Abstract
Changes in foot structure, particularly the presence of flatfeet, have been associated with various limitations in physical performance. This study aimed to investigate the relationship between flexible flatfeet and functional movement, balance, agility, and core muscle strength in young females. Ninety-six female students between the ages of 18 and 25 voluntarily participated in this study. The navicular drop test was used to evaluate the longitudinal arch of the foot. The participants were classified into flexible flatfeet (n = 25) and normal feet (n = 71) groups. Fundamental movement evaluated by the functional movement screening test (FMS); static balance using the Sharpened-Romberg test; dynamic balance using Y-test; agility and coordination using 4 × 9-m shuttle run; endurance of the abdominal muscles and lumbar spine extensor muscles using respectively Partial curl-up and maintaining the plank position, were evaluated. The results of the independent t-test and Mann–Whitney U test showed a significant difference between the two groups in functional movement, abdominal muscle endurance, static balance and lumbar extensor muscle endurance variables (p ≤ 0.05). In the normal feet group, a significant correlation was found between functional movements with abdominal muscle endurance, dynamic balance and agility. The results of this study indicate that individuals with flexible flatfeet exhibited significant impairments in functional movement, core muscle strength, and balance compared to those with normal foot arches. These findings highlight the importance of early identification and appropriate interventions for individuals with flexible flatfeet to mitigate potential negative consequences on physical performance and overall health.
Similar content being viewed by others
Introduction
Foot sole condition significantly impacts daily activities, including standing, walking, and running1,2,3. Changes in sole structure, including arch changes, expose the foot to injuries from physical activities1. It is assumed that defects in the quality of coordination, flexibility, and strength of the foot arch and change in the kinetics of the foot disrupt the function of the foot and make people prone to balance disorders1,2,4. While almost 80% of people have some kind of foot problems, the most common of these disorders at any age is flatfeet deformity5. According to previous studies, prevalence of flatfeet is reported to be around 25% in the general population6,7. This prevalence appears to be higher in females, individuals with a higher body mass index (BMI) and in individuals with larger feet6,8. The incidence of flatfeet in infancy and early childhood is normal, and with increasing age, the arch of the foot acquires a normal shape8.
The occurrence of flatfeet can be due to several factors. It may be present from birth (congenital flatfeet) or it may develop in the later stages of life (acquired flatfeet)9. Proposed causative factors for acquired flatfeet include: age, obesity and not wearing shoes in early childhood6,8,10. In addition, improper function of extrinsic and intrinsic foot muscles at birth or later in life has been reported as a causative factor11. On the other hand, this abnormality is probably caused by the laxity of the internal longitudinal arch ligament (plantar calcaneonavicular and long plantar ligament)12. Ligament laxity causes the foot to drop inward and deviate to a valgus position, altering joint mechanics and foot alignment. This can cause deltoid ligament strain and chronic joint capsule injury in flat feet. Abnormal bone structure and ligament laxity contribute to these issues13. Flatfeet are often associated with pain and often affect speed and balance walking, which increases the risk of falling14,15,16; it also affects mobility, postural stability and movement patterns, which has a deteriorating effect on people’s quality of life17,18,19.
Scattered studies have been conducted in relation to the effect of foot biomechanics on the motor skill-related factors. The Cote et al. study examined the impact of foot arch height on static and dynamic stability; the results showed higher stability in pronated feet compared to supinated feet, but no significant difference with normal feet group20. Khramtsov et al. evaluated also the level of stability in 112 children with flat and normal arch, and the results showed that children with flatfeet have less vertical stability than individual with normal arch21. Harrison and Littlewood investigated the relationship between flexible flatfeet and postural stability in 18-to-33-year olds; the results showed that by increasing the shape change of the flexible flatfeet, the amount of static postural stability decreases22. Al Abdulwahab and Kachanathu studied the effects of various degrees of foot posture on static balance in healthy adults; the results showed increasing the foot posture index (FPI) has an effect on static balance in healthy people23. Song et al. compared foot pressure, ground reaction force, and balance ability in young adults with flexible flatfeet; the results showed no significant difference in peak vertical force, but static balance was significantly lower in flexible flatfeet compared to normal feet24. Therefore, the results in the field of effect of sole foot biomechanics on balance and stability are contradictory.
The position of the skeletal structures directly affects the adjacent structures25. Weight bearing activities involve coupling closed kinetic and kinematic chains of foot, ankle, knee, and hip joints. Foot position changes postural and movement of proximal joints26,27. As result, after flatfeet deformity, pronation of the foot causes internal rotation of the tibia, knee valgus and internal rotation of the hip joint occurs when weight bearing. This affects the muscular chain, causing pelvis position changes, lumbar spine position changes, and trunk instability27,28,29. Therefore, probably during the implementation of fundamental movement patterns, this defective kinetic and kinematic chain may affect people’s performance. The Functional Movement Screen (FMS) is also an assessment tool used to measure trunk and core strength as well as fundamental movement patterns in a range of physical activities (such as deep squat, hurdle step, in-line lunge, shoulder mobility, active straight leg raise, trunk stability push-up, rotary stability)30,31. FMS can detect poor movement patterns, dysfunctions and asymmetries in the body30. It is primarily used to predict future risk of injury and to establish baseline exercise levels following treatment, rehabilitation, or performance training in active adults30,31. Since poor posture can affect joints, bone structures and soft tissues and cause musculoskeletal disorders28, it seems logical to use the FMS score as a posture assessment tool. Despite the importance of this issue, not much research has been conducted in this area. Only Fallahasady et al. examined the relationship between lumbar hyperlordosis and functional movement screening scores and core muscle endurance, finding that lumbar lordosis angle affects core muscle endurance but not FMS execution32.
The effect of sole foot biomechanics on muscle strength as one of the motor skill-related factors was investigated only in the research of Yalcin et al. The results no significant difference in the strength of the evertor and invertor muscles between individual with flexible flatfeet and the control group33. On the other hand, fewer research has been conducted on the effect of sole foot biomechanics on performance scales. Sahin et al. investigated the relationship between pes planus degree, balance and jump performance in athletes; the results indicated that by increasing the pes planus degree, static balance and vertical jump decrease significantly34. Therefore, the effect of sole foot biomechanics on fundamental movement patterns and health- and motor skill-related scales is not clear. Therefore, the objectives of this study were: (1) comparison of the FMS score between subjects with and without flexible flatfeet; (2) comparison of the strength of the abdominal muscles and spinal extensor muscles between subjects with and without flexible flatfeet; (3) comparison of the coordination and agility between subjects with and without flexible flatfeet; (4) comparison of the stability between subjects with and without flexible flatfeet; and (5) investigating the relationship between the FMS score with the strength of the abdominal muscles and spinal extensor muscles, the coordination and agility, and the stability in subjects with and without flexible flatfeet. We hypothesized that subjects with flexible flatfeet would exhibit lower FMS scores, decreased strength of abdominal and spinal extensor muscles, impaired coordination and agility, and reduced stability compared to subjects with normal foot arches. Additionally, we hypothesized a stronger correlation between FMS scores and health- and motor skill-related scales in the normal feet group compared to the flatfeet group.
Materials and methods
Study design and participants
The current study is a cross-sectional and comparative research that was conducted in compliance with ethical principles and has the code of ethics number IR/SSRI.REC.2022.13901.1950 from the Sport Sciences Research Institute, and written informed consent was obtained from all participants. The ethics board authorized the participants (aged 18 years old and over) to give their own consent based on the low risk factor in this study. All experiments were performed in accordance with relevant guidelines and regulations. The study procedures were in accordance with the latest version of the Declaration of Helsinki. Human participants’ names and other HIPAA identifiers removed from all sections of the manuscript, including supplementary information.
For this purpose, 96 female students between the ages of 18 to 25 voluntarily participated in this study (all of them completed a written consent form), that after evaluated the longitudinal arch of the foot (using the navicular drop test35), the participants were divided into flexible flatfeet (n = 25) and normal feet (n = 71) groups (Sample size was calculated using G ∗ power 3.1.9.4 (Franz Faul, Kiel, Germany) based on data from a similar study36. A required sample size of 23 was determined by calculating an estimated effect size of 0.75, an alpha level of 0.05, and a power of 0.70. Consequently (statistical test: difference between two independent means), a total of 46 individuals (23 in each group) were required). The study population consisted solely of female students enrolled in a women’s teacher training college. Given the nature of the institution, which exclusively caters to female students, it was deemed appropriate to focus the study on this specific population. This approach allowed for a more homogeneous sample and facilitated a deeper understanding of the phenomenon within this particular context.
The inclusion criteria consist of: being in the age range of 18–25 years, complete health of the nervous, muscular and skeletal system (except flexible flatfeet) [a navicular drop of 5–9 mm between both measurements was considered a normal arch, while a navicular drop of 10 mm or more was considered a low arch (flatfoot)37; also using the World Health Organization’s BMI classification system, individuals were categorized as underweight (BMI < 18.5), normal weight (18.5 ≤ BMI < 24.9), or overweight (25 ≤ BMI < 29.9].
The exclusion criteria consist of: structural flatfeet, professional athletes or individual who had regular sports activities, volunteers with obvious symptoms of abnormalities in the lower limbs and feet (except flexible flatfeet), history of neurological, rheumatic, metabolic diseases, mental disorders, disorder in the vestibular system, history of balance disorder and frequent positional dizziness, severe trunk abnormalities such as severe scoliosis, and kyphosis38.
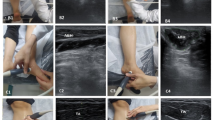
Testing procedure
In order to measure the endurance of the abdominal muscles and spinal extensor muscles, the Partial curl-up test and the maintaining plank position test were used. The partial curl-up test involves lying supine with knees bent at 140 degrees and feet flat on the floor. The participants performs controlled, slow repetitions of curling up their upper body, touching their fingertips to their knees, and then returning to the starting position. The test is terminated when the subject can no longer maintain proper form or reach the target number of repetitions. The number of correct repetitions is counted39,40. The plank test required the participants to maintain 90° between the trunk and elbows. Only the elbows and toes were allowed to touch the mat. Additionally, adjustable movements, if any, must be corrected within 3 s; otherwise, the assessment was terminated. The total time recorded while maintaining the proper position was included in the analysis41. The ICC for test–retest for the partial curl-up test and the plank test was provided in Table 1.
The static balance test was conducted using a Sharpened Romberg test. The subject stood without shoes on a flat surface, with their dominant foot in tandem with their non-dominant foot. Their hands crossed on the chest, and their eyes were closed. The time the person is able to maintain the posture before the balance is disturbed was considered as the person’s score42. The ICC for test–retest for the Sharpened Romberg test was provided in Table 1.
The Y-test was used to measure dynamic balance. The subject stood with one leg, the stance leg, on the starting block, and used her opposite leg, the reach leg, to push the reach indicator box as far as possible in the anterior, posterolateral, and posteromedial directions. Each participant completed 3 testing trials in each direction with each leg after completing 6 practice trials. Only the values from the 3 testing trials were used to calculate the subject’s scores. Scores for each direction were calculated by dividing the average reach distance (in cm) by the participant’s leg length (in cm) and multiplying by 100 to get the percentage of the leg length. To calculate the composite score, the sum of maximum reaches in each of the 3 directions was divided by 3 times the leg length43. The ICC for test–retest for the Y-test was provided in Table 1.
A 4 × 9-m shuttle run test was used to measure agility. With the 4 × 9-m shuttle run, the subjects stood behind the starting line and on command, they started the 9-m run. At the end of the 9-m section, the subjects were asked to stop with one foot beyond a marker, while reversing the running direction and sprinting back to the start where the same reversing of movement direction was required. After the fourth 9-m section, when the subjects crossed the finish line, the time was stopped. A hand-held stopwatch was used to measure the sprint time to the nearest 0.01 s (Q & Q, HS43, China). The best value of two consecutive trials was used for the statistical analysis44. The ICC for test–retest for the 4 × 9-m shuttle run test was provided in Table 1.
The Functional Movement Screening Test (FMS) was used to assess functional performance in individuals. The study used a 0–3 ordinal system, with scores ranging from 3 for perfect performance to 0 for pain-related movements. The FMS included seven tests: deep squat, hurdle step, in-line lunge, shoulder mobility, active straight leg raise, trunk stability push-up, and rotary stability. The composite score for all seven movements was recorded. Instruments utilized for the Functional Movement Screening test included the FMS Kit which includes a measuring device, hurdle step, stretch bands, measuring stick31,45,46. The ICC for test–retest for the FMS test was provided in Table 1.
Statistical analysis
All information is presented based on mean and standard deviation. The Independent t-test, the Pearson’s Correlation Coefficient and the Linear Regression were used for statistical analysis of the data. Before conducting these tests, the Shapiro–Wilk test was used to check the normality of the data, and the Levene’s test was used to check the equality of variances. Since for the variables of static and dynamic balance, agility and endurance of spinal extensor muscles, normality and equality of variances (homogeneity of variance) was not met; therefore, the equivalent non-parametric test (Mann–Whitney U test) was used for inter-group comparison. To investigate the correlation between functional movement scores and variables of balance, agility, and endurance, the Pearson’s correlation test was first done; subsequently, a logistic regression analysis was conducted. Prior to this, necessary assumptions were verified, including the absence of perfect multicollinearity through Pearson correlation coefficients and the linearity of the relationship using scatterplots.. A significance level of 0.05 was considered for all calculations. All statistical calculations were done using IBM SPSS Statistics v.24 software.
Results
The demographic characteristics of the subjects by group are presented in Table 2. As can be seen, there is a significant difference between two groups in the weight and body mass index (BMI), but no significant difference was found in the age and height. Also, there was considerable variability in BMI within both groups. This variability may be attributed to factors such as sample heterogeneity and the influence of confounding variables like genetics and physical activity levels47,48. Previous studies have indicated a link between obesity and flatfeet6. However, our findings showed that the flatfeet group had a higher BMI compared to the normal feet group in the current study.
The independent t-test was used to compare between groups in the variables of functional movements and endurance of abdominal muscles. Non-parametric Mann–Whitney U test was used for inter-group comparison of variables of static balance, dynamic balance, agility and endurance of spinal extensor muscles. There is a significant difference between the two groups in the test of functional movements, endurance of abdominal muscles, static balance and endurance of spinal extensor muscles (Table 3).
Pearson’s correlation test was used to investigate the correlation between the scores of functional movements with health- and motor skill-related variables in the flexible flatfeet group and the normal feet group (Before, the data of static balance, dynamic balance, agility and endurance of spinal extensor muscles were normalized using a two-step approach for transforming continuous variables to normal data in SPSS—the Rank Fractional Cases and Compute Variables49). In order to investigate this relationship, health- and motor skill-related factors were considered as predictor variables and functional movement test as criterion variable (Tables 4, 5).
According to the correlation coefficient results that values are not significant at the 0.05 level; it can be concluded that the health- and motor skill-related factors in the flatfeet group are not correlated with the functional movement test.
According to the correlation coefficient results, it can be concluded that the functional movements test has a relationship with the abdominal muscle endurance variable with a correlation value of 0.476, and the functional movements test has a relationship with the dynamic balance variable with a correlation value of 0.415. Since these coefficients are positive, the relationship between these variables is parallel. This means that by increasing the endurance of the abdominal muscles and dynamic balance, the functional movement test scores will increase. The functional movements test has a relationship with the agility variable with a correlation value of − 0.309. Since this coefficient is negative, the relationship between these two variables is inverse. This means that by reducing the time of the agility test, the scores of the functional movements test will increase.
Therefore, in order to investigate whether the endurance of abdominal muscles, dynamic balance and agility can significantly predict the results of the functional movements test, we investigated the relationship between the variables and the logical connection between the significant correlations by a logistic regression test (Table 6); prior to conducting the logistic regression analysis, the functional movement score variable was dichotomized.
The results indicated that abdominal muscle endurance (B = 0.316, Exp(B) = 1.37) was significantly associated with higher functional movement scores. This means that for every one-unit increase in abdominal muscle endurance, the odds of achieving a higher functional movement score increased by approximately 1.37 times. Similarly, dynamic balance (B = 0.091, Exp(B) = 1.095) was also positively associated with functional movement scores, although to a lesser extent. Individuals with greater abdominal muscle endurance and dynamic balance were more likely to have higher functional movement scores.
Discussion
The aim of this study was to compare functional movement and health- and motor skill-related fitness in women with and without flexible flatfeet. The main result of the present study was that the test scores of functional movements, abdominal muscle endurance, static balance and spinal extensor muscle endurance were significantly lower in individual with flexible flatfeet than in the group with normal feet. On the other hand, there was a significant correlation between functional movement test scores with abdominal muscle endurance, dynamic balance, and agility scores in individual with normal feet (that is, abdominal muscle endurance, dynamic balance, and agility scores are able to predict functional movement test scores); however, no significant correlation was found between the functional movement test scores and health- and motor skill-related factors in the flexible flatfeet group.
The results showed that the scores of functional movements are significantly lower in the flexible flatfeet group than the normal feet group (Table 3); in other words, foot biomechanics affects the movement performance of people in static and dynamic state. The results of the present study were not consistent with the study of Fallahasady et al.32. Probably due to the fact that Fallahasady et al. investigated the relationship between lumbar hyperlordosis deformity and Functional Movement Screening (FMS) scores32; while in this research, the relationship between flexible flatfeet deformity and Functional Movement Screening scores has been investigated. Therefore, the inconsistency of the investigated abnormalities can be the reason for the inconsistency of the two studies.
The postural of the feet and ankles affects the performance of all activities based on weight bearing such as: standing, bending, reaching, squatting, walking and lunging50. Since the functional movements include deep squat, in-line lunge, and hurdle step, therefore, probably individual with flexible flatfeet due to the limitation of dorsiflexion28 in performing these dynamic movements provide a weaker performance than individual with normal feet—that is, the lack of dorsiflexion in the ankle directly affects flexion and extension of the knee. Since many weight-bearing activities such as squatting and lunging require ankle dorsiflexion and knee flexion simultaneously28; therefore, it probably has an effect on reducing the scores of functional movements in the flatfeet group.
The results showed that the static balance is significantly lower in the flexible flatfeet group than the normal feet group (Table 3). The results of the present study were consistent with the studies of Khramtsov et al., Al Abdulwahab and Kachanathu, Song et al.21,23,24. Feet connection with the ankle, knee and hip joints form the kinematic chain of the lower body which regulates the balance of the body in a static and dynamic state. The feet are located at the farthest point of this chain and act as a base of support for the kinematic chain51. Based on this, it is believed that any small dynamic change in the feet affects the control of body posture20. But the results of the present study were not consistent with the study of Cote et al.20. Probably because Cote et al. used the Chattecx balance system to measure postural sway during standing on one leg with eyes open and closed, while this research used the Sharpened-Romberg balance test to evaluate balance42). Therefore, the use of different methods to evaluate static balance can be the reason for the inconsistency of the two studies.
The results showed that the endurance of abdominal and spinal extensor muscles is significantly lower in the flexible flatfeet group than the normal feet group (Table 3). The results of the present study were consistent with the study of Elataar et al.52. The position of the skeletal structures directly affects the adjacent structures25. It can be assumed that a change in the position of the foot can lead to a change in the posture and movement of the proximal joints26,27. As result, after flatfeet deformity, pronation of the foot causes internal rotation of the tibia, knee valgus and hip internal rotation occurs when weight bearing. This affects the muscular chain, causing pelvis position changes25,27 which ultimately causes instability of the trunk and a decrease in the endurance of core muscles27,28,29.
The results showed a positive correlation between the results of the functional movement screening test (FMS) with abdominal muscle strength and dynamic balance (Y test) in the normal feet group. The results of the present study were consistent with the study of Harshbarger et al. and Chang et al.53,54. Harshbarger et al. attributed the significant correlation to the fact that both assessments require central muscle stability to maintain postural stability during limb movements53.
Also, consistent with Chang et al.54, our study found a positive correlation between agility scores and FMS scores. Chang attributed the correlation between agility test scores and FMS test to similar task requirements (better central muscle stability and dynamic balance control for task execution54). However, logistic regression analysis did not support a significant predictive relationship between agility and FMS (Tables 5 and 6), suggesting that while these variables are related, agility may not be a strong predictor of overall FMS performance.
The study found no significant correlation between functional movement screening test results and agility, coordination, dynamic balance, and central muscle strength scores in the flatfeet group. Despite reduced health and motor skill-related factors, individuals with flexible flatfeet can overcome impairments in motor skill-related factors like dynamic balance and coordination during daily activities and movement55, but movements of FMS are not movements that are constantly repeated. Therefore, a significant correlation between health- and motor skill-related factors with the FMS test was not discovered in the flexible flatfeet group.
A limitation of this study was the unequal sample size between the two groups, particularly the smaller sample size in the flexible flatfoot group. This imbalance may have influenced the statistical power of the study and could potentially limit the generalizability of the findings to a broader population. Additionally, the study population was limited to female students, which may restrict the generalizability of the results to a wider population. Future research should aim to recruit larger and more balanced samples, including both male and female participants, to address these limitations and enhance the robustness of the findings.
Conclusion
The deformity of flexible flatfeet can cause defects in people’s health- and motor skill-related factors, which, as a result, affects people’s movement performance; therefore, according to this study, patients should be aware of this potential deficiency and as a result, benefit from appropriate rehabilitation exercises for the conservative treatment of flexible flatfeet.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request, due to the confidentiality of participants’ information.
References
Williams, D. S. et al. Lower extremity kinematic and kinetic differences in runners with high and low arches. J. Appl. Biomech. 17(2), 153–163 (2001).
Levinger, P. et al. A comparison of foot kinematics in people with normal-and flat-arched feet using the Oxford Foot Model. Gait Posture 32(4), 519–523 (2010).
Tsai, L.-C. et al. Comparison of different structural foot types for measures of standing postural control. J. Orthop. Sports Phys. Ther. 36(12), 942–953 (2006).
Dahle, L. K. et al. Visual assessment of foot type and relationship of foot type to lower extremity injury. J. Orthop. Sports Phys. Ther. 14(2), 70–74 (1991).
Hogan, M. T. & Staheli, L. T. Arch height and lower limb pain: An adult civilian study. Foot Ankle Int. 23(1), 43–47 (2002).
Pita-Fernandez, S. et al. Flat foot in a random population and its impact on quality of life and functionality. J. Clin. Diagnost. Res. 11(4), 22 (2017).
Dare, N., Onyije, F. & Osoma, S. Pes planus (flatfoot) in male and female adults of Bayelsa-Nigeria. Electron. J. Biomed. 3, 17–21 (2012).
Pfeiffer, M. et al. Prevalence of flat foot in preschool-aged children. Pediatrics 118(2), 634–639 (2006).
Shibuya, N. et al. Characteristics of adult flatfoot in the United States. J. Foot Ankle Surg. 49(4), 363–368 (2010).
Sachithanandam, V. & Joseph, B. The influence of footwear on the prevalence of flat foot. A survey of 1846 skeletally mature persons. J. Bone Joint Surg. Br. 77(2), 254–257 (1995).
Mulligan, E. P. & Cook, P. G. Effect of plantar intrinsic muscle training on medial longitudinal arch morphology and dynamic function. Manual Therapy 18(5), 425–430 (2013).
Lobo, M. & Greisberg, J. Adult acquired flatfoot. Foot Ankle Core Knowl. Orthop. 1, 38–57 (2007).
Arachchige, S. N. K., Chander, H. & Knight, A. Flatfeet: Biomechanical implications, assessment and management. Foot 38, 81–85 (2019).
Menz, H. B., Morris, M. E. & Lord, S. R. Foot and ankle risk factors for falls in older people: A prospective study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 61(8), 866–870 (2006).
Frances, J. M. & Feldman, D. S. Management of idiopathic and nonidiopathic flatfoot. Instr. Course Lect. 64, 429–440 (2015).
Demetracopoulos, C. A. et al. Outcomes of a stepcut lengthening calcaneal osteotomy for adult-acquired flatfoot deformity. Foot Ankle Int. 36(7), 749–755 (2015).
Kaoulla, P., Frescos, N. & Menz, H. B. A survey of foot problems in community-dwelling older Greek Australians. J. Foot Ankle Res. 4(1), 1–7 (2011).
Gorter, K. J., Kuyvenhoven, M. M. & de Melker, R. A. Nontraumatic foot complaints in older people. A population-based survey of risk factors, mobility, and well-being. J. Am. Podiatric Med. Assoc. 90(8), 397–402 (2000).
Menz, H. B. et al. Foot pain in community-dwelling older people: An evaluation of the Manchester Foot Pain and Disability Index. Rheumatology 45(7), 863–867 (2006).
Cote, K. P. et al. Effects of pronated and supinated foot postures on static and dynamic postural stability. J. Athletic Train. 40(1), 41 (2005).
Khramtsov, P. & Kurganskiĭ, A. Functional stability of the vertical posture in children depending on foot arch condition. Vestnik Rossiiskoi akademii meditsinskikh nauk 5, 41–44 (2009).
Harrison, P.-L. & Littlewood, C. Relationship between pes planus foot type and postural stability. Indian J. Physiother. Occup. Therapy 4(3), 21–24 (2010).
Al Abdulwahab, S. S. & Kachanathu, S. J. The effect of various degrees of foot posture on standing balance in a healthy adult population. Somatosensory Motor Res. 32(3), 172–176 (2015).
Song, J.-Y., Park, S.-H. & Lee, M.-M. The comparison of the difference in foot pressure, ground reaction force, and balance ability according to the foot arch height in young adults. Ann. Appl. Sport Sci. 9(2), 0 (2021).
Kothari, A. et al. Are flexible flat feet associated with proximal joint problems in children?. Gait Posture 45, 204–210 (2016).
Maffetone, P. The assessment and treatment of muscular imbalance—The Janda approach. J. Bodywork Movement Therap. 14(3), 287–288 (2010).
Khamis, S. & Yizhar, Z. Effect of feet hyperpronation on pelvic alignment in a standing position. Gait Posture 25(1), 127–134 (2007).
Price, J., The biomechanics method for corrective exercise. In Human Kinetics (2018).
Izraelski, J. Assessment and treatment of muscle imbalance: The Janda approach. J. Can. Chiropract. Assoc. 56(2), 158 (2012).
Cook, G. et al. Functional movement screening: The use of fundamental movements as an assessment of function-part 1. Int. J. Sports Phys. Therapy 9(3), 396 (2014).
Cook, G., Burton, L. & Hoogenboom, B. Pre-participation screening: The use of fundamental movements as an assessment of function—Part 2. North Am. J. Sports Phys. Therapy 1(3), 132 (2006).
Fallahasady, E. et al. The relationship between core muscle endurance and functional movement screen scores in females with lumbar hyperlordosis: A cross-sectional study. BMC Sports Sci. Med. Rehabil. 14(1), 1–8 (2022).
Yalcin, E. et al. Isokinetic measurements of ankle strength and proprioception in patients with flatfoot. Isokinetics Exerc. Sci. 20(3), 167–171 (2012).
Şahin, F. N. et al. Examining the relationship between pes planus degree, balance and jump performances in athletes. Int. J. Environ. Res. Public Health 19(18), 11602 (2022).
Shrader, J. A. et al. Navicular drop measurement in people with rheumatoid arthritis: Interrater and intrarater reliability. Phys. Therapy 85(7), 656–664 (2005).
Zhang, C.-Q. et al. The effects of mindfulness training on beginners’ skill acquisition in dart throwing: A randomized controlled trial. Psychol. Sport Exerc. 22, 279–285 (2016).
Marouvo, J., Castro, M. & Sousa, F. Correlation between different tests to diagnose flatfoot condition. In Advances and Current Trends in Biomechanics 192–196 (CRC Press, 2021).
Hedayati, R., et al., The attention needed for balance controlling in young patients with flatfoot. In Koomesh 25–34 (2016).
Ozcan Kahraman, B. et al. Developing a reliable core stability assessment battery for patients with nonspecific low back pain. Spine 41(14), E844–E850 (2016).
Sidney, K. & Jetté, M. The partial curl-up to assess abdominal endurance: Age and sex standards. Res. Sports Med. Int. J. 2(1), 47–56 (1990).
Laurson, K. R., et al., Designing health-referenced standards for the plank test of core muscular endurance. In Measurement in Physical Education and Exercise Science 1–8 (2022).
Yim-Chiplis, P. K. & Talbot, L. A. Defining and measuring balance in adults. Biol. Res. Nurs. 1(4), 321–331 (2000).
Plisky, P. J. et al. Star excursion balance test as a predictor of lower extremity injury in high school basketball players. J. Orthopaed. Sports Phys. Therapy 36(12), 911–919 (2006).
Makhlouf, I. et al. Combination of agility and plyometric training provides similar training benefits as combined balance and plyometric training in young soccer players. Front. Physiol. 9, 1611 (2018).
Cook, G., Burton, L. & Hoogenboom, B. Pre-participation screening: The use of fundamental movements as an assessment of function–part 1. North Am. J. Sports Phys. Therapy 1(2), 62 (2006).
Everard, E. M., Harrison, A. J. & Lyons, M. Examining the relationship between the functional movement screen and the landing error scoring system in an active, male collegiate population. J. Strength Condition. Res. 31(5), 1265–1272 (2017).
Fesinmeyer, M. D. et al. Genetic risk factors for BMI and obesity in an ethnically diverse population: Results from the population architecture using genomics and epidemiology (PAGE) study. Obesity 21(4), 835–846 (2013).
Schwarzfischer, P. et al. BMI and recommended levels of physical activity in school children. BMC Public Health 17, 1–9 (2017).
Templeton, G. F. A two-step approach for transforming continuous variables to normal: Implications and recommendations for IS research. Commun. Assoc. Inf. Syst. 28(1), 4 (2011).
Schamberger, W. The Malalignment Syndrome: Implications for Medicine and Sport (Elsevier Health Sciences, 2012).
Dawe, E. J. C. & Davis, J. (vi) Anatomy and biomechanics of the foot and ankle. Orthopaed. Trauma 25(4), 279–286 (2011).
Elataar, F. F. et al. Core muscles’ endurance in flexible flatfeet: A cross-sectional study. J. Musculoskeletal Neuronal Interact. 20(3), 404 (2020).
Harshbarger, N. D., Anderson, B. E. & Lam, K. C. Is there a relationship between the functional movement screen, star excursion balance test, and balance error scoring system?. Clin. J. Sport Med. 28(4), 389–394 (2018).
Chang, W.-D. et al. Comparison of functional movement screen, star excursion balance test, and physical fitness in junior athletes with different sports injury risk. BioMed Res. Int. 8, 2020 (2020).
Shumway-Cook, A. & Woollacott, M. H. Motor Control: Translating Research into Clinical Practice (Lippincott Williams & Wilkins, 2007).
Acknowledgements
We would like to express our special gratitude to all the students who voluntarily participated in this study.
Author information
Authors and Affiliations
Contributions
RY, HS and MG conceived of the presented idea. RY, HS, MG and G A. K developed the study and performed the measurement. RY and MG done the statistical analysis. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study obtained ethical clearance from the Sport Sciences Research Institute. Prior to participation, all students were informed about the study’s objectives, and written and verbal informed consent was obtained from each participant.
Consent for publication
We give our consent for the publication of identifiable details, which can include details within the text (“Material”) to be published in the above Journal and Article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ghorbani, M., Yaali, R., Sadeghi, H. et al. The impact of flatfeet on the correlation between functional movement scores, balance, agility, and core muscle strength in young females: a cross-sectional study. Sci Rep 15, 5077 (2025). https://doi.org/10.1038/s41598-025-89364-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-89364-8