Abstract
This study aimed to evaluate the efficacy of intra-articular injection of 5% Dextrose (D5W) prolotherapy in treatment symptoms of Temporomandibular Joint (TMJ) Disc Displacement without Reduction (DDwoR) with limited mouth opening (Closed-Lock) of patients’refractory to pharmacological and physical therapy. This pilot study included twenty female patients suffering from symptoms of DDwoR with limited mouth opening mentioned in the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD). Participants were randomly assigned into two groups; the study group patients were injected with D5W, while the control group patients were injected with 0.9% normal saline (NS). The measured variables included pain intensity on opening and closing according to the Numerical Rating Scale (NRS). Moreover, Unassisted Maximum Interincisal Opening (MIO) was measured with a millimeter-scaled ruler. These were measured before and four times after injection (2 weeks, 2 months, 6 months, and 12 months). The level of significance was set at α = 0.05. Gradual increase in MIO values in both groups with significant difference in the last time (p < 0.001), while values of NRS in both groups decreased with a significant difference in favor of the study group (p < 0.001), except for the last time (p = 0.065). In conclusion, D5W significantly affects relieving pain in female closed-lock patients.
Similar content being viewed by others
Introduction
Internal Derangement (ID) is a type of Temporomandibular Joint Disorder (TMD) that refers to a disorder in the relationship between the mandibular condyle, articular disc, and articular eminence. This disorder leads to displacement of the articular disc, often anteriorly or anteromedially1, and the clinical manifestations of this disorder are variable. According to recent literature, TMD affects 34% of the population2.
Disc Displacement without Reduction (DDwoR) of the (TMJ) is a less common ID. Its prevalence among TMD is estimated at 2–8%3,4.
DDwoR is divided depending on a mandibular range of motion into a displacement with limited mouth opening (Closed-lock) and another without limited mouth opening according to the taxonomy of the Diagnostic Criteria for Temporomandibular Disorders (DC/TMD), the essential characteristic of the first is a severe limitation of the mouth opening that interferes with the ability to eat5, this is after elongation of the joint ligaments and the loss of the elasticity of the superior retrodiscal lamina6, which makes it difficult for the disc to return to its physiological position, and results pain from the excessive and continuous load on the retrodiscal tissues due to its direct articulation with the head of the condyle and preventing the displaced disc from completing its translational movement7.
Closed-Lock (CL) is usually diagnosed by a sudden and continuous limitation of mouth opening after a history of clicking8; the most common cause of it is trauma. This case may be microtrauma, accompanied by parafunctional habits, or macrotrauma, such as a hit on the jaw9. An annoying disorder usually prevents the patient from performing his daily activities. The practitioner may stand perplexed in front of his inability to relieve his patient, so treatment is recommended when the pain does not go away spontaneously10. Therapeutic strategies for CL range from conservative treatments to surgical intervention; it should be initially treated by the most straightforward and least invasive intervention11; most methods of conservative management seem to be effective in decreasing pain and re-establishing the physiological range of motion and include education and counselling, pharmacotherapy, exercise therapy, mandibular manipulation and occlusal splints therapy12. Failure of conservative treatment may force the specialist to move to more invasive treatments such as Intra-articular injection (IAI) or arthrocentesis. The standard active substances currently used for injection to treat TMD are autologous blood products as a stimulator of tissue regeneration and hyaluronic acid as a viscosupplementation13,14. Combining more than one substance in injection after arthrocentesis appears to have a promising future15. Recently, NSAIDs have been used, but the results have been conflicting. Therefore, further clinical studies are needed16. Most injections are performed after arthrocentesis, although some clinicians perform injections without arthrocentesis17.
Dextrose prolotherapy (DPT) is a non-invasive technique that stimulates the proliferation of the tendons and ligaments18 and promotes joint healing by intra or periarticular dextrose injection. It is used for the treatment of tendinopathies19. Recently, it has been proven to be a successful technique for the treatment of symptoms related to the ID of TMJ20,21 and especially hypermobility22, advised to apply it for patient’s refractory to conservative treatments23. It is desirable because it is effective and low-cost.
The mechanism of action of DPT has been unclear until now18. However, studies have shown that low concentrations of dextrose solution enhance the wound-healing process through growth factors. Moreover, high concentrations (hypertonic) cause local cell death through their osmotic effect, which results in the healing of the affected area24.
In recent literature, subcutaneous or perineural injections of 5% dextrose (D5W) have been found to have a neurosensory effect that contributes to alleviating pain resulting from neurogenic inflammation25,26.
High concentrations of dextrose have been used to treat ID21,27. To the best of our knowledge, no study has evaluated the effect of low concentrations (less than 10%) on it, especially D5W, which has proliferative analgesic characteristics.
In the absence of consensus on the optimal treatment for DDwoR28, and because a good percentage of DDwoR patients do not improve spontaneously without treatment, it is essential to treat all patients at the onset of symptoms to avoid possible future consequences. It is difficult to predict the possibility of developing osteoarthritis of TMJ29. The study aims to evaluate the effectiveness of the D5W injection within retrodiscal tissues on the main symptoms associated with CL compared with normal saline after the failure of initial conservative therapies to test the hypothesis that D5W is more effective in relieving the symptoms.
Materials and methods
Study design and ethical approval
This pilot study conducted on female patients diagnosed with unilateral CL who came to the Department of Oral and Maxillofacial Surgery at the Faculty of Dentistry at Damascus University between October 2022 and April 2024. The study followed the Helsinki Declaration for the ethical principles for medical research involving human subjects.
The randomized controlled clinical trial was retrospectively registered on www.isrctn.com (Registration ID: ISRCTN63941479 on 21/01/2025) and approved by the Local Research Ethics Committee of the Faculty of Dentistry (DN-02092024-306).
Inclusion criteria
-
1.
Female patients aged 18–35 years presenting with symptoms of unilateral DDwoR with limited mouth opening (≤ 2 months) mentioned in the DC/TMD, maximum assisted opening < 40 mm, and complain that restricted mouth opening interferes with the ability to eat, history of joint clicking followed by sudden limiting of the mouth opening and pain without clicking.
-
2.
Initial conservative treatments (pharmacological-physical) failed to improve their symptoms.
-
3.
Level pain ≥ 5 on the Numeric Rating Scale (NRS).
Exclusion criteria
-
1.
Allergy to dextrose.
-
2.
Having parafunctional habits.
-
3.
Restriction of mouth opening by spasm muscles.
-
4.
Previous exposure to IAI.
-
5.
Unwillingness to continue.
Randomization
A resident fellow in the Department of Oral and Maxillofacial Surgery divided the patients into two equal groups after giving each one a code with sequential numbers (1,2,3, etc.) and randomly allocating them using the randomization tool https://www.randomizer.org/.
The random distribution was hidden in envelopes and given to the treating physician before treatment. The study group patients were injected with 5% Dextrose (D5W), while the control group patients were injected with 0.9% Normal Saline (NS).
Blinding
Both materials were prepared and placed in identical sterile cartridges by a resident physician in the Department of Oral and Maxillofacial Surgery, who marked them with the number (1 or 2). Neither the patients nor the researchers knew what the number meant, and it remained unknown to everyone except that physician until the end of the follow-up period for all patients.
Requirement and eligibility criteria
The principal investigator (Y. S. T.) met patients who complained of click, pain, difficulty opening the mouth, and other TMD symptoms and found that they had one of TMD after reviewing their medical and clinical history. After careful clinical examination, it was confirmed that only 38 patients suffered from symptoms similar to those of CL. They were informed of the treatment method, and informed consent was obtained.
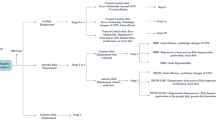
Conservative treatment was started with pharmacotherapy (ketoprofen 50 mg TID) and at-home exercise therapy (active and passive) mentioned in the study by Yoshida et al.30 for 4 weeks and told to follow up if there was no improvement to start the second stage of treatment which is IAI therapy.
Injection procedure
The patient was placed in a semisupine position, and to neutralize the patient’s fear, a local anesthetic gel was applied a few minutes before the injection. The preauricular area was disinfected with povidone 4%, and a line was drawn from the lateral canthus to the most posterior and central point on the tragus (the Holmlund–Hellsing line); on this line 10 mm anterior to the tragus, point A was marked, and 10 mm below this point was marked other B (Fig. 1).
The solution to be injected was prepared away from the patients’ eyes according to the randomization process, and the patient was asked to open his mouth as wide as possible; the tip of a 27-gauge needle with 35 mm length was inserted starting at point B to a depth of approximately 25 mm in an anteromedial direction along the posterior portion of the condylar neck to reach the retrodiscal area (Fig. 2) and to standardize the injection technique and ensure consistency and to ensure that the needle tip is in the target area, two essential things were adopted; aspect posterior of the condylar neck was palpated, and the sensation of hit needle tip with the roof of the articular fossa before withdrawn it slightly, then was injected 1 ml of solution (D5W or NS) slowly after aspiration, and patients were injected only once.
Post- injection care
After injection, a dry dressing was applied. Patients were instructed to follow a soft diet to reduce the load on the joint avoiding NSAIDS and taking penicillin 500 mg for 7 days, and acetaminophen 500 mg only when pain occurs.
Outcomes measurements
The effectiveness of the treatment was evaluated by studying the following variables:
-
1.
Unassisted MaximumInterincisal Opening (MIO) including overlap was measured with a millimeter-scaled ruler (Fig. 3).
-
2.
Pain intensity on opening and closing was scored with Numerical Rating Scale (NRS) from (0-10) grades, 0 (no pain), while 10 (the worst possible pain).
These variables were measured before injection (T0), after 2 weeks (T1), 2 months (T2), 6 months (T3), and 12 months (T4) of the treatment.
All follow-up outcomes were measured by a same blinded resident physician in the Department of Oral and Maxillofacial Surgery.
Statistical analysis
Microsoft Excel (2007) was used for data entry and was analyzed using SPSS software for Windows Version (20.00).
Shapiro–Wilk test was used to test the normality of data distribution, and according to the study design and data distribution, t-test for independent samples was appropriate to determine the type of differences between the two study groups, whether they are significant or not. A p-value less than 0.05 was considered statistically significant.
Results
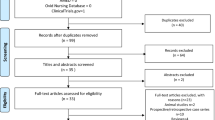
The flow chart of the study was described in (Fig. 4).
In the present study, twenty female patients with symptoms of unilateral DDwoR with limited mouth opening were included. Only mild pain in some patients after D5W administration was noted. None of them complained of complications and none needed to take analgesics except for one in each group The ages of the patients ranged from 18 to 30 years, there was no significant difference between the two study groups regarding age (Table 1).
There were no statistically significant differences in NRS and MIO between the two study groups in T0.
A gradual increase in mean MIO values was observed during the follow-up periods in both groups without significant differences in the mean change at the first three follow-up periods (p > 0.05). Still, a considerable difference appeared in T4 (p < 0.001). The effect sizes, according to the Cohen index, were small to medium in T2 (0.39) and T3 (0.43), while it was clinically significant in T1 (0.93) and T4 (1.5). (Table 2; Fig. 5)
A decrease in the mean values of NRS in both groups was observed during the follow-up periods. Still, the study group had a more significant decrease significantly when compared with the reduction in the control group at the first three follow-up periods (p < 0.001), without the last (p = 0.065). According to the index Cohen, the effect sizes were huge in the first three follow-up periods and had great clinical significance (3.21, 3.37, 4.61), respectively, while it was medium in T4 (0.62). (Table 3; Fig. 6).
A steady increase in both groups was noted, but the curve began to indicate a difference in favor of the study group before T3, and this continued untilT4.
The decrease in both groups was noted, but the decline between T0 and T1 is severe and clearly in favor of the study group.
Discussion
This study was designed to evaluate the clinical efficacy of D5W in improving symptoms of CL after the failure of initial conservative therapies, considering that DPT is safe and has a few side effects. It included patients with unilateral CL as it is easier to assess and study its symptoms, and female patients were adopted, as is well known, who were more prone to TMD than males31. Because there is a difference between the sexes in the range of motion, limiting the study to only one gender would unify the sample and reduce confusion. Thus, this would reduce the sample size, considering that the incidence of this disorder is low among TMD.
The primary treatment for CL aims to free the articular disc from its lock by stimulating the posterior articular zone healing and strengthening the ligaments and posterior bundle by reducing inflammation. This treatment is the justification for targeting retrodiscal area with injection, which was based on the results of studies32,33, which reported that treating disc displacement with reduction patients with dextrose injection is beneficial, as they relieve pain and joint clicking and improve mouth opening better than injection into the superior or inferior space.
The primary sources of dextrose are corn and wheat, so any patient who is hypersensitive to these components has been excluded. However, if the allergy appears, its effect will be local and mild, considering that the joint cavity is small.
The diagnosis in the study design was based on DC/TMD, which has good validity (sensitivity: 80% and specificity: 97%)34, and with the help of clinical signs and symptoms. In the normal state, the opening-to-lateral movement is approximately 4:135, which is helpful and clinically crucial in diagnosing and identifying the origin of the limitation. A restriction in the lateral movement to the opposite side and deviation of the mandible to the affected side when the mouth is wide open indicates unilateral DDwoR. The diagnosis was established without difficulty, and patients were excluded when suspicion arose.
Evaluating the patient’s psychological and behavioural factors at the onset of symptoms is essential in neutralizing them. The presence of oral habits is associated with a poor psychological state and a high probability of developing TMD in females36. Accordingly, individuals with parafunctional habits were excluded. Therefore, the present pilot study represents an instance of ID with isolated joint ligament damage, independent of other contributing factors that might perpetuate the condition.
To the best of our knowledge, there is only one clinical study conducted on patients with CL who were injected with inflammatory 50% dextrose to enhance the effects of the treatment after auriculotemporal nerve block and mandibular condyle exercise objective to recapture the disc27. Some of the patients were suffering from joint degeneration, which may affect the demonstration of the true efficacy of DPT on CL. Moreover, it did not determine the true and accurate value of the variables. Patients were not prevented from taking NSAID drugs after the injection, and this remains a matter of controversy. Moreover, the treatment mechanism is assumed to be based on the induction of an inflammatory process.
This pilot study is the first conducted on patients with CL to the best of our knowledge that evaluated the effect of injection D5W as a treatment option available in the medical literature to improve the healing process and relieve pain; the current study relied on studying the actual effect of D5W injection by comparing it with NS without adding any anesthetic solution, because temporary numbness may occur after using it and sometimes worrying for some patients, and because local anesthetics used in injection intra-articular may have a chondrogenic effect. It may also have a short-term pain relief effect37, as Asan et al. reported that a single injection of a local anesthetic solution has a toxic impact on chondrocytes and, consequently, degenerative changes in the surfaces of the TMJ38, and because we do not need to auriculotemporal nerve block as long as the pain induced by injection is minor as compared with injection sterile water39.
One of the indications for prolotherapy is cases that does not respond to conservative treatments40, and is recommended for chronic musculoskeletal pain19. Initial conservative treatment was short for several reasons: Yoshida et al. study41 indicated that conservative treatment early in the onset of symptoms in younger patients has a good prognosis. In our estimation, symptoms could improve quickly because the inclusion conditions were consistent with what was mentioned in that study. Moreover, long periods of conservative treatment may expose patients to joint degeneration if it fails; Lei et al.42 reported that the probability of degeneration in adolescents and young adults with CL increases after one month of injury; most were female (84.70%).
Stabilization splints or others were not used in conservative treatment because they require long-term commitment, which is one of the negatives that can be avoided with IAI. Returning to the Priyadarshini et al.20, they compared prolotherapy with splint therapy for the management ID, it was found that prolotherapy is better than splints in providing long-term clinical comfort and symptom relief during a one-year follow-up.
Hypertonic dextrose solution has been used to treat hypermobility disorders with severe ligament laxity. At the same time, there may be no need to use it in the case of DDwoR due to the difference in the severity of injury between them and because a low-concentration injection may be sufficient to stimulate growth factors that affect area regeneration. The inflammation resulting from high concentrations may be unbearable for some of them and prompt them to return to the analgesics they have grown tired of taking over the past period.
There is no specific protocol for the number of injections used during the treatment period and the volume of injected material. When the articular disc is displaced, the condyle moves closer to the articular fossa, narrowing the articular space. It was believed that the larger the volume of the injected material, the greater the space expansion, which will lead to results unrelated to the intrinsic effect of the material but rather related to the increased hydrostatic pressure effect and the duration of the material’s presence within the area. Therefore, the current study adopted the smallest volume used in dextrose prolotherapy studies (1 ml) after returning to a systematic review23. Similarly, repeated injections’ excessive positive effect may depend on the repeated deposition of the material within the tissues43. We believe that involving other structures with retrodiscal tissues during the treatment process will have no significant effect, given that it is the most damaged structure.
The basic symptoms of patients with CL-restricted mouth opening and pain associated with opening and closing were studied, expressed in precise values, not by proving or denying their existence, to highlight the exact effect of the treatment.
The patients were constantly contacted to check on their condition, which helped strengthen their confidence. Follow-up was maintained until the end of the observation period, and no withdrawals were recorded.
The results of our study confirmed our hypothesis that D5W is more effective than NS and can be interpreted as the targeted area during injection, which is the retrodiscal tissues, composed of loose connective tissue that is highly vascularized and innervated. The rapid and immediate analgesic effect seen after a single injection of D5W was significant clinically. Since dextrose has a neurosensory effect, this may be the reason for the considerable difference between the two study groups. The exact mechanism of action is unclear, but the hypothesized mechanism is that it reduces nerve inflammation by inhibiting sensory receptors and stopping the release of substance P and calcitonin gene-related peptides, which are known to cause pain. Therefore, dextrose injection may affect tiny polypeptide neurotransmitter fibers associated with neuropathic pain, and it appears that dextrose injection reduces pain in a variety of chronic musculoskeletal pain conditions.
This interpretation was based on a study by Bertrand et al.44 in which the application of a cream containing mannitol (related to dextrose) and another containing placebo was compared to a painful area after the TRPV-1 receptor (responsible for producing pain) was stimulated by capsaicin, the result was fast pain relief with mannitol, which was explained by a decrease regulation of this receptor after direct exposure to the cream. Moreover, Wu et al.39 found that a single ultrasound-guided injection perineural of D5W for carpal tunnel syndrome patients was significantly superior to saline injection in reducing pain and disability. Smigel et al.45 reported that D5W had a distinct analgesic effect compared to saline after epidural injection in patients with chronic non-surgical low back pain for 15 min to 48 h.
The exact mechanism of action of D5W on the regeneration and healing of connective tissue is not understood. Still, it is reported that it is through the induction of growth factors that contribute to the formation of mature collagen and the strengthening of loose ligaments and tendons to repair and restore the area to normal balance between the components of the TMJ.
Assuming that the defect in the condyle-disc complex that contributed to the displacement of the articular disc was due to the poor efficiency of the retrodiscal tissues, the improvement of movement is related to two things: the first is the repair and restoration of damaged retrodiscal tissues through the previously mentioned regenerative mechanism, which allows the disc to gradually return to its previous position, which is clinically manifested by an increase in mouth opening, and the other is that with the increased frequency of mouth opening, the disc is displaced more anteriorly and the stretching of the ligaments behind the disc increases, resulting in a clinical increase in mouth opening not related to regeneration.
Woo et al.46 reported that 1% dextrose can promote the proliferation of fibroblasts and increase the synthesis of type 1 collagen.
The delay in the onset of a significant clinical difference in MIO in favor of the study group, despite the proven regenerative effect of D5W, can be attributed to the following: slow impact of a single D5W injection, where the time required for improvement is related to the degree of damage and pathological change in the structure of the area and the time needed to repair it. The difference in the pathology degree between one disorder and another needs a difference in the repair period. Perhaps the rapid regenerative effect of D5W and the significant clinical improvement in movement depends on the continuation of proliferative stimulation related to several factors: the impact of the substance itself, its size, and the effect of the needle prick. Repeated injections ensure the continuation of the proliferative stimulation by ensuring that the previous effects continue longer than the period guaranteed by a single injection. The substance itself has a chemically stimulating effect on growth factors, and the larger the volume of the substance, the longer the organism needs to absorb it. As for the needle prick, it causes mechanical damage that tears the tissues and stimulates proliferation. However, what is the required quantity and the number of injections needed? This question is what future research should revolve around.
From the above, rapid improvement in pain in favor of the study group did not coincide with improved movement, and the noticeable improvement in both groups may be due to the hydrostatic pressure results from the fluid injection that may have the effect of breaking down adherences between the joint surfaces and release it47. This process contributes to the gradual return of the disc, and coincides with the improvement of the mouth opening. It has been reported that saline intra-articular injection may reduce the concentration of inflammatory mediators and thus improve symptoms, as it is biologically neutral48. Another reason for improvement is that the concentration of chloride ions in saline is 51 mmol/L higher than the extracellular concentration49. This difference, in turn, affects the osmotic balance, which causes local injury followed by regeneration. However, the effect of saline administration has not yet been determined.
Rapid pain relief is necessary but not sufficient. It is an essential part of treatment and has clinical importance no less than movement. It makes patients look at treatment with satisfaction because they no longer need to take analgesics, and this is consistent with the fundamentals of treating TMD, which are to reduce pain, improve quality of life, and prevent further harm. In any case, the practitioner must explain to the patient that improvement in movement will be gradual and will notice the difference later.
Returning to the medical literature, our results in this study are consistent with those of other DPT studies and differ from others.
Referring to the injection site, the current results match with the Younis et al.32 that found a difference in the effect of dextrose injection relates to the injection location when injection into inferior joint space and retrodiscal tissues improved pain and mouth opening. Additionally, the current findings met Zhou et al. study mentioned above27; their result was improved pain and mandibular function and increased mouth opening and lateral movements after two weeks of treatment, and it was mentioned that the success rate reached 97.5% after 6 months.
The results of the current study were consistent with Mohammed et al.1, which evaluated the effect of DPT on ID patients. Their results showed a 60% reduction in pain, while the improvement in mouth opening was 6.4 mm after two weeks of treatment. Symptoms continued to improve gradually during the 12-week follow-up period.
The current results agree with RCT50 that studied the effect of intra-articular injection of (20% dextrose/0.2% lidocaine) with comparing to (sterile water/0.2% lidocaine) in improving pain and jaw dysfunction in chronic TMD patients, which showed statistically significant superiority of the study group concerning pain intensity after 6 months and continued until 12 months of follow-up.
In an RCT conducted by Hassanien et al.51 that compared the effect of injection dextrose 12.5% with lidocaine 2% with the effect of low-level laser in managing TMD, it showed a decrease in the pain intensity variable in both groups. However, there was no significant difference between them; the reduction in the DPT group was early after two weeks of treatment, which is consistent with our study. It also showed that the DPT group was significantly more effective in rapidly improving the maximum mouth opening; the difference may be that the injection in this study was in three reference points, and may that stimulate a multiple regenerative effect, manifested in the appearance of a better improvement of the mouth opening.
Two RCTs showed that injection of 20% dextrose with 0.2% lidocaine compared to 0.2% lidocaine alone at superior joint space improved symptoms in temporomandibular dysfunction patients after follow-up for 3 months, where the values of NRS decreased rapidly during the first month and this is consistent with our study, but with a statistically significant difference between the two groups in favor of the study group21 and its absence in the other study52.
The current results are also disagreed with Haggag et al.53 study that compared the effect of injection of 25% dextrose to NS on bilateral DDwR, which showed a significant difference between the two groups in maximum mouth opening. The difference with us may have been due to the involvement of the superior joint space with the retrodiscal tissues in the injection or perhaps because the degree of retrodiscal ligament damage and the extent of displacement is more significant in DDwoR than in DDwR. Hence, there is a difference in the severity of the pathology, which plays a role in the emergence of the clinical effect of regeneration.
Although reducing pain intensity in the Gibaly et al.54 that compared deep dry needling (DDN) with DDN followed by injection of 12.5% dextrose to treatment DDwR, the current results are different regarding the delay in thesignificant differenceappearance between the two groups (after 5 months). This result may be due to the difference in concentration used. D5W has rapid analgesic neurosensory properties and is non-inflammatory, while concentrations higher than 10% are inflammatory and may require longer for their effect to appear.
Like others, this study has some limitations. The first is the inability to guide the injection radiology. Although the ultrasound-guided injection does not differ in decreased level pain from the non-guided injection, as mentioned in the Alhaj Kheder et al.55, it helps in a safe entry and with one prick towards the target area. This problem was avoided using a fine needle, dependent on reference points, and accurately angulated as possible to minimize potential harm.
Second, the diagnosis was not proven, and the patients were not followed up with an MRI, although it is the gold standard for diagnosis. However, it is only indicated if invasive surgical treatment is an option, and its importance lies in helping to locate the disc during surgery accurately, in addition to its high cost. Manfredini et al.56 reported that MRI confirmed all clinically diagnosed cases of DDwoR, as the clinical diagnosis did not give a false positive, while MRI had an over-positive effect in confirming clinically undiagnosed cases. However, the necessity of establishing the diagnosis by MRI is still controversial, but considering that the goal of treatment is to eliminate the clinical chief complaint, relying on the clinical diagnosis is sufficient to decide to perform the treatment. Finally, Although the sample size of this study is limited and affects the reliability of the results, it represents a preliminary clinical trial to test the effect of D5W when initial conservative treatment has failed in females. It is worth noting that during the entire research period, only this number of patients came to the department despite our continuous efforts to include as many people as possible in the research sample. Therefore, to generalize the results of this study further studies with a larger sample size of both genders are recommended. Studying the radiological changes that occurred after treatment is our next step, and conduct a histological study to show the effect of D5W on joint structures, especially on retrodiscal tissues, and conduct an epidemiological survey of unilateral and bilateral DDwoR to determine its prevalence among patients with TMD.
Conclusion
Within the limitations of the present study, single D5W injection has a rapid and long-term significant effect on relieving pain in female CL patients, while its effect in improving mouth opening is slow.
Data availability
De-identified data are available upon reasonable request to the corresponding author.
References
Mohammed, M. R., Hamad, S. A., Al-Dawoody, A. D., Shehab, A. A. & Ahmed, O. S. Effect of dextrose prolotherapy on internal derangement of the temporomandibular joint. Eur. Rev. Med. Pharmacol. Sci. 27 (11), 4883–4889 (2023).
Zieliński, G., Pająk-Zielińska, B. & Ginszt, M. A Meta-Analysis of the global prevalence of temporomandibular disorders. J. Clin. Med. ;13(5). (2024).
Manfredini, D. et al. Research diagnostic criteria for temporomandibular disorders: a systematic review of axis I epidemiologic findings. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 112 (4), 453–462 (2011).
Poveda-Roda, R., Bagan, J. V., Sanchis, J. M. & Carbonell, E. Temporomandibular disorders. A case-control study. Med. Oral Patol. Oral Cir. Bucal. 17 (5), e794–800 (2012).
Peck, C. C. et al. Expanding the taxonomy of the diagnostic criteria for temporomandibular disorders. J. Oral Rehabil. 41 (1), 2–23 (2014).
Dias, G. M. et al. MRI changes and clinical characteristics in temporomandibular joints with displacement of the articular disk without reduction - a cross-sectional observational study. Cranio 1–10. (2023).
Miernik, M. & Więckiewicz, W. The basic Conservative treatment of temporomandibular joint anterior disc displacement without Reduction--Review. Adv. Clin. Exp. Med. 24 (4), 731–735 (2015).
Al-Baghdadi, M., Durham, J. & Steele, J. Timing interventions in relation to temporomandibular joint closed lock duration: a systematic review of ‘locking duration’. J. Oral Rehabil. 41 (1), 24–58 (2014).
Bouloux, G. F. et al. Guidelines for the Management of Patients with Orofacial Pain and Temporomandibular Disorders. J. Oral Maxillofac. Surg.
Di Giacomo, P. et al. Conservative therapies for TMJ closed lock: A randomized controlled trial. J. Clin. Med. ;11(23). (2022).
Al-Baghdadi, M. et al. TMJ disc displacement without reduction management: A systematic review. J. Dent. Res. 93 (7 Suppl), 37s–51s (2014).
Dimitroulis, G. Management of temporomandibular joint disorders: A Surgeon’s perspective. Aust Dent. J. 63 (Suppl 1), S79–s90 (2018).
Lubecka, K. et al. Update on evidence and directions in temporomandibular joint injection techniques: A rapid review of primary research. J. Clin. Med. ;13(14). (2024).
Chęciński, M. et al. Current clinical research directions on temporomandibular joint Intra-Articular injections: A mapping review. J. Clin. Med. ;12(14). (2023).
Hegab, A. F., Hameed, H., Hassaneen, A. M. & Hyder, A. Synergistic effect of platelet rich plasma with hyaluronic acid injection following arthrocentesis to reduce pain and improve function in TMJ osteoarthritis. J. Stomatol. Oral Maxillofac. Surg. 124 (1s), 101340 (2023).
Liu, S., Hu, Y. & Zhang, X. Do intra-articular injections of analgesics improve outcomes after temporomandibular joint arthrocentesis? A systematic review and meta-analysis. J. Oral Rehabil. 48 (1), 95–105 (2021).
Chęciński, M., Chęcińska, K., Nowak, Z., Sikora, M. & Chlubek, D. Treatment of mandibular hypomobility by injections into the temporomandibular joints: A systematic review of the substances used. J. Clin. Med. ;11(9). (2022).
Bae, G., Kim, S., Lee, S., Lee, W. Y. & Lim, Y. Prolotherapy for the patients with chronic musculoskeletal pain: systematic review and meta-analysis. Anesth. Pain Med. (Seoul). 16 (1), 81–95 (2021).
Hauser, R. A., Lackner, J. B., Steilen-Matias, D. & Harris, D. K. A systematic review of dextrose prolotherapy for chronic musculoskeletal pain. Clin. Med. Insights Arthritis Musculoskelet. Disord. 9, 139–159 (2016).
Priyadarshini, S. et al. Evaluation of prolotherapy in comparison with occlusal splints in treating internal derangement of the temporomandibular joint - A randomized controlled trial. J. Craniomaxillofac. Surg. 49 (1), 24–28 (2021).
Louw, W. F., Reeves, K. D., Lam, S. K. H., Cheng, A. L. & Rabago, D. Treatment of Temporomandibular Dysfunction With Hypertonic Dextrose Injection (Prolotherapy): A Randomized Controlled Trial With Long-term Partial Crossover. Mayo Clin Proc. 94 (5), 820-32 (2019).
Nagori, S. A. et al. The efficacy of dextrose prolotherapy over placebo for temporomandibular joint hypermobility: A systematic review and meta-analysis. J. Oral Rehabil. 45 (12), 998–1006 (2018).
Sit, R. W. et al. Efficacy of hypertonic dextrose injection (prolotherapy) in temporomandibular joint dysfunction: a systematic review and meta-analysis. Sci. Rep. 11 (1), 14638 (2021).
Dasukil, S., Shetty, S. K., Arora, G. & Degala, S. Efficacy of prolotherapy in temporomandibular joint disorders: an exploratory study. J. Maxillofac. Oral Surg. 20 (1), 115–120 (2021).
Köroğlu, Ö., Orscelik, A., Yener-Karasimav, O., Demir, Y. & Solmaz, İ. Is 5% dextrose prolotherapy effective for radicular low back pain? GULHANE Med. J. 61, 123 (2019).
Kim, H., Kim, H. J., Jung, Y. H., Do, W. & Kim, E. J. The effect of perineural injection therapy on neuropathic pain: a retrospective study. J. Dent. Anesth. Pain Med. 24 (1), 47–56 (2024).
Zhou, H., Xue, Y. & Liu, P. Application of auriculotemporal nerve block and dextrose prolotherapy in exercise therapy of TMJ closed lock in adolescents and young adults. Head Face Med. 17 (1), 11 (2021).
Al-Moraissi, E. A. et al. Treatment of painful temporomandibular joint disc displacement without reduction: network meta-analysis of randomized clinical trials. Int. J. Oral Maxillofac. Surg. 53 (7), 584–595 (2024).
Emshoff, R., Bertram, A., Hupp, L. & Rudisch, A. Condylar erosion is predictive of painful closed lock of the temporomandibular joint: a magnetic resonance imaging study. Head Face Med. 17 (1), 40 (2021).
Yoshida, H. et al. Evaluation of mandibular condylar movement exercise for patients with internal derangement of the temporomandibular joint on initial presentation. Br. J. Oral Maxillofac. Surg. 49 (4), 310–313 (2011).
Alrizqi, A. H. & Aleissa, B. M. Prevalence of temporomandibular disorders between 2015-2021: A literature review. Cureus 15 (4), e37028 (2023).
Younis, M., Shah, A. & Rashid, A. Evaluating the effect of dextrose prolotherapy on temporomandibular disorders by choosing different injection Sites- A comparative clinical study. Int. J. Contemp. Med. Res. [IJCMR] ;7. (2020).
Fouda, A. A. Change of site of intra-articular injection of hypertonic dextrose resulted in different effects of treatment. Br. J. Oral Maxillofac. Surg. 56 (8), 715–718 (2018).
Schiffman, E. et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network** and orofacial pain special interest group†. J. Oral Facial Pain Headache. 28 (1), 6–27 (2014).
Gauer, R. L. & Semidey, M. J. Diagnosis and treatment of temporomandibular disorders. Am. Fam. Phys. 91 (6), 378–386 (2015).
Yang, W. et al. College students with oral habits exhibit worse psychological status and Temporomandibular-Related quality of life: A correlational study. Pain Res. Manag. 2022, 6079241 (2022).
Lubecka, K. et al. Intra-Articular local anesthetics in temporomandibular disorders: A systematic review and Meta-Analysis. J. Clin. Med. ;13(1). (2023).
Asan, C. Y. et al. Chondrotoxic effects of intra-articular injection of local anaesthetics in the rabbit temporomandibular joint. Int. J. Oral Maxillofac. Surg. 51 (10), 1337–1344 (2022).
Wu, Y. T. et al. Six-month Efficacy of Perineural Dextrose for Carpal Tunnel Syndrome: A Prospective, Randomized, Double-Blind, Controlled Trial. Mayo Clin. Proc. 92(8):1179-89. (2017).
Cusi, M. et al. The use of prolotherapy in the sacroiliac joint. Br. J. Sports Med. 44 (2), 100–104 (2010).
Yoshida, H. et al. Prognostic factor of mandibular condylar movement exercise for patients with internal derangement of the temporomandibular joint on initial presentation: preliminary report. J. Craniomaxillofac. Surg. 41 (5), 356–358 (2013).
Lei, J. et al. Degenerative temporomandibular joint changes associated with recent-onset disc displacement without reduction in adolescents and young adults. J. Craniomaxillofac. Surg. 45 (3), 408–413 (2017).
Majumdar, S. K., Krishna, S., Chatterjee, A., Chakraborty, R. & Ansari, N. Single injection technique prolotherapy for hypermobility disorders of TMJ using 25% dextrose: A clinical study. J. Maxillofac. Oral Surg. 16 (2), 226–230 (2017).
Bertrand, H., Kyriazis, M., Reeves, K. D., Lyftogt, J. & Rabago, D. Topical mannitol reduces Capsaicin-Induced pain: results of a Pilot-Level, Double-Blind, randomized controlled trial. Pm R. 7 (11), 1111–1117 (2015).
Maniquis-Smigel, L. et al. Analgesic Effect of Caudal 5% Dextrose in Water in Chronic Low Back Pain. A Randomized Controlled Trial of Epidural Injection. Anesthesiol. Pain Med. (2016).
Woo, M. S. et al. The proper concentrations of dextrose and Lidocaine in regenerative injection therapy: in vitro study. Korean J. Pain. 34 (1), 19–26 (2021).
Zheng, L., Gao, L., Hu, Y., Zhang, L. & Guan, Y. Progress in the study of temporomandibular joint lavage in temporomandibular joint disorder. J. Multidiscip. Healthc. 17, 2175–2184 (2024).
Chęciński, M. et al. Intra-Articular physiological saline in temporomandibular disorders May be a treatment, not a placebo: A hypothesis, systematic review, and Meta-Analysis. J. Clin. Med. 13, 21 (2024).
Hoorn, E. J. Intravenous fluids: balancing solutions. J. Nephrol. 30 (4), 485–492 (2017).
Lam, S., Reeves, K. & Rabago, D. Dextrose prolotherapy for chronic temporomandibular pain and dysfunction: results of a Pilot-Level randomized controlled study. Arch. Phys. Med. Rehabil. 97, e139 (2016).
Hassanien, N., Kamel, H. & Rashed, S. Dextrose prolotherapy versus low level laser therapy (LLLT) for management of temporomandibular joint disorders (TMD): clinical randomized controlled study. Egypt. Dent. J. 66, 95–106 (2020).
Zarate, M. A., Frusso, R. D., Reeves, K. D., Cheng, A. L. & Rabago, D. Dextrose prolotherapy versus Lidocaine injection for temporomandibular dysfunction: A pragmatic randomized controlled trial. J. Altern. Complement. Med. 26 (11), 1064–1073 (2020).
Haggag, M. A., Al-Belasy, F. A. & Said Ahmed, W. M. Dextrose prolotherapy for pain and dysfunction of the TMJ reducible disc displacement: A randomized, double-blind clinical study. J. Craniomaxillofac. Surg. 50 (5), 426–431 (2022).
Gibaly, A., Abdelmoiz, M. & Alghandour, A. N. Evaluation of the effect of dextrose prolotherapy versus deep dry needling therapy for the treatment of temporomandibular joint anterior disc displacement with reduction: (a randomized controlled trial). Clin. Oral Investig. 28 (9), 475 (2024).
Alhaj Kheder, M. B., Kandil, N. M., El-Ghareeb, T., Abdel Aziz, O. M. & Zeitoun, R. Ultrasound-Guided vs Non-Guided prolotherapy for internal derangement of temporomandibular joint. A randomized clinical trial. J. Ultrasound Med. 43 (8), 1401–1412 (2024).
Manfredini, D. & Guarda-Nardini, L. Agreement between research diagnostic criteria for temporomandibular disorders and magnetic resonance diagnoses of temporomandibular disc displacement in a patient population. Int. J. Oral Maxillofac. Surg. 37 (7), 612–616 (2008).
Acknowledgements
The presented article is a part of the MCS’s study of Yazan Said Taleb approved by the Damascus University Faculty of Dentistry, Damascus, Syria.
Funding
This research is funded by Damascus University (funder No. 501100020595).
Author information
Authors and Affiliations
Contributions
Y.S.T. conceptualized the idea, provided the treatment, and contributed to the writing, documenting, and interpretation of data.; M.Z. conceptualized the idea and supervised the research. Y.A.T contributed to write the main manuscript, made the revision, formatting, and reediting of the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Institutional review board statement
The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Institutional Review Board of Damascus University (DN-02092024-306).
Informed consent
Informed consent was obtained from all subjects/caregivers involved in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Taleb, Y.S., Zenati, M. & Alsayed Tolibah, Y. Dextrose prolotherapyeffectin improving thetemporomandibular joint disc displacement symptoms without reduction refractory to conservative treatment: a pilot study. Sci Rep 15, 18269 (2025). https://doi.org/10.1038/s41598-025-03041-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-03041-4