stress of conscience questionnaire
Reliability
All individual items met the cut-off criteria for item-total correlations above 0.3. The internal consistency reliability was satisfactory (total Cronbach’s alpha = 0.837). The results were also consistent if the Part A and Part B questions were measured for reliability separately or as combined index scores (Table 2).
Factor analysis
Exploratory factor analysis (EFA)
Principal component analysis was conducted on the index (i.e. question A multiplied by question B) for all items. The Kaiser–Meyer–Olkin (KMO) was 0.884 and Bartlett’s test of sphericity was significant (chi-square = 1459.16; p < 0.001). The Kaiser criteria of an eigenvalue > 1, the Cattel scree test (Fig. 1) and the rotated PCA (varimax rotation) yielded a two-factor solution which explained 54.26% of the total variance. The rotated factor matrix loadings were greater than 0.5 (Table 2).
Confirmatory factor analysis (CFA)
Factor loadings for the two‐factor model ranged from 0.50 to 0.79 and two latent factors also closely correlated (Fig. 2). The two‐factor model was associated with good model fit (CMIN/DF = 2.639; P-value < 0.001; CFI = 0.961; TLI = 0.948; SRMR = 0.041; RMSEA = 0.059 and PCLOSE = 0.155). In contrast, the one‐factor model fit indicated that some fit indices were not acceptable (CMIN/DF = 6.508; P-value < 0.001; CFI = 0.865; TLI = 0.826; SRMR = 0.068; RMSEA = 0.108 and PCLOSE = 0.000) (Table 2).
The test/retest procedure was assessed using Pearson’s correlation coefficient, which ranged from 0.77 (Internal demands) to 0.85 (Total score).
Correlations of stress of conscience, moral sensitivity, and hospital ethical climate
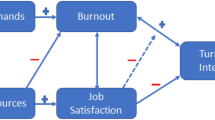
Table 3 shows the correlations of stress of conscience, moral sensitivity and the ethical climate of the hospital. The intensity of SC among the nurses and midwives surveyed increased with the deterioration of selected indicators of the ethical climate of the hospital—relationships with managers, the hospital and doctors; deterioration of relationships in these areas increased the subjects’ stress of conscience, while the overall indicator of the ethical climate of the hospital remained independent of the intensity of SC. The relationship between these variables was weak, as indicated by the Person r coefficient value (Table 3).
The components of SC, internal and external demands, were found to be uncorrelated with any variables—apart from each other and the overall intensity of SC (Table 3).
In addition, the analysis showed that the respondents’ moral sensitivity were higher the more ethical the climate of the hospital in which they worked was. In addition, overall moral sensitivity increased with the intensity of internal SC. Pearson’s r value indicates a weak strength of these correlations and, in the case of the relationship between moral sensitivity and the patient relationship, an average one. Indicators of moral sensitivity correlated with the overall scale score (Table 3).
The individual hospital ethical climate indicators and the overall score correlated strongly and positively with each other (Table 3).
Discussion
In Polish settings, according to literature review, no research tool is available to assess the Stress of the Conscience among nurses and midwives. The present study was conducted to examine selected psychometric properties of the Polish version of the Stress of the Conscience Questionnaire and analyse correlations between stress of conscience moral sensitivity and hospital ethical climate. The process of adaptation, validation and examination of the psychometric properties of the Polish version of the Stress of the Conscience Questionnaire provides the opportunity to fill in the gaps in the current body of knowledge within this issue.
The two fundamental elements in the evaluation process of a measurement instrument are its reliability and validity25. The results obtained in this study confirm that the Polish 10-item version of the Stress of the Conscience Questionnaire is a reliable and stable tool with acceptable psychometric properties. The overall internal consistency of the Polish version of the Stress of the Conscience Questionnaire in terms of Cronbach’s alpha was high (0.837) and revealed good properties of the scale. Cronbach’s alphas in different validation studies of SCQ varied between α = 0.83. In the Glasberg et al. [2006] version1 to α = 0.84 in the Ahilin et al. study26. The two‐factor model was associated with good model fit, whereas the one‐factor model fit indicated that some fit indices were not acceptable.
In the literature, research results demonstrate a positive correlation between stress of conscience and demographic variables such varied as a function of age, years of work and marital status26, professional burnout27 and personalised care28.
The present study investigated the correlation of hospital ethical climate, moral sensitivity and stress of conscience. Analysis of our own results showed that overall moral sensitivity increased with the intensity of internal stress of conscience. Moral sensitivity and stress of conscience were also positively correlated among nurses working in psychiatric wards in Finland and Japan29. Different results were obtained by Borhani et al.30, who found no association between moral sensitivity and moral stress among nurses working in intensive care units. Protection from guilt-related stress on a psychiatric ward was provided by a therapeutic environment in which aggressive behaviour was properly managed31. A negative dimension of moral sensitivity was associated with high levels of stress of conscience32,33. Edvardsson et al.34 found that implementing national guidelines for person-centered care reduced stress of conscience. Similarly, Molin et al.35 showed that more quality time with clients decreases stress of conscience.
The intensity of stress of conscience among the nurses and midwives studied increased with the downgrading of selected indicators of the ethical climate of the hospital—relationships with managers, the hospital and physicians; the deterioration of relationships in these areas increased the subjects’ stress of conscience, while the overall index of the ethical climate of the hospital remained independent of the intensity of stress of conscience. An aspect that ensures the quality and safety of patient care is collaboration within the interdisciplinary team, which can be hindered by inadequate communication36. The creation of a positive ethical climate in the hospital, including positive relationships with colleagues, managers, the hospital and physicians seems essential to reduce the intensity of perceived stress of conscience by nurses and midwives working in hospitals. Interesting results were obtained by Nilsson et al.36, in which nurses working in an intensive care unit during the COVID-19 pandemic found that the events that stressed their conscience the most were those related to a lack of energy to devote to the family as they expected, or those caused by the high professional demands of clinical work36. Sugg et al.37, on the other hand, highlighted deficiencies in the delivery of care among nurses working on COVID-19 wards. These nurses felt that they were unable to provide adequate levels of support, reassurance and interaction with patients, and furthermore had difficulty supporting patients’ emotional wellbeing and mental health. Furthermore, they stated that they felt a lack of maintaining respect for patients’ values, beliefs and dignity37. Subsequent studies have confirmed that factors that protect against conscientious health care workers’ stress include mastery and control of professional responsibilities, a supportive environment on the ward, professional affiliation, and less conflict between colleagues27,31. What is more implementing expert training and ongoing education in communication for nurses is essential for responding adequately and humanely to patients’ expectations38. Also, recent research findings highlights the need to address rationed nursing care among registered and practical nurses to improve teamwork and patient care outcomes in acute care settings determining the further course of investigation39.
Limitations
Many factors may influence nurses and midwives stress of conscience working on the clinical settings. Future research should explore additional factors, considering specific wards and employing qualitative methods. Moreover, as the first study to measure conscientious stress among Polish hospital nurses and midwives using the SCQ-Pol tool, no prior comparable studies exist. Also, participants were recruited from two voivodeships in Poland, limiting the generalizability of our results to regions with similar demographics and age structures of nurses and midwives19. Lastly, some of the surveys were collected during the COVID-19 pandemic, which may have impacted on how the stress of conscience, moral sensitivity and hospital ethical climate were perceived by nurses and midwives. The results may not fully reflect the different experiences of midwives, which may be a topic for future, more directed research. However, we chose to include midwives in the group of nurses in our study due to the lack of significant statistical differences between the two groups (statistical analysis was performed, results indicated that the study group is homogeneous, there were no differences between nurses and midwives: Internal demands; External demands and restrictions and total score of SCQ as well as among study participants before and during COVID-19 pandemic). This may be due to the limited survey population and the exclusion of employees from hospitals converted to treat only COVID-19 patients.
Conclusion
The Polish version of the Stress of Conscience Questionnaire serves as a reliable and valid instrument designed to evaluate the frequency and intensity of stressful situations encountered by healthcare professionals in clinical settings, as well as the resultant troubled conscience they may experience. Implementing the questionnaire allows healthcare institutions to systematically identify and assess common stressful situations and the associated levels of troubled conscience among their staff. This awareness enables targeted interventions and support strategies. This could involve training programs, ethical discussions, or organizational changes to improve working conditions and interpersonal relationships. By prioritizing the ethical climate within hospitals, institutions promote a culture of ethical decision-making and moral sensitivity among healthcare professionals. This not only benefits patient care but also contributes to the professional satisfaction and well-being of staff. Enhancing the ethical climate within hospitals is paramount in fostering supportive relationships among colleagues, managers, and physicians. Such efforts are essential not only for alleviating the perceived stress of conscience among medical staff but also for augmenting their moral sensitivity and overall well-being. By cultivating a culture that prioritizes ethical considerations, mutual respect and positive communication between the therapeutic team healthcare institutions can create environments that promote professional fulfilment and patient-centered care.
Data availability
All data generated and analysed during the current study are not publicly available due to the need to protect the participants’ privacy and confidentiality, but they can be obtained from the corresponding author on a reasonable request.
References
Glasberg, A. L. et al. Development and initial validation of the stress of conscience questionnaire. Nurs. Ethics 13(6), 633–648. https://doi.org/10.1177/0969733006069698 (2006).
Crowell, S., Malpas, J. & Kukla, R. The ontology and temporality of conscience. Continental Philos. Rev. 35, 1–34 (2002).
Langston, D. Conscience and other virtues (Penn State University Press, 2001).
Habermas, J. Moral Consciousness and Communicative Action. 1981/1990, Polity, Cambridge (Original work in German published 1981).
Crowell, S. & Malpas, J. Review article. [Review of the book Transcendental Heidegger]. Parrhesia J. (2008). Available from http://www.parrhesiajournal.org/parrhesia05/parrhesia05_farin.pdf.
Häggström, E., Skovdahl, K., Fläckman, B., Kihlgren, A. L. & Kihlgren, M. To feel betrayed and to feel that you are betraying the older residents: Caregivers’ experiences at a newly opened nursing home. J. Clin. Nurs. 13(6), 687–696. https://doi.org/10.1111/j.1365-2702.2004.00939.x (2004).
Häggström, E. Municipal care for older people: Experiences narrated by caregivers and relatives [Dissertation]. Karolinska Institutet (2005).
Gastmans, C. A fundamental ethical approach to nursing: Some proposals for ethics education. Nurs. Ethics 9(5), 494–507. https://doi.org/10.1191/0969733002ne539oa (2002).
Weaver, K. Ethical sensitivity: State of knowledge and needs for further research. Nurs. Ethics 14(2), 141–155. https://doi.org/10.1177/0969733007073694 (2007).
Park, M., Kjervik, D., Crandell, J. & Oermann, M. H. The relationship of ethics education to moral sensitivity and moral reasoning skills of nursing students. Nurs. Ethics 19(4), 568–580. https://doi.org/10.1177/0969733011433922 (2012).
Dziurka, M. & Dobrowolska, B. Determinants of moral sensitivity of midwives and nurses – current state of knowledge. Nurs. 21st Century 22(1(82), 41–47. https://doi.org/10.2478/pielxxiw-2023-0006 (2023).
Olson, L. Ethical climate in health care organizations. Int. Nurs. Rev. 42, 85–90 (1995).
Lee, E. J. & Chae, Y. R. A. Structural model on the moral distress in clinical nurses. J. Muscle Jt. Health. 29, 194–204. https://doi.org/10.5953/JMJH.2022.29.3.194 (2022).
Lee, J. S. & Lee, S. Y. Ethical climate and patient safety competencies between nurses in long-term care hospital. J. Converg. Cult. Technol. 7, 237–242 (2021).
Noh, Y. G. & Lee, O. S. Factors related to ethical climate of nurses in Korea: A systematic review. J. Health Inform. Stat. 45, 261–272. https://doi.org/10.21032/jhis.2020.45.3.261 (2020).
Lanes, T. C. et al. Evaluation of ethical climate in health services: A systematic review. Rev. Bioética. 28, 718–729. https://doi.org/10.1590/1983-80422020284436 (2020).
Glasberg, A. L. Factors associated with ‘stress of conscience’ in healthcare. Scand. J. Caring. Sci. 22(2), 249–258 (2008).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 61(4), 344–349. https://doi.org/10.1016/j.jclinepi.2007.11.008 (2008).
Number of nurses and midwives registered and employed. Supreme Chamber of Nurses and Midwives. Avaiable in Polish at: https://nipip.pl/liczba-pielegniarek-poloznych-zarejestrowanych-zatrudnionych/.
Ministry of Health. Report of coronavirus infection (SARS-CoV-2). Avaiable in Polish at: https://www.gov.pl/web/koronawirus/wykaz-zarazen-koronawirusem-sars-cov-2.
International Test Commission (2017). International test commission guidelines for translating and adapting tests, Second edition. Available from: http://www.intestcom.org.
Olson, L. L. Hospital nurses’ perceptions of the ethical climate of their work setting. Image J. Nurs. Sch. 30(4), 345–349. https://doi.org/10.1111/j.1547-5069.1998.tb01331.x22 (1998).
Dziurka, M. et al. Hospital ethical climate survey – selected psychometric properties of the scale and results among Polish nurses and midwives. BMC Nursing 21, 295. https://doi.org/10.1186/s12912-022-01067-x (2022).
Lutzen, K., Dahlqvist, V., Eriksson, S. & Norberg, A. Developing the concept of moral sensitivity in health care practice. Nurs. Ethics 13, 187–196 (2006).
Tavakol, M. & Dennick, R. Making sense of Cronbach’s alpha. Int. J. Med. Educ. 2, 53–55. https://doi.org/10.5116/ijme.4dfb.8dfd (2011).
Åhlin, J., Ericson-Lidman, E., Norberg, A. & Strandberg, G. A comparison of assessments and relationships of stress of conscience, perceptions of conscience, burnout and social support between healthcare personnel working at two different organizations for care of older people. Scand. J. Caring Sci. 29, 277–287 (2015).
Juthberg, C., Eriksson, S., Norberg, A. & Sundin, K. Perceptions of conscience in relation to stress of conscience. Nurs. Ethics 14(3), 329–343. https://doi.org/10.1177/0969733007075868 (2007).
Orrung Wallin, A., Jakobsson, U. & Edberg, A. K. Job strain and stress of conscience among nurse assistants working in residential care. J. Nurs. Manag. 23(3), 368–379. https://doi.org/10.1111/jonm.12145 (2015).
Ohnishi, K. et al. Impact of moral sensitivity on moral distress among psychiatric nurses. Nurs. Ethics 26(5), 1473–1483. https://doi.org/10.1177/0969733017751264 (2018).
Borhani, F., Abbaszadeh, A., Mohamadi, E., Ghasemi, E. & Hoseinabad-Farahani, M. J. Moral sensitivity and moral distress in Iranian critical care nurses. Nurs. Ethics 24(4), 474–482. https://doi.org/10.1177/0969733015604700 (2017).
Tuvesson, H. & Eklund, M. Nursing staff stress and individual characteristics in relation to the ward atmosphere in psychiatric in-patient wards. Issues Ment. Health Nurs. 38(9), 726–732. https://doi.org/10.1080/01612840.2017.1324929 (2017).
Zhang, H., Wang, K., Liu, Y. & Chan, D. K. Factors associated with stress of conscience among emergency medical technicians in China. Int. J. Nurs. Pract. 19(Suppl 3), 89–96. https://doi.org/10.1111/ijn.12176 (2013).
Tuvesson, H., Eklund, M. & Wann-Hansson, C. Stress of Conscience among psychiatric nursing staff in relation to environmental and individual factors. Nurs. Ethics 19(2), 208–219. https://doi.org/10.1177/0969733011419239 (2012).
Edvardsson, D., Sandman, P. O. & Borell, L. Implementing national guidelines for person-centered care of people with dementia in residential aged care: Effects on perceived person-centeredness, staff strain, and stress of conscience. Int. Psychogeriatr. 26(7), 1171–1179. https://doi.org/10.1017/S1041610214000258 (2014).
Molin, J., Lindgren, B. M., Graneheim, U. H. & Ringnér, A. Time Together: A nursing intervention in psychiatric inpatient care: Feasibility and effects. Int. J. Ment. Health Nurs. 27(6), 1698–1708. https://doi.org/10.1111/inm.12468 (2018).
Nilsson, U., Odom-Forren, J., Ring, M., van Kooten, H. & Brady, J. M. Stress of conscience of COVID-19 among perianaesthesia nurses having worked in a COVID-ICU during the coronavirus pandemic: an international perspective. BMC Nurs. 21(1), 82. https://doi.org/10.1186/s12912-022-00862-w (2022).
Sugg, H. V. R. et al. Fundamental nursing care in patients with the SARS-CoV-2 virus: Results from the “COVID-NURSE” mixed methods survey into nurses’ experiences of missed care and barriers to care. BMC Nurs. 20(1), 215. https://doi.org/10.1186/s12912-021-00746-5 (2021).
Mazur, J., Kozakiewicz, A., Białorudzki, M. & Izdebski, Z. Selected aspects of patient communication and occupational burnout among nurses working during the COVID-19 pandemic. Nurs. 21st Century 22(3), 139–146. https://doi.org/10.2478/pielxxiw-2023-0022 (2023).
Kohanová, D., Solgajová, A. & Bartoníčková, D. The association of rationed nursing care and the level of teamwork in acute care setting: A cross-sectional study. Nurs. 21st Century 23(2), 100–105. https://doi.org/10.2478/pielxxiw-2024-0017 (2024).
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conceptualization: MD, AJ, BD; collection of the data: MD, AJ, BD; statistical analysis: MD, KJ; investigation: MD, BD; methodology: MD, KJ, BD; writing—original draft: MD; writing—review & editing: MD, BD. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interest
The authors declare no competing interests.
Ethical approval
The research was conducted in accordance with the Declaration of Helsinki after obtaining the approval of the Bioethics Committee at the Medical University of Lublin (number: KE-0254/267/2020). The participants were informed about the anonymity of the study, the voluntary nature of participation, the study objective, the data collection process, and the right to resign from the study at any stage.
Informed consent
Informed consent was obtained from all subjects and/or their legal guardian(s).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Dziurka, M., Jedynak, A., Jurek, K. et al. Correlation of nurses’ and midwives’ stress of conscience with hospital ethical climate and moral sensitivity. Sci Rep 15, 17276 (2025). https://doi.org/10.1038/s41598-025-02180-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-02180-y