Abstract
The war and siege in Tigray, Ethiopia, have devastated the region’s health system, critically impacting care for people living with HIV. This study aimed to assess the outcomes and factors affecting HIV patients during this crisis. An independent, repeated cross-sectional study was conducted at Ayder Comprehensive Specialized Hospital between October and November 2022. Data from prewar and during the war periods were analyzed using descriptive statistics and logistic regression. Among 440 participants (mean ages: 39 prewar and 41.2 during war), poor outcomes increased significantly during the war (28.6% prewar vs. 54.5% during war, p < 0.001). ART drug availability dropped by 68.8%, while only 10.6% and 30.7% accessed IPT and CPT, respectively. Services like CD4 and viral load determinations were severely disrupted (p < 0.001), with frequent ART switches and more missed appointments. Prewar factors associated with poor outcomes included severe malnutrition (AOR 3.98; 95% CI 1.04–15.22) and viral load > 1000 copies (AOR 6.68; 95% CI 2.91–15.32). During the crisis, significant factors included travel from distant areas (AOR 2.56; 95% CI 1.14–5.74), CD4 count > 200 cells/ml (AOR 0.27; 95% CI 0.08–0.97). The war and siege in Tigray significantly worsened HIV outcomes by disrupting care services and limiting access to essential treatments.
Similar content being viewed by others
Introduction
HIV/AIDS is a global public health problem with cases reported virtually from every corner of the world, with the majority being inhabitants of the sub-Saharan Africa region, accounting for 22.5 million patients1,2. As of 2021, there was a report of 612,925 and 50,703 people living with HIV in Ethiopia and Tigray, respectively. In Tigray, approximately 43,000 HIV patients were accessing ART drugs in the 141 ART clinic facilities1,3,4.
HIV patients’ lives have been improving over time due to the introduction of highly active antiretroviral treatment (HAART). However, man-made problems such as conflict have adversely affected the mortality and morbidity of HIV/AIDS patients. For example, the risk of HIV transmission increases during and after conflict due to complex social factors with armed conflicts due to increased gender-based violence, especially in the case of rape as a “weapon of war”, displacement leading to the disintegration of families and communities and so forth leading to increased vulnerability to HIV2,4,5. Conflict disrupts established epidemiological patterns, often driving the virus into rural areas that were previously less affected, thereby altering the dynamics of the epidemic6. Studies conducted in war-torn settings in Sub-Saharan Africa reveal alarming statistics, with viral non-suppression rates reaching up to 30% and loss to follow-up as high as 43.5%7.
In conflict-affected areas, access to prevention services and HAART is significantly limited because of health system disruption. However, the literature also shows that continuing ART in different conflict areas is feasible. One of the best experiences of access to ART medication in three severely war-affected areas was the experience of MSF on the effective provision of ART in Yemen and the Central Republic of Africa (CRA), where run-away bags containing 3–4 months of ART medications and health cards including helpline to call in case they faced drug shortages in sudden violent eruptions were applied. The other was a case study in Haiti in which the ART supply chain was not disrupted2,8,9.
The ongoing war in the Tigrai region of Ethiopia that started in early November 2020 displaced 2.5 million internally, and nearly 70,000 fled to Sudan. This was followed by the siege imposed by the Ethiopian government and its allies after the Tigrayan defense forces liberated most parts of Tigrai, including the capital city, Mekelle, at the end of June 2021. This has brought enormous damage to the health system, ranging from complete destruction, looting, and displacement of professionals, including health workers, to the de facto blockade of food, medicine, and fuel, as well as interruption of banking services, communication, and other essential services10,11. According to an MSF report, prior to the war, Tigray had one of the best health systems in Ethiopia, with relatively well-equipped and well-functioning hospitals as well as referral systems throughout the region. As a result of the war, Tigrai’s health system completely collapsed due to widespread looting, vandalization, and total destruction of health facilities by Eritrean and Ethiopian troops12,13. However, from a study conducted in Tigrai from November 2020 to June 2021 during the active war within the region, only 30% of hospitals, 17% of health centers, 11.5% of ambulances, and none of the 712 health posts were functional11. According to the UN and USAID reports, Tigray was deliberately blocked by the Ethiopian government and allies from accessing aid, including medications10,11. The media outlets describe many deaths related to chronic illness because of a lack of medication, including ART. This signposts there was a significant disruption of HIV care service delivery during the war and siege. As a result, there is a fear of increasing HIV transmission in the community, death due to opportunistic infections, and the risk of drug resistance.
In Tigrai, there was a single study that assessed HIV service provision in rural health facilities during the first 8 months of the war14; however, there is a scarcity of data on the impact of the continuing war and the complete siege applied by the federal government on individual patients as well as further damage to service provision. This study hypothesizes that the war and siege in Tigray significantly worsened HIV outcomes by reducing access to antiretroviral therapy (ART) and other critical HIV care services such as disruption of CD4 and viral load monitoring. It highlights the devastating health impacts of conflict and emphasizes the need for resilient strategies, such as mobile health units and emergency stockpiling, to maintain HIV care in crises and inform global healthcare responses in conflict-affected regions.
Methodology
Study area
This study was conducted in Ayder Comprehensive Specialized Hospital (ACSH) from October 20 to November 20, 2022. ACSH is located in Mekelle, the capital city of Tigray. Mekelle is located in northern Ethiopia, 783 km from the capital city of Addis Ababa. Tigray is surrounded by Eritrea to the north, the Amhara region to the south, Sudan to the west, and the Afar region to the east. The estimated area of the region is 50,079 km2 with a total population of 7,070,260 at a density of 140/km215. The ACSH serves more than nine million people from Tigray, the northern part of Amhara, Afar. Although the hospital has ART clinics, following the eruption of the war in November 2020, HIV tests and ART services were interrupted.
Study design and period
A cross-sectional study design was used to assess the effect of the war and siege on HIV/AIDS patients enrolled in the ART clinic of ACSH before (starting from November 2018 to October 2020) and during the war and siege of Tigray (November 2020 to October 2022). Data regarding ART and HIV/AIDS-related characteristics were collected from October 20 to November 20, 2022.
Data source
ART drug-related data were collected before the war and during the siege and war on the availability of drug options from ART pharmacies. Regarding individual patient status, the last measurement data were collected from the patient chart and registration before the eruption of the war and during the war and siege.
Source population
All patients enrolled in the ART clinic of ACSH.
Study population
All patients enrolled in the ACSH ART clinic who had follow-up data since 2018.
Study unit
ART patient enrolled in the ACSH ART clinic were selected by the sampling technique and fulfilled the inclusion criteria.
Eligibility criteria
The study aims to show the effect of the war and siege on HIV patients, so all HIV/AIDS patients were enrolled in the ART clinic of ACSH who had follow-up data since 2018 were included in this study, but patients with incomplete chart information and those who lost their charts were excluded.
Variables
Dependent variable
Poor patient outcome was a dependent variable in this study. It is defined if the study subject has treatment failure, drop out, lost to follow up, or death outcomes documented in the follow up chart.
Independent variables
Socio-demographic factors such as age, sex, address (from Mekelle city vs. out of Mekelle city), clinical characteristics like CD4 count which is classified in to < 200 cells/mm3 and ≥ 200 cells/mm3), viral load count that is classified in to < 1000 viral copies versus ≥ 1000 viral copies, frequent change of ART drugs due to shortage, drug discontinuation. Other clinical variable in this study was nutritional status based on Anthropometry. To assess Anthropometry for adults body mass index (BMI) defined by kilogram/meter2. The categorical variable of BMI was classified as follows: Normal weight–BMI [18.5–25], moderate malnutrition–BMI [16–18.4] and severe malnutrition–BMI ≤ 16. For children and pregnant mothers mid upper arm circumference (MUAC) was used to assess nutritional status. Availability of ART, laboratory and voluntary counselling services were also assessed.
Sample size and sampling technique
Based on the work of Johnston and his coworkers, sample size determination is required when planning chart reviews and other retrospective studies that aim to describe disease patterns16. HIV/AIDS-related reports since 2018 were used to assess the trend of the disease and its characteristics. The minimum sample size for the study was estimated using a single proportion formula with the assumptions of the proportion of people with HIV/AIDS who lost ART was 15.07%, 95% confidence interval, and a 5% margin of error17. The minimum sample size including a 10% non-response rate was 217, but 220 samples before and during the war and siege period were used to assess the outcome status of participants under ART. To attain the maximum representation of the samples and minimize selection bias, simple random sampling techniques using software sampling technique were applied to select patients from ART register by their unique ART registration number in both periods (before the war and during the war and siege). The selected patient registration number was checked for duplication and took data based on the prepared data abstraction tool as demonstrated in the flow diagram (Fig. 1).
Data collection tools and techniques
A structured data abstraction tool was prepared based on the availability of data from the registration and chart of the patients enrolled in the ART clinic, which is related to the topic. The tool has socio-demographic and clinical characteristics and risk factors associated with the outcome of the patients. Regarding data before and during the war and siege, the last measurements from their chart and registration of the patients were collected. Data were collected using ODK software from ART registration and patient charts selected by the sampling technique. Incomplete data were excluded from the study and replaced accordingly. To minimize the information bias, data collectors were professionals who have experience on ART registration and clinical description of HIV/AIDS.
Data quality control
A one-day intensive training was provided to the five data collectors on how to fill data to ODK software and on methods of sampling. The tool was pretested in 20 charts of patients under ART in Mekelle General Hospital. Each day-filled questionnaires were checked for completeness and feasibility. The collected data using ODK were cross-checked by principal investigators.
Data management and analysis
Data were cleaned and coded and then exported to SPSS 22 for analysis. Descriptive analysis was applied for categorical variables and mean and standard deviation (SD) for continuous variables. Chi-squared and p values were used to compare variables and reports before the war and during the war and siege. Binary logistic regression was performed to assess the relationship between outcome and independent variables. Variables with a p value of < 0.25 in the bivariate analysis were exported to multivariable analysis. In multivariable logistic regression, a p value < 0.05 with AOR (95% CI) was used to assess the level of statistical significance. Multicollinearity was assessed to check confounding variables. Model fitness was checked using the Hosmer and Lemishow test (0.786 and 0.268 for both pre-and during the war, respectively).
Operational definition
Stable outcome: if a patient enrolled in the ART clinic for ACSH has a good prognosis from the disease.
Poor outcome: is defined in this study if one or more of the following elements occurred in the study participants18; (1) Treatment failure is defined if the study participant developed stage 3 and/or stage-4 AIDS defining illness, or CD4 count < 200 cells/mm3, or if viral load > 1000 copies/ml despite ART. (2) Drop out, lost to follow up and missed appointments. (3) Death due to HIV related illness.
Result
Sociodemographic characteristics
In this study, a total of 440 participants were enrolled with a 100% response rate. More than 90% of the study subjects were 15 years and above. Nearly half of the study participants were women. Many of the them came from Mekelle (Table 1).
Clinical and service condition of participants
CD4 count and viral load determination had significant differences during the war compared with the prewar period (p < 0.001). There were frequent ART switches in the last 2 years during the crisis compared with the prewar period (p < 0.001). Similarly, most of the participants discontinued their ART regimens during the war and siege compared to the prewar period (p < 0.001) (Table 2).
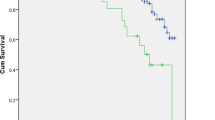
Outcome status of the participants
In this study, 63 (28.6%) and 120 (54.5%) of the participants in the prewar period and during the war and siege period had poor outcome status (p ≤ 0.001), respectively (Fig. 2).
Similarly, the trend of some outcome indicators like drop out, lost to follow-up and death increased amid the crisis period (Fig. 3).
Medication and laboratory service-related factors
Before the war, laboratory services such as CD4 count, viral load, and PCR (DBS) were consistently available for a year but dropped to less than 3 months during the conflict. HIV counseling and testing also declined sharply, from nearly 10,000 tests in 2018–2019 to 3780 in 2021 to none in 2022. Availability of ART medications was better before the war, with most drugs (85%) in stock year-round. During the war, over two-third of ART drugs, including second line treatment, were unavailable for over a year. First line drugs like TDF based regimens faced intermittent shortages lasting 3–9 months. The use of IPT and CPT by participants decreased significantly, attributed to drug unavailability. Most adults relied on 1E and 1J ART regimens, while children used 4C.
Associated risk factors for the poor outcome status of ART
This study identified various factors associated with poor out come before and during the war. Before the war, severe malnutrition was associated with increased poor out come by four-fold. While patients whose viral load was determined were 93% less likely to have poor outcomes. A viral load above 1000 copies raised the risk 6.7 times. During the war, patients from outside Mekelle faced a 2.56 times higher risk of poor outcomes compared to Mekelle residents. A CD4 count above 200 cells/mm³ reduced the risk by 73%. Frequent ART regimen changes reduced the risk of poor outcomes by 88%, and taking CPT lowered the risk by 57% (Table 3).
Discussion
In this study, the poor outcome status of participants had a significant difference whereby 63 (28.6%) had a poor outcome before the war compared to the 120 (54.5%) who had a poor outcome during the war and siege. Regarding medication and laboratory services, more than 85% of services in the prewar period were available, whereas over 68% of ART drugs and laboratory services were unavailable for a year during the crisis. Factors such as nutritional status, viral load copies, and their determination were associated with poor outcomes before the war, while address, CD4 count, use of CPT, and frequent ART change in the last 2 years were associated with poor outcomes.
This study showed that 54.5% of participants had poor outcome status during the war and siege, which is almost double compared to the prewar period, and it is also supported by the yearly report of the hospital19. This figure is significantly higher than outcomes reported in Kenya (post-election crisis), Sub-Saharan Africa (MSF studies), CAR, and Yemen8,20,21,22. Although all people living with HIV/AIDS, including those in conflict areas, are strongly recommended to start ART and continue their follow-up23, in contrary in the Tigray crisis there was a complete obstruction of access to medications to the region. A possible explanation for the high number of poor outcome statuses in this study could be firstly during the first round of war (November 2020 to June 2021), there was no security guarantee for safe transportation amid the active war, where several pieces of evidence have shown that civilians were targeted24,25; secondly starting from the end of June 2021, no ART and laboratory supplies were received due to the war and defacto blockade26; and the third reason was there was no coordinated effort of the Federal/Regional Ministry of Health and nongovernmental agencies to support the provision of drug regimens in the region. On the other hand, during the conflict and crisis in CAR and Yemen, and other sub-Saharan African countries, MSF provided ART medications using different modalities8,20, unlike in Tigray, where MSF and NRC were banned from providing humanitarian operations, which led to shortages in ART and laboratory supplies, leaving patients without essential services. During the siege period there was complete blockage of medical supplies, food, telecom services, power supply, transportation, banking, and other vital services imposed by the federal government27.
The war and siege significantly hampered ART and OI prophylactic medication supplies and laboratory services such as viral load, CD4 testing, and voluntary counseling and testing (VCT). For example, in Liberia, Cotidiviore and Haiti, while shortages existed, some ART supplies reached patients, highlighting the more severe systemic collapse in Tigray9,28,29). This was despite increasing global and local determinations aiming at improving access to antiretroviral treatment in sub-Saharan Africa and promoted that the lack of essential medicines in conflict settings, including ART, is a violation of human rights30,31. However, in Tigrai, during the 2-year-long crisis, there was a complete collapse of the health system, and many health facilities were either destroyed, looted, and/or minimally functioning11,12.
Unlike in Tigray, in other conflict-affected settings it is uncommon to see reports of significant disruption of ART provision. The MSF experience in Bukavu can be a lesson, where they reported sufficient medication supplies in the health facilities during the conflict, and those who were displaced to neighboring Rwanda were able to collect their ARVs in Rwanda31. In the case of Tigray crisis there was uncoordinated efforts between local governments and NGOs, unlike the collaborative approaches in settings like Bukavu.
Participants with severe under-nutrition before the war and siege were at four times higher risk of poor outcome status compared with their counterparts. This result is similar to the findings of a study performed in Metema Ethiopia and Tanzania, where low BMI was associated with a risk of death among ART users22,32. In addition, participants whose viral load was determined and viral load above 1000 copies had a poor outcome status. This was also supported by the study done in Metema Ethiopia32, where viral loads above 1000 copies have a higher risk of death. Poor viral suppression is very concerning particularly in conflict settings with collapsed health systems because it leads to a wider dissemination of the virus in the community and it hastens the progression of the disease in the HIV infected patients.
During the war and siege period, participants who traveled a long distance to access HIV care had a two times higher risk of having a poor outcome status. During that period, services such as transportation, telecommunication, banking, and most health facilities were closed. For these reasons, participants who were coming from outside of Mekelle had a greater risk of having poor outcome status. This result was supported by a qualitative study performed in Ethiopia, where lack of transportation was found to be among the barriers to ART follow-up33. Participants with a CD4 count above 200 cells/mm were 73% less likely to develop poor outcome status. This result is similar to a study performed in South Africa where participants with a high CD4 count were less likely to be lost to follow-up34. Despite the fact that maintaining CD4 monitoring is crucial in mitigating poor outcomes, due to the devastating supply chain disruptions in the region only 38.9% of patients received CD4 determination during the war period which was reduced by half compared to those during the prewar time.
Having frequent ART switches had a positive relationship with ART follow-up status. In this study, participants who switched ART regimens in the last 2 years were 88% less likely to have a poor outcome status than those who interrupted. In peacetime, ART regimen change is done due to the change in guidelines and the emergence of new and efficient drug combinations23,35, but during the crisis period, the frequent change was due to the unavailability of ART drugs, and patients were forced to switch to ART available in stocks. Even though frequent changing might carry the potential risk of HIV resistance, in crisis time, it is better to provide medications that are available in the facility than leave patients without any form of therapy. This might have an advantage to some extent in reducing the infectivity rate, for example in the case of mother-to-child transmission, however it has also negative consequences like risk of resistance, toxicity and possible drug interactions.
Individuals who have taken CPT during the war and siege period had a positive outcome status. This result is similar to the study conducted in the Sheka zone and northwestern Ethiopia, where patients not on CPT were at higher risk of death and loss from follow-up36,37. This is because taking CPT has a positive impact on their functional and health status, but during the war and siege, there was a CPT shortage, and most of the participants were not taken.
Deliberate blockage of essential HIV medications in conflict settings like Tigray represents a violation of human rights, as highlighted by global health initiatives. Additionally, it contrasts to the SDG target 3.3 of ending HIV epidemic by 2030, as well as to the WHO goals of 95% of all people living with HIV should have a diagnosis, 95% of whom should be taking life saving antiretroviral treatment, and 95% of people living with HIV on treatment should achieve a suppressed viral load by 2025. So in conflict settings with complete system collapse, like in the case of Tigray, it requires a new approach to maintain medical supply and international pressure to secure uninterrupted ART supplies.
Strengths and limitations of the study
The study showed the impact of war and siege on the outcome and service disruption in the study area. The other limitation of this study is that it did not look in detail into treatment failure, as there was an erratic CD4 determination and a complete absence of viral load determination during the data collection time. In this study to be consistent the last BMI documented in the study participants’ medical record was taken, so as weight can fluctuate with time we believe that it affected the study findings. Due to the lack of communication, the number of deaths might be overlooked because an increasing number of dropouts and lost follow-ups were seen on whom the deceased ones might be. Due to the cross-sectional nature of the study design were like recall bias, measurement bias, and the absence of temporal association between outcome and explanatory variables which makes it difficult to establish causality.
Conclusion and recommendation
In this study, almost double the participants had poor outcome status during war and siege than in the prewar period. The majority of the participants were lost to follow-up, and there were also dropouts. HIV service provision was significantly disrupted; 68% of ART drugs were unavailable for a year. In addition, there were erratic CD4 and viral load determinations due to the lack of supplies for 16 months in the hospital. Before the war, factors such as malnutrition, high viral load copies, and erratic viral load determination were associated with poor outcomes, while long distance travel, low CD4 count, and patients not on CPT during the war and siege were independent risk factors for poor outcomes. The war has adversely affected the lives of HIV patients. To ensure continuity of essential medical services in conflict zone, it is important to strengthen international aid coordination and alternative supply chain, including cross boarder supply options which mitigated disruptions in CAR, Yemen and Bukavu. Proactive measures like stockpile ART and other medical supplies in high risk regions can maintain availability during the siege or transport disruptions. Advocate for international recognition that denial of essential HIV care during conflicts violates human rights, increasing accountability for governments and international actors. By applying these recommendations, findings from this study can inform policies and interventions in other conflict-affected regions, ultimately improving health outcomes for individuals living with HIV/AIDS.
Data availability
The dataset of this study is available from the corresponding author upon request. The data can not be shared publically to protect study participants privacy.
Abbreviations
- ACSH:
-
Ayder Comprehensive Specialized Hospital
- ART:
-
Antiretroviral treatment
- CPT:
-
Cotrimoxazole preventive therapy
- IPT:
-
INH preventive therapy
- DBS:
-
Dried blood test
- 1J:
-
Tenofovir, lamivudine and daltgravir
- 1E:
-
Tenofovir, lamivudine, and efavirenz
- 4C:
-
Tenofovir, Lamivudine and Lopinavir boosted with ritonavir
References
UNAIDS. Preliminary UNAIDS 2021 Epidemiological Estimates, Global HIV Statistics (2022). Available from: https://www.unaids.org/en/resources/fact-sheet.
Samuels, F., Harvey, P. & Bergmann, T. HIV and AIDS in Emergency Situations. Synthesis Report (Overseas Development Institute, London, 2008). Available from: http://cdn-odi-production.s3.amazonaws.com/media/documents/4277.pdf.
EPHI. HIV Related Estimates and Projectionsin Ethiopia for the Year 2021–2022 (EPHI, Addis Ababa, 2022). Available from: https://ephi.gov.et/wp-content/uploads/2022/09/9-HIV_Estimates_and_projection_for_the_year_2021_and_2022.pdf.
Tigray External Affair Office. Tigray Health Sector Annual Bulletin 2021 (Tigray Regional Health Bureau, Mekelle, 2021). Available from: https://tigrayeao.info/wp-content/uploads/2022/02/final-annual-bulletincompressed.pdf.
Friedman, J. & Veleny, E. V. Responding to HIV in Afghanistan (2008). Available from: https://www.aidsdatahub.org/sites/default/files/resource/responding-hiv-afghanistan.pdf.
Daw, M., El-Bouzedi, A. & Ahmed, M. The impact of armed conflict on the prevalence and transmission dynamics of HIV infection in Libya. Front. Public Health 10, 779778 (2022).
Kebede, H. K. et al. The impact of armed conflicts on HIV treatment outcomes in sub-Saharan Africa: A systematic review and meta-analysis. Confl. Health 8, 40 (2024).
Ferreyra, C., O’Brien, D., Alonso, B., Al-Zomour, A. & Ford, N. Provision and continuation of antiretroviral therapy during acute conflict: The experience of MSF in Central African Republic and Yemen. Confl. Health 12(30), 1–7 (2018).
Honoré, J. G., Balan, J. G., Thimothé, G., Diallo, J. & Barnhart, S. Instability adversely affects HIV care in Haiti. Lancet 388, 1877–1878 (2016).
USAID. Ethiopia-Tigray Crisis (2021). Available from: https://www.usaid.gov/sites/default/files/2022-05/2021_09_30_USG_Tigray_Fact_Sheet_11.pdf.
Gesesew, H. et al. The impact of war on the health system of the Tigray region in Ethiopia: An assessment. BMJ Glob. Health 6(11), 1–9 (2021).
OMNATigray. Medical Crisis in Tigray 2020–2021 (2021). Available from: https://omnatigray.org/wp-content/uploads/2021/04/Medical-Crisis-in-Tigray-.pdf.
MSF. People Left with Few Healthcare Options in Tigray as Facilities Looted, Destroyed (2021). Available from: https://www.msf.org/health-facilities-targeted-tigray-region-ethiopia.
Weledegebriel, M. G. et al. The impact of war on HIV/AIDS service provision: In rural health facilities of Tigray, Northern Ethiopia, a cross-sectional study. PLoS ONE. 18(5), 1–10 (2023).
Population Projection of Ethiopia for All Regions at Wereda Level from 2014–2017. Federal Democratic Republic of Ethiopia Central Statistical Agency. Retrieved 4 June 2018.
Johnston, K., Lakzadeh, P., Donato, B. & Szabo, S. M. Methods of sample size calculation in descriptive retrospective burden of illness studies. BMC Med. Res. Methodol. 19(9), 1–7 (2019).
Leshargie, C. T., Demant, D., Burrowes, S. & Frawley, J. The proportion of loss to follow-up from antiretroviral therapy (ART) and its association with age among adolescents living with HIV in sub-Saharan Africa: A systematic review and meta-analysis. PLoS ONE 17(8), e0272906. https://doi.org/10.1371/journal.pone.0272906 (2022).
FMOH. Ethiopian National Guideline for Comprehensive HIV Prevention, Care, and Treatment (Federal Ministry of Health, 2017).
ACSH. Annual Report 2021–2022 (Ayder Comprehensive Specialized Hospital, Mekelle, 2022).
O’Brien, D. P. et al. Provision of antiretroviral treatment in conflict settings: The experience of Médecins Sans Frontières. Confl. Health 4(12), 1–9 (2010).
Mann, M. et al. Antiretroviral treatment interruptions induced by the Kenyan postelection crisis are associated with virological failure. J. Acquir. Immune Defic. Syndr. 64(2), 220–224 (2013).
Gunda, D. W., Nkandala, I., Kilonzo, S. B., Kilangi, B. B. & Mpondo, B. C. Prevalence and risk factors of mortality among adult HIV patients initiating ART in rural setting of HIV care and treatment services in North Western Tanzania: A retrospective cohort study. BMC Res. Notes 10(197), 1–6 (2017).
WHO. Guidelines for Managing Advanced HIV Disease and Rapid Initiation of Antiretroviral Therapy (WHO Team, Geneva, 2017). Available from: https://www.who.int/publications/i/item/9789241550062.
UN. Tigray Conflict is a Health Crisis for 6 Million People, and ‘The World is Not Paying Attention’: Tedros (2022). Available from: https://news.un.org/en/story/2022/10/1129697.
UNOCHA. Tigray Aid Situation Worsening by the Day, Warn UN Humanitarians (2021). Available from: https://news.un.org/en/story/2021/09/1099022.
WHO. Crisis in Northern Ethiopia (2022). Available from: https://www.who.int/emergencies/situations/crisis-in-tigray-ethiopia.
Kruk, M. E. et al. Availability of essential health services in post-conflict Liberia. Research 88, 527–534 (2010).
Betsi, N. A. et al. Effect of an armed conflict on human resources and health systems in Côte d’Ivoire: Prevention of and care for people with HIV/AIDS. AIDS Care 18(4), 356–365 (2006).
UNAIDS, UNCHR. Handbook on HIV and Human Rights for National Human Rights Institutions (Geneva, Switzerland, 2007). Available from: https://www.ohchr.org/sites/default/files/Documents/Publications/HandbookHIVNHRIs.pdf.
Weiser, S. D. et al. The association between food insecurity and mortality among HIV-infected individuals on HAART. J. Acquir. Immune Defic. Syndr. 52(3), 342–349 (2009).
Culbert, H. et al. HIV treatment in a confl ict setting: Outcomes and experiences from Bukavu, Democratic Republic of the Congo. PLoS Med. 4(5), 794–799 (2007).
Workie, K. L., Birhan, T. Y. & Angaw, D. A. Predictors of mortality rate among adult HIV-positive patients on antiretroviral therapy in Metema Hospital, Northwest Ethiopia: A retrospective follow-up study. AIDS Res. Ther. 18(27), 1–11 (2021).
Biadgilign, S., Deribew, A., Amberbir, A. & Deribe, K. Barriers and facilitators to antiretroviral medication adherence among HIV-infected paediatric patients in Ethiopia: A qualitative study. J. Soc. Asp. HIV/AIDS 6(4), 148–154 (2009).
Arnesen, R., Moll, A. P. & Shenoi, S. V. Predictors of loss to follow-up among patients on ART at a rural hospital in KwaZulu-Natal, South Africa. PLoS ONE 12(5), 1–12 (2017).
FMoH. National Consolidated Guidelines for Comprehensive HIV Prevention, Care and Treatment (Addis Ababa, 2018). Available from: https://www.afro.who.int/sites/default/files/2019-04/National%20Comprehensive%20HIV%20Care%20%20Guideline%202018.pdf.
Assemie, M. A., Leshargie, C. T. & Petrucka, P. Outcomes and factors affecting mortality and successful tracing among patients lost to follow-up from antiretroviral therapy in Pawi Hospital, Northwest Ethiopia. Trop. Med. Health 47(52), 1–7 (2019).
Shaweno, T. & Shaweno, D. When are patients lost to follow-up in pre-antiretroviral therapy care? A retrospective assessment of patients in an Ethiopian rural hospital. Infect. Dis. Poverty 4(27), 1–8 (2015).
Acknowledgements
We would like to thank our study participants for their willingness, our data collectors, and the hospital staff.
Author information
Authors and Affiliations
Contributions
MGW contributed to the conception and design. ATN and TG performed the data analysis and result writing. MGW, ATN, TG, HH, TG, NT, BT, EK, and AG contributed to the research design and data collection of the study. MGW, ATN, and TG underwrote the discussion section. MGW, ATN, SK, RT, BT, TG, and BY contributed to the interpretation and revision of the draft manuscript. ATN and TG prepared the figures and tables. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethical Clearance was obtained from the Institutional Review Board of College of Health Science, Mekelle University with a reference number of 2018/2022. All data were fully anonymized before we accessed them and the Institutional Review Board of College of Health Science waived the requirement for informed consent. Confidentiality was maintained at all levels of the study and all the information obtained was used for this study only. We confirm that all the methods were carried out in accordance with relevant Institutional guidelines and regulations.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Weledegebriel, M.G., Nigusse, A.T., Gebru, T. et al. Outcome of HIV patients on ART during the war and siege in a tertiary hospital in Northern Ethiopia: a cross-sectional study. Sci Rep 15, 6434 (2025). https://doi.org/10.1038/s41598-025-90848-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-90848-w