Abstract
Primary aldosteronism (PA) is the most common endocrinologic hypertension, affecting 3.9–15% of hypertensive patients. While unilateral PA is potentially curable through adrenalectomy, a significant proportion of patients experience persistent hypertension despite successful surgery. This study developed and validated a novel predictive scoring model for persistent hypertension following adrenalectomy based on 363 patients from a 25-year single-center experience. Persistent hypertension occurred in 59.5% of patients postoperatively. Multivariable analysis identified five independent predictors: age ≥ 50 years, dyslipidemia, BMI ≥ 25 kg/m2, use of ≥ 3 antihypertensive medications, and hypertension duration ≥ 5 years. The model demonstrated excellent discriminative ability with area under the curve of 0.81 in internal validation and 0.72 in external validation. Predictive risk scores were categorized into low-risk (0–1), intermediate-risk (2–3), and high-risk (4–5) groups, with persistent hypertension rates of 23.5%, 72.1%, and 90.6%, respectively. This practical scoring system enables improved preoperative counseling and individualized management planning using readily available clinical parameters.
Similar content being viewed by others
Introduction
Primary aldosteronism (PA) is a disorder caused by excessive aldosterone secretion from the adrenal glands. It is the most common cause of endocrine hypertension, with a prevalence ranging from 3.9 to 15% among all hypertensive patients1,2,3,4,5. Histopathological abnormalities in unilateral PA can be categorized as aldosterone-producing adenoma which is the most common form and the less common one is adrenal hyperplasia. This unilateral PA can potentially be cured by unilateral adrenalectomy6. Although hypokalemia and elevated aldosterone levels can be corrected after adrenalectomy, normalization of these biochemical parameters does not guarantee blood pressure control. A significant proportion of patients continue to experience persistent hypertension postoperatively, with reported resolution rates ranging from 20–72%7. Possible contributors to persistent hypertension include coexisting essential hypertension, vascular remodeling, and chronic kidney disease, among other factors8,9.
Previous studies have attempted to identify factors predicting the resolution of hypertension following adrenalectomy for unilateral PA, beginning as early as 2008. Zarnegar et al. developed a model known as the Aldosteronoma Resolution Score (ARS) to estimate the likelihood of successful blood pressure control in patients with unilateral PA after surgery. They identified four significantly predictive variables including use of two or fewer antihypertensive medications preoperatively, body mass index (BMI) ≤ 25 kg/m2, duration of hypertension ≤ 6 years, and female gender10. Despite showing promise, this scoring system is not widely used in current practice. A key limitation is that it was developed at a single treatment center in the United States, with a sample size of only 100 patients, which may affect the generalizability of its findings to other countries11. Moreover, recent studies have highlighted a range of other factors that may predict successful resolution of hypertension, including a plasma aldosterone level ≥ 35 ng/dL, contralateral adrenal abnormalities, and the absence of diabetes mellitus12,13,14. Conversely, investigations on predictors of persistent hypertension following adrenalectomy remain limited. There is only one nomogram-based study that evaluated factors associated with persistent hypertension, but even that study has notable constraints and has not been widely validated15.
We are interested in identifying the variable factor associated with persistent hypertension after adrenalectomy in unilateral PA utilizing over twenty-five years of experience in a major referral hospital in the country. Our aim is to create a novel predictive scoring model to estimate the likelihood of persistent hypertension, thereby providing valuable information to patients prior to surgery and aiding in follow-up planning.
Patients and methods
Study design and participants
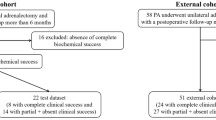
This study is a retrospective cohort study. We reviewed clinical data from patients with unilateral PA who underwent laparoscopic adrenalectomy at King Chulalongkorn Memorial Hospital between January 2000 and June 2024. The study was approved by Chulalongkorn University’s Institutional Review Board. Informed consent was waived due to the retrospective design and the absence of impact on patient interests or privacy. Eligible patients were those with unilateral PA who underwent adrenalectomy and were diagnosed according to the Endocrine Society guidelines, based on a history of hypertension (with or without hypokalemia) and positive results on both screening and confirmatory biochemical tests, as described below. Computerized tomography (CT) or magnetic resonance imaging (MRI) was initially performed to identify adrenal lesions. In patients under 35 years old with a clear unilateral lesion and a normal contralateral adrenal gland, adrenal vein sampling (AVS) was not performed. In all other cases, AVS was used to confirm unilateral PA and determine lateralization. AVS was performed under continuous cosyntropin stimulation (50 µg/h) with sequential catheterization of both adrenal veins. Successful catheterization was confirmed by a selectivity index of ≥ 5:1 (adrenal vein/inferior vena cava cortisol ratio), and lateralization was defined as an aldosterone/cortisol ratio from one adrenal gland at least four times higher than that of the contralateral side. Exclusion criteria included evidence of more than one type of adrenal hormone overproduction, diagnosis of adrenocortical carcinoma, active malignancies, severe cardiac or renal failure, thyroid dysfunction, lack of follow-up within six months after surgery, and absence of biochemical success according to the Primary Aldosteronism Surgery Outcome (PASO) criteria.
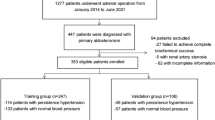
A total of 760 adrenalectomy patient records were reviewed, and 363 eligible patients were enrolled. These patients were randomly divided into training and testing groups for predictive model development (Fig. 1).
Data collection
We recorded the demographic data including age, weight, height, BMI, clinical, and laboratory parameters. History of diabetes mellitus, chronic kidney disease, ischemic heart disease and, smoking habits, drinking habits, family history of hypertension, maximum systolic BP and diastolic BP, duration of hypertension, number of antihypertensive medications, which were also interpreted as defined daily dose (DDD) based on the World Health Organization’s (WHO) Anatomical Therapeutic Chemical/defined daily dose index16, preoperative serum potassium, blood urea nitrogen, plasma aldosterone concentration (PAC), plasma renin activity (PRA), HbA1C, Tumor size (maximal diameter), lesion character (unilateral or bilateral), left ventricular hypertrophy by electrocardiogram, proteinuria using dipstick test, preoperatively. Then we collected the postoperative data including blood pressure, serum potassium, PAC, PRA and detailed usage of antihypertensive medications.
Diagnosis of primary aldosteronism
The diagnosis of PA was established according to the Endocrine Society Clinical Practice Guidelines17, following a structured approach of screening and confirmatory testing. Positive screening for PA was defined as a plasma aldosterone-renin ratio (ARR) > 20 ng/dL per ng/mL/hr, with PAC > 15 ng/dL and PRA < 1.0 ng/mL/hr17. Measurements of PAC and PRA were performed using the radioimmunoassay (RIA) technique. All laboratory measurements adhered to standardized protocols as recommended by the guidelines, including discontinuation of interfering antihypertensive medications for 2–4 weeks prior to testing. Patients were maintained in a normokalemic state with liberal sodium intake.
For confirmatory testing at our institution, we primarily employed two methods: the saline infusion test (SIT) and the captopril challenge test (CCT). The SIT was performed in a controlled clinical setting, with patients in a supine position after overnight fasting. Two liters of 0.9% normal saline were infused intravenously over 4 h, with blood samples for PAC and PRA collected before and after infusion. PA was confirmed when post-infusion PAC remained > 10 ng/dL (> 280 pmol/L), while values < 5 ng/dL (< 140 pmol/L) excluded the diagnosis. For the CCT, patients were seated for 1 h before baseline sampling, followed by oral administration of captopril (50 mg). Repeat samples were collected 2 h post-administration. PA was confirmed when post-captopril PAC failed to decrease by at least 30% from baseline, or when the post-captopril ARR remained > 20 ng/dL per ng/mL/hr. This test was particularly valuable for patients with contraindications to volume expansion.
Definition of hypertension, chronic kidney disease, diabetes mellitus, and dyslipidemia
Hypertension is defined as a persistent elevation in office systolic BP ≥ 140 mmHg and/or diastolic BP ≥ 90 mmHg18. Chronic kidney disease (CKD) is classified according to the Kidney Disease: Improving Global Outcomes (KDIGO) criteria, defined as an estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73 m2 for at least three months, regardless of cause19. Diabetes mellitus is diagnosed according to the American Diabetes Association (ADA) guidelines as a fasting plasma glucose ≥ 7.0 mmol/L or a plasma glucose ≥ 11.1 mmol/L two hours after an oral glucose tolerance test20. Dyslipidemia is defined as elevated triglycerides (≥ 150 mg/dL), low high-density lipoprotein cholesterol (HDL-C; <40 mg/dL), and/or elevated low-density lipoprotein cholesterol (LDL-C; ≥130 mg/dL or current use of LDL-lowering agents)21.
Definition of postoperative outcome
After reviewing all data, we classified the patients into two groups after adrenalectomy according to PASO criteria. The first group is persistent hypertension, if they were categorized partial or absent clinical success, which means they still had hypertension or continued to need antihypertensive medications to control blood pressure. The second group, complete clinical success, comprised patients who have normal blood pressure (< 140/90 mmHg) without taking any antihypertensive medication. Clinical outcomes were routinely assessed at 6 months after adrenalectomy, with additional follow-up assessments conducted within 12 months postoperatively for patients who did not achieve complete clinical success at the initial evaluation7.
Statistical analysis
Demographic, clinical, and laboratory parameters were analyzed using descriptive statistics. Continuous variables are expressed as median and interquartile range, and categorical variables are presented as frequency and percentage. Differences in continuous and categorical variables between the two groups were assessed using the Wilcoxon rank sum test and the Chi-square test or Fisher’s exact test, respectively. Models were developed using a 70/30 training/testing split ratio. Univariable and multivariable logistic regression analyses were performed. Variables with P < 0.1 in the univariable analysis were included in the multivariable analysis, which was subsequently refined using the backward stepwise likelihood ratio method to obtain the final model. Individual predictors included in the final model were assigned a score by dividing the coefficient for each predictor by the lowest coefficient among all predictors in the model and rounding to the nearest integer22. Internal and external validation of the final model was conducted, and performance was evaluated using the area under the curve (AUC) and the Hosmer–Lemeshow (HL) goodness-of-fit test for the training and testing datasets, respectively. Model performance was also assessed using a calibration curve. We used 1000 bootstrap resampling iterations to assess internal and external validity. All P values reported are two-sided, and statistical significance was defined as P < 0.05. Statistical analyses were performed using Stata version 18 (Stata Corp., College Station, Texas).
Results
Among 363 patients who underwent adrenalectomy and met the inclusion criteria, 147 patients (40.5%) achieved complete resolution of hypertension, while 216 patients (59.5%) experienced persistent hypertension postoperatively.
The baseline characteristics of both training (n = 254) and testing (n = 109) groups are presented in Table 1. No significant differences were observed between the groups except for preoperative serum potassium levels (2.8 mmol/L vs. 3.0 mmol/L, P = 0.02).
Table 2 demonstrates the baseline characteristics of patients in the training group, stratified by postoperative outcomes (persistent hypertension versus complete resolution). Significant differences were identified in age, BMI, gender, smoking status, duration of hypertension, number and defined daily dose (DDD) of antihypertensive medications, presence of diabetes mellitus, dyslipidemia, chronic kidney disease, serum creatinine, and eGFR. Variables showing significant differences between these groups, along with clinically relevant factors for hypertension, were included in subsequent univariable and multivariable analyses, as shown in Table 3.
The final predictive model for persistent postoperative hypertension incorporated five key variables: age ≥ 50 years, presence of dyslipidemia, BMI ≥ 25 kg/m2, number of antihypertensive medications ≥ 3, and duration of hypertension ≥ 5 years (Table 4). Based on these variables, a risk score was developed to assess the likelihood of persistent hypertension following adrenalectomy. The model demonstrated a stepwise increase in the probability of persistent hypertension with each additional point in the scoring system: 15.9% for a score of 0, 34.6% for a score of 1, 59.8% for a score of 2, 80.7% for a score of 3, 92.2% for a score of 4, and 97.1% for a score of 5 (Fig. 2). For clinical applicability, the risk scores were divided into three categories: low risk (score 0–1), intermediate risk (score 2–3), and high risk (score 4–5). In our training cohort, the predictive percentages of persistent hypertension for each risk category were 23.5% for low risk, 72.1% for intermediate risk, and 90.6% for high risk, respectively.
The predictive model demonstrated good discriminative ability, with AUC values of 0.81 (95% CI: 0.75–0.86) for internal validation and 0.72 (95% CI: 0.62–0.81) for external validation. The calibration plot showed good agreement between predicted and observed outcomes (Fig. 3).
Receiver operating characteristic curves (ROC) and calibration plot of the model. (A) ROC of the variables correlated with persistent hypertension (age ≥50 years, presence of dyslipidemia, body mass index (BMI) ≥ 25 kg/m2, number of antihypertensive medications ≥ 3, and duration of hypertension ≥ 5 years). (B) The calibration plot indicating good agreement predictive possibility in training group. (C) The calibration plot indicating good agreement predictive possibility in testing group.Abbreviations: HT, Hypertension.
Given the collinearity between the number of antihypertensive medications and the DDD of antihypertensive medication these variables were analyzed separately. The multivariable analysis incorporating DDD and the alternative predictive model are presented in the supplementary information 1.
Discussion
In this study, we developed and validated a predictive model for persistent postoperative hypertension in patients with unilateral primary aldosteronism (PA) undergoing adrenalectomy. Multivariable analysis identified several key predictive factors, including age ≥ 50 years, presence of dyslipidemia, BMI ≥ 25 kg/m2, number of antihypertensive medications, and duration of hypertension. Our findings are based on robust data collected prospectively from patients who underwent adrenalectomy. The observed complete hypertension cure rate of 40.5% aligns with recent international multicenter studies7,23.
The predictive factors identified in our study are fundamental clinical parameters readily obtainable through routine patient history and physical examination, each supported by established physiological mechanisms. Advanced age has been independently associated with dysregulated aldosterone physiology due to histopathological changes in the adrenal glands of older populations24, and it is a significant predictor of persistent hypertension following adrenalectomy12,17,25. This association may be attributed to age-related physiological changes, including arterial stiffening and alterations in the renin-angiotensin-aldosterone system, which can impede complete blood pressure normalization even after successful surgical intervention8,26,27.
Obesity (BMI ≥ 25 kg/m2) in PA patients is associated with a worse cardiometabolic profile and a greater requirement for antihypertensive medications, even at similar PAC and PRA levels. Excessive adipose tissue contributes to elevated production of adipokines, which modulate inflammatory pathways, oxidative stress, and endothelial dysfunction, while also enhancing sympathetic nervous system and renin-angiotensin-aldosterone system. Although obesity does not seem to directly affect PAC or PRA levels in PA patients, these interrelated mechanisms may exacerbate hypertension severity and impair blood pressure control28. In the postoperative setting, persistent hypertension in obese patients may reflect a multifactorial process involving hemodynamic changes, insulin resistance, sleep-disordered breathing, and neurohormonal dysregulation, including alterations in the leptin-melanocortin pathway29,30. Consistently, previous studies have shown that patients with lower BMI tend to achieve better hypertension remission following adrenalectomy10,14,31.
Dyslipidemia, particularly low HDL cholesterol, has been observed in PA patients; however, the mechanisms linking circulating aldosterone and lipid concentrations remain poorly understood5,32. Some evidence suggests that adipose tissue-derived factors, such as leptin, may stimulate adrenal aldosterone secretion33. Additionally, dyslipidemia may contribute to persistent hypertension post-adrenalectomy by accelerating atherosclerosis and endothelial dysfunction, leading to increased arterial stiffness and impaired vascular reactivity34,35. These pathophysiological changes may compromise optimal blood pressure control, as demonstrated in a large worldwide cohort study36.
The impact of hypertension duration can be explained by the documented effects of prolonged aldosterone exposure, including oxidative DNA damage, inflammation, fibrosis, and vascular injury. Chronic exposure to elevated aldosterone levels may result in persistent hypertension even after successful adrenalectomy36. Similarly, the number of preoperative antihypertensive medications typically serves as an indicator of hypertension severity and treatment resistance, reflecting target organ damage, including increased vascular resistance and hypertensive cardiomyopathy. These structural and functional alterations may persist despite successful correction of the primary endocrine abnormality37,38.
Previous cohort studies have similarly attempted to develop predictive models by identifying variables associated with hypertension resolution after adrenalectomy. Various predictive factors have been reported, including BMI, number of antihypertensive medications, duration of hypertension, gender, serum creatinine, and presence of diabetes mellitus10,14,38. However, there remains limited research specifically focused on predicting persistent hypertension after adrenalectomy, which represents an equally important clinical consideration. Compared to the only previous study that developed a nomogram for predicting persistent hypertension after adrenalectomy15, our study demonstrates several advantages, including a larger sample size and the inclusion of antihypertensive medication usage as a predictor, which serves as a key indicator of hypertension severity. Furthermore, our predictive model achieved a higher area under the curve (AUC) compared to the previous study: 0.81 (95% CI: 0.75–0.86) versus 0.78 (95% CI: 0.72–0.84).
Limitations of our study include its single-center, retrospective design and the predominance of an Asian population, which may limit the generalizability of the score to other ethnic groups. Increasing the sample size in future studies could enhance statistical power and improve the model’s discrimination and calibration. Therefore, external validation in larger and more ethnically diverse populations is warranted to confirm the accuracy and performance of this predictive tool across different settings.
In conclusion, our study has developed an efficient predictive score for persistent hypertension in unilateral PA patients following laparoscopic adrenalectomy. The score utilizes readily available basic clinical parameters and is based on a large cohort with comprehensive data collection. We believe this predictive score offers a practical and user-friendly tool that will prove valuable in patient counseling and treatment planning.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Rossi, G. P. et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J. Am. Coll. Cardiol. 48, 2293–2300 (2006).
Young, W. F. Primary aldosteronism: Renaissance of a syndrome. Clin. Endocrinol. 66, 607–618 (2007).
Lim, P. O., Dow, E., Brennan, G., Jung, R. T. & MacDonald, T. M. High prevalence of primary aldosteronism in the Tayside hypertension clinic population. J. Hum. Hypertens. 14, 311–315 (2000).
Douma, S. et al. Prevalence of primary hyperaldosteronism in resistant hypertension: A retrospective observational study. Lancet 371, 1921–1926 (2008).
Monticone, S. et al. Prevalence and clinical manifestations of primary aldosteronism encountered in primary care practice. J. Am. Coll. Cardiol. 69, 1811–1820 (2017).
Reincke, M. et al. Diagnosis and treatment of primary aldosteronism. Lancet Diabetes Endocrinol. 9, 876–892 (2021).
Williams, T. A. et al. Outcomes after adrenalectomy for unilateral primary aldosteronism: An international consensus on outcome measures and analysis of remission rates in an international cohort. Lancet Diabetes Endocrinol. 5, 689–699 (2017).
Proye, C. A. et al. Essential hypertension: First reason for persistent hypertension after unilateral adrenalectomy for primary aldosteronism? Surgery 124, 1128–1133 (1998).
Rossi, G. P. et al. Vascular remodeling and duration of hypertension predict outcome of adrenalectomy in primary aldosteronism patients. Hypertension 51, 1366–1371 (2008).
Zarnegar, R. et al. The aldosteronoma resolution score: Predicting complete resolution of hypertension after adrenalectomy for aldosteronoma. Ann. Surg. 247, 511–518 (2008).
Vorselaars, W. et al. Validation of the aldosteronoma resolution score within current clinical practice. World J. Surg. 43, 2459–2468 (2019).
Zhang, X., Zhu, Z., Xu, T. & Shen, Z. Factors affecting complete hypertension cure after adrenalectomy for aldosterone-producing adenoma: Outcomes in a large series. Urol. Int. 90, 430–434 (2013).
BiLiGe, W. et al. Predicting factors related with uncured hypertension after retroperitoneal laparoscopic adrenalectomy for unilateral primary aldosteronism. Medicine 98, e16611 (2019).
Morisaki, M. et al. Predictors of clinical success after surgery for primary aldosteronism in the Japanese nationwide cohort. J. Endocr. Soc. 3, 2012–2022 (2019).
Li, Z. et al. Predictive model for persistent hypertension after surgical intervention of primary aldosteronism. Sci. Rep. 13, 11868 (2023).
WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD Index 2025. Norwegian Institute of Public Health. https://atcddd.fhi.no/atc_ddd_index. Accessed 1 Jan 2025 (2025).
Funder, J. W. et al. The management of primary aldosteronism: Case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 101, 1889–1916 (2016).
McEvoy, J. W. et al. 2024 ESC guidelines for the management of elevated blood pressure and hypertension. Eur. Heart J. 45, 3912–4018 (2024).
Levey, A. S. et al. Definition and classification of chronic kidney disease: A position statement from kidney disease: Improving global outcomes (KDIGO). Kidney Int. 67, 2089–2100 (2005).
American Diabetes Association Professional Practice Committee. 2. Diagnosis and classification of diabetes: Standards of care in Diabetes-2025. Diabetes Care 48, S27–S49 (2025).
Grundy, S. M. et al. 2018 executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 139, e1046-e1081 (2019).
Mehta, H. B., Mehta, V., Girman, C. J., Adhikari, D. & Johnson, M. L. Regression coefficient-based scoring system should be used to assign weights to the risk index. J. Clin. Epidemiol. 79, 22–28 (2016).
Vorselaars, W. et al. Clinical outcomes after unilateral adrenalectomy for primary aldosteronism. JAMA Surg. 154, e185842 (2019).
Nanba, K. et al. Age-related autonomous aldosteronism. Circulation 136, 347–355 (2017).
Utsumi, T. et al. Development of a novel nomogram to predict hypertension cure after laparoscopic adrenalectomy in patients with primary aldosteronism. World J. Surg. 38, 2640–2644 (2014).
Belikov, A. V. Age-related diseases as vicious cycles. Ageing Res. Rev. 49, 11–26 (2019).
Oliveros, E. et al. Hypertension in older adults: Assessment, management, and challenges. Clin. Cardiol. 43, 99–107 (2020).
Ruiz-Sánchez, J. G. et al. Effect of obesity on clinical characteristics of primary aldosteronism patients at diagnosis and postsurgical response. J. Clin. Endocrinol. Metab. 109, e379–e388 (2023).
Lu, S. C. & Akanji, A. O. Leptin, obesity, and hypertension: A review of pathogenetic mechanisms. Metab. Syndr. Relat. Disord. 18, 399–405 (2020).
El Meouchy, P. et al. Hypertension related to obesity: Pathogenesis, characteristics and factors for control. Int. J. Mol. Sci. 23 (2022).
Picado, O. et al. Long-term outcome success after operative treatment for primary aldosteronism. Surgery 169, 528–532 (2021).
Liang, N. P. et al. The association between aldosterone and lipid profiles in patients with primary aldosteronism. Sci. Rep. 15, 8755 (2025).
Vecchiola, A., Lagos, C. F., Carvajal, C. A., Baudrand, R. & Fardella, C. E. Aldosterone production and signaling dysregulation in obesity. Curr. Hypertens. Rep. 18, 20 (2016).
Halperin, R. O. et al. Dyslipidemia and the risk of incident hypertension in men. Hypertension 47, 45–50 (2006).
Otsuka, T. et al. Dyslipidemia and the risk of developing hypertension in a Working-Age male population. J. Am. Heart Assoc. 5, e003053 (2016).
Vorselaars, W. et al. Clinical outcomes after surgery for primary aldosteronism: Evaluation of the PASO-investigators’ consensus criteria within a worldwide cohort of patients. Surgery 166, 61–68 (2019).
van der Linden, P., Steichen, O., Zinzindohoué, F. & Plouin, P. F. Blood pressure and medication changes following adrenalectomy for unilateral primary aldosteronism: A follow-up study. J. Hypertens. 30, 761–769 (2012).
Wachtel, H. et al. Long-term blood pressure control in patients undergoing adrenalectomy for primary hyperaldosteronism. Surgery 156, 1394–1402 (2014).
Acknowledgements
The authors would like to express their gratitude to the Department of Endocrinology, King Chulalongkorn Memorial Hospital, for their valuable collaboration and support. We also thank the hospital staff for their assistance throughout this study.
Author information
Authors and Affiliations
Contributions
K.H. and S.S. developed the project concept and collected data. K.H. performed the data analysis and wrote the main manuscript. K.P. assisted with data collection and provided administrative support. S.R., M.U., D.S., P.P., and G.S. provided administrative support throughout the study. A.S. contributed to project development, managed the data, and edited the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was conducted in accordance with the ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Harirugsakul, K., Suharitdumrong, S., Panumatrassamee, K. et al. Novel predictive factors scoring model for persistent hypertension after adrenalectomy in patients with primary aldosteronism. Sci Rep 15, 18935 (2025). https://doi.org/10.1038/s41598-025-03912-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-03912-w