Abstract
Low bone mineral density (BMD) impairs the stability of the bone-screw interface, which leads to screw loosening after spinal instrumentation. Quantitative computed tomography (QCT) and dual-energy X-ray absorptiometry (DXA) were applied to measure BMD of screw trajectories and other regions of the vertebrae in this paper, and the aim was to analyze the best effective tool and BMD of the best appropriate vertebral site to predict pedicle screw loosening after lumbar fusion surgery. 186 patients who underwent lumbar interbody fusion and pedicle screws placement were analyzed retrospectively. Patients were divided into 2 groups according to whether there was screw loosening: fissure is greater than or equal to 1 mm around the screws at follow-up CT scans. The volumetric BMD (vBMD) was measured by QCT in the central vertebral body, pedicle, and screw trajectory region, and DXA was applied for the lumbar spine and hip area BMD (aBMD). The overall pedicle screw loosening rate was 33.9% (63/186). Demographic data, health history, and the lumbar aBMD were not significantly different between the two groups. Multivariate analysis revealed showed that the hip aBMD, vBMD in the central vertebral body, pedicle, and screw trajectory regions were independent risk factors for screw loosening. Additionally, Receiver operating characteristic curve revealed the screw trajectory vBMD had the greatest area under the curve for predicting screw loosening. The screw trajectory vBMD using QCT had a stronger predictive value than the vBMD in other regions of the vertebrae and the hip aBMD, and had a more representative bone quality measurement in the bone-screw binding region.
Similar content being viewed by others
Introduction
Pedicle screws are currently the conventional fixation method for the surgical treatment of lumbar diseases, which can be effectively applied in three-column spinal fixation to reconstruct lumbar stability and promote segmental fusion1. Pedicle screw loosening is one of the most common complications and can lead to persistent back pain, fusion failure, and pseudoarthrosis formation2. The strong association between low bone mineral density (BMD) and screw loosening was well established. Because bone screw integration is significantly reduced in osteoporotic patients, the postoperative screw loosening rate can reach 62.8%3. With the aging of the global population, the increasing number of patients with lumbar degenerative diseases are comorbid with osteoporosis4. Osteoporosis has been reported in 39.7% of lumbar fusion surgery patients aged over 50 years5. The patient’s BMD, therefore, provides important information for selecting the appropriate surgical option and predicting clinical outcomes. Dual-energy X-ray absorptiometry (DXA) is the most commonly applied bone quality assessment method at present. Lumbar DXA leads to higher BMD measurements than the actual data, due to the inability to distinguish the interference of dense calcifications such as degenerated vertebral hyperplasia bone, abdominal vascular calcifications, and facet joint hyperplasia, which could result in screw loosening, especially in the elderly patients6.
Quantitative computed tomography (QCT) accurately reflects specific bone density in different regions by three-dimensional measurement. This approach can avoid the interference of pathological bone formation on the results, particularly for patients with degenerative lumbar changes, thus QCT is a more reliable method to assess spinal BMD7. In addition, QCT-based finite element models of the spine allow biomechanical studies and have been shown to estimate bone strength more than DXA-based BMD. However, to our knowledge, there were few studies have been performed to predict screw loosening by QCT. The International Society for Clinical Densitometry recommended that QCT was routinely represented by density information in the central region of the cancellous bone of the vertebral body8. Because there are regional differences in BMD within the vertebrae, BMD measurements at specific sites may mask differences in the different regions9. Regional bone quality analysis showed that the BMD in the area around the screws inside the vertebral body and the pedicle region had a greater impact on screw stability than vertebral body BMD9. On the basis of the above studies, the aim of our study is to analyze whether the volumetric BMD (vBMD) of pedicle screw trajectories could predict screw loosening more accurately than other regions of the vertebrae or other ways for BMD measurement.
Methods
Patients
The study was conducted according to the Declaration of Helsinki (revised 2013) and was approved by the Ethics Committee of Honghui Hospital Affiliated with Xi’an Jiaotong University (202005125). We reviewed patients with lumbar degenerative diseases who underwent posterior lumbar interbody fusion (PLIF) with pedicle screw fixation in our hospital from July 2019 to August 2021. All patients had undergone single level interbody lumbar fusion with polyether ether ketone cage packed with autogenous bone. The same type of titanium screws and rods were used in all cases, with varying but clinically relevant screw sizes. All patients provided informed consent for surgery.
Inclusion criteria: (1) QCT for vertebrae and DXA for lumbar spine and hip were performed within 1 month before surgery; (2) patients aged over 50 years at the time of surgery were treated within L3-S1; and (3) patients were followed up for a minimum of 12 months. Exclusion criteria: (1) Incorrect screw path for the first placement; (2) history of lumbar internal fixation surgery; and (3) patients with secondary osteoporosis caused by primary or metastatic spinal tumor, lumbar tuberculosis, ankylosing spondylitis, drugs, or other metabolic diseases. All patients’ surgeries were planned and performed by the same spine surgical team. Demographic data (sex, age, body mass index (BMI)), and health status (diabetes, hypertension, smoking habits) were obtained from the hospital information system for further analysis.
Bone quality evaluation
DXA examination using Hologic Discovery model A densitometers (Hologic, Inc., Bedford, MA, USA) was conducted prior to surgery to determine the areal BMD (aBMD) of the lumbar spine (L1 to L4 vertebrae) and total hip using standard procedures before surgery. The BMD values were recorded in the form of T scores and recorded as T1 and T2 respectively (Fig. 1).
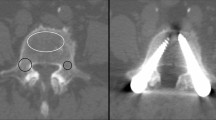
For QCT, L5 vertebrae were selected for the vBMD measurement in every patient. QCT image sequences were acquired using a computational tomography (CT) scanner (Siemens SOMATOM Definition Flash, Siemens Healthcare, Forchheim, Germany) with a QCT system (QCT Pro v5.0, Mindways Software, Inc., Austin, TX, USA) and calibrated in advance using a quality control phantom. A standard QCT-corrected phantom was placed under the waist during the CT procedure. The scan data was imported to the QCT workstation for analysis processing, and oval regions of interest (ROIs) were automatically generated in the cancellous bone region in the center of the L5 vertebra body (Fig. 2A). The ROIs of the screws through the pedicle region were manually drawn by rotating the axial and sagittal views (Fig. 2B). The ROIs of the pedicle screw trajectory was delineated as regions adapted to screw insertion locations, including the vertebral body, pedicle, and articular processes (Fig. 2C). Manual correction was performed to avoid cortical bone and areas of osteosclerosis. In this study, we defined the conventional QCT measurement area (vertebral body), pedicle area, and screw trajectory area as area A, area B, and area C, respectively.
To test measurement reliability, 10 patients from each group were randomly selected, and the QCT values of these 20 patients were independently performed at the Honghui Hospital by 2 surgeons (L.D. and C.X).
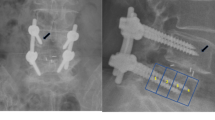
Screw loosening assessment
The presence of screw loosening was confirmed by CT during the 1-year postoperative follow-up period, and screw loosening was defined as the observed width of radiolucent areas is ≥ 1 mm around the pedicle screw (Fig. 3). Patients were assigned to the loosening or non-loosening group according to whether screw loosening had occurred. 63 patients were included in the loosening group and 123 patients in the non-loosening group.
Statistical analysis
SPSS statistical software, version 20.0 (IBM Corporation, Armonk, NY) was used for all statistical analyses. The Shapiro-Wilk test was applied to verify the normal distribution of continuous variables. The intraclass correlation coefficient (ICC) was calculated to identify the repeatability of measured continuous variables (ICC ≥ 0.8 represents excellent reliability). Normally distributed measurement data were presented as mean ± standard deviation and analyzed using the t-test. The Mann–Whitney U test was used for those not following normal distribution (A-vBMD, B-vBMD). Quantitative data were analyzed by the chi-square test or Fisher’s exact test. Logistic regression analysis was performed for variables reaching a significance level of P < 0.1. Receiver operating characteristic (ROC) curves were used to assess the value of predicting loosening, and the area under the curve (AUC) was calculated. The Youden index was applied to establish the optimal threshold. P < 0.05 was considered to be statistically significant.
Results
A total of 186 patients (89 males and 97 females) with a mean age of 64.60 ± 9.06 years were included in the final analysis. The screw loosening rate within one year after lumbar interbody fusion was 33.9%. There were no significant differences between the two groups in age, gender, BMI, smoking, or the presence of diabetes or hypertension (P > 0.05) (Table 1). In the preoperative aBMD comparison, the loosening group displayed significantly smaller T2 (hip aBMD) values than the control group (P < 0.05), whereas T1 (lumbar aBMD) values showed no statistically significant difference (P > 0.05) (Table 1).
Two surgeons showed high agreement in measuring the A-vBMD (vertebral body), B-vBMD (pedicle area), and C-vBMD (screw trajectory area), with ICCs of 0.914, 0.887, and 0.901, respectively. The vBMD values in the non-loosening group were significantly higher than those in the screw loosening group, regardless of whether the vBMD was measured for the above-mentioned three regions (P < 0.05) (Table 1).
According to the results of univariate analysis, the T2 and vBMD values measured in the three regions with statistical differences were included in the logistic regression analysis. Considering the excellent consistency between the vBMD measured in these regions, regression analysis of the different vBMD values was performed separately. The results showed that T2 and the vBMD measured in the three regions A, B, and C were independent risk factors contributing to screw loosening (Table 2).
ROC curve analysis was performed to separately evaluate the predictive value of T2 and the vBMD in different regions for screw loosening. The AUC was 0.596 (95% CI, 0.509 to 0.684, P = 0.032) for T2, 0.682 (95% CI, 0.603 to 0.762, P < 0.001) for A-vBMD, 0.714 (95% CI, 0.636 to 0.791, P < 0.001) for B-vBMD, and 0.736 (95% CI, 0.659 to 0.812, P < 0.001) for C-vBMD (Table 3). The AUC value of the C-vBMD was the highest, which indicated vBMD of screw trajectory area measured by the QCT is a better predictive parameters for screw loosening (Fig. 4). The optimal threshold value of the vBMD of the screw trajectory constructed using the Youden index was 119.5 for predicting pedicle screw loosening.
Discussion
Loosening of screws has always been one of the key factors affecting internal fixation stability12. The loss of bone screw integration will cause poor initial stability after surgery, resulting in cage displacement, subsidence, and nonunion, which will adversely affect the prognosis of patients and increase the rate of revision surgery13. Patients with osteoporosis were more likely to have postoperative screw loosening than patients with normal bone mass. A meta-analysis by Rometsch et al.14 suggested that screw loosening is twice as frequent in osteoporotic patients as in normal-bone subjects.
DXA is the gold standard for patients diagnosed with osteoporosis. However, the working principle of DXA leads to certain deviations in the assessment of bone quality in degenerative spinal diseases. Zou et al.5reported that about one-quarter of patients with a non-osteoporotic lumbar T-score had osteoporosis diagnosed by CT scan, suggesting that the diagnosis by lumbar DXA is likely to be a false negative in patients with spinal degeneration. Our study showed that there was no significant difference in lumbar spine T values between the loosening and non-loosening groups, which was consistent with previous findings15,16,17. This suggested that lumbar spine T scores could not be used as a predictor of risk of pedicle screw fixation failure. Nevertheless, the measurement of hip DXA is not affected by lumbar degeneration, it had become a routine addition for BMD measurement of DXA. We found that the loosening group had significantly lower hip T scores than the control group. However, because the hip BMD can only indirectly reflect the lumbar spine BMD, there are still some deviations in estimating the bone mass at the lumbar surgical site.
In recent years, many studies have applied CT to determine the Hounsfield Unit (HU) value to evaluate lumbar bone quality. Zou et al.17showed that the HU values of the vertebral body in the screw loosening group were significantly lower than those without loosening, and concluded that the HU value could predict pedicle screw loosening. Recent studies101115;; showed that the HU measured in the plane of the pedicle screw trajectory more accurately predicted screw loosening than the vertebral body HU. This is because the use of the HU to assess vertebral bone quality can only be based on two-dimensional planar measurements and cannot be analyzed from a three-dimensional perspective, and HU measurements for a single plane may mask differences between different regions. In addition, the HU value itself does not fully represent BMD. Currently, QCT can readily convert the HU to the three-dimensional vBMD and accurately reflect local bone quality. Kulkarni et al.18 recommended that QCT should replace DXA as the gold standard for assessing spinal osteoporosis. QCT is routinely applied to measure BMD in the central region of the cancellous bone of the vertebral body, considering that there are different regional differences in BMD and strength of the vertebrae. The aim of our study was, therefore, to apply QCT to predict screw loosening after lumbar fusion and to compare the predictive performance of different QCT measurement regions for pedicle screw loosening. The results showed that the screw trajectory vBMD was a better predictor than other regions.
In a cadaveric biomechanical study, Wichmann et al.19found that the BMD in the pedicle screw zone correlated better with the axial screw pullout strength than BMD values for the screw trajectory. It should be noted, however, that the axial pullout of pedicle screws from vertebral bodies in cadaveric specimens does not realistically mimic the stress of pedicle screws inside the human body. By integrating the load cell into the internal spinal fixation, it was found that the main load on the screw in vivo is along the craniocaudal direction rather than the axial direction20. Song et al.1 further showed by finite element models that the axial pulling force is not a risk factor for screw loosening in osteoporotic patients in pedicle screw fixation, and screws are more likely to loosen due to loading in the craniocaudal direction. Our study also found that the screw trajectory vBMD values displayed a better predictive performance for screw loosening than the pedicle zone vBMD in patients after lumbar fusion.
The incidence of screw loosening after lumbar fusion in the present study was 33.9%. This was higher than that reported in previous studies evaluating screw loosening based on X-ray images (7–30%)21,22,23. CT scans were applied in the present study to determine whether screws were loose. CT has been shown to have higher sensitivity and specificity than X-ray and is the best indicator of screw loosening after spinal fusion24. In addition, a relatively high proportion of our included patients received fixation of ≥ 3 levels, and the length of fixation was also shown to be a risk factor for screw loosening by Li et al.2.
Preoperative assessment of bone quality is important for surgical planning and evaluation of screw failure. However, the current preoperative bone quality examination of patients is not ideal. Although the majority of patients scheduled for surgery are older, according to Allen et al.25, only 44% of physicians will perform BMD testing for patients before performing spinal instrumentation surgery. For patients undergoing lumbar spine surgery, CT examination is often one of the necessary steps for preoperative evaluation. Assessment of bone quality by QCT allows efficient and convenient utilization of existing CT scans to assess bone quality without increasing radiation exposure or financial burden26. To reduce radiation exposure, a single scan ranging from three vertebral levels was used in our hospital. We chose to focus on the L5 vertebra given that the area at the highest risk of degenerative changes and displaying the most severe conditions thereof in lumbar structures is the L4–S1 level.
This study has several limitations. First, this was a single-center retrospective study and did not include patients with severe osteoporosis treated intraoperatively with expansion screws or bone cement screws, which may have caused some selection bias. Multicenter and prospective studies are needed to verify these results. Second, no data were collected on the clinical symptoms of the patients and the impact of screw loosening on their daily activities could not be assessed. Third, the follow-up time was relatively short, and a longer follow-up time may help to assess the impact of screw loosening on interbody fusion.
Conclusions
This study suggested that the vBMD measured by QCT was a good predictor of the risk of screw loosening after lumbar degenerative surgery. In addition, the prediction ability of the screw trajectory vBMD was better than those of the vBMD in other regions of the vertebrae and the aBMD in the hip. In conclusion, results of our study revealed that the screw trajectory vBMD measured by QCT was a more accurate parameter to assess the BMD of the bone-screw binding region and predict pedicle screw loosening.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Song, F. et al. Craniocaudal toggling increases the risk of screw loosening in osteoporotic vertebrae. Comput. Meth Programs Biomed. 238, 107625 (2023).
Li, W. et al. Vertebral bone quality score as a predictor of pedicle screw loosening following surgery for degenerative lumbar disease. Spine 48 (23), 1635–1641 (2023).
El Saman, A. et al. Reduced loosening rate and loss of correction following posterior stabilization with or without Pmma augmentation of pedicle screws in vertebral fractures in the elderly. Eur. J. Trauma. Emerg. Surg. 39, 455–460 (2013).
Wang, L. et al. Prevalence of osteoporosis and fracture in China: the China osteoporosis prevalence study. Jama Netw. Open. 4, e2121106 (2021).
Zou, D. et al. Prevalence of osteoporosis in patients undergoing lumbar fusion for lumbar degenerative diseases: A combination of Dxa and Hounsfield units. Spine 45, E406–E410 (2020).
Cheng, X. et al. Opportunistic screening using Low-Dose Ct and the prevalence of osteoporosis in China: A nationwide, multicenter study. J. Bone Min. Res. 36, 427–435 (2021).
Adams, J. E. Quantitative computed tomography. Eur. J. Radiol. 71, 415–424 (2009).
Shepherd, J. A., Schousboe, J. T., Broy, S. B., Engelke, K. & Leslie, W. D. Executive Summary of the 2015 Iscd Position Development Conference On Advanced Measures From Dxa and Qct: Fracture Prediction Beyond Bmd. J. Clin. Densitom. 18, 274–286 (2015).
Li, D. et al. A study of screw placement to obtain the optimal Pull-Out resistance of lumbar pedicle screws-Analysis of Hounsfield units measurements based on computed tomography. Bmc Musculoskelet. Disord. 23, 124 (2022).
Ishikawa, K. et al. A novel method for the prediction of the pedicle screw stability: regional bone mineral density around the screw. Clin. Spine Surg. 31, E473–E480 (2018).
Xu, F. et al. Hounsfield units of the vertebral body and pedicle as predictors of pedicle screw loosening after degenerative lumbar spine surgery. Neurosurg. Focus. 49, E10 (2020).
Löffler, M. T. et al. Opportunistic osteoporosis screening reveals low bone density in patients with screw loosening after lumbar Semi-Rigid instrumentation: A Case-Control study. Front. Endocrinol. 11, 552719 (2020).
Weiser, L. et al. Insufficient stability of pedicle screws in osteoporotic vertebrae: Biomechanical correlation of bone mineral density and pedicle screw fixation strength. E Eur. Spine J. 26, 2891–2897 (2017).
Rometsch, E. et al. Screw-Related complications after instrumentation of the osteoporotic spine: A systematic literature review with Meta-Analysis. Glob Spine J. 10, 69–88 (2020).
Sakai, Y. et al. Hounsfield unit of screw trajectory as a predictor of pedicle screw loosening after single level lumbar interbody fusion. J. Orthop. Sci. 23, 734–738 (2018).
Zhao, X. et al. Optimizing lumbar pedicle screw trajectory utilizing a 3D-Printed Drill guide to ensure placement of pedicle screws into higher density bone May improve pedicle screw pullout resistance. World Neurosurg. 158, e459–e464 (2022).
Zou, D., Sun, Z., Zhou, S., Zhong, W. & Li, W. Hounsfield units value is a better predictor of pedicle screw loosening than the T-Score of Dxa in patients with lumbar degenerative diseases. Eur. Spine J. 29, 1105–1111 (2020).
Kulkarni, A. G. et al. Should Q-Ct be the gold standard for detecting spinal osteoporosis?? Spine 47, E258–E264 (2022).
Wichmann, J. L. et al. Quantitative Dual-Energy Ct for Phantomless evaluation of cancellous bone mineral density of the vertebral pedicle: correlation with pedicle screw Pull-Out strength. Eur. Radiol. 25, 1714–1720 (2015).
Graichen, F., Bergmann, G. & Rohlmann, A. Patient monitoring system for load measurement with spinal fixation devices. Med. Eng. Phys. 18, 167–174 (1996).
Chen, Z. et al. Prediction of pedicle screw loosening using an Mri-Based vertebral bone quality score in patients with lumbar degenerative disease. World Neurosurg. 171, e760–e767 (2023).
Ohtori, S. et al. Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine. 38(8), E487–E492 (2013).
Shu, L., Muheremu, A., Ji, Y., Zhang, R. & Liu, W. Prediction of Lumbar Pedicle Screw Loosening Using Hounsfield Units in Computed Tomography. Curr Med Imaging. 20, 1–6 (2023).
Spirig, J. M., Sutter, R., Götschi, T., Farshad-Amacker, N. A. & Farshad, M. Value of standard radiographs, computed tomography, and magnetic resonance imaging of the lumbar spine in detection of intraoperatively confirmed pedicle screw Loosening-a prospective clinical trial. Spine J. 19 (3), 461–468 (2019).
Allen, R. T., Lee, Y. & Garfin, S. R. Spine Surgeons Survey On Attitudes Regarding Osteoporosis and Osteomalacia Screening and Treatment for Fractures, Fusion Surgery, and Pseudoarthrosis., :602–604. (2009).
Yang, X. et al. Quantitative assessment of zonal trabecular volumetric bone mineral density in Middle-Aged and elderly women using quantitative computed tomography. Quant. Imaging Med. Surg. 13, 2278–2286 (2023).
Author information
Authors and Affiliations
Contributions
Conceptualization, C.X. and L.D.; methodology, JC.J. and YT.Z.; formal analysis, C.X., JC.J. and YT.Z.; data curation, C.X., JC.J. and XQ.H.; writing—original draft preparation, C.X., JC.J. and YT.Z.; writing—review and editing, L.D. and XQ.H.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Institutional review board statement
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Review Committee of Honghui Hospital Affiliated with Xi’an Jiaotong University. (No: 202005125).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, C., Ji, J., Zhang, Y. et al. Correlation analysis of BMD in different regions of the vertebrae determined by QCT and DXA on pedicle screw loosening. Sci Rep 15, 11850 (2025). https://doi.org/10.1038/s41598-025-91816-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-91816-0