Abstract
To enhance attention on low-income patients with hemophilia, it is essential to urge governments and coagulation factor manufacturers to increase their investment in hemophilia care. This would ensure that low-income patients receive an adequate supply of clotting factors for both replacement therapy and prophylaxis. Clinical data from 171 low-income hemophilia patients were collected in Shandong Province between January 2017 and December 2019. “Low-income” is defined as having a per capita disposable income below the average for the years 2017 to 2019 in Shandong Province. The data collected included age, education, activity levels of factor VIII/IX and anti-factor VIII/IX inhibitors, therapeutic regimen, viral infections, and annual bleeding rate (ABR). Additionally, the translated and validated Chinese version of the Haemophilia Quality of Life questionnaire for adults (Haem-QoL-A), Hemophilia Joint Health Scores (HJHS), and annualized consumption of factor VIII or prothrombin complex concentrate (PCC) were applied. In our study, a total of 171 male patients—131 adults and 40 children—were included, and the median age was 30 years. The average annual income of these patients was $446.9. Of these, 133 patients (77.8%) were diagnosed with hemophiliac arthropathy. Eight out of 150 patients had anti-factor VIII inhibitors, while only one patient had anti-factor IX inhibitors. Among the 171 patients, only six children received low-dose prophylaxis (10–15 IU/kg, 1–2 times per week), while the remaining 165 patients received only inadequate on-demand treatment. In terms of viral infections, 20 patients (11.7%) were infected with transfusion-associated viruses. The median annual bleeding rate (ABR) was 20 bleeding events per year (range: 2-100). The mean Haem-QoL-A score was 62.3 ± 14.5. The mean total Hemophilia Joint Health Score (HJHS) for children was 8.1 ± 7.1, and for adults with hemophilia A or B (HA/HB), it was 40.1 ± 20.0 (P < 0.05). The annual per capita factor dosage for the 171 low-income hemophilia patients was calculated to be 6,182 IU/year. Providing additional support and care for low-income patients is crucial. Early prophylaxis in children is particularly important for protecting joint health.
Similar content being viewed by others
Introduction
Hemophilia is an X-linked congenital bleeding disorder resulting from a deficiency in coagulation factor VIII (FVIII) in hemophilia A (HA) or factor IX (FIX) in hemophilia B (HB). This deficiency arises from mutations in the respective clotting factor genes1. Common sites of severe bleeding in hemophilia patients include joints (hemarthrosis), muscles (particularly deep compartments such as the iliopsoas, calf, and forearm), and recurrent joint hemorrhages, which can lead to chronic arthropathy and even the loss of joint movement2. Currently, replacement therapy involves the administration of FVIII and FIX concentrates via intravenous injection, either episodically to treat acute bleeding or according to prophylactic regimens to prevent bleeding episodes3. However, activated prothrombin complex concentrate (aPCC) is not available in China, and many hemophilia B patients, as well as those with anti-FVIII/FIX inhibitors, are treated with prothrombin complex concentrate (PCC). A global study on factor VIII use has shown that replacement therapy has significantly improved the morbidity and mortality of individuals with hemophilia A in high-income countries4,5. The use of factor replacement therapy has also increased in developing countries. However, for some low-income patients in these regions, particularly in Shandong Province, limited visibility of hemophilia and the high cost of treatment result in inadequate care. This inadequate treatment leads to severe consequences, including chronic pain, joint deformities, arthropathy, disabilities, and even death during childhood or early adulthood6. The income level of patients within a country plays a significant role in determining their access to treatment and overall prognosis. In low- and lower-middle-income countries with limited healthcare resources, some hemophilia patients die from bleeding without receiving any replacement therapy, while those who survive often face joint deformities and other disabilities7. Therefore, a retrospective analysis of clinical data is essential for identifying issues and implementing early interventions. This approach can help reduce the incidence of joint arthropathy, improve patient quality of life, and establish a foundation for future targeted interventions.
Patients and methods
Patients
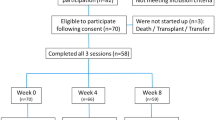
This descriptive study included 171 low-income hemophilia patients who received targeted poverty alleviation assistance at our center from January 2017 to December 2019. Over the three-year period, the Shandong Provincial Health Commission and the Shandong Hemophilia Diagnosis and Treatment Center collaboratively implemented precision poverty alleviation efforts for hemophilia patients, providing a total of $684,931 worth of blood-derived coagulation factors free of charge to low-income hemophilia patients in Shandong Province. According to the Shandong Provincial Bureau of Statistics, the per capita annual disposable income in the province was $4,000 from 2017 to 2019, with the national poverty alleviation threshold defined as an annual income of less than $446.9. The annual income of the patients enrolled in this study was provided by the local government. Targeted poverty alleviation for hemophilia involves providing free human coagulation factors (FVIII and PCC) to low-income patients, through support from the Shandong Provincial Health Commission and plasma-derived medicinal product manufacturers, such as Shandong Taibang Co., Ltd. The study was approved by the Ethics Committee of Shandong Blood Center and conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all enrolled patients and their legally authorized guardians.
Study variables and definitions
According to the international definition, the severity of hemophilia is categorized based on clotting factor activity levels: mild (0.05–0.40 IU/dL), moderate (0.01–0.05 IU/dL), or severe (< 0.01 IU/dL)8. This study collected various patient characteristics, including sex, age, education (China’s education system includes primary school, junior high school, senior high school, and college, with the latter two being considered higher education), and marital status (defined as reaching the legal marriage age in China). Clinical symptoms, family history (either familial or sporadic), type of hemophilia, disease severity, presence of hemophilia arthropathy (including chronic pain, decreased joint range of motion, loss of strength, and functional disability), viral infections, and presence of anti-FVIII/FIX inhibitors were also recorded. Additionally, information on bleeding events and replacement treatments—such as on-demand treatment, insufficient treatment (where coagulation factor replacement therapy is only used for severe bleeding episodes like intracranial or gastrointestinal bleeding, or when bleeding causes unbearable pain), and low-dose prophylaxis (10–15 IU/kg, 1–2 times per week)—was collected.
Laboratory diagnosis and testing
FVIII: C and FIX:C levels were measured using one-stage clotting assays (Coagpia® APTT-N; Sysmex Co.). Anti-FVIII/FIX inhibitors were screened and quantified using the Bethesda assay. A positive inhibitor titer was defined as > 0.6 Bethesda units (BU)/mL, with a titer ≥ 5 BU considered a hig titer.
Blood-borne virus detection
HBsAg (hepatitis B surface antigen), HCV antibody, HIV antibody/antigen, and RPR (anti-TP, syphilis) tests were performed using ELISA. Two different reagents were used for the initial test and retest. If both reagents tested positive, the result was considered positive. If one reagent tested positive, a retest was required; if any reagent tested positive during the retest, the result was considered positive. In cases of a positive anti-HIV test, confirmation was obtained by sending the sample to the Shandong Centers for Disease Control and Prevention in China for Western blotting (WB) testing.
ABR, Haem-QoL-A and HJHS
The annualized bleeding rate (ABR) was recorded through patient medical history inquiries. Bias was considered due to potential inaccuracies in self-reported bleeding events. The translated and validated Chinese version of the Haemophilia Quality of Life Questionnaire for Adults (Haem-QoL-A) was used9. This questionnaire consists of 41 items across four domains: physical health, emotions and feelings, work and school, and treatment. Missing data were recorded as 0 and were excluded from the scoring process. For both total score analysis and analysis of each Haem-QoL-A domain, the scale scores were converted to a 0–100 scale, where 0 represents the best quality of life and 100 represents the worst. Joint status was assessed using the Hemophilia Joint Health Score (HJHS) version 2.1, which includes six individual joint scores (ranging from 0 to 20) and a global gait score (ranging from 0 to 4), yielding a total score (0–124). A higher HJHS indicates worse joint health.
Statistical analysis
Data analysis was performed using the statistical software SPSS 20.0 (SPSS, Inc., Chicago, IL, USA). Descriptive statistics are presented as frequencies and percentages for categorical variables. Continuous data are reported as medians with ranges (25th–75th percentile) or means with standard deviations (SDs). Factor consumption was analyzed using paired t-tests, provided that normality was confirmed. The significance level was set at P < 0.05. Pearson’s correlation was used to assess the strength of associations between the HJHS score and the Haem-QoL-A score.
Results
Clinical data of hemophilia patients
The study included 171 participants, and their sociodemographic characteristics, health conditions, and clinical data are presented in Table 1.
Bloodborne infections
A total of 161 hemophilia patients were tested for HBsAg, anti-HCV, anti-HIV, and anti-TP. The percentages of patients who tested positive for HBsAg, anti-HCV, anti-HIV, and anti-TP were 4.3% (7/161), 8.7% (14/161), 0.6% (1/161), and 0% (0/161), respectively. Significant differences were observed in the anti-HCV positivity rates between the different age groups (> 18 years vs. ≤18 years), while no significant differences were found in the other viral infection groups (Table 2).
Bleeding and quality of life
In our study, 77.8% of hemophilia patients had joint arthropathy, as assessed through joint evaluation. Prior to the implementation of targeted poverty alleviation measures, 102 patients received on-demand treatment, 63 never received treatment or only received infusion of plasma-derived products in cases of severe bleeding (Table 3). The median annual bleeding rate (ABR) was 20 bleeding events/year (range: 2-100). A total of 131 adult patients participated in the Haem-QoL-A questionnaire, of whom 9 were excluded due to incomplete responses; Joint disease status was evaluated in 94 patients, while the remaining 37 could not be evaluated due to severe joint deformities. Of the 40 pediatric patients, 31 (77.5%) were evaluated using the HJHS, and the remaining 9 were not evaluated due to acute bleeding. The mean HJHS scores of adults in different age groups (18–40 years and > 40 years) were 35.31 ± 19.05 and 51.25 ± 17.95, respectively, while the mean HJHS was significantly lower in the pediatric population (8.1 ± 7.1) (Fig. 1). In the 94 adults, Pearson’s correlation was used to assess the strength of the association between the HJHS score (40.06 ± 20.02) and the Haem-QoL-A score (61.47 ± 16.10), revealing a weak positive relationship (r = 0.273, P = 0.008, < 0.05) (Fig. 2).
Discussion
As the most populous country in the world, China is estimated to have at least 130,000 individuals with hemophilia10. Based on the population distribution in Shandong Province, there should be over 5,000 hemophilia patients. However, only more than 3,000 hemophilia patients are currently registered at the Shandong Hemophilia Treatment Center. It is important to recognize that many patients remain unregistered, a situation primarily attributed to limited awareness of hemophilia and economic constraints. The establishment of the Hemophilia Treatment Center Collaborative Network of China (HTCCNC) in 2004 has contributed to the gradual improvement of hemophilia care nationwide. Additionally, the inclusion of coagulation factor products for hemophilia treatment in the National Medical Insurance System has significantly alleviated the economic burden on individuals with hemophilia11. With China’s economic development, both the government and healthcare institutions have increased their investments in hemophilia care, leading to more standardized treatment for low-income patients. In light of these findings and in line with the Healthy China Initiative and targeted poverty alleviation policies, we conducted a retrospective study of 171 low-income hemophilia patients from January 2017 to December 2019. Despite these advancements, some impoverished hemophilia patients continue to face challenges in diagnosis and treatment, both in China and globally. Therefore, our study aims to advocate for greater support from governmental organizations, medical insurance systems, and social workers to assist low-income hemophilia patients.
In our study, 50.8% of patients had moderate hemophilia, while 43.8% had severe disease. Contrary to findings from other studies12,13 our cohort exhibited a lower proportion of severe disease. This discrepancy may be attributed to the fact that bleeding is more common and easily detectable in patients with moderate to severe hemophilia. The most frequent hemorrhagic manifestations in these patients were recurrent hemarthroses, particularly in the elbows, knees, and ankles, which led to progressive joint destruction, irreversible crippling arthropathy, and chronic pain14,15. We found that 53.8% of the patients had a family history of hemophilia, which aligns with other studies reporting that approximately 30% of individuals newly diagnosed with hemophilia have no family history, often due to de novo mutations12,16, Regarding education, the majority of our participants had primary education (38.0%), followed by 25.7% with junior high school education. Similar findings were reported in Bangladesh, where educational attainment in hemophilia patients was also limited due to poverty and illness17. As a result, few patients in our study were able to complete higher education. In the UK, a national register of hemophilia patients has been maintained since 1968, with about 5,000 individuals with hemophilia A registered. The prevalence of hemophilia B is approximately one-fifth that of hemophilia A13. In our study, we observed that 87.7% of patients had hemophilia A and 12.3% had hemophilia B. This is consistent with the general prevalence of bleeding disorders, where hemophilia A is the most common (72.3%), followed by hemophilia B (11.5%)17. This suggests that hemophilia B may present less frequently, potentially leading to fewer patients seeking hospital care.
In China, recombinant or highly purified plasma-derived factor concentrates are unavailable for prophylaxis in a significant number of low-income hemophilia patients due to their high cost. Historically, blood transfusion with Fresh Frozen Plasma (FFP) and cryoprecipitation have been the primary approaches for managing these patients. However, these methods pose a high risk of transfusion-transmitted infections (TTIs). Our study revealed a 4.3% rate of HBsAg positivity, which aligns with the hepatitis B positivity rate of 628 hemophilia patients in our center in 2012. The relatively low prevalence of HBV in our patients may be attributed to mandatory HBV screening for blood donors and the introduction of the HBV vaccination program in 1992 18. Hepatitis C (HCV) infection, another major cause of mortality in hemophilia patients19,20. is primarily transmitted through the administration of pooled factor concentrates, cryoprecipitates, or FFP21. The HCV infection rate detected in our center was 8.7%. Notably, all the infected patients were over 18 years old, which can be attributed to the fact that, since 1993, anti-HCV testing has been included in the routine blood screening of healthy blood donors, leading to the elimination of most anti-HCV-positive individuals. By the end of 2014, the HIV/AIDS incidence in China was reported to be 0.037% of the total population21.
However, our study found that 0.58% (1/171) of the patients were co-infected with HCV and HIV, which is primarily linked to previous unsafe blood transfusions. Fortunately, we did not identify any syphilis-positive patients, though it is important to emphasize the need for timely anti-TP testing in hemophilia patients to prevent transfusion-related infections. Therefore, it is crucial to focus on preventing viral infections and improving blood quality, as these factors directly influence the prognosis and quality of life for hemophilia patients.
Inhibitors are a serious complication of replacement therapy for patients with hemophilia A and B. A major complication in approximately 30% of patients is the development of alloantibodies (inhibitors) that inactivate factor VIII activity. This may necessitate the use of extremely costly bypassing agents or the induction of immune tolerance therapy, both of which can significantly impact patients’ quality of life and complicate their medical management22. The main risk factors for the development of inhibitors in hemophilia include ethnicity, family history23, gene mutation type24, exposure day25, a and FVIII product choices26,27. Patients with transient inhibitors, or those whose inhibitors have been eliminated through treatment, are excluded from prevalence data. However, they would be included in incidence data (the number of new cases within a defined period, typically one year) or cumulative incidence data (the number of new cases over a more extended period, adjusted for varying follow-up durations of different patients)28. In our study, all inhibitor-positive patients did not receive immune tolerance therapy, and it is possible that some patients may have had transient inhibitors. According to our statistical analysis, the incidence of inhibitors in 150 patients with hemophilia A at our center was 5.3%, which is significantly lower than the 20–30% incidence typically reported in the literature for hemophilia A29. Several factors may explain this lower incidence, including the infrequent infusion of coagulation factors, delayed inhibitor detection, or the advanced age at which coagulation factor infusion was initiated. Additionally, the prevalence of inhibitors in hemophilia B patients in our study was 4.8%. Giangrande PLF reported that the incidence of inhibitor development in hemophilia B patients is much lower than in hemophilia A patients, typically ranging from 1 to 6% 23. Our results are consistent with these findings, potentially due to the limited number of hemophilia B patients included in the study.
The 2020 (3rd edition) World Federation of Hemophilia (WFH) Guidelines for the Management of Hemophilia clearly indicate8. Although prophylaxis reduces the risk of breakthrough bleeds, and thus, there is a requirement for access to additional doses for prompt treatment. Approximately 10% of individuals with hemophilia, primarily in upper-middle-income countries, have some, though insufficient, access to therapies30, while the remaining 15% in high-income countries (HICs) have full access to advanced therapies and treatment regimens31. However, only approximately 75% of people with haemophilia worldwide, primarily in low-income countries (LICs) and lowermiddle-income countries (LMICs), have no or limited access to therapy32,33, This issue also affects our low-income patients with hemophilia in Shandong Province. The development of joint arthropathy in hemophilia patients is primarily attributed to insufficient on-demand or non-prophylaxis therapy, which is often due to economic constraints or limited drug availability. As a result, these patients develop varying degrees of arthropathy, some leading to disability. Clinical evidence from both China and other countries suggests that, compared with on-demand treatment, even a low-dose prophylaxis regimen can significantly reduce bleeding in children with hemophilia, though it may still result in some joint damage34,35. In China, among all registered hemophilia patients, only 15% of those aged < 18 years and 7% of those aged > 18 years were estimated to be receiving prophylaxis36. Currently, prophylaxis in children has significantly improved. Our study also found that children who received prophylaxis experienced fewer joint bleeding events compared to those who received on-demand treatment. Imaging studies revealed that 6 hemophilia patients (29%) receiving prophylaxis exhibited signs of joint disease, whereas 14 patients (74%) receiving intermittent treatment showed similar signs (P < 0.05)37. Therefore, promoting prophylactic treatment is essential for enhancing joint protection and improving the overall quality of life for these patients.
Under on-demand treatment, the HJHS scores were significantly higher in adult patients than in pediatric patients, and the scores increased with age. In our study, the mean total HJHS in children was 8.1 ± 7.1, whereas in adults with hemophilia A (HA) or B (HB), the mean score was 40.1 ± 20.0 (P < 0.05). However, Wilkins et al. reported that the median total HJHS in children with HA/HB was 0, while in adults with HA/HB, the median score was 18, with 11 out of 273 patients being compliant in recording treatment using HaemTracker38. Additionally, a study by Wilkins et al. on 29 adult participants with moderate hemophilia from 11 centers in England, Scotland, and Wales found the mean total score to be 10.8 ± 5.239. The median HJHS score for patients on prophylactic treatment in their study was 2 (range 0–17) for pediatric patients, with a median age of 10 years (range 6–15)40. These results are more favorable than those observed in our study. Furthermore, we found a positive correlation (r = 0.273, P = 0.008 < 0.05) between HJHS scores and Haem-QoL-A in adults. indicating that higher HJHS scores are associated with poorer quality of life. Although recent advances have led to substantial improvements in patient outcomes, patients with hemophilia continue to experience joint and functional impairment, acute and chronic pain, and poor mental health, all of which should have a negative impact on HRQoL41. The high Haem-QoL-A scores may reflect the ‘disability paradox,’ as observed in other studies with similar findings42. The disability paradox refers to the phenomenon where individuals with disabilities report levels of satisfaction and QoL comparable to or even higher than those without disabilities, despite facing significant challenges related to access, mobility, and societal participation43. Therefore, prophylactic treatment plays a crucial role in protecting the joints of hemophilia patients.
In 2018, according to the World Federation of Hemophilia, the per capita dosage of blood coagulation factor VIII was 2.40 IU globally, whereas in China, it was only 0.026 IU36, significantly lower than in European and American countries. This discrepancy is partly due to the fact that the vast majority of people with hemophilia A (PWHA) in countries like China and India have not been diagnosed or treated. Consequently, the per capita usage of factor VIII (IU per capita) does not accurately reflect the care provided to identified patients and can result in an unrealistic financial burden for concentrated FVIII expenditures, especially when a country does not allocate sufficient funds for hemophilia A treatment6. The amount of coagulation factor used by individuals with hemophilia A (PWHA) is indicated in International Units (IUs) per person. According to our center’s precision poverty alleviation program, the annual factor consumption for hemophilia A patients is only 18,450 IUs, significantly lower than the national average for Chinese patients. Specifically, the average usage of clotting factor VIII among hemophilia A patients in Shandong Province is approximately 20,382 IUs. The higher occurrence of joint deformities and disability among low-income patients can be attributed to their economic status, which has significantly impacted their standard of living. However, with the support of national poverty alleviation policies, charitable organizations, and the national health care system, low-income hemophilia patients now have access to life-saving treatments and increased medical insurance reimbursement rates. Despite this progress, prophylactic treatment remains perceived as prohibitively expensive, with an estimated annual per-patient cost of €129,365 in the UK and €196,117 in France44. In China, challenges such as a large patient population persist. Many patients discontinue or fail to adhere to treatment due to factors like long-term use, high costs, and the need for self-infusion or self-care. Furthermore, prophylaxis is not available for adult patients because the National Reimbursement Drug List (NRDL) does not provide financial assistance for adult prophylaxis, which may result in discontinuation of treatment for patients aged over 18 years45.
Although the clinical data of 171 patients were retrospectively analyzed in this study, we did not evaluate the Annual Bleeding Rate (ABR), Hemophilia Joint Health Score (HJHS), or Haem-QoL-A following the use of free coagulation factor FVIII or PCC replacement therapy. Additionally, the follow-up treatment of these patients was not assessed. Therefore, future research will focus on the continued monitoring of clinical data from these low-income patients. Furthermore, non-factor replacement therapies such as subcutaneous emicizumab and intravenous efanesoctocog alfa are not currently covered by health insurance in China, making these treatments prohibitively expensive for low-income hemophilia patients.
In conclusion, low-income hemophilia patients in Shandong Province face significant challenges, including insufficient treatment and a lack of prophylaxis. Unlike more than 70% of hemophilia patients globally, China has sufficient coagulation factor producers, yet these patients do not receive adequate care due to factors such as limited awareness of the disease and inadequate medical insurance policies. Our study highlights the critical unmet needs and challenges faced by individuals with hemophilia in Shandong Province. Addressing these issues requires a comprehensive approach, including improvements in healthcare infrastructure, expansion of the healthcare workforce, and securing sustainable funding. Increasing the availability of affordable prophylactic treatments through local manufacturing and public-private partnerships is essential.
Data availability
The data that support the findings of this study are available on request from the corresponding author.The data are not publicly available due to privacy or ethical restrictions.
References
Srivastava, A. et al. Guidelines for the management of hemophilia. Haemophilia 19 (1), e1-47. (2013). https://doi.org/10.1111/j.1365-2516. 2012. 02909.x.
Peyvandi, F., Garagiola, I. & Young, G. The past and future of haemophilia: diagnosis, treatments, and its complications. Lancet 388 (10040), 187–197. https://doi.org/10.1016/S0140-6736(15)01123-X (2016).
Mannucci, P. M. & Tuddenham, E. G. The hemophilias–from royal genes to gene therapy. N Engl. J. Med. 344 (23), 1773–1779. https://doi.org/10.1056/NEJM200106073442307 (2001).
Aledort, L. M. Unsolved problems in haemophilia. Haemophilia 4 (4), 341–345. https://doi.org/10.1046/j.1365-2516.1998.440341.x (1998).
Lee, C. A. Towards achieving global haemophilia care–World Federation of Hemophilia programmes. Haemophilia (4), 463–473. https://doi.org/10.1046/j.1365-2516.1998.440463.x (1998).
Stonebraker, J. S. et al. A study of reported factor VIII use around the world. Haemophilia 16 (1), 33–46. https://doi.org/10.1111/j.1365-2516.2009.02131.x (2010).
Ampaiwan Chuansumrit, T. et al. National strategic advocacy to manage patients with inherited bleeding disorders in low and lower-middle income countries. Expert Rev. Hematol. 16 (12), 1063–1076. https://doi.org/10.1080/17474086.2023.2293092 (2023).
Srivastava, A. et al. WFH guidelines for the management of Hemophilia, 3rd edition. Haemophilia 26 (S6), 1–158. https://doi.org/10.1111/hae.14046 (2020).
Lindvall, K. et al. Quality of life in adult patients with haemophilia - a single centre experience from Sweden. Haemophilia 18 (4), 527–531. https://doi.org/10.1111/j.1365-2516.2012.02765.x (2012).
Ozelo, M. C. et al. Meeting the challenges of haemophilia care and patient support in China and Brazil. Haemophilia 18 (Suppl 5), 33–38. https://doi.org/10.1111/j.1365-2516.2012.02890.x (2012).
Qu, C. et al. Analysis of hospitalization of people withhemophilia-12 years of experience in a single center. Res. Pract. Thromb. Haemostasis. 6 (5), e12764. https://doi.org/10.1002/rth2.12764 (2022).
Payal, V. et al. Clinical profile of hemophilia patients in Jodhpur Region. Asian J. Transfus. Sci. 10 (1), 101–104. https://doi.org/10.4103/09736247.164269 (2016).
Berntorp, E. et al. Nat. Rev. Dis. Primers 7(1):45. https://doi.org/10.1038/s41572-021-00278-x. (2021).
Roosendaal, G. et al. Haemophilic arthropathy: the importance of the earliest haemarthroses and consequences for treatment. Haemophilia 14 (Suppl 6), 4–10. https://doi.org/10.1111/j.1365-2516.2008.01882.x (2008).
Daffunchio, C. et al. Clinical and ultrasound evaluation of patients with haemophilia on prophylaxis. Haemophilia 27 (4), 641–647. https://doi.org/10.1111/hae.14312 (2021).
Ljung, R. C. & Sjorin, E. Origin of mutation in sporadic cases of haemophilia A. Br. J. Haematol. 106, 870–874 (1999).
Islam, M. N. et al. Clinical profile and demographic characteristics of moderate and severe hemophilia patients in a tertiary care hospital of Bangladesh. Orphanet J. Rare Dis. 17 (1), 254. https://doi.org/10.1186/s13023-022-02413-7.18 (2022).
Peng, H. M. et al. Transfusion-transmitted infections in hemophilia patients who underwent surgical treatment: a study from a single center in north China. Arch. Med. Sci. 16 (2), 308–312. https://doi.org/10.5114/aoms.2020.92892 (2020).
Mazepa, M. A. et al. Men with severe hemophilia in the United States: birth cohort analysis of a large national database. Blood 127 (24), 3073–3081. https://doi.org/10.1182/blood-2015-10-675140 (2016).
Franchini, M. et al. Treatment of chronic hepatitis C in haemophilic patients with interferon and Ribavirin: a meta-analysis. J. Antimicrob. Chemother. 61 (6), 1191–1200. https://doi.org/10.1093/jac/dkn119 (2008).
Alter, H. J. & Klein, H. G. The hazards of blood transfusion in historical perspective. Blood 112 (7), 2617–2626. https://doi.org/10.1182/blood-2008-07-077370 (2008).
van Velzen, A. S. et al. Intensity of factor VIII treatment and the development of inhibitors in non-severe hemophilia a patients: results of the INSIGHT case-control study. J. Thromb. Haemostasis: JTH. 15 (7), 1422–1429. https://doi.org/10.1111/jth.13711 (2017).
Giangrande, P. L. F. et al. European principles of inhibitor management in patients with haemophilia. Orphanet J. Rare Dis. 13 (1), 66. https://doi.org/10.1186/s13023-018-0800-z (2018).
Rosendaal, F. R. et al. Genetic risk stratification to reduce inhibitor development in the early treatment of hemophilia A: a SIPPET analysis. Blood 130 (15), 1757–1759. https://doi.org/10.1182/blood-2017-06-791756 (2017).
van den Berg, H. M. et al. Timing of inhibitor development in more than 1000 previously untreated patients with severe hemophilia A. Blood 134 (3), 317–320. https://doi.org/10.1182/blood.2019000658 (2019).
Franchini, M. et al. Systematic review of the role of FVIII concentrates in inhibitor development in previously untreated patients with severe hemophilia a: a 2013 update. Semin Thromb Hemost 2013, 39 (7), 752 – 66. (2013). https://doi.org/10.1055/s-0033-1356715
Marcucci, M. et al. Type and intensity of FVIII exposure on inhibitor development in PUPs with haemophilia A. A patient-level meta-analysis. Thromb. Haemost. 113 (5), 958–967. https://doi.org/10.1160/TH14-07-0621 (2015).
Wight, J. & Paisley, S. The epidemiology of inhibitors in haemophilia A: a systematic review. Haemophilia 9 (4), 418–435. https://doi.org/10.1046/j.1365-2516.2003.00780.x (2003).
Peyvandi, F., Mannucci, P. M., Garagiola, I. & ea tl. Randomized Trial of Factor VIII and neutralizing antibodies in Hemophilia A. N Engl. J. Med. 374 (21), 2054–2064. https://doi.org/10.1056/NEJMoa1516437 (2016).
Eshghi, P. et al. Haemophilia in the developing countries: the Iranian experience. Arch. Med. Sci. 6, 83–89. https://doi.org/10.5114/aoms.2010.13512 (2010).
Skinner, M. W. et al. Achieving the unimaginable: health equity in haemophilia. Haemophilia 26, 17–24. https://doi.org/10.1111/hae.13862 (2020).
Jones, P. & Robillard, L. The World Federation of Hemophilia: 40 years of improving haemophilia care worldwide. Haemophilia 9, 663–669. https://doi.org/10.1046/j.1351-8216.2003.00831.x (2003).
O’Mahony, B. & Black, C. Expanding hemophilia care in developing countries. Semin Thromb. Hemost. 31, 561–568. https://doi.org/10.1055/s-2005-922228 (2005).
Kavakli, K. et al. Prophylaxis vs. on-demand treatment with BAY 81-8973, a full-length plasma protein-free recombinant factor VIII product: results from a randomized trial (LEOPOLD II). J. Thromb. Haemostasis: JTH. 13 (3), 360–369. https://doi.org/10.1111/jth.12828 (2015).
Wu, Y. et al. Long-term joint outcomes of regular low-dose prophylaxis in Chinese children with severe haemophilia A. Haemophilia 27 (2), 237–244. https://doi.org/10.1111/hae.14256 (2021).
Stonebraker, J. S. et al. The World Federation of Hemophilia Annual Global Survey 1999–2018. Haemophilia 26 (4), 591–600. https://doi.org/10.1111/hae.14012 (2020).
Gringeri, A. et al. A randomized clinical trial of prophylaxis in children with hemophilia A (the ESPRIT Study). J. Thromb. Haemostasis: JTH. 9 (4). https://doi.org/10.1111/j.1538-7836.2011.04214.x (2011). 700 – 10.
Wilkins, R. A. et al. Twelve-month prevalence of haemarthrosis and joint disease using the Haemophilia Joint Health score: evaluation of the UK National Haemophilia database and haemtrack patient reported data: an observational study. BMJ Open. 12 (1). https://doi.org/10.1136/bmjopen-2021-052358 (2022).
Wilkins, R. A. et al. The impact of ankle haemarthropathy in patients with moderate haemophilia. Haemophilia 29 (2), 600–607. https://doi.org/10.1111/hae.14720 (2022).
Li, Y. et al. Comparison of joint status using ultrasound assessments and Haemophilia Joint Health score 2.1 in children with haemophilia. Front. Med. 10 https://doi.org/10.3389/fmed.2023.1193830 (2023).
O’Hara, S. et al. Disease burden and remaining unmet need in patients with haemophilia a treated with primary prophylaxis. Haemophilia 27 (1), 113–119. https://doi.org/10.1111/hae.14171 (2021).
O’Hara, J. et al. Evidence of a disability paradox in patient-reported outcomes in haemophilia. Haemophilia 27 (2), 245–252. https://doi.org/10.1111/hae.14278 (2021).
Albrecht, G. L. & Devlieger, P. J. The disability paradox: high quality of life against all odds. Soc. Sci. Med. 48 (8), 977–988. https://doi.org/10.1016/s0277-9536(98)00411-0 (1999).
O’Hara, J. et al. The cost of severe haemophilia in Europe: the CHESS study. Orphanet J. Rare Dis. 12 (1), 106. https://doi.org/10.1186/s13023-017-0660-y (2017).
Sun, J. et al. Factor VIII replacement prophylaxis in patients with hemophilia A transitioning to adults: a systematic literature review. Orphanet J. Rare Dis. 16 (1), 287. https://doi.org/10.1186/s13023-021-01919-w (2021).
Funding
This work was supported by Shandong Provincial Medical and Health Science and Technology Development Plan (202303041419, 202314011476).
Author information
Authors and Affiliations
Contributions
JW conducted the conception and design of the study; QL, YC, YHF, CCQ, TTW, HHW, XQZ participated in acquisition of data, analysis and interpretation of data; JW drafted the article and revised it critically for important intellectual content; final approval of the version to be submitted by QL.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, J., Cheng, Y., Fang, Y. et al. Retrospective analysis of clinical data from 171 low-income patients with hemophilia in Shandong Province. Sci Rep 15, 5867 (2025). https://doi.org/10.1038/s41598-025-90436-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-90436-y