Abstract
Hematological parameters available on automated hematology analyzers have been shown to be useful indicators for hematological disorders. However, extensive studies especially in aplastic anemia for these indices are sparse. Our aim was to investigate the clinical utility of hematological parameters in aplastic anemia. The retrospective study included 146 patients with aplastic anemia and 150 normal controls matched in age and gender, where clinical characteristics and hematological parameters were classified and statistically analyzed. The study showed a statistical difference in the hematological parameters between aplastic anemia patients and controls. White blood cells, absolute neutrophil count, platelet, absolute reticulocyte count, mean reticulocyte volume, immature reticulocyte fraction, mean sphered cell volume, and light scattering reticulocyte count showed significant differences between non-severe aplastic anemia and severe aplastic anemia (p < 0.05). The analysis of the ROC curve showed that the hematological parameters were valuable for the differential diagnosis of severe aplastic anemia (areas under curve of white blood cell, absolute neutrophil count, platelet, absolute reticulocyte count, mean reticulocyte volume, immature reticulocyte fraction, mean sphered cell volume, light scatter reticulocytes were 0.620–0.859). Meanwhile, a combination of absolute neutrophil count, absolute reticulocyte count and mean sphered cell volume (AUC 0.893, 95% confidence interval 0.842–0.943, sensitivity 78.9%, specificity 85.7%) showed excellent precision for the differential diagnosis of severe aplastic anemia. Hematological parameters are readily available parameters that can be helpful to differentiate severe aplastic anemia from non-severe aplastic anemia. They may extend valuable prospects for clinical practice and research in aplastic anemia.
Similar content being viewed by others
Introduction
Aplastic anemia (AA) is a rare and heterogeneous immune-mediated bone marrow failure syndrome. It is defined as pancytopenia with hypocellular bone marrow that is not due to an abnormal infiltration or recognized disease process1. The reticulocyte count can reflect the erythropoietic activity of bone marrow and has been a useful indicator for diagnosing and monitoring the response of bone marrow to anemia therapy2. Modern automated blood cells analyzers provide hematological parameters as indicators in some hematological disorders. In the literature, studies on these indices have been conducted in the diagnosis of iron deficiency anemia and hereditary spherocytosis, monitoring hematopoietic stem cell transplantation, bone marrow regeneration, etc3,4. However, studies extensively especially in AA for these indices are sparse. This study aimed to evaluate the hematological parameters for AA with the DxH 800 hematology analyzer.
Materials and methods
Patients
A total of 146 newly diagnosed patients with AA at Shanxi Bethune Hospital from June 2020 to March 2024 were retrospectively enrolled in this study. One hundred and fifteen gender- and age-matched normal controls were also included. AA patients were confirmed according to the criteria of the International Agranulocytosis and Aplastic Anemia Study (1987)5. Patients with AA were divided into the non-severe aplastic anemia group (NSAA) and the severe aplastic anemia group (SAA) according to the severity of the AA classification (Camitta criteria)6,7. The bone marrow biopsy had to be consistent with the diagnosis. Hypoproliferative myelodysplastic syndrome/acute myelocytic leukemia, paroxysmal nocturnal hemoglobinuria (PNH), autoantibody-mediated pancytopenia, inherited bone marrow failure syndrome, and other causes of pancytopenia/hypocellular were excluded. This study was approved by the Ethics Committee of Shanxi Bethune Hospital.
Samples and measurements
All venous blood samples were collected in 3 mL tubes of dipotassium ethylenediamine tetraacetic acid (K2 EDTA) (BD., USA) and processed in 6 h. DxH 800 hematology analyzer (Beckman Coulter, Miami, FL, USA) was used for whole blood hematological measures. The hematological parameters were retrieved as follows: white blood cell (WBC), absolute neutrophil count (ANC), absolute lymphocyte count (ALC), red blood cell (RBC), hemoglobin (HGB), platelet (PLT), absolute reticulocyte count (ARC), mean reticulocyte volume (MRV), immature reticulocyte fraction (IRF), mean sphered cell volume (MSCV) and high light scatter reticulocytes (HLR). All laboratory practices complied with the manufacture’s instructions and established standard operating procedures.
Statistics
IBM SPSS Statistics 29.0 was used for the analysis. Chi-square tests and the Mann-Whitney U test were used to compare categorical and numerical variables, respectively. The correlations between the numerical variables were tested with the Spearman rank correlation test. All variables with p < 0.05 in the univariate analysis were included in the multivariate analysis. Logistic regression was used to assess independent predictors of SAA in multivariate analyses with a stepwise selection algorithm of important covariates. Receiver operating characteristic (ROC) curve analysis was performed to determine the sensitivity, specificity, and cut-off values of hematological parameters in the differential diagnosis of SAA and NSAA. The evaluation of the accuracy for the differential was based on the area under the curve (AUC). A p-value of less than 0.05 was considered statistically significant.
Results
Demographic characteristics and hematological data of patients with AA and normal controls
A total of 146 newly diagnosed AA patients ( aged 5 to 85 years, median: 45 years, 78 male and 46 female) admitted to Shanxi Bethune Hospital were retrospectively studied. Normal controls matched in sex and age ( aged 5 to 80 years, median: 39 years, 83 male and 67 female) were also included. The AA patients showed significantly lower WBC、ANC、ALC、RBC、HGB、PLT、ARC、HRL, while higher MRV、IRF、MSCV compared to the normal controls (p < 0.001). No significant inter-group differences were observed between groups in gender and age distribution. The variables are summarized in Table 1.
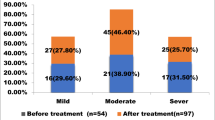
Comparison of data of NSAA and SAA patients
NSAA and SAA patients were compared by the Chi-square test or the Mann-Whitney U test, WBC, ANC, ARC, MRV, IRF, MSCV, and HRL in SAA patients were statistically lower than in NSAA (p < 0.001), PLT in SAA patients was statistically lower than in NSAA (p < 0.05). There were no significant differences in gender, PNH, ALC, RBC and HGB between the groups (p > 0.05). The characteristics and the box plot of values are shown in Table 2; Fig. 1A–I.
Factors related to SAA with univariate analysis and multivariate analysis using univariate and binomial logistic regression analysis
Univariate analysis indicated that AGE, WBC, ANC, ARC, MRV, IRF, MSCV and HRL were negatively correlated with SAA, while ALC, RBC, HGB, and PLT were not correlated with SAA(data not shown). Multivariate analysis indicated that ANC, ARC and MSCV were negatively correlated with SAA (r = 0.229, p = 0.000), (r = 0.961, p = 0.001), (r = 0.931, p = 0.002) (Table 3 ).
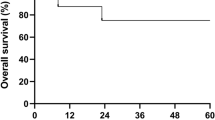
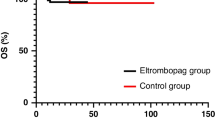
Analysis of the receiver operating characteristic curve (ROC) on the parameters for discrimination of patients with SAA from NSAA
Based on clinical data, we generated ROC curves to evaluate and compare the predictive values of WBC, ANC, ARC, MRV, IRF, MSCV and HRL by determining the cut-off values with optimized sensitivity and specificity (Fig. 2). The areas under the curve (AUC) of WBC, ANC, PLT, ARC, MRV, IRF, MSCV, and HRL were 0.731, 0.858, 0.62, 0.822, 0.729, 0.773, 0.788 and 0.826, respectively. The AUC of the combination of ANC, ARC, and MSCV (AUC 0.893, 95% confidence interval 0.842–0.943, sensitivity 78.9%, specificity 85.7%) showed an excellent precision for differentiating SAA from NSAA. The cut-off values, sensitivity, and specificity for the above factors are shown in Table 4.
Results of the receiver operating characteristic (ROC) analysis on parameters for discrimination of patients with SAA from NSAA. WBC white blood cell, ANC absolute neutrophil count, PLT platelet, ARC absolute reticulocyte count, MRV mean reticulocyte volume, IRF immature reticulocyte fraction, MSCV mean sphered cell volume, HLR light scatter reticulocytes.
Discussion and conclusion
Aplastic anemia is a rare Immune-mediated haemopoietic stem cell disorder that is characterized by pancytopenia and hypocellular bone marrow. Three main pathophysiological mechanisms can cause bone marrow failure: chemical and physical damage, immune destruction, and constitutional genetic defects8. There are unusual inherited aplastic anemia and most acquired form. This study mainly discusses on the latter. We defined SAA as bone marrow cellularity of less than 30% associated with cytopenia in the peripheral blood, which meets at least two of the criteria: (i) ANC < 0.5 × 109/L, (ii) platelet < 20 × 109/L and (iii) ARC < 60 × 109 /L. NSAA was identified as AA that did not fulfilling the criteria for SAA9,10. We retrospectively evaluated the role of baseline clinical characteristics and hematological data in aplastic anemia. We found that white blood cells, erythrocytes, and platelets of AA patients were significantly decreased than controls, the same as most aplastic anemia with pancytopenia. WBC, ANC, and PLT in patients with SAA were statistically lower than in NSAA (p < 0.01) and gender, ALC, RBC, and HGB were not significant differences between the SAA and NSAA groups (p > 0.05). Furthermore, the PNH clones are small in aplastic anemia, and positive PNH was not associated with the severity of AA, which is consistent with previous studies8,11.
Reticulocytes, are immature, nonnucleated erythrocytes reserving a small network of basophilic organelles, consisting of rotoporphyrin and RNA. Reticulocyte enumeration provides a simple and effective means to reflect bone marrow hematopoietics12. Reduced reticulocytes suggest that bone marrow hematopoietic decline. More importantly, reticulocytes changes occurred before neutrophils when bone marrow was damaged. Therefore, ARC is not only an indicator of anemia diagnosis, the severe category, but also a predictor of monitoring of efficacy therapy and the evaluate of prognosis13,14. On DxH 800 hematology analyzers, reticulocytes are stained with an RNA dye and analyzed by flow cytometry providing higher precision and accuracy. Reticulocyte volume and light scatter are related to cell immaturity, more immature reticulocytes are larger, more RNA-containing cells cause higher light scatter. Therefore, reticulocyte parameters (ARC, MRV, IFR, MSCV, HLR) are generated15,16. MRV is the average volume of all retic events, and MSCV is the average volume of the red cell population of reticulocytes. HLR are more immature reticulocytes among RBC that are not influenced by ARC17. IRF is a fraction of the same HLR count (in region 3–10) to the total reticulocyte count, reflecting erythropoietic activity18,19.
The diagnosis of SAA is based on blood cells and bone marrow aspiration/biopsy, which are not routine. Furthermore, the severity of AA is more closely related to the number of peripheral blood cells than bone marrow cellularity20. So there are a few reports about hematological parameters in SAA. As we know, ANC is not a diagnostic and the prognostic indicator of SAA, but is the earliest marker for erythroid engraftment21. ARC is shown to correlate with the response to immunosuppressive treatment22,23. ALC and PLT are used as indicators for monitoring and evaluating therapy with immunosuppressive therapy with or without thrombopoietin24,25. IRF and HLR can be used to estimate the iron status pre-and post-transfusion18. However, our study focused on reticulocyte parameters in AA. Firstly, compared to the normal controls, the AA patients showed significantly lower ARC and HRL, while higher MRV, IRF, and MSCV. It suggeusted that there were younger immature reticulocytes in AA than in controls. Secondly, a univariate and multivariate analysis of baseline parameters was performed to evaluate the predictive value in SAA. The study showed that hematological parameters were associated with SAA. Finally, we found that a combination of ANC, ARC, and MSCV showed excellent precision in differentiating SAA from NSAA. To our knowledge, it is the first extensive especially report on hematological parameters in aplastic anemia.
Due to the retrospective study design, this study has some limitations, which a relatively small number of patients is not expected to be sufficient to guarantee statistical power. Further large studies are needed to verify our results for use in the clinical setting.
In conclusion, our study provides further insight into the clinical efficacy of the hematological parameters in aplastic anemia, especially the combination of ANC, ARC, and MSCV can serve as an indicator for differentiating SAA from NSAA. These indices are obtained in routine tests and utilize peripheral blood samples, it is therefore a less invasive procedure than obtaining bone marrow samples. Hematological parameters are a cost-effective alternative, which will benefit the diagnosis and management of aplastic anemia.
Data availability
Data available on request by email to corresponding author.
References
Killick, S. B. et al. Guidelines for the diagnosis and management of adult aplastic anaemia. Br. J. Haematol. 172 (2), 187–207. https://doi.org/10.1111/bjh.13853 (2016).
Piva, E., Brugnara, C., Chiandetti, L. & Plebani, M. Automated reticulocyte counting: state of the art and clinical applications in the evaluation of erythropoiesis. Clin. Chem. Lab. Med. 48 (10), 1369–1380. https://doi.org/10.1515/CCLM.2010.292 (2010).
Teixeira, C., Barbot, J. & Freitas, M. I. Reference values for reticulocyte parameters and hypochromic RBC in healthy children. Int. J. Lab. Hematol. 37 (5), 626–630. https://doi.org/10.1111/ijlh.12374 (2015).
Hoenemann, C. et al. Reticulocyte and erythrocyte hemoglobin parameters for iron deficiency and anemia diagnostics in Patient blood management. Narrative Rev. J. Clin. Med. 10 (18), 4250. https://doi.org/10.3390/jcm10184250 (2021).
Incidence of aplastic. anemia: the relevance of diagnostic criteria. By the international agranulocytosis and aplastic anemia study. Blood 70 (6), 1718–1721 (1987).
Camitta, B. M., Rappeport, J. M., Parkman, R. & Nathan, D. G. Selection of patients for bone marrow transplantation in severe aplastic anemia. Blood 45 (3), 355–363 (1975).
Bacigalupo, A. et al. Bone marrow transplantation (BMT) versus immunosuppression for the treatment of severe aplastic anaemia (SAA): a report of the EBMT SAA working party. Br. J. Haematol. 70 (2), 177–182. https://doi.org/10.1111/j.1365-2141.1988.tb02460.x (1988).
Young, N. S. Aplastic Anemia. N. Engl. J. Med. 379 (17), 1643–1656. https://doi.org/10.1056/NEJMra1413485 (2018).
Kwon, J. H. et al. Clinical course of non-severe aplastic anemia in adults. Int. J. Hematol. 91 (5), 770–775. https://doi.org/10.1007/s12185-010-0601-1 (2010).
Lohrmann, H. P., Kern, P., Niethammer, D. & Heimpel, H. Identification of high-risk patients with aplastic anaemia in selection for allogeneic 0one-marrow transplantation. Lancet (London England) 2 (7987), 647–650. https://doi.org/10.1016/s0140-6736(76)92462-4 (1976).
Kulagin, A. et al. Prognostic value of paroxysmal nocturnal haemoglobinuria clone presence in aplastic anaemia patients treated with combined immunosuppression: results of two-centre prospective study. Br. J. Haematol. 164 (4), 546–554. https://doi.org/10.1111/bjh.12661 (2014).
Buttarello, M. Laboratory diagnosis of anemia: are the old and new red cell parameters useful in classification and treatment, how?. Int. J. Lab. Hematol. 38 (Suppl 1), 123–132. https://doi.org/10.1111/ijlh.12500 (2016).
Perez-Ecija, A., Martinez, C., Fernandez-Castañer, J. & Mendoza, F. J. The immature reticulocyte fraction (IRF) in the Sysmex XN-1000V Analyzer can differentiate between causes of regenerative and non-regenerative Anemia in Dogs and cats. Anim. Open Access J. MDPI 14 (2), 349. https://doi.org/10.3390/ani14020349 (2024).
Afable, M. G. 2 et al. Efficacy of rabbit anti-thymocyte globulin in severe aplastic anemia. Haematologica 96 (9), 1269–1275. https://doi.org/10.3324/haematol.2011.042622 (2011).
Zhang, H. F., Huang, Z. D., Wu, X. R., Li, Q. & Yu, Z. F. Comparison of T lymphocyte subsets in aplastic anemia and hypoplastic myelodysplastic syndromes. Life Sci. 189, 71–75. https://doi.org/10.1016/j.lfs.2017.09.020 (2017).
Höchsmann, B., Rojewski, M. & Schrezenmeier, H. Paroxysmal nocturnal hemoglobinuria (PNH): higher sensitivity and validity in diagnosis and serial monitoring by flow cytometric analysis of reticulocytes. Ann. Hematol. 90 (8), 887–899. https://doi.org/10.1007/s00277-011-1177-4 (2011).
Yahng, S. A. et al. New proposed guidelines for early identification of successful myeloid and erythroid engraftment in hematopoietic stem cell transplantation. J. Clin. Lab. Anal. 28 (6), 469–477. https://doi.org/10.1002/jcla.21712 (2014).
Stripeli, F. et al. Post-transfusion changes in serum hepcidin and iron parameters in preterm infants. Pediatr. Int. 60 (2), 148–152. https://doi.org/10.1111/ped.13478 (2018).
Piva, E., Brugnara, C., Spolaore, F. & Plebani, M. Clinical utility of reticulocyte parameters. Clin. Lab. Med. 35 (1), 133–163. https://doi.org/10.1016/j.cll.2014.10.004 (2015).
Scheinberg, P. Acquired severe aplastic anaemia: how medical therapy evolved in the 20th and 21st centuries. Br. J. Haematol. 194 (6), 954–969. https://doi.org/10.1111/bjh.17403 (2021).
Young, N. S. Acquired aplastic anemia. JAMA 282 (3), 271–278. https://doi.org/10.1001/jama.282.3.271 (1999).
Zaimoku, Y. et al. Predicting response of severe aplastic anemia to immunosuppression combined with eltrombopag. Haematologica 107 (1), 126–133. https://doi.org/10.3324/haematol.2021.278413 (2022).
Li, R. et al. Predicting response of severe aplastic Anemia to rabbit-antithymocyte immunoglobulin based immunosuppressive therapy combined with Eltrombopag. Front. Immunol. 13, 884312. https://doi.org/10.3389/fimmu.2022.884312 (2022).
Scheinberg, P. et al. Predicting response to immunosuppressive therapy and survival in severe aplastic anaemia. Br. J. Haematol. 144 (2), 206–216. (2005).
Brodsky, R. A., & Jones, R. J. Aplastic anaemia. Lancet (London, England) 365 (9471), 1647–1656. (2005).
Author information
Authors and Affiliations
Contributions
Lizhong Zhang and Xiaonan Han performed the literature research and conceived the study. Qiujuan Zhu and Yu Qin gathered data. Yanan Jia performed statistical analyses. Lizhong Zhang supervised the process and reviewed, edited, and approved the final version of this manuscript. All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
All procedures performed in studies involving human participants were following the ethical standards of the institutional research committee and with the Helsinki Declaration of 1975, as revised in 2008. Approval was obtained from the Ethics Committee of Shanxi Bethune Hospital. The Ethics Committee of Shanxi Bethune Hospital allowed the researchers to collect pseudonymized sociodemographic and morbidity relevant data from patients who gave Broad Consent.
Consent to participate
This retrospective study was approved by the institutional review board of Shanxi Bethune Hospital, and informed consent was waived.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, L., Han, X., Zhu, Q. et al. Clinical utility of hematological parameters in aplastic anemia. Sci Rep 15, 2946 (2025). https://doi.org/10.1038/s41598-025-86917-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-86917-9