Abstract
The study goals were measurement of the choroidal thickness (CT) and investigation of related factors among children. Third-grade students at an elementary school in Tokyo participated in this study. A total of 119 schoolchildren underwent measurements of the axial length (AL), non-cycloplegic objective refraction (SE), and CT. The CT was divided into nine regions: the subfoveal area with a diameter of 1 mm (C0), a 5-mm-diameter circle-C0 (C1), and a 9-mm-diameter circle (C2); each was further divided into four quadrants. The SE, AL, and C0 CT were, respectively, − 1.57 ± 1.56 diopters, 23.39 ± 0.80 mm, and 297.73 ± 57.88 μm. Multiple regression analysis showed that the time spent using a computer was associated significantly with the CT in the C0 and the inferior C2 (C0: β = -0.728, P = 0.028; inferior C2: β = -0.527, P = 0.048), and the reading distance was associated significantly with the CT in the superior and nasal C2 (superior, β = 1.664, P = 0.007; nasal, β = 1.128, P = 0.015). In addition, time spent using smartphones, tablets, or handheld gaming devices was associated significantly with the CT in the superior and inferior C2 (superior C2: β = 0.259, P = 0.018; inferior C2: β = 0.262, P = 0.013). In conclusion, reading distance and time spent on digital devices may be associated with choroid thickness in children.
Similar content being viewed by others
The prevalence of myopia is increasing globally, particularly in East Asia and North America, and has become a significant public health issue1 The incidence of high myopia and pathological myopia, which pose a threat in later years, is also increasing worldwide. Some reports have suggested that by 2050, approximately half of the global population will be myopic, with about 10% having high myopia2 Japan is no exception to this trend, and we previously reported the high prevalence rates of myopia among preschool children3. elementary school students, and junior high school students in Tokyo4.
High myopia, which alters the shape of the eyeball, can lead to various eye diseases that cause blindness, such as retinal detachment, glaucoma, optic neuropathy, myopic maculopathy, and myopic choroidal neovascularization5,6 According to Bullimore et al., the progression of myopia by 1 diopter (D) increases the risk of blindness, myopic maculopathy, retinal detachment, and glaucoma by 24–31%, 58%, 30%, and 20%, respectively. Moreover, controlling myopia by 1 D can reduce the incidence of myopic maculopathy, retinal detachment, and glaucoma by 37%, 23%, and 17%, respectively, indicating that myopia control can prevent vision-impairing conditions6,7 A correlation between the age of onset of myopia and its severity also was reported, with an earlier onset age associated with higher degrees of myopia in the future8 Therefore, it is considered crucial to control the progression of myopia from an early age in childhood to prevent future high myopia.
Although the mechanism of myopia progression remains unclear, several environmental factors, such as near work1,9 and outdoor activity time1,9,10,11, are highly likely to be related to myopia. Several studies also have reported an association between myopia and choroidal thinning12,13,14.
Understanding the impact of environmental factors on the choroidal thickness (CT) could potentially lead to the prevention of myopia onset and the progression to high myopia. In addition to studies reporting factors that influence the CT, several reports also have examined the relationship between the CT and environmental factors. For example, it was reported previously that 2 h of outdoor activity temporarily thins the choroid15, and furthermore, choroidal thinning has been associated with rapid eye growth16. Conversely, one study reported a 13 ± 22 μm increase in the CT in children aged 10 to 15 years after 18 months of outdoor exercise (30 min/day)17, while another reported an increase in CT following daily morning light therapy18 These findings indicate that the current evidence remains inconclusive. In addition, other environmental factors, such as aerobic exercise, also have been shown to transiently increase the CT immediately after activity19,20 However, no studies have evaluated the associations between environmental factors, including lifestyle habits, and CT by subdividing the choroid into specific regions. Therefore, we measured the CT of elementary school students and conducted a survey on lifestyle and other factors to investigate the environmental factors affecting the CT.
Methods
Study design and study populations
This investigation was a school based, cross-sectional study conducted among third-grade students at a public elementary school in Tokyo, Japan, in July 2023. The Ethics Committee of the Keio University School of Medicine approved this study, which adhered to the Declaration of Helsinki. Informed consent was obtained from all subjects or their legal guardians. Among those who provided parental consent and completed the questionnaire (n = 135), students with available CT data (n = 124) were included in the analysis. After excluding children undergoing myopia treatment, i.e., low-concentration atropine or orthokeratology (n = 5), 119 students were analyzed (Supplementary Fig. S1). Although a history of eye diseases affecting visual function also was an exclusion criterion, no such children were identified.
Measures
The participants underwent ophthalmologic examinations, which included measuring refractive errors using autorefractometry and assessing ocular biometric factors such as axial length (AL), central corneal thickness, corneal curvature, anterior chamber depth, lens thickness, and CT. Height and weight also were recorded. Refraction and other biometric factors were measured objectively in a noncycloplegic state using the HOYA iTrace Surgical Workstation (Tracey Technologies). The AL was measured by noncontact optical biometry using a swept-source optical coherence tomography (OCT) biometer (IOLMaster 700, Carl Zeiss Meditec AG). We recorded the AL 10 times and averaged the data. The CT was measured automatically around 12 PM using the Xephilio OCT-S1 (Canon Medical Systems Corporation), and a CT map was created using the OCT Research Tool Ver. 2.0 (Canon Medical Systems Corporation). The CT map was created using the default settings of the software and divided into nine regions (Fig. 1) as follows: first, a circle with a 1-mm diameter was defined as the C0 region. The area subtracting the C0 region from a 5-mm-diameter circle was defined as the C1 region. Further, the area subtracting the 5-mm-diameter circle from a 9-mm-diameter circle was defined as the C2 region. A total of nine regions were investigated: the C0 and C1 and C2 regions each divided into four quadrants (temporal, superior, nasal, and inferior). The optic disc was excluded; it was considered as a 1.5-mm-diameter area.
The 9 regions of the choroid. A central circle (C0) with a 1-mm diameter was created around the macula. A 5-mm diameter circle (C1) and a 9-mm diameter circle (C2) were then defined, with C1 representing the area between 1 mm and 5 mm, and C2 representing the area between 5 mm and 9 mm. Both C1 and C2 were divided into four equal regions.
Children and their parents completed a questionnaire that included questions about outdoor activity time, near work activities, and family history of myopia. The mean number of hours spent outdoors daily was calculated using the formula: [(hours spent on a weekday) × 5 + (hours spent on a weekend day) × 2]/7.4
Regarding near work activities, participants were asked to estimate the time spent using computers, smartphones, tablets, handheld gaming devices, reading/studying, and reading distance. Among these, smartphones, tablets, and handheld gaming devices were considered equivalent near work activities, and their total time was compared.
Statistical analysis
We included only the data from the right eyes for the analysis. First, using Tukey’s test, we compared the CTs among the nine regions. We then calculated Pearson’s correlation coefficients to examine the correlation between CT in the C0 region and non-cycloplegic spherical equivalent (SE), and between the CT in the C0 region and AL. Subsequently, we conducted simple linear regression analysis. The CT in each region was set as the dependent variable, and independent variables included gender, height, AL, factors obtained from the questionnaire (outdoor activity time, computer usage time, smartphone/tablet/handheld gaming device usage time, reading/studying time, reading distance, and family history of myopia). Finally, we performed multiple regression analysis. Similar to simple regression analysis, the CT in each region was set as the dependent variable, and independent variables included factors with a P < 0.25 from the simple regression analysis, selected for each region using the forced entry method evaluation. Furthermore, the population was stratified into two groups based on a reading distance of 30 cm11,21,22,23 and outdoor activity time of 2 hours11,24 as reported previously. For each stratification, comparisons of CT in each region between the two groups were analyzed using the Mann–Whitney U test.
All statistical analyses were conducted using SPSS software, version 29 (IBM Inc.). All P values were two-sided, and P < 0.05 was considered statistically significant. The variance inflation factor (VIF) among all variables was below 10 in our multiple regression analyses, indicating a low risk of multicollinearity issues. Moreover, since there were no school-age children with an axial length of 26 mm or greater, CT correction was not applied.
Results
In this study, we defined myopia as a SE of -0.5 diopter (D) or less. Table 1 shows the background of the 119 analyzed children (66 boys). The prevalence of myopia was 79.8%. The mean (standard deviation [SD]) SE was − 1.57 (1.56) D, the mean (SD) AL was 23.39 (0.80) mm, and the mean (SD) CT in the C0 region was 297.73 (57.88) µm.
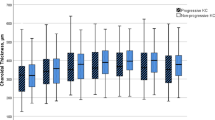
Figure 2 compares the CT across the four quadrants of the C1 and C2 regions. In all regions, the CT was thickest in the temporal region, followed by the superior, inferior, and nasal quadrants, respectively. Significant differences were observed in the regions excluding the superior and inferior quadrants of the C1 region.
Figure 3a shows the correlation between the CT in the C0 region and SE; Fig. 3b shows the correlation between the CT in the C0 region and AL. The CT in the C0 region was significantly positively correlated with the SE (R = 0.215, P = 0.019). Specifically, for every 1-D increase in myopia, the CT decreased by 8.0 μm. Additionally, the CT in the C0 region was significantly negatively correlated with the AL (R = -0.330, P < 0.001). For every 1-mm increase in the AL, the CT in the C0 region decreased by 24.1 μm.
We present the results of multiple regression analysis using factors selected from simple regression analysis. For the C0 region, the computer usage time was associated significantly (β = − 0.728; 95% confidence interval [CI], − 1.376 to − 0.080; P = 0.028) with the CT (Table 2). Across all the C1 regions and C2 temporal region, no environmental factors were associated significantly with the CT (Supplementary Tables S1–S5). In the C2 superior region, the smartphone/tablet/handheld gaming usage time (β = 0.259; 95% CI, 0.045 to 0.474; P = 0.018) and reading distance (β = 1.664; 95% CI, 0.468 to 2.860; P = 0.007) were associated significantly with the CT (Supplementary Table S6). Similarly, in the C2 nasal region, the reading distance also was associated significantly (β = 1.128; 95% CI, 0.224 to 2.032; P = 0.015) with the CT (Table 3). In the C2 inferior region, the computer usage time (β = − 0.527; 95% CI, − 1.050 to − 0.005; P = 0.048) and the smartphone/tablet/handheld gaming usage time (β = 0.262; 95% CI, 0.058 to 0.467; P = 0.013) were associated significantly with the CT (Supplementary Table S7). Overall, the AL was associated with the CT across all regions except the C2 nasal region. Furthermore, a stratified analysis based on reading distance showed that participants with a reading distance of 30 cm or longer had a thicker choroid across all regions C0, C1, and C2 compared to those with a reading distance shorter than 30 cm. A statistically significant difference was particularly observed in the C2 superior region (Supplementary Table S8). Similarly, when stratified by outdoor activity time using a 2-hour cutoff, no clear trend in CT was observed between the two groups (Supplementary Table S9). These findings indicate that no contradictory or inverse associations emerged compared with the aforementioned results.
To summarize, a longer AL generally was associated with thinner choroid across all regions except the C2 nasal region. Longer computer usage time was associated with a thinner choroid in the C0 and C2 inferior regions, while longer smartphone/tablet/handheld gaming usage time was associated with a thicker choroid in the C2 superior and inferior regions. Additionally, longer reading distance was linked to a thicker choroid in the C2 superior and nasal regions.
Discussion
Multiple reports have been published on the CT in relation to age and ethnicity,14 CT and blood flow,25,26 and CT and accommodative function27,28,29 Our study specifically identified a significant association between the CT in the disc-macular area and the reading distance.
When we compared the current participants with those of similar age in previous studies,30,31,32,33,34,35,36 the average CT (C0) of our subjects was slightly thinner to approximately the same degree. Because no published studies divided the choroidal region or set detailed age groups as in the current study, precise comparisons were challenging. In addition, differences in measurement times also may have affected the variations in the results due to diurnal fluctuations. For example, a previous study30 of healthy children aged 3 to 16 years reported a subfoveal CT of 332.33 ± 73.07 μm, with subgroup analyses showing 322.71 ± 76.21 μm for 6- to 8-year-olds and 340.86 ± 68.33 μm for 9- to 11-year-olds. Furthermore, when we compared the average CT by area in our study, the choroid was observed to thin from the temporal to the nasal side, consistent with previous reports involving children,30,31 adults,12 and both32 In addition, there was a positive correlation between the CT and refractive error, with our study indicating that a 1-D increase in myopia resulted in 8.0 μm of choroidal thinning, which agreed with previous findings of 10.0 µm14,37 and 15 μm38 There was also a negative correlation between the CT and AL, with a 1-mm increase in the AL resulting in 24.1 μm of choroidal thinning, which was comparable to previous results of 16.2 μm,37 21 μm,14 and 32 μm38.
The results of our univariate and multivariate analyses identified near work as an environmental factor related to the CT. Specifically, computer usage time and reading distance were associated with choroidal thinning. An important report by Yokoi et al.39 examined the choroid by region and found that 83% of adults with pathological myopia and patchy atrophy had choroidal thinning or atrophy between the optic disc and macula in childhood. This suggests that the “optic disc-macular area” is critical in myopia progression, and that maintaining the CT in this area during childhood may be important for preventing future pathological myopia. In our study, the optic disc-macular area corresponded to the C1 nasal and C2 nasal regions, and the reading distance was the environmental factor that affected that area. Therefore, maintaining a longer reading distance in childhood could potentially prevent choroidal thinning in this area and reduce the risk of future pathological myopia.
Recent reports have suggested that outdoor activity time is important for controlling myopia,4,9,10,40,41,42 but we did not find an association with CT in the current study. This may have occurred because our study was conducted in one elementary school with an average outdoor activity time of 82 ± 49 min daily, which is less than 2 h, resulting in minimal individual differences.
Various studies have reported on the impact of digital devices such as smartphones on CT and myopia,43,44,45,46,47 with no definitive conclusions. A systematic review47 of 15 studies that included 49,789 individuals reported that seven studies showed a relationship between screen exposure time and myopia. Among the five studies that conducted meta-analyses, screen exposure time was unrelated to the prevalence or onset of myopia.
Limitations.
This study had several limitations. First, it was a cross-sectional survey conducted at one institution and in children in one school grade. Therefore, the participants were relatively limited, and the findings might not have fully reflected the overall trends in children. Second, we did not use cycloplegics because we conducted the study during regular school classes. Cycloplegic autorefraction is the criterion standard according to several studies and the white paper presented by the International Myopia Institute48,49,50 Considering this, it is possible that the refraction reported in the current study was overestimated. Nonetheless, since the ALs were measured, we considered that the degree of myopia was assessed accurately through the AL. Third, there was recall bias since the lifestyle data were collected from a questionnaire. For example, the reported usage time for each type of digital device may not be entirely accurate. In the present study, we performed separate analyses for handheld and stationary digital devices to examine whether the outcomes differed by device type. However, aggregating all devices under a single category of “digital device use” may potentially improve the accuracy of the data. Furthermore, the incorporation of devices51,52 to objectively assessing near work time and distance will be considered in future research.
Thus, while handheld digital devices such as smartphones may impact myopia, further objective measurements are necessary to definitively consider screen exposure time as an independent risk factor. The current study found an association between longer use of smartphones, tablets, and handheld games and thicker choroids, suggesting the need for prospective studies.
Conclusions
Childhood CT is correlated significantly with the refractive error and AL. In particular, a longer reading distance, which is associated with the region between the optic nerve head and the macula, was correlated with certain ocular parameters in this study. Although causality cannot be inferred due to the cross-sectional nature of the study, these findings suggested that reading distance may be a relevant factor affecting the choroid. Further longitudinal studies with larger sample sizes are needed to investigate this association more comprehensively.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Grzybowski, A., Kanclerz, P., Tsubota, K., Lanca, C. & Saw, S. M. A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol. 20, 27. https://doi.org/10.1186/s12886-019-1220-0 (2020).
Holden, B. A. et al. Global prevalence of myopia and high myopia and Temporal trends from 2000 through 2050. Ophthalmology 123, 1036–1042. https://doi.org/10.1016/j.ophtha.2016.01.006 (2016).
Maruyama, T. et al. Children in Tokyo have a long sustained axial length from age 3 years: the Tokyo myopia study. J. Clin. Med. 11. https://doi.org/10.3390/jcm11154413 (2022).
Yotsukura, E. et al. Current prevalence of myopia and association of myopia with environmental factors among schoolchildren in Japan. JAMA Ophthalmol. 137, 1233–1239. https://doi.org/10.1001/jamaophthalmol.2019.3103 (2019).
Mimura, R. et al. Ultra-Widefield retinal imaging for analyzing the association between types of pathological myopia and posterior Staphyloma. J. Clin. Med. 8. https://doi.org/10.3390/jcm8101505 (2019).
Haarman, A. E. G. et al. The complications of myopia: A review and Meta-Analysis. Invest. Ophthalmol. Vis. Sci. 61, 49. https://doi.org/10.1167/iovs.61.4.49 (2020).
Bullimore, M. A. et al. The risks and benefits of myopia control. Ophthalmology 128, 1561–1579. https://doi.org/10.1016/j.ophtha.2021.04.032 (2021).
Chua, S. Y. et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol. Opt. 36, 388–394. https://doi.org/10.1111/opo.12305 (2016).
Rose, K. A. et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 115, 1279–1285. https://doi.org/10.1016/j.ophtha.2007.12.019 (2008).
He, X. et al. Time outdoors in reducing myopia: A School-Based cluster randomized trial with objective monitoring of outdoor time and light intensity. Ophthalmology 129, 1245–1254. https://doi.org/10.1016/j.ophtha.2022.06.024 (2022).
Zhang, D. et al. Prevalence and associated factors of myopia among school students in Shenyang, China: a cross-sectional study. Front. Public. Health. 11, 1239158. https://doi.org/10.3389/fpubh.2023.1239158 (2023).
Ohsugi, H., Ikuno, Y., Oshima, K. & Tabuchi, H. 3-D choroidal thickness maps from EDI-OCT in highly myopic eyes. Optom. Vis. Sci. 90, 599–606. https://doi.org/10.1097/OPX.0b013e3182924017 (2013).
Meng, Q. Y. et al. Choroidal thickness, myopia, and myopia control interventions in children: a Meta-analysis and systemic review. Int. J. Ophthalmol. 16, 453–464. https://doi.org/10.18240/ijo.2023.03.17 (2023).
Kobia-Acquah, E., Flitcroft, D. I., Lingham, G., Paudel, N. & Loughman, J. Choroidal thickness profiles and associated factors in myopic children. Optom. Vis. Sci. 100, 57–66. https://doi.org/10.1097/opx.0000000000001973 (2023).
Lou, L. & Ostrin, L. A. The outdoor environment affects retinal and choroidal thickness. Ophthalmic Physiol. Opt. 43, 572–583. https://doi.org/10.1111/opo.13107 (2023).
Read, S. A. Ocular and enviornmental factors associated with eye growth in childhood. Optom. Vis. Sci. 93, 1031–1041 (2016).
Read, S. A., Alonso-Caneiro, D., Vincent, S. J. & Collins, M. J. Longitudinal changes in choroidal thickness and eye growth in childhood. Invest. Ophthalmol. Vis. Sci. 56, 3103–3112. https://doi.org/10.1167/iovs.15-16446 (2015).
Read, S. A. et al. Daily morning light therapy is associated with an increase in choroidal thickness in healthy young adults. Sci. Rep. 8, 8200. https://doi.org/10.1038/s41598-018-26635-7 (2018).
Insa-Sánchez, G. et al. Choroidal thickness and volume modifications induced by aerobic exercise in healthy young adults. Ophthalmic Res. 64, 604–612. https://doi.org/10.1159/000511201 (2021).
Sayin, N., Kara, N., Pekel, G. & Altinkaynak, H. Choroidal thickness changes after dynamic exercise as measured by spectral-domain optical coherence tomography. Indian J. Ophthalmol. 63, 445–450. https://doi.org/10.4103/0301-4738.159884 (2015).
Huang, H. M., Chang, D. S. & Wu, P. C. The association between near work activities and myopia in Children-A systematic review and Meta-Analysis. PLoS One. 10, e0140419. https://doi.org/10.1371/journal.pone.0140419 (2015).
Tang, S. M. et al. Effect of myopic undercorrection on habitual reading distance in schoolchildren: the Hong Kong children eye study. Ophthalmol. Ther. 12, 925–938. https://doi.org/10.1007/s40123-022-00628-2 (2023).
Ip, J. M. et al. Role of near work in myopia: findings in a sample of Australian school children. Invest. Ophthalmol. Vis. Sci. 49, 2903–2910. https://doi.org/10.1167/iovs.07-0804 (2008).
Wu, P. C. et al. Increased time outdoors is followed by reversal of the Long-Term trend to reduced visual acuity in Taiwan primary school students. Ophthalmology 127, 1462–1469. https://doi.org/10.1016/j.ophtha.2020.01.054 (2020).
Liang, X. et al. Investigation of choroidal blood flow and thickness changes induced by near work in young adults. Curr. Eye Res. 48, 939–948. https://doi.org/10.1080/02713683.2023.2222234 (2023).
Liu, Y., Wang, L., Xu, Y., Pang, Z. & Mu, G. The influence of the choroid on the onset and development of myopia: from perspectives of choroidal thickness and blood flow. Acta Ophthalmol. 99, 730–738. https://doi.org/10.1111/aos.14773 (2021).
Nickla, D. L. & Wallman, J. The multifunctional choroid. Prog Retin Eye Res. 29, 144–168. https://doi.org/10.1016/j.preteyeres.2009.12.002 (2010).
Kaphle, D., Schmid, K. L., Suheimat, M., Read, S. A. & Atchison, D. A. Central and peripheral choroidal thickness and eye length changes during accommodation. Ophthalmic Physiol. Opt. 43, 311–318. https://doi.org/10.1111/opo.13084 (2023).
Woodman-Pieterse, E. C., Read, S. A., Collins, M. J. & Alonso-Caneiro, D. Regional changes in choroidal thickness associated with accommodation. Invest. Ophthalmol. Vis. Sci. 56, 6414–6422. https://doi.org/10.1167/iovs.15-17102 (2015).
Nadeem, S. Macular choroidal thickness and correlations in a healthy pediatric South Asian cohort: A spectral domain optical coherence tomography study. J. Biophotonics. 16, e202300039. https://doi.org/10.1002/jbio.202300039 (2023).
Xiong, F. et al. Subfoveal choroidal thickness in myopia: an OCT-Based study in young Chinese patients. J. Ophthalmol. 2020, 5896016. https://doi.org/10.1155/2020/5896016 (2020).
Zhu, D. et al. Choroidal thickness in school children: the gobi desert children eye study. PLoS One. 12, e0179579. https://doi.org/10.1371/journal.pone.0179579 (2017).
Prousali, E., Dastiridou, A., Ziakas, N., Androudi, S. & Mataftsi, A. Choroidal thickness and ocular growth in childhood. Surv. Ophthalmol. 66, 261–275. https://doi.org/10.1016/j.survophthal.2020.06.008 (2021).
Bidaut-Garnier, M. et al. Choroidal thickness measurement in children using optical coherence tomography. Retina 34, 768–774. https://doi.org/10.1097/IAE.0b013e3182a487a4 (2014).
Nagasawa, T. et al. Macular choroidal thickness and volume in healthy pediatric individuals measured by swept-source optical coherence tomography. Invest. Ophthalmol. Vis. Sci. 54, 7068–7074. https://doi.org/10.1167/iovs.13-12350 (2013).
Ruiz-Moreno, J. M. et al. Macular choroidal thickness in normal pediatric population measured by swept-source optical coherence tomography. Invest. Ophthalmol. Vis. Sci. 54, 353–359. https://doi.org/10.1167/iovs.12-10863 (2013).
Biyik, K. Z. et al. Subfoveal choroidal thickness at age 9 years in relation to clinical and perinatal characteristics in the population-based generation R study. Acta Ophthalmol. 98, 172–176. https://doi.org/10.1111/aos.14178 (2020).
Wei, W. B. et al. Subfoveal choroidal thickness: the Beijing eye study. Ophthalmology 120, 175–180. https://doi.org/10.1016/j.ophtha.2012.07.048 (2013).
Yokoi, T. et al. Peripapillary diffuse chorioretinal atrophy in children as a sign of eventual pathologic myopia in adults. Ophthalmology 123, 1783–1787. https://doi.org/10.1016/j.ophtha.2016.04.029 (2016).
Guo, Y. et al. Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology 120, 277–283. https://doi.org/10.1016/j.ophtha.2012.07.086 (2013).
Wu, P. C. et al. Myopia prevention and outdoor light intensity in a School-Based cluster randomized trial. Ophthalmology 125, 1239–1250. https://doi.org/10.1016/j.ophtha.2017.12.011 (2018).
Singh, N. K. et al. Prevalence of myopia and associated risk factors in schoolchildren in North India. Optom. Vis. Sci. 96, 200–205. https://doi.org/10.1097/opx.0000000000001344 (2019).
Hansen, M. H. et al. Low physical activity and higher use of screen devices are associated with myopia at the age of 16–17 years in the CCC2000 eye study. Acta Ophthalmol. 98, 315–321. https://doi.org/10.1111/aos.14242 (2020).
Guan, H. et al. Impact of various types of near work and time spent outdoors at different times of day on visual acuity and refractive error among Chinese school-going children. PLoS One. 14, e0215827. https://doi.org/10.1371/journal.pone.0215827 (2019).
Enthoven, C. A. et al. The impact of computer use on myopia development in childhood: the generation R study. Prev. Med. 132, 105988. https://doi.org/10.1016/j.ypmed.2020.105988 (2020).
Foreman, J. et al. Association between digital smart device use and myopia: a systematic review and meta-analysis. Lancet Digit. Health. 3, e806–e818. https://doi.org/10.1016/s2589-7500(21)00135-7 (2021).
Lanca, C. & Saw, S. M. The association between digital screen time and myopia: A systematic review. Ophthalmic Physiol. Opt. 40, 216–229. https://doi.org/10.1111/opo.12657 (2020).
Flitcroft, D. I. et al. IMI - Defining and classifying myopia: A proposed set of standards for clinical and epidemiologic studies. Invest. Ophthalmol. Vis. Sci. 60, M20–m30. https://doi.org/10.1167/iovs.18-25957 (2019).
Gwiazda, J. et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest. Ophthalmol. Vis. Sci. 44, 1492–1500. https://doi.org/10.1167/iovs.02-0816 (2003).
Wolffsohn, J. S. et al. IMI - Myopia control reports overview and introduction. Invest. Ophthalmol. Vis. Sci. 60, M1–m19. https://doi.org/10.1167/iovs.18-25980 (2019).
Bhandari, K. R. & Ostrin, L. A. Objective measures of viewing behaviour in children during near tasks. Clin. Exp. Optom. 105, 746–753. https://doi.org/10.1080/08164622.2021.1971049 (2022).
Zhang, Y. et al. Clouclip combined with a questionnaire on the influence factors of myopia in children. Front. Pediatr. 11, 1228257. https://doi.org/10.3389/fped.2023.1228257 (2023).
Acknowledgements
We thank Taro Nakamura, the principal of the elementary school; Kazue Sasaki, the school nurse of the elementary school; Toshihiro Abe, the chief coordinator of the school home community; Takashi Tominaga, Yuta Shigeno, Masaharu Takeuchi, and Emiko Kagawa for assistance with the examination; Tomoko Omori, Rika Kobayashi, Natsumi Yamada, Asuka Kobayashi, Kasumi Ishibashi, Noa Tashiro, Nichika Moriyama, Yurina Nakajima, Nana Maeda, Rikako Takeuchi and Kouko Douken for assistance with the measurements, Ryo Takemura for providing statistical advice; and Lynda Charters for editing the English in this manuscript.
Funding
This work was supported by the Charitable Trust Fund for Ophthalmic Research in Commemoration of Santen Pharmaceutical’s Founder and JINS Endowed Research Laboratory for Myopia.
Author information
Authors and Affiliations
Contributions
A.H. and E.Y. had full access to all study data and take responsibility for the integrity of the data and the accuracy of the data analysis. E.Y. and H.T. contributed to the conception and design of the study. A.H. and E.Y. were responsible for data acquisition, analysis, and interpretation. A.H., E.Y., and H.T. drafted the manuscript. All authors critically revised the manuscript for important intellectual content. A.H. conducted the statistical analysis. K.T., T.K., H.T., and K.N. supervised the study.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Hashimoto, A., Yotsukura, E., Ogawa, M. et al. Thicker peripapillary choroid may be associated with behavioral factors in Tokyo’s children. Sci Rep 15, 17868 (2025). https://doi.org/10.1038/s41598-025-02825-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-02825-y