Abstract
The increasing use of antiviral drugs, combined with an aging population, has resulted in a growing number of older adults living with HIV. Unfortunately, high-risk sexual behavior among older individuals with HIV has led to HIV retransmission. Our study aimed to analyze the sexual behavior of elderly men with HIV in Chongqing and evaluate the factors influencing high-risk sexual behavior using a logistic regression model. The study involved 774 participants with an average age of 62 years. Of the participants, 45.74% (N = 354) reported having sex in the past year, and 13.70% (N = 106) reported high-risk sexual behavior in the same period. Our study identified several factors associated with high-risk sexual behavior, such as low education level, commercial and temporary sexual partners, and lack of awareness and use of condoms. The results highlight the significant prevalence of high-risk sexual behavior among HIV-infected older men in Chongqing, and the potential risk of secondary transmission. Therefore, targeted interventions and education programs are needed, particularly for men over 50 years old, those with low education level, and those who engage in commercial or temporary sexual partnerships. Specifically, promoting condom use and increasing awareness of HIV/AIDS knowledge should be prioritized to decrease the prevalence of high-risk sexual behavior and prevent further transmission of the virus.
Similar content being viewed by others
Introduction
Acquired Immune-deficiency Syndrome (AIDS) is a syndrome caused by infection with the human immunodeficiency virus (HIV) that primarily manifests as immune compromise1. China, as the world’s most populous developing country, has been challenged with high rates of HIV/AIDS since the outbreak. By the end of 2020, over one million people were living with HIV infection in China, with heterosexual transmission being the primary route, accounting for 74.2% of cases in 20202. The increasing use of antiviral drugs, coupled with an aging population, has resulted in a rising number of older adults living with HIV3. China now faces the new challenge of an excessive HIV/AIDS prevalence in the middle-aged and elderly population (aged ≥ 50 years).
In contrast to women, men remain sexually active beyond the age of 504. In a study in the United States which included a nationally representative sample of older adults (n = 3005, age range: 57–85), 95.19% of older male respondents reported having had sex in the last year, and 42.38% engaged in sexual activity more than twice per month5. However, older men exhibit a less comprehensive grasp of HIV in comparison to their younger counterparts. This limited understanding of HIV may contribute to elevated levels of high-risk sexual behavior6. Such behavior, which includes nonmarital sexual activity, engagement with multiple sexual partners, and a lack of condom use, has the potential to lead to secondary transmission of HIV and an increase in HIV prevalence among older age groups7,8. As the body ages, the organ functions of the elderly continue to decline, and immune capacity diminishes9. Older adults with HIV have more rapid disease progression and higher mortality than younger patients10. Therefore, the sexual behavior of older people living with HIV, particularly their high-risk sexual behavior and its influencing factors, cannot be ignored.
Chongqing, located in the southwest of China and bordering Sichuan province, is the largest municipality directly under the Central Government in China and the economic and political center of the southwestern region11. Chongqing has a large immigrant population and has become one of the most severe cities in China affected by the HIV/AIDS epidemic. Case reports indicate that since 1995, the epidemic has spread to a broader age range, and the proportion of newly diagnosed older HIV/AIDS cases has been increasing annually12. Between 1988 and 2003, the average proportion of patients diagnosed with HIV aged 50 years and older rose sharply from 3.6 to 45.4%, and the proportion of older male cases increased from 2.4% in 2002 to 51.8% in 201713,14. In a recent study of heterosexual cases of HIV/AIDS infection reported in Chongqing, commercial sex infections predominated in HIV/AIDS patients 50 years of age and older (53.30%)15. High rates of HIV infection have been reported among older male clients in Chongqing, with most of them having lower rates of condom use during sexual intercourse with female sex workers (FSWs)12.
While several studies have investigated the sexual behavior of the general elderly population, few have focused on older adults with HIV in Chongqing. This study aims to understand the sexual behavior and factors influencing sexual behaviours of HIV-infected men aged 50 years and older in Chongqing, providing a scientific basis for the formulation of targeted prevention and control measures aimed at reducing the risk of HIV/AIDS retransmission.
Methods
This study aimed to investigate the sexual behavior and influencing factors of HIV-infected men aged 50 years and older in Chongqing. In this section, we describe the study participants, survey methods, and key variables used in the study.
Study participants
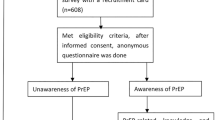
The eligibility criteria for study participants were as follows: (1) aged 50 years or older; (2) male; (3) HIV/AIDS patients; (4) receiving or received ART antiviral treatment; (5) no history of epilepsy or severe mental illness; (6) able to answer questions independently.
Study survey
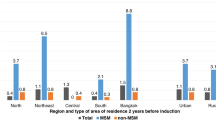
Convenient sampling was used to select four districts in Chongqing where the middle-aged and elderly AIDS epidemic was more severe (people living with HIV > 2000 cases): two districts in urban areas (Yubei and Shapingba District), one in suburban area (Kaizhou District), and one in rural-urban fringe area (Jiangjin District). A total of 800 individuals were recruited, with 200 individuals from each district.
Research is typically carried out at the local hospital’s infection clinic in June-Dec 2021, where patients who are regularly taking medication or undergoing routine testing are recruited. If a potential survey participant meets the research criteria, physicians will provide a comprehensive explanation of the survey’s purpose and significance and invite the patient to participate. All investigators involved in the study are well-trained healthcare professionals, including outpatient physicians experienced in providing voluntary HIV counseling and testing services.
Upon obtaining consent from the participants, investigators will conduct face-to-face interviews using a structured questionnaire that included demographic information, sexual behavior, and information on antiviral treatment. During these interviews, the questions are read aloud to the participants, and their responses are recorded. Subsequently, the investigators review the answers for completeness and logical consistency. As a token of appreciation, respondents who complete the questionnaire receive small gifts such as laundry detergent, paper towels.
Key variables
Demographic characteristics: Participants self-reported their age, ethnicity, place of residence, education, occupation, and monthly income.
AIDS knowledge: AIDS knowledge was assessed using eight relevant questions in the “China AIDS Prevention and Treatment Supervision and Evaluation Framework (Trial)” issued by the Office of the State Council AIDS Prevention and Control Committee in 2007. Individuals who correctly answered six or more questions were deemed to have sufficient HIV/AIDS knowledge, while those who answered less than six questions were considered to have insufficient HIV/AIDS-related knowledge16. The questionnaire has been widely used in previous studies and has demonstrated good reliability and validity in assessing HIV/AIDS knowledge among Chinese populations (Cronbach-α = 0.846).
Sexual behavior: Participants self-reported their sexual orientation, sexual frequency in the last year, and whether they used aphrodisiacs in the last year. Additionally, participants reported the frequency of condom use during sexual behavior with fixed, commercial, or temporary partners in the last year and the latest sexual behavior, with answer options including “never”, “sometimes used”, and “used every time”.
Infection and treatment data: Medical staff investigated file data, including the latest CD4 test value at the time of investigation, the duration of antiviral therapy, and the test value of the latest viral load.
Fixed sexual partners: Fixed sexual partners were defined as a spouse or common-law partner with a relationship duration of at least three months.
Commercial sexual partners: Commercial sexual partners were defined as a relationship partner whose purpose is to exchange money or material equivalents.
Temporary sexual partners: Temporary sexual partners were defined as non-commercial, non-fixed sexual partners.
High-risk sexual behavior: High-risk sexual behavior was defined as failing to consistently use condoms during each sexual behavior.
Ethical considerations
The research protocol has received ethics approval from the Ethics Committee of the Chongqing Center for Disease Control and Prevention. Participation in the study was voluntary, and all participants signed informed consent prior to their involvement. This research was performed in accordance with the Declaration of Helsinki and the local regulations.
Statistical analysis
All statistical analyses were performed using SPSS version 23.0 (IBM, Armonk, New York). Categorical variables were described using composition ratios to provide a clear and concise summary of the distribution of demographic and behavioral characteristics among the study participants. Univariate analysis was used for comparisons between groups, and the factors meaningful in univariate analysis were included in the binary logistic regression model. The latest high-risk sexual behavior and high-risk sexual behavior in the last year were used as the dependent variables (1 = Yes, 0 = No), and the relevant influencing factors were screened. Statistical significance is defined as P < 0.05. All statistical analyses were conducted using IBM SPSS Statistics version 23.0 (IBM Corp., Armonk, NY, USA). Categorical variables were presented as proportions. Univariate analysis was performed to compare groups, and factors that showed statistical significance in univariate analysis were included in the binary logistic regression model. High-risk sexual behavior in the last year and latest high-risk sexual behavior were considered as dependent variables (1 = Yes, 0 = No), and relevant influencing factors were identified. Statistical significance was set at P < 0.05.
Results
A total of 774 HIV-infected men participated in the study, with a high response rate of 96.75%. The average age of participants was 62 years (range: 50–92 years). Most respondents lived in urban areas (60.21%) and were married (67.31%). The education level was concentrated in primary school/illiteracy (52.33%), and the majority of participants were unemployed at the time of the survey (73.13%), with a monthly income of less than 3,000 yuan (75.06%). The overall rate of AIDS knowledge was 65.63%. Only 2.97% of participants reported using an aphrodisiac in the last year. The majority had a CD4 level above 200/mm3 (76.49%), a viral load of less than 50 copies/ml (77.26%), and had been on antiviral treatment for more than 3 years (63.44%) (see Table 1).
Among the 774 men with HIV who participated in the study, 45.74% (354/774) reported engaging in sexual behavior during the last year. Out of the 354 respondents who had sexual behavior, 318 reported having a regular partner. Among them, 82.08% (261/318) reported using a condom during their latest sexual encounter, while 72.33% (230/318) reported consistent condom use during the last year. However, 15.09% (48/318) of respondents reported never using a condom.
In terms of commercial sexual behavior, 11.30% (40/354) of the respondents reported engaging in it during the last year. Out of these 40 respondents, 82.50% (33/40) reported having more than one sexual partner. The proportion of condom use during the latest sexual encounter was 52.50% (21/40), while 47.50% (19/40) reported consistent condom use during the last year. However, 40.00% (16/40) of the people who had commercial sex never used a condom.
Temporary sexual behavior was reported by 9.32% (33/354) of the respondents, with 60.61% (20/33) of them having more than one sexual partner. Among them, 87.88% (29/33) reported using a condom during their latest sexual encounter, while 63.64% (21/33) reported consistent condom use during the last year. 15.15% (5/33) reported never using a condom. (Table 2)
9.82% (76/774) of the respondents reported engaging in high-risk sexual behavior during their latest sexual activity. Univariate analysis revealed that several factors were significantly associated with high-risk sexual behavior, including education level, marital status, monthly income, aphrodisiac use, commercial sexual partners, temporary sexual partners, and duration of ART treatment. Subsequently, multivariate analysis incorporating these significant factors showed that individuals who engaged in commercial sexual behavior were more likely to report high-risk sexual behavior (OR = 11.844, 95% CI: 5.245–26.744) compared to those without commercial sexual partners. Additionally, individuals who had been undergoing ART treatment for 1–2 years were less likely to engage in high-risk sexual behavior (OR = 0.189, 95% CI: 0.082–0.434) (Table 3).
It was found that 106 out of 774 respondents (13.70%) reported engaging in high-risk sexual behavior in the last year. Univariate analysis showed that several characteristics were significantly associated with high-risk sexual behavior, including age, education level, marital status, aphrodisiac use, commercial sexual behavior, temporary sexual behavior, CD levels, viral load, and duration of treatment. To determine which factors were independently associated with high-risk sexual behavior, the researchers conducted a multivariate analysis that included all significant factors from the univariate analysis. The results showed that respondents who were 60–69 years old (OR = 2.515, 95%CI: 1.268–4.988), had used aphrodisiacs or assistive drugs (OR = 3.016, 95% CI: 1.070–8.501), engaged in commercial sexual behavior (OR = 6.674, 95% CI: 2.969 to 15.001), or had temporary sexual behavior (OR = 3.058, 95% CI: 1.196–7.817) had a higher likelihood of engaging in high-risk sexual behavior in the last year. Conversely, respondents with a junior high school/high school education level (OR = 0.507, 95% CI: 0.306–0.842), those with a duration of treatment of 1–2 years (OR = 0.268, 95%CI: 0.101–0.712) or ≥ 3 years (OR = 0.376, 95%CI: 0.143, 0.989) were less likely to engage in high-risk sexual behavior in the last year (Table 4).
Discussion
Our findings revealed a high percentage of sexually active HIV-infected males in Chongqing, with 45.74% reporting sexual intercourse in the past year, which was higher than the percentage reported in Guangxi, China (28.8%)17. Furthermore, the proportion of high-risk sexual behavior among older men with HIV in Chongqing was high (13.70%), which could lead to the risk of secondary transmission. Our study identified several factors associated with high-risk sexual behavior, such as low education level, commercial and temporary sexual partners, and lack of awareness and use of condoms.
Our study identified condom use as a critical indicator of high-risk sexual behavior, both in the last instance and in the past year. Notably, our study found low rates of condom use, which was lower than that reported in Thailand (90.60%)18 and higher than those reported in the United States (39.60%)19. Many older men with erectile dysfunction are reluctant to use condoms as they perceive it may interfere with sexual pleasure, thereby increasing the risk of HIV transmission8. Moreover, Individuals who engaged in commercial sexual behavior were also more likely to engage in high-risk sexual behavior. 20.62% of HIV-infected older men engaged in both commercial and temporary sexual behaviors in the past year, which was higher than the prevalence of non-marital sexual activity among the elderly in Chongqing in 2017 (18.87%)20. Compared to the rate of condom use with fixed sexual partners (72.33%) among older men with HIV in Chongqing, the rate of condom use with commercial sexual partners (47.50%) and temporary sexual partners (63.64%) was lower in the past year. Engaging in commercial sex among people living with HIV may result from a lack of a sexual partner or reluctance to transmit the virus to a spouse or regular partner due to HIV infection21. Furthermore, sex workers are at a higher risk of sexually transmitted HIV and have a lower rate of condom use22. Therefore, it is crucial to intensify efforts to combat commercial sex and continue to promote the consistent use of condoms.
Another important finding of our study is the association between prolonged ART and reduced high-risk sexual behavior. In general, Long-term antiviral therapy may make patients more aware of the importance of adhering to treatment and the potential harms of spreading HIV, which can help prevent high-risk sexual behavior. However, individuals on ART for 1–2 years were less likely to engage in high-risk sexual behavior than those on ART for ≥ 3 years, which may be due to a decline in patient adherence, changes in mentality, and the development of a “fearless” and “indifferent” attitude towards HIV23,24. This underscores the importance of implementing interventions to maintain long-term adherence to antiretroviral treatment, as well as continuing to promote and educate the public on the risks of HIV transmission, in order to effectively prevent HIV spread among older adults.
Our study revealed that educational attainment was significantly associated with high-risk sexual behavior in the overall study population, with individuals with less than junior high school education being more likely to engage in high-risk sexual behavior in the past year, consistent with previous research25,26. Meanwhile, our study found that older HIV-infected men in Chongqing generally have a lower level of education and a lower awareness rate of AIDS knowledge, which may contribute to their engagement in high-risk sexual behavior. Specifically, we found that the awareness rate of AIDS knowledge among this population was only 65.63%, which is lower than the national target of 85% set by the “13th Five-Year Plan for Curbing and Preventing HIV/AIDS” in China. A previous study found that respondents with sufficient knowledge about AIDS were more likely to use condoms during sexual activity25. It is possible that people with higher levels of education may have better access to information about HIV testing and treatment, and are therefore more likely to adhere to treatment and avoid engaging in high-risk sexual behaviors that could negatively impact their health. This finding highlights the need for targeted education and awareness campaigns that focus on HIV/AIDS prevention and safe sex practices for older adults.
Based on our research findings, younger individuals with HIV infection were found to be more likely to engage in high-risk sexual behavior in the past year compared to those aged over 70 years, which is consistent with commonly held beliefs27. This may be due to the fact that older adults often experience one or more chronic illnesses as they age, and the medications used to treat these conditions can reduce sexual performance and result in a decreased frequency of sexual activity28.
The study also highlights the importance of addressing the use of aphrodisiacs among older adults. The use of aphrodisiacs was found to increase the risk of high-risk sexual behavior, which is consistent with the findings of Noroozi29. Aphrodisiacs have been shown to increase sexual pleasure and the number of commercial sexual acts in older adults30. This suggests that interventions aimed at reducing the use of aphrodisiacs may be effective in reducing HIV transmission among older adults.
Our study found that the majority of participants were unemployed (73.13%), which is consistent with the demographic profile of older adults, many of whom are retired or unable to re-enter the workforce. While this finding was not statistically significant in the univariate analysis, it highlights the need for alternative interventions that address the social and psychological needs of older adults. Social isolation and lack of meaningful activities have been linked to risky behaviors, including unsafe sexual practices, among older adults31. Therefore, community-based programs that promote social interaction, mental health, and healthy aging could be effective in reducing HIV transmission in this population. For example, organizing recreational activities, peer support groups, and educational workshops on healthy relationships and safe sex practices may help older adults build stronger social networks and reduce their engagement in high-risk behaviors32. Additionally, healthcare providers should consider integrating sexual health education into routine care for older adults, addressing misconceptions about HIV transmission and promoting the consistent use of condoms, especially among those who remain sexually active33.
In addition to targeting men over 50 years old, education and awareness campaigns should also be extended to their younger counterparts, including female sex workers (FSWs) and other sexual partners. Younger partners may play a crucial role in HIV transmission dynamics, and their awareness of HIV prevention strategies can significantly reduce the risk of secondary transmission34. Therefore, comprehensive interventions should address both older men and their sexual networks to effectively curb the spread of HIV.
However, our study has some limitations that need to be addressed. First, the generalizability of the results may be limited by the nature of the research topic. As this study only focuses on HIV-infected men aged 50 and above in Chongqing, the findings may not be applicable to other populations or settings. Secondly, the study uses a convenience sampling method, which may affect the representativeness of the sample. Participants recruited through this method may not be representative of the entire population of HIV-infected men aged 50 and above in Chongqing. Therefore, caution should be exercised when generalizing the findings to the wider population. Additionally, recall and responder bias may have affected the accuracy with which participants reported past sexual behaviors and health-related practices.
Conclusion
The findings of this study highlight the significant prevalence of high-risk sexual behavior among HIV-infected older men in Chongqing, and the potential risk of secondary transmission. Our results suggest that targeted interventions and education programs are needed, particularly for men over 50 years old, those with low education level, and those who engage in commercial or temporary sexual partnerships. Specifically, efforts to promote condom use and increase awareness of HIV/AIDS knowledge should be prioritized to decrease the prevalence of high-risk sexual behavior and prevent further transmission of the virus.
Data availability
The corresponding author can provide all of the datasets used in this study upon reasonable request.
References
Fauci, A. S. The acquired immune deficiency syndrome: the ever-broadening clinical spectrum. Jama 316(2), 230 (2016).
He, N. Research progress in the epidemiology of HIV/AIDS in China. China CDC Wkly. 3 (48), 1022–1030 (2021).
Lima, V. D. et al. AIDS incidence and AIDS-related mortality in British Columbia, Canada, between 1981 and 2013: a retrospective study. Lancet HIV 2(3), e92–97 (2015).
Srinivasan, S. et al. Sexuality and the older adult. Curr. Psychiatry Rep. 21(10), 97 (2019).
Lindau, S. T. et al. A study of sexuality and health among older adults in the united States. N Engl. J. Med. 357(8), 762–774 (2007).
Zhang, T. et al. Awareness of HIV/AIDS and its routes of transmission as well as access to health knowledge among rural residents in Western China: a cross-sectional study. BMC Public. Health 19(1), 1630 (2019).
Li, N. et al. A qualitative study on high risk behaviors and related factors of reported HIV/AIDS cases aged 60 years and above in some areas of Henan province. Zhonghua Liu Xing Bing Xue Za Zhi. 38(9), 1161–1164 (2017).
Odimegwu, C. O. & Mutanda, N. Covariates of high-risk sexual behaviour of men aged 50 years and above in sub-Saharan Africa. Sahara J. 14(1), 162–170 (2017).
Guaraldi, G., Milic, J. & Mussini, C. Aging with HIV. Curr. HIV/AIDS Rep. 16(6), 475–481 (2019).
Leng, S. X. & Margolick, J. B. Aging, sex, inflammation, frailty, and CMV and HIV infections. Cell. Immunol. 348, 104024 (2020).
Yang, S. et al. HIV epidemics in Shenzhen and Chongqing, China. PLoS One. 13(2), e0192849 (2018).
Wang, Y. et al. Changing trends of HIV, syphilis, and hepatitis C among male migrant workers in Chongqing, China: nine consecutive Cross-Sectional surveys, 2010–2018. Int. J. Environ. Res. Public. Health 17, 3 (2020).
Wu, G. et al. Higher risks of virologic failure and All-Cause deaths among older people living with HIV in Chongqing, China. AIDS Res. Hum. Retroviruses. 35(11–12), 1095–1102 (2019).
Zhou, Y. et al. Independent risk factors for deaths due to AIDS in Chongqing, China: does age matter?. Front. Med. (Lausanne) 7, 586390 (2020).
Wu, J. et al. Characteristics of newly reported HIV/AIDS cases with heterosexual mode of transmission in six districts of Chongqing city. Zhonghua Liu Xing Bing Xue Za Zhi 41(6), 919–923 (2020).
Zhuang, X. et al. HIV-related high-risk behaviors among Chinese migrant construction laborers in Nantong. Jiangsu PLoS One 7(3), e31986 (2012).
Zhao, Q. et al. Age differences in sexual risk behaviors and related factors among people living with HIV in Guangxi, China. AIDS Care 30(4), 523–530 (2018).
Srithanaviboonchai, K. et al. Sexual behavior and attitudes toward sex of older adults living with HIV. AIDS Behav. 24(6), 1825–1834 (2020).
Starks, T. J., Millar, B. M. & Parsons, J. T. Predictors of condom use with main and casual partners among HIV-positive men over 50. Health Psychol. 34(11), 1116–1122 (2015).
Jiang, G. J. et al. Survey on extramarital sexual behaviors and HIV infection in middle-aged and elderly people aged 50 and above in selected areas of Chongqing. Zhonghua Liu Xing Bing Xue Za Zhi 39(11), 1438–1442 (2018).
Wu, P. et al. HIV-positive clients of female sex workers in Hunan Province, China: a mixed methods study assessing sexual relationships and risk behavior by type of partner. BMC Public. Health 19(1), 1129 (2019).
Zhang, Q. et al. HIV prevalence and factors influencing the uptake of voluntary HIV counseling and testing among older clients of female sex workers in Liuzhou and Fuyang Cities, China, 2016-2017: a cross-sectional study. Biomed. Res. Int. 2020, 9634328 (2020).
Vu, T. M. T. et al. Sexual risk behaviors of patients with HIV/AIDS over the course of antiretroviral treatment in Northern Vietnam. Int. J. Environ. Res. Public. Health 15, 6 (2018).
Okoboi, S. et al. Risky sexual behavior among patients on long-term antiretroviral therapy: a prospective cohort study in urban and rural Uganda. AIDS Res. Ther. 15(1), 15 (2018).
Du, X. et al. Factors associated with risk sexual behaviours of HIV/STDs infection among university students in Henan, China: a cross-sectional study. Reprod. Health. 18(1), 172 (2021).
Chen, X. et al. Epidemiological profile and molecular genetic characterization of HIV-1 among female sex workers and elderly male clients in Guangxi, China. Emerg. Microbes Infect. 10(1), 384–395 (2021).
Houle, B. et al. Sexual behavior and HIV risk across the life course in rural South Africa: trends and comparisons. AIDS Care 30(11), 1435–1443 (2018).
Merghati-Khoei, E. et al. Sexuality and elderly with chronic diseases: a review of the existing literature. J. Res. Med. Sci. 21, 136 (2016).
Noroozi, M. et al. Methamphetamine use and HIV risk behavior among men who inject drugs: causal inference using coarsened exact matching. Harm Reduct. J. 17(1), 66 (2020).
Lu, H. et al. Sildenafil use and relevant risk factors among middle-aged or elderly male clients of female commercial sex workers in the central areas of Guangxi, China. Zhonghua Liu Xing Bing Xue Za Zhi 35(11), 1218–1222 (2014).
Yang, Y. et al. Lifetime commercial heterosexual behavior among HIV negative elderly men from rural Chengdu, China: a modified knowledge-attitude-practice perspective. BMC Public. Health. 21(1), 2095 (2021).
Merchant, R. A. et al. Community-Based Peer-Led intervention for healthy ageing and evaluation of the ‘HAPPY’ program. J. Nutr. Health Aging. 25(4), 520–527 (2021).
Wang, B. et al. Loneliness and its correlates among older adults living with HIV: a multicenter cross-sectional study. J. Affect. Disord. 341, 228–235 (2023).
Stone, J. et al. Estimating the contribution of key populations towards HIV transmission in South Africa. J. Int. AIDS Soc. 24(1), e25650 (2021).
Acknowledgements
We would like to thank the staff of the local CDC in Yubei District, Kaizhou District, Jiangjin District, and Shapingba District for their assistance in recruiting participants and providing support during the study.
Funding
This study was funded by Chongqing medical scientific research project (2023MSXM113), Chongqing Natural Science Foundation Project (cstc2021jcyj-msxmX1171), and the first batch of key disciplines on public health in Chongqing (YWBF2022072).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Chongyang Bai, Long Li, Chao Zhou. The first draft of the manuscript was written by Tianyu Tan and Shan Li. Wei Zhang provided critical review of the manuscript. Guohui Wu provided the funding. All authors commented on the previous versions and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by The Ethics Committee of the Chongqing Center for Disease Control and Prevention (Project No: KY-2022-022-2).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tan, T., Li, S., Bai, C. et al. Prevalence and risk factors of high-risk sexual behavior among elderly men with HIV infection in Chongqing, China. Sci Rep 15, 8053 (2025). https://doi.org/10.1038/s41598-025-92661-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-92661-x