Abstract
This in vitro study aims to evaluate various surface treatments on the shear bond strength and failure mode of CAD/CAM PMMA teeth to the heat-polymerized acrylic denture base. The study sample consisted of 100 teeth that were divided equally into five groups: Group 1: denture artificial teeth (control), Group 2: PMMA teeth without surface treatment, Group 3: PMMA teeth with MMA etching, Group 4: PMMA teeth with sandblasting (aluminum oxide particles), and Group 5: PMMA teeth with perpendicular grooves. The shear bond strength test was performed using a universal testing machine and the failure mode was recorded. Data were analyzed using ANOVA followed by Tukey’s post-hoc tests (α = 0.05). MMA increased the shear bond strength compared with other surface treatments (sandblasting and perpendicular grooves; P < 0.001). Sandblasting and perpendicular grooves showed no significant difference in the shear bond strength (P = 0.548 and 0.061; respectively). There were statistically significant differences in the frequencies of failure mode between the studied groups (P < 0.001). The control, PMMA, and PMMA + Sandblasting groups showed the weakest bonding. MMA application improved the shear bond strength for CAD/CAM PMMA teeth, the perpendicular groove seems to be not sufficiently effective, while the sandblasting cannot be considered as a surface treatment.
Similar content being viewed by others
Introduction
Complete dentures are one of the most widely used treatment options for edentulous patients. Although dental implants have provided an alternative treatment protocol to complete dentures, the complexities of treatment, contraindications for surgery, and financial issues make dental implants an unavoidable treatment option for many patients1. Although there has been significant improvement in the remaining natural teeth into old age in Western countries, the overall rate of edentulous patients in less developed countries is still increasing2. The prevalence of edentulism in people over the age of 65 years in Europe is between 15 and 78%.3
Tooth loss affects the quality of life of the edentulous patient due to his pronunciation, speech, and aesthetics; in addition, to the inability to chew4. Complete dentures are a suitable treatment option, as the patient is given a removable prosthetic made of acrylic, which acts as a replacement for the entire tooth and the supporting tissue4,5. Computer-aided design and manufacturing (CAD/CAM) techniques have been introduced to manufacture removable dental appliances6. CAD/CAM discs manufactured from PMMA show superiority in terms of physical and mechanical properties, residual monomers, surface roughness, antibacterial ability, and stain resistance compared to thermoplastic acrylic7.
Bonding failure between artificial teeth and acrylic bases is a major problem when fabricating removable prosthetics, previous studies have reported that bond failure between artificial teeth and acrylic bases is estimated at approximately 22–30%;8,9 another study estimated that the bond failure could be 33%.7 Therefore, the bond between the artificial teeth and the acrylic bases is one of the most important considerations for the durability of removable prosthetics9,10.
Many studies have attempted to enhance the bond strength between conventional denture bases and resin artificial teeth using different surface treatment methods11,12,13. However, the number of studies evaluating the bond strength between t CAD/CAM teeth and acrylic denture bases has been very limited8,14.
The shear bond strength test is the most commonly used type of test to measure the bond strength between acrylic base and artificial teeth15. The shear stress that occurs between artificial teeth and the acrylic bases can be modified by using a chemical bonding agent (methacrylate), and conditioning the bond surface (when the artificial teeth are bonded to the acrylic bases)16,17.
Thus, many studies have focused on enhancing the bond strength between denture bases and artificial teeth; as Barbosa et al. found an increase in bond strength after application of wax solvent and methacrylate monomer18,19. Furthermore, air abrasion and sandblasting were used to enhance bond strength between acrylic teeth and denture bases20,21.
Studies that deal with the bond strength between the resin denture base and CAD/CAM PMMA teeth are rare. Therefore, this study aimed to evaluate the effect of monomer application, sandblasting, and perpendicular grooves on the bond strength between CAD/CAM PMMA teeth and the heat-polymerized acrylic denture base. The null hypothesis was that the surface treatment methods applied would not make any difference in the bond strength between the CAD/CAM PMMA teeth and the denture base.
Results
The mean shear bond strength (in MPa) of the tested groups was 13.6 for the PMMA + MMA group, 10.6 for the control group, 9.5 for the PMMA + Grooves group, 8.2 for the PMMA + SB group, and 6.5 for the PMMA group (Table 1). One-way ANOVA test showed a statistically significant difference in shear bond strength among the tested groups (P = 0.000; Table 1).
Tukey test results showed that the PMMA group had lower shear bond strength than the PMMA + MMA groups with a statistically significant difference (p = 0.000; Table 2), and the PMMA + MMA group showed higher shear bond strength than the PMMA + SB and PMMA + Grooves groups with statistically significant differences (p = 0.000, 0.003; respectively). As for the rest of the comparisons between groups, there were no statistically significant differences (P > 0.05; Table 2).
Table 3 shows that there were statistically significant differences in the frequencies of failure mode between the studied groups. In the PMMA and PMMA + SB groups, the adhesive failure was 100% (the weakest bonding). The adhesive failure was 50% in the PMMA + MMA group, while both cohesive and combined failures reached 50% which confirms the improvement in the bonding of this group (Table 3).
The combined failure in the PMMA + Grooves group was 60% which is much greater than the adhesive failure (15%) and the cohesive failure (25%).
Discussion
CAD/CAM designed and manufactured resin is one of the materials that are constantly being developed in dentistry, and it is also considered a promising material for making removable dentures. Its most important characteristics are that it meets the aesthetic requirements of the patient, low water absorption, and almost non-existent residual monomer content22.
The present study aimed to study the effect of three surface treatments on the bond strength between CAD/CAM PMMA teeth and the heat-polymerized acrylic denture base to decide the most appropriate choice for clinical use. A heat-polymerized acrylic resin denture base was chosen due to its constant need when repairing and lining dentures23.
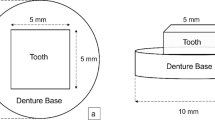
The denture bases were made with dimensions of (20 × 20 × 10) mm to fit the dimensions of the base of the universal testing machine to ensure that the model does not shift after being fixed on the testing machine.
The rectangular shape (6 × 8 × 10) mm was chosen for the teeth in this study to resemble the dimensions of the molar attachment surface and according to the dimensions of the teeth in the Han et al. study14. The teeth samples were adhered to the wax denture bases with the tip of a heated wax knife and immersed 1 mm (ridge lap bond); this differs from the situation when teeth are set up in the laboratory, as they are immersed in wax to a greater depth and their inner surface is irregular, and thus the results of this study reflect stronger results and greater success in clinical conditions.
After opening the crucibles, the samples were gently trimmed from the side containing the acrylic tooth to ensure that all excess resin of the acrylic base was removed, and all samples were immersed in distilled water at 37 °C for 24 h according to the recommendations of ISO/TS 11405:2003, without changing the distilled water during the immersion period, and were left in distilled water until the shear bond test was performed24.
The shear bond test was performed using a universal testing machine, with a cutting head at a speed of 1 mm/min, which is consistent with Klaiber et al. and Prpić et al. studies25,26. The force at which failure occurred and the failure mode were recorded.
The mean shear bond strength in the PMMA group was weaker than in the rest of the groups, while the mean shear bond strength in the PMMA + MMA group was the best. MMA etching improved the shear bond strength of CAD/CAM-designed and milled acrylic resin teeth to conventional heat-polymerized acrylic.
This result is consistent with the Palitsch et al. study27, as Methyl methacrylate appears to be the gold standard and increases the bond strength compared to other surface modifications. This result is also consistent with Takahashi et al., Palitsch et al., and Klaiber et al. results11,25,27, where MMA application contributed the highest shear bond strength. However, these results differed from Aavedra et al., and this difference can be attributed to the difference in the duration of application of MMA to the bonding surface13.
The sandblasting method was adopted through a high-pressure of aluminum oxide particles towards the surface of the material prepared for bonding for 15 s at 6 bar from a distance of 10 mm to the surface. Thus, providing a larger surface area, enhancing the bonding, and forming stronger bonds28.
The sandblasting method caused an increase in the bonding strength, which may be explained by exposing the surface layer and removing it to reach a surface with a higher free surface energy29. The free surface energy of the newly sanded acrylic resin surface is greater than that of the untreated surface, which may be a reason for improving the bonding30.
The aluminum oxide particles were not effective enough to increase the free surface energy area and as is known the effect of sandblasting is a purely micro-mechanical effect and this in turn did not improve the bonding as in the PMMA + MMA group.
This result is consistent with Helal et al. study31, which found that the sandblasting method was not effective in improving the bond between prefabricated teeth and CAD/CAM denture bases, but the sandblasting was performed using 250-micron aluminum oxide particles for 15 s at 70 bar from a distance of 10 mm.
This result is also consistent with Klaiber et al. study25, which found that there was any positive association between sandblasting and increasing shear bond strength between CAD/CAM PMMA teeth and denture bases. The same result was found in Han et al. study14, as the sandblasting on Vita MFT teeth did not increase the shear bond strength between Vita MFT teeth and the heat-polymerized denture resin bases.
The groove drilling method was adopted based on the Takakusaki et al. study32, which found that drilling perpendicular fixing grooves # would be effective in increasing the shear bond strength and improving the bond between artificial teeth and denture bases. After mechanical testing, the PMMA + Grooves group improved the shear bond strength, but the statistical analysis showed no statistically significant differences between groups.
The mechanism of failure has been employed as a measure of bonding performance; adhesive failures have been considered the least acceptable, combined failures acceptable, and cohesive failures perfect33. The higher shear bond strength values lead to higher percentages of cohesive and combined failures, which is in accordance with Akin et al. study16.
Adhesive failure was observed in 100% of the control, PMMA without any modifications, and sandblasting groups, which may be attributed to the weak bonding strength. The PMMA + MMA group showed 50% cohesive failure which indicates good bonding strength. Although the combined failure was 60% in the PMMA + Grooves group, the cohesive failure rate was 15%.
Although this research was carried out in a laboratory manner that simulates the oral environment in terms of immersion in distilled water to compensate for the absorption of water by the heat-polymerized acrylic, one of the main limitations of this study is that it will still differ from clinical conditions due to the absence of chewing forces that differ from one person to another, the duration of application of these forces, the difference in the occlusion pattern, and the humidity conditions.
Materials and methods
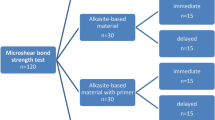
The sample size was calculated using G. Power 3.1.9 software (G*Power 3.1.9, Heinrich Hein Universität Düsseldorf, Düsseldorf, Germany). A sample size of 100 teeth was obtained based on Prpić et al. study34 (Effect size f = 0.50, α err prob = 0.05, power (1 − β err prob) = 0.80, number of groups = 5).
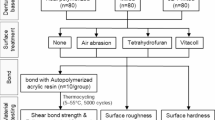
The total sample consisted of 100 teeth in the shape of rectangular cuboids (6 × 8 × 10 mm), which were divided into five groups (Fig. 1):
Group 1 (control): 20 denture artificial teeth (molars) trimmed with carbide bur using a micromotor to obtain the required dimensions. (It was trimmed to make the correlation surface area equal to the rest of the groups to standardize during comparison and statistical analyses).
The remaining four groups were PMMA tooth samples were milled from pre-prepared discs using the CAD/CAM by designing a digital model in the shape of a cube with the required dimensions (6 × 8 × 10 mm): Group 2: 20 teeth without any surface treatment method, Group 3: 20 teeth were etched with MMA, Group 4: 20 teeth were roughed using sandblasting with aluminum oxide particles (AL2O3), Group 5: 20 teeth where grooves were made in the form of perpendicular lines # (gutter width 0.5 mm, depth 1 mm, distance between gutters 1 mm) on the bond surface of the tooth (groove width 0.5 mm, depth 1 mm, distance between grooves 1 mm).
The denture base was as follows: 100 wax pieces in the shape of rectangular cuboids with dimensions (20 × 20 × 10 mm) to be later transformed into thermoplastic acrylic resin.
The control group received ready-made artificial teeth, trimmed to these dimensions with a micromotor to standardize them (6 × 8 × 10 mm), while the experimental groups prepared from CAD/CAM discs of prepolymerized PMMA resin (white PMMA block). Exocad (Exocad Dental CAD, Exocad GmbH, Darmstadt, Germany) was used to design the CAD/CAM teeth, which were translated into STL files. Finally, PMMA rectangular cuboids (6 × 8 × 10 mm) were prepared using a lathe machine (DWX-51-ROLAND, DGA CAD\CAM, Japan) in humid conditions (with cooling). All dental samples were cleaned using ultrasonic with distilled water for 10 min and dried with water and oil-free air for 20 s.
PMMA disc tooth samples (Marco Dental, PRC) were divided into subgroups: without modifications, sandblasting, MMA, and # grooves. The sandblasting was achieved using 50 μm aluminum oxide particles (Cobra, Renfert Gmbh, Hilzinge, Germany) for 15 s at 6 bar from a distance of 10 mm to the surface and at a 90° angle. An air/water syringe was used to clean residual alumina particles and powder from tooth surfaces.
For the modified subgroup (# grooves) by diamond burs, the tooth surfaces were treated and roughed using a straight round end, blue diamond burs (SR-11, 141-012 M-RA, CA Diamond Burs-Smedent-Shanghai) with a slight touch in one direction at a speed of 25,000 rpm to make perpendicular grooves #. During the roughing procedure, the bur was placed parallel to the tooth for 5 s, and then air syringing was used to clean the tooth surfaces.
For teeth in the MMA-treated group, MMA monomer (Methyl methacrylate) was applied using a bond brush to coat the teeth surfaces for 180 s. All teeth were ready to receive the wax denture bases (manufactured in the shape of rectangular cuboids; 20 × 20 × 10 mm), which were adhered surface to surface with the teeth using traditional thermal polymerization through the tip of a heated wax knife (Fig. 2).
Then the wax model with the artificial tooth was placed in the lower half of the crucible so that the wax model was immersed in the gypsum (Neo Gemma 70, Samwoo Co., Ulsan, Korea). After the gypsum setting, it was isolated with silicates, the second part of the crucible was applied and the gypsum was cast until it was filled.
After the gypsum setting, the crucible is placed in boiling water for 4–6 min to melt the wax. Then the crucible is opened, the wax is removed, and the tooth attachment surface is washed with clean boiled water twice, and cleaned using a soft brush.
Heat-polymerized PMMA dental resin (VertexTM Rapid Simplified) was mixed and filled according to the manufacturer’s instructions for filling the gypsum mold, and the crucibles were placed in a heat-curing machine (Hanau Curing Unit, USA) to be immersed in water at 74 °C. This temperature was maintained for 1.5 h before the water bath reached 100 °C and was left to boil for 1 h.
After polymerization, the sample crucibles were carefully removed, and excess resin was cut off. All prepared samples were stored in distilled water at 37 °C for 24 h (according to ISO/TS 11405) before shear testing was performed. The shear bond strength was recorded using a universal testing machine (Instron crop, Canton, MA. USA) by a cutting head at a speed of 1 mm/min until failure occurred (Fig. 3). Shear bond strength was calculated using the following formula:
The failure mode was also defined and classified as follows: score 1 cohesive failure of the teeth (fracture within the artificial or CAD/CAM PMMA teeth body), score 2 cohesive failure of the resin denture base (fracture within the resin dental denture base body), score 3 adhesive failure. (failure between denture tooth and denture base), score 4 combined failure (cohesive and adhesive failure at the same time) (Figs. 4-A, 4-B, and 4-C). Failure was classified using a dental loupe (Olympus SZX10, Olympus, Tokyo, Japan) at 5× magnification.
Statistical analysis was performed using IBM SPSS V.21 (IBM SPSS Statistics® version 21, IBM Corp.). The Kolmogorov-Smirnov test was applied to analyze data distribution, followed by One-Way ANOVA and Tukey HSD tests to compare the effect of surface treatments by the mean shear bond strength. Descriptive statistics were presented as mean, standard deviation, standard error, minimum, and maximum. The significance level was set at 0.05.
Conclusion
Within the limitations of this study, the application of MMA monomer can be suggested as the most effective and efficient surface treatment method for bonding the CAD/CAM resin teeth to a conventional thermoplastic denture base. The use of a perpendicular groove can also be considered a reliable option for surface treatment and conditioning, but it seems to be not sufficiently effective. The sandblasting cannot be considered a surface treatment method for bonding the CAD/CAM resin teeth.
Data availability
The data provided for the results presented in this study is available through the corresponding author upon request.
Abbreviations
- PMMA:
-
polymethyl methacrylate
- CAD/CAM:
-
computer-aided design/computer-aided manufacturing
- MMA:
-
Methyl methacrylate
- SB:
-
sandblasting
- SPSS:
-
Statistical package for social sciences
References
MacEntee, M. I. & Walton, J. N. The economics of complete dentures and implant-related services: A framework for analysis and preliminary outcomes. J. Prosthet. Dent. 79, 24–30 (1998).
Kailembo, A., Preet, R. & Stewart Williams, J. Common risk factors and edentulism in adults, aged 50 years and over, in China, Ghana, India and South Africa: results from the WHO Study on global AGEing and adult health (SAGE). BMC Oral Health. 17, 1–16 (2017).
Petersen, P. E. The world oral health report 2003: Continuous improvement of oral health in the 21st century–the approach of the WHO Global Oral Health Programme. Commun. Dent. Oral Epidemiol. 31, 3–24 (2003).
Boucher, C. O. Complete denture prosthodontics—the state of the art. J. Prosthet. Dent. 92, 309–315 (2004).
Al-Dwairi, Z. N., Tahboub, K. Y., Baba, N. Z., Goodacre, C. J. & Özcan, M. A comparison of the surface properties of CAD/CAM and conventional polymethylmethacrylate (PMMA). J. Prosthodont. 28, 452–457 (2019).
Lima, J. M. C., Anami, L. C., Araujo, R. M. & Pavanelli, C. A. Removable partial dentures: Use of rapid prototyping. J. Prosthodont. 23, 588–591 (2014).
Darbar, U., Huggett, R. & Harrison, A. Denture fracture–a survey. Br. Dent. J. 176, 342–345 (1994).
Choi, J. J. E. et al. Bond strength of denture teeth to heat-cured, CAD/CAM and 3D printed denture acrylics. J. Prosthodont. 29, 415–421 (2020).
Schneider, R. L., Curtis, E. R. & Clancy, J. M. Tensile bond strength of acrylic resin denture teeth to a microwave-or heat-processed denture base. J. Prosthet. Dent. 88, 145–150 (2002).
Dandiwal, N. et al. Evaluation of shear bond strength of three different acrylic resin and artificial denture teeth with and without monomer application. J. Contemp. Dent. Pract. 20, 94–100 (2019).
Takahashi, Y., Chai, J., Takahashi, T. & Habu, T. Bond strength of denture teeth to denture base resins. Int. J. Prosthodont. 13 (2000).
Bolender, Z., Zarb, G. & Eckert, S. Prosthodontic treatment for edentulous patients. Complete denture and implant-supported prostheses. Mosby (2004).
Saavedra, G. et al. Bond strength of acrylic teeth to denture base resin after various surface conditioning methods before and after thermocycling. Int. J. Prosthodont. 20 (2007).
Han, S. Y., Moon, Y. H. & Lee, J. Shear bond strength between CAD/CAM denture base resin and denture artificial teeth when bonded with resin cement. J. Adv. Prosthodont. 12, 251 (2020).
Sirisha, K., Rambabu, T., Ravishankar, Y. & Ravikumar, P. Validity of bond strength tests: A critical review-part II. J. Conservative Dentistry Endodontics. 17, 420–426 (2014).
Akin, H., Kirmali, O., Tugut, F. & Coskun, M. E. Effects of different surface treatments on the bond strength of acrylic denture teeth to polymethylmethacrylate denture base material. Photomed. Laser Surg. 32, 512–516 (2014).
Gharebagh, T. G., Hamedirad, F. & Miruzadeh, K. Comparison of bond strength of acrylic, composite, and nanocomposite artificial teeth to heat-cure acrylic denture base resin. Front. Dentistry. 16, 166 (2019).
Barbosa, D. B., Barão, V. A. R., Monteiro, D. R., Compagnoni, M. A. & Marra, J. Bond strength of denture teeth to acrylic resin: Effect of thermocycling and polymerisation methods. Gerodontology 25, 237–244 (2008).
Barbosa, D. B., Monteiro, D. R., Barão, V. A. R., Pero, A. C. & Compagnoni, M. A. Effect of monomer treatment and polymerisation methods on the bond strength of resin teeth to denture base material. Gerodontology 26, 225–231 (2009).
Kurt, M., Saraç, Y. Ş., Ural, Ç. & Saraç, D. Effect of pre-processing methods on bond strength between acrylic resin teeth and acrylic denture base resin. Gerodontology 29, e357–e362 (2012).
CHUNG, K. H., Chung, C., Chung, C. & Chan, D. Effect of pre-processing surface treatments of acrylic teeth on bonding to the denture base. J. Rehabil. 35, 268–275 (2008).
Srinivasan, M. et al. CAD/CAM milled complete removable dental prostheses: An in vitro evaluation of biocompatibility, mechanical properties, and surface roughness. Dent. Mater. J. 37, 526–533 (2018).
Le Bars, P. et al. Different Polym. Base Removable Dentures? Polym. 16, 40 (2023).
International Standards Organization. Dental Materials—Testing of Adhesion to Tooth Structure, 2nd ed; Technical Specification ISO/TS 11405; International Standards Organization (ISO): Geneva, Switzerland. (2003).
Klaiber, D. et al. Bonding behavior of conventional pmma towards industrial cad/cam pmma and artificial resin teeth for complete denture manufacturing in a digital workflow. Materials 14, 3822 (2021).
Prpić, V., Schauperl, Z., Glavina, D., Ćatić, A. & Čimić, S. Comparison of shear bond strengths of different types of denture teeth to different denture base resins. J. Adv. Prosthodont. 12, 376 (2020).
Palitsch, A., Hannig, M., Ferger, P. & Balkenhol, M. Bonding of acrylic denture teeth to MMA/PMMA and light-curing denture base materials: the role of conditioning liquids. J. Dent. 40, 210–221 (2012).
Akın, H., Tugut, F., Mutaf, B., Guney, U. & Ozdemir, A. Effect of sandblasting with different size of aluminum oxide particles on tensile bond strength of resilient liner to denture base. Cumhuriyet Dent. J. 14, 5–11 (2011).
Bhochhibhoya, A., Mathema, S. & Maskey, B. An evaluation on effect of surface treatment and mechanical modifications on shear bond strength between acrylic denture teeth and heat cure acrylic denture base resin. EC Dent. Sci. 6, 1450–1462 (2016).
Bahrani, F. & Khaledi, A. A. R. Effect of surface treatments on shear bond strength of denture teeth to denture base resins. Dent. Res. J. 11, 114 (2014).
Helal, M. A. et al. Comparative effect of different surface treatments on the shear bond strength of two types of artificial teeth bonded to two types of denture base resins. J. Prosthodont. 31, 427–433 (2022).
Takakusaki, K. et al. Effect of retention hole designs in artificial teeth on failure resistance of the connection with thermoplastic resin. Dent. Mater. J. 41, 573–579 (2022).
Yoshida, Y. et al. Self-assembled nano-layering at the adhesive interface. J. Dent. Res. 91, 376–381 (2012).
Prpić, V., Schauperl, Z., Ćatić, A., Dulčić, N. & Čimić, S. Comparison of mechanical properties of 3D-printed, CAD/CAM, and conventional denture base materials. J. Prosthodont. 29, 524–528 (2020).
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
Nour Alhouda Alhomsi: Conceptualization, Methodology, Project administration, Data curation, Investigation, Roles/writing - original draft. Ammar Almustafa Conceptualization, Methodology, Project administration, Resources, Supervision, Roles/writing - original draft, Writing - review and editing. Hasan Alzoubi: Formal analysis, Methodology, Writing - review and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Alhomsi, N.A., Almustafa, A. & Alzoubi, H. Evaluation of different surface treatments on the bond strength of CAD/CAM PMMA denture teeth to heat-polymerized acrylic denture base. Sci Rep 15, 1255 (2025). https://doi.org/10.1038/s41598-025-85840-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-85840-3