Abstract
Platelet-derived microparticles (PDMPs) participate in ischemic brain injury. We further determined the relationships between serum PDMPs levels and early neurological deterioration (END) as well as functional outcome after acute cerebral infarction (ACI). In this prospective cohort study, serum PDMPs levels were measured in 125 controls and 621 patients with ACI. Univariate analysis and multivariate analysis were sequentially applied to investigate the relations of serum PDMPs levels to END and poor prognosis (modified Rankin scale score > 2) at six months after ACI. Serum PDMPs levels were significantly higher in patients than in controls (median, 14.00 ng/L vs. 27.00 ng/L; P < 0.001). Serum PDMPs levels were strongly correlated with infarction volume (ρ = 0.532, P < 0.001), National Institutes of Health Stroke Scale score (ρ = 0.627, P < 0.001) and modified Rankin scale score (ρ = 0.528, P < 0.001). It was independently associated with END [odds ratio (OR) 1.117, 95% confidence interval (CI) 1.008–1.238; P = 0.001] and poor prognosis (OR 1.092, 95% CI 1.066–1.119; P = 0.001). There were linear relationships between serum PDMPs levels and risks of poor prognosis (P for non-linear = 0.055) plus END (P for non-linear = 0.061) under restricted cubic spline. Using subgroup analysis, significant interaction existed between serum PDMPs levels and age in association of poor prognosis (P for interaction = 0.006), as well as between serum PDMPs levels and coronary heart disease in association of END (P for interaction = 0.017). Serum PDMPs levels significantly discriminated the development of poor prognosis (Area under curve 0.705, 95% CI 0.632–0.778; P < 0.001) and END (The area 0.733, 95% CI 0.664–0.803; P < 0.001). Serum PDMPs levels may predict the risk of END and 6-month poor prognosis in patients with ACI.
Similar content being viewed by others
Introduction
Acute cerebral infarction (ACI) accounts for approximately 75% of cerebrovascular diseases, causing serious social problems and heavy economic burden1,2. Early neurological deterioration (END), a common adverse event after ACI, is very frequently associated with risk of poor prognosis in such patients3,4. Recently, there has been a growing interest in discriminating new biological markers for ACI to aid in predicting prognosis, assessing disease severity and exploring pathophysiological process5,6.Platelet-derived microparticles (PDMPs) are small particles that are shed from the plasma membrane and enter the peripheral circulation after platelet activation7. PDMPs play important roles in many physiological and pathological processes, such as deep vein thrombosis, stroke, and acute myocardial infarction8,9,10. Reportedly, anti-platelet therapy can prevent END and improve 6-month outcome in patients with acute stroke, indicating that END could be related to platelet activation11. Compelling data have shown that PDMPs may boast critical effects in ACI. Chiva-Blanch et al.12 found that the concentration of PDMPs was significantly increased in the ischemic stroke patients compared to the controls. Schrick et al.13 reported that some platelet derived microparticles may monitor the response to anti-platelet therapy and predict the next vascular event in stroke patients. Chiva-Blanch et al. found that the concentration of PDMPs was significantly increased in the ischemic stroke patients compared to the controls. Thus, it is hypothesized that PDMPs may be potential prognostic predictors of END and neurological outcome following ACI. Here, serum PDMPs levels were quantified in a cohort of patients with ACI, in order to reveal the relationship between serum PDMPs levels, END and neurological outcome of ACI.
Methods
Study design, patient and control enrollments, and ethical approval
In this prospective observational cohort study, we consecutively enrolled patients with ACI, who were admitted at the Wenzhou Central Hospital (Wenzhou, China) from January 2018 to January 2022. Inclusion criteria were as follows: (1) age of 18 years or greater; (2) hospital admission within 12 h after onset of stroke symptom; (3) the clinical diagnoses were confirmed by computerized tomography (CT) or Magnetic Resonance Imaging (MRI) according to the Chinese Stroke Association 2023 guidelines14. Exclusion criteria were in the following: (1) previous thrombolysis or endovascular therapy; (2) coexistence with other neurological diseases, such as severe traumatic brain injury, intracranial tumors and infections; (3) severe diseases in other organs, such as liver, heart, lung and kidney failure, ascites and cirrhosis; (4) refusal to participation, unqualified samples, incomplete clinical data or loss to follow-up. A group of healthy individuals were recruited as controls. This study complied with the Declaration of Helsinki and its later amends15 and its protocol was approved by the Ethics Committee at the Wenzhou Central Hospital (No. L2024-03-020). All patients’ proxies or controls themselves submitted written informed consent to participate in this study.
Data collections, END definition and outcome assessment
Some relevant data were collected, including demographic variables, medication use, medical history, cigarette smoking and alcohol drinking. The severity of the neurological deficit was assessed at admission by use of the National Institutes of Health Stroke Scale (NIHSS) score16. END was defined as poststroke 24-hour NIHSS total score increasing by ≥ 4 or the NIHSS individual score increasing by ≥ 2 compared with baseline17. According to the definition, we divided the patients into END and non-END groups. In addition, we assessed the functional outcome based on the modified Rankin score (mRS) at 6 months after onset of stroke. Patients with an mRS > 2 were considered to have a poor outcome, and ≤ 2 predicted a favorable outcome. The patients were classified into different groups by at least two experienced senior neurologists.
Laboratory examination
Peripheral venous blood samples from all patients were at admission taken and controls’ samples at entry into study. All blood samples were drawn into vacutainers containing ethylenediaminetetra acetic acid and acid citrate dextrose using 21-gauge needles to minimize platelet activation. The samples were gently mixed and then kept at room temperature for the maximum period of 1 h. Immediately after centrifugation at 8000 g for 5 min, 200 µL was collected from the upper-layer supernatant of the samples to avoid contamination by platelets. The collected samples were stored at − 80℃ until analysis. PDMPs levels were determined in a blinded fashion using the PDMPs ELISA kit (Otsuka Pharmaceutical Co., Ltd., Tokyo, Japan) according to the manufacturer’s instructions18. The coefficients of variation is below 10%. The kit used two monoclonal antibodies against glycoproteins CD42a and CD42b to measure PDMPs levels. Each sample was measured twice, and mean values were recorded.
In addition, other laboratory indicators, such as triglycerides, total cholesterol, high-density-lipoprotein cholesterol (HDL-c), low-density-lipoprotein cholesterol (LDL-c), glucose, platelet count, activated partial thromboplastin time (APTT), thrombin time (TT) and fibrinogen levels, were measured and recorded at the same time.
Statistical analysis
Data analyses were performed using Statistical Package for Social Sciences Version 23.0. (IBM Corp., Armonk, NY, USA) and R software (version 4.3.2; R Foundation for Statistical Computing). We plotted the figures via GraphPad Prism version 8.0 (GraphPad Software Inc., La Jolla, CA, USA). The Kolmogorov-Smirnov test was utilized for estimating the compatibility of normally distributed data. For continuous data, homogeneous data were expressed as the mean ± standard deviation, while non-homogeneous data were presented as median and 25th–75th percentiles.All normally-distributed data were compared using the independent-sample Student’s t-test. Data shown to be non-normally distributed were analyzed using the Mann-Whitney U test. Logistic regression analysis was used to determine the relationships between serum PDMPs levels and END as well as poor outcome at 6 months in patients with ACI. In the model, we entered the variables with a p-value of < 0.05 on the univariate analyses, and the odds ratio (OR) value and 95% confidence interval (CI) were calculated. Furthermore, we conducted subgroup analyses to assess whether the potential covariables (age, gender, hypertension, diabetes mellitus, coronary heart disease, dyslipidemia, smoker, alcohol, anti-platelet therapy and thrombolysis) modified the relationships between serum PDMPs levels and END as well as poor outcome at 6 months. The interactions between serum PDMPs levels and END as well as poor outcome at 6 months were tested using the likelihood ratio test of models with interaction terms. Additionally, we applied restricted cubic spline regression models to explore the shapes of the associations between serum PDMPs levels and END as well as poor outcome at 6 months in patients with ACI. The receiver operating characteristic (ROC) curve was constructed to investigate the predictive value of serum PDMPs levels for END and 6-month poor outcomes in ACI patients, and area under curve (AUC) and 95% CI values were calculated. The difference of P < 0.05 was defined as statistical significance.
Results
Participant characteristics
Initially, 762 patients with ACI were assessed. According to exclusion criteria, 141 patients were excluded because of the reasons outlined in Fig. 1. Finally, a total of 621 patients were under assessment. Additionally, 125 healthy individuals were recruited as controls. In Table 1, there were no significant differences between the patients and the healthy controls in age (P = 0.167), sex percentage (P = 0.266), BMI(P = 0.103), smoking (P = 0.469), and drinking (P = 0.123), while percentages of diabetes mellitus (P < 0.001) and hypertension (P < 0.001) were substantially higher in the patients than in the controls. Other baseline demographical, clinical, radiological and biochemical characteristics of patients are displayed in Table 2.
Correlation of serum PDMPs levels with disease severity
In Fig. 2, serum PDMPs levels in patients with ACI were significantly higher than those in healthy controls (P < 0.001). Figure 3 shows that serum PDMPs levels were positively correlated with infarction volume (P < 0.001) and NIHSS scores at admission (P < 0.001). Also, Infarction volume was divided into three groups: small infarct (< 10 cm3), medium infarct (10–100 cm3), and large infarct (> 100 cm3). There was a significant difference in serum PDMPs levels among the three infarction volumes, with the highest levels detected in patients with large infarct (P < 0.05; Fig. 4). The patients were also divided into three groups according to NIHSS score: NIHSS score below 6, NIHSS score 6–10, and NIHSS score above 10. Figure 4 shows that serum PDMPs levels were markedly highest in patients with NIHSS score above 10 (P < 0.05).
Comparison of serum platelet-derived microparticles levels in the light of different infarction volumes and National Institutes of Health Stroke Scale score in patients with acute cerebral infarction. PDMPs means platelet-derived microparticles; NIHSS, National Institutes of Health Stroke Scale. *P < 0.05.
Serum PDMPs levels and poor prognosis
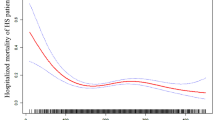
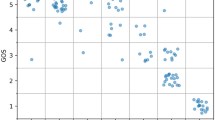
Figure 5 shows that serum PDMPs levels had a significant upward trend when patients’ mRS scores increased (P < 0.001). Also, serum PDMPs levels were significantly different among subgroups with different mRS scores (P < 0.001; Fig. 5). An aggregated of 186 (30.0%) patients experienced poor prognosis. As shown in Table 1, as opposed to patients with good prognosis, those with poor prognosis had significantly elevated percentage of diabetes mellitus (P < 0.05), and displayed substantially increased age (P < 0.01), body mass index (P < 0.05), NIHSS scores (P < 0.01), infarction volume (P < 0.05), serum glucose levels (P < 0.05), platelet count (P < 0.01) and PDMPs levels (P < 0.01). In addition, the ROC curve displays that serum PDMPs levels significantly predicted poor prognosis after ACI (Fig. 6, P < 0.001), and serum PDMPs levels > 22.50 ng/L predicted poor prognosis, with medium-high sensitivity and specificity values (Maximum Youden index J = 0.316; Fig. 6). Using the binary logistic regression analysis, age, NIHSS score and serum PDMPs levels were independently associated with END (all P < 0.05; Table 3). Furthermore, under restricted cubic spline, there was a linear relationship between serum PDMPs levels and poor prognosis risk in patients with ACI (P > 0.05; Fig. 7). In Fig. 8, serum PDMPs levels significantly interacted with age (P < 0.01), but not with gender, hypertension, diabetes mellitus, coronary heart disease, dyslipidemia, smoker, alcohol, anti-platelet therapy and thrombolysis (all P > 0.05).
Association of serum PDMPs levels with END after stroke
A total of 171 (27.5%) patients suffered from END after stroke. As shown in Table 4, compared with patients without END, those with END had substantially higher body mass index (P < 0.05), NIHSS score (P < 0.05), infarction volume (P < 0.05), proportion of diabetes mellitus (P < 0.05), serum glucose levels (P < 0.01), serum PDMPs levels (P < 0.01) levels and serum fibrinogen levels (P < 0.05). Multivariate analysis demonstrated that infarction volume, NIHSS scores and serum PDMPs levels were the independent predictors of END after ACI (All P < 0.05; Table 5). According to the ROC curve in Fig. 9, serum PDMPs levels significantly predicted the development of END after ACI (P < 0.001) and using the Youden method, serum PDMPs levels > 24.00 ng/L distinguished patients at risk of END with medium-high sensitivity and specificity values. Further restricted cubic spline shows the linear relationships between serum PDMPs levels and risk of END in patients with ACI (P > 0.05, Fig. 10). The subgroup analyses demonstrated that serum PDMPs levels were significantly associated with END in most categories, stratified by age, gender, hypertension, diabetes mellitus, coronary heart disease, dyslipidemia, smoker, alcohol, anti-platelet therapy and thrombolysis (all P < 0.05). Except coronary heart disease (P < 0.05), other variables had no significant interactions with serum PDMPs levels (all P > 0.05; Fig. 11).
Discussion
The current study investigated relationships between serum PDMPs concentrations and END in addition to clinical outcomes in ACI patients. Our study confirmed that (1) as compared with controls, PDMPs levels in serum of patients with ACI were increased significantly; (2) serum PDMPs levels of ACI patients were highly correlated with disease severity indicated by infarction volume and NIHSS score; and were also with 6-month mRS score; (3) serum PDMPs levels were independently associated with END and poor outcome at 6 months in patients with ACI and moreover, similar findings were observed in the subgroup analysis, further emphasizing the robustness of these associations. Hence, serum PDMPs may be a potential prognostic biomarker of ACI.
Previous studies showed that the incidence of END after ACI was 8.7–28.1%19,20. The incidence of END in our study was 27.5%. Currently, the underlying mechanisms of END are not fully understood. Several studies have revealed that high platelet reactivity is associated with increased risk of END in patients with ischemic stroke21 and anti-platelet therapy could prevent END and improves prognosis in these patients22, suggesting that platelet activation maybe an important factor in END in patients with ACI.
Microparticles may be released from cells upon cell activation or cell injury, or following cell activation-independent processes, including senescence and apoptosis23. They interact with neighboring cells through direct extracellular interactions and have also been shown to deliver their cytosolic contents to target cells as a means of altering cellular function24. In 1967, Wolf et al.25 showed that platelet shedding after activation results in “platelet dust”, which is now called PDMPs. PDMPs are generated during platelet activation or might result from platelet apoptosis. They are the common indicators reflecting platelet activation, which harbor approximately 100 times more prothrombotic properties than platelets. Thus, detection of PDMPs can indirectly reflect the functional status of platelets26.
Previous studies have indicated that PDMPs might play a role in the autoimmune diseases27, metabolic dysfunction and inflammation28, and contributes to tumor progression in several tumor cells29. Expression of PDMPs may be involved in various atherosclerosis and thrombotic diseases, including the development process in venous thromboembolism and myocardial infarction. Specifically, the levels of PDMPs showed significant elevation in both ST-elevation myocardial infarction and deep vein thrombosis30,31, and may reflect the severity of acute myocardial infarction as well as prothrombotic state32. Geng et al.33 reported that PDMPs levels were increased in myocardial infarction rats, and could be used as a tool to assess infarction area.
In cerebrovascular diseases, PDMPs have been found to induce cell proliferation, neurogenesis, and angiogenesis at the cerebral infarct boundary zone in a stroke model in vivo34. Additionally, PDMPs might exert a remote protective effect against cerebral ischemic–reperfusion injury9. These data indicate that PDMPs might exert a protective effect on ischemic injury. Another clinical study involving 57 ischemic stroke patients showed that circulating levels of platelet derived CD41 + microparticles were significantly related to reperfusion and recanalization, and high levels of peripheral CD41 + microparticles concentrations were detected in patients with partial or complete recanalization35. Our study showed that serum PDMPs levels were significantly increased in patients with END, and independently associated with END in patients with ACI. The subgroup analysis also confirmed that serum PDMPs levels was positively associated with END in patients with coronary heart disease, highlighting the importance of reducing serum PDMPs levels in patients with premorbid coronary heart disease. Kanazawa et al.36 found that baseline platelet count in venous blood at admission may affect the prognosis of cerebral infarction and END, which supported our results and suggested that platelet status and function could be closely related to END.
Recently, some studies has reported the role of new biomarkers in predicting the outcomes in ACI patients. Zhang et al.37 showed that serum Cav-1 combined with NGB may be helpful to predict the risk of END and 3-month poor prognosis after r intravenous thrombolysis in patients with acute ischemic stroke. Another meta-analysis found that the C-Reactive Protein/Albumin ratio was significantly associated with unfavorable outcomes38. These data indicated the intrinsic relationship of neuroinflammation with unfavorable outcomes in patients with ACI. As an inflammatory biomarker, PDMPs has been observed an significant increase in stroke patients28,39, suggesting the potential role of PDMPs as a prognostic biomarker for ACI. However, these studies were limited by relatively small sample sizes, the absence of detailed data on END, or the variability in follow-up durations (ranging from 1.5 to 90 days), which may lead to diverse impacts on outcomes. In addition, due to adoption of published literature, the meta-analysis was subject to a degree of heterogeneity and publication bias. The present study involved a relatively large sample of patients (621 patients with ACI), followed up for 6 months, and enriched the limited current evidence on the association between PDMPs and END and extends this relationship specifically to patients with ACI. The identification and quantification of PDMPs may thus be useful for the prediction of END after ACI.
A growing body of data have pointed to the prognostic role of circulating PDMPs concentrations in various kinds of cancers40,41. However, it is unclear whether there may be a correlation between serum PDMPs levels and severity plus clinical outcomes in patients with ACI. Our study not only demonstrated that serum PDMPs levels were highly associated with the severity of the neurological deficit estimated by infarction volume and NIHSS score at admission, but also showed that serum PDMPs levels were highly correlated with the functional outcome based on mRS score at 6 months after onset of stroke. Furthermore, we performed ROC analysis to reveal that serum PDMPs levels displayed a good prognostic predictive ability. Overall, it is plausible that increased serum PDMPs levels should be associated with 6-month poor prognosis of ACI, substantializing serum PDMPs as a potential prognostic biomarker of ACI.
Although a series of statistical methods were applied here to reveal some interesting results that serum PDMPs may be a potential prognostic biomarker of ACI, the current study has several limitations. First, this is a single-center study, which is characterized by a relatively small sample size, and therefore, a further cohort study with a larger sample size is required to prove our conclusions. Second, although there may be coexpression of some specific antigens between megakaryocyte-derived microparticles and PDMPs in healthy individuals, the PDMPs ELISA kit in the study used two monoclonal antibodies against glycoproteins CD42a and CD42b, which have not been detected in megakaryocyte-derived microparticles42. Thus, the kit had good specificity. Functional differences between the two microparticles would be the direction of future researches. Third, some relevant variables (such as age, diabetes and hypertension) were unbalanced between ACI patients and health controls. The further matching cohorts were needed to determine the difference in serum PDMPs levels. Finally, serum PDMPs levels were measured in a time point after ACI in this study and dynamic change of serum PDMPs levels is not detected. Investigating serial change of its level in future may be of clinical significance. Whereas, the current study was a pilot and exploratory study, which could provide some new information for the further studies. Thus, the independent and multicenter studies measuring serial PDMP levels were needed to validate the findings.
Conclusions
This study confirmed that increased serum PDMPs levels at admission are strongly relevant to the severity determined by infarction volume and admission NIHSS scores. Moreover, elevated serum PDMPs levels could assist in predicting the risk of END occurrence and poor prognosis at 6 months after ACI in patients, indicating that PDMPs in serum might have the potential to be a useful prognostic biomarker in patients with ACI.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available because they are personal data, but are available from the corresponding author upon reasonable request.
References
Mendelson, S. J. & Prabhakaran, S. Diagnosis and management of transient ischemic attack and acute ischemic stroke: A review. JAMA 325(11), 1088–1098 (2021).
Herpich, F. & Rincon, F. Management of acute ischemic stroke. Crit. Care Med. 48(11), 1654–1663 (2020).
He, L. et al. Capsular warning syndrome: clinical analysis and treatment. Capsular warning syndrome: clinical analysis and treatment. BMC Neurol. 19(1), 285 (2019).
Fisher, M. & Savitz, S. I. Pharmacological brain cytoprotection in acute ischaemic stroke-renewed hope in the reperfusion era. Nat. Rev. Neurol. 18(4), 193–202 (2022).
Kuriyama, N. et al. Evaluation of factors associated with elevated levels of platelet-derived microparticles in the acute phase of cerebral infarction. Clin. Appl. Thromb. Hemost. 16(1), 26–32 (2010).
Mechtouff, L. et al. Association of blood biomarkers of inflammation with penumbra consumption after mechanical thrombectomy in patients with acute ischemic stroke. Neurology 99(18), e2063–e2071 (2022).
Kassassir, H. et al. Platelet-derived microparticles stimulate the invasiveness of colorectal cancer cells via the p38MAPK-MMP-2/MMP-9 axis. Cell. Commun. Signal. 21(1), 51 (2023).
Signorelli, S. S. et al. Platelet-derived microparticles (MPs) and thrombin generation velocity in deep vein thrombosis (DVT): Results of a case-control study. Vasc Health Risk Mana. 16, 489–495 (2020).
Shan, L. Y. et al. Platelet-derived microparticles are implicated in remote ischemia conditioning in a rat model of cerebral infarction. CNS Neurosci. Ther. 19(12), 917–925 (2013).
Hartopo, A. B. et al. Circulating platelet-derived microparticles associated with postdischarge major adverse cardiac events in ST-Elevation acute myocardial infarction. Cardiol. Res. Pract. 2020, 6721584 (2020).
Wang, C. et al. Clopidogrel plus aspirin prevents early neurologic deterioration and improves 6-month outcome in patients with acute large artery atherosclerosis stroke. Clin. Appl. Thromb. Hemost. 21(5), 453–461 (2015).
Chiva-Blanch, G. et al. Microparticle shedding from neural progenitor cells and vascular compartment cells is increased in ischemic stroke. PLoS One. 11(1), e0148176 (2016).
Schrick, D. et al. Circulating microvesicles in convalescent ischemic stroke patients: A contributor to High-On-Treatment residual platelet reactivity?? Front. Biosci. (Landmark Ed) 27(5), 158 (2022).
Liu, L. et al. Chinese stroke association guidelines for clinical management of ischaemic cerebrovascular diseases: Executive summary and 2023 update. Stroke Vasc Neurol. 8(6), e3 (2023).
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. https://www.wma.net/members-area/working-documents/201804_cs_english/
Khatri, P. Intravenous thrombolysis before thrombectomy for acute ischaemic stroke. Lancet 400(10346), 76–78 (2022).
Seners, P. et al. Prediction of early neurological deterioration in individuals with minor stroke and large vessel occlusion intended for intravenous thrombolysis alone. JAMA Neurol. 78(3), 321–328 (2021).
Nomura, S. et al. Assessment of an ELISA kit for platelet-derived microparticles by joint research at many institutes in Japan. J. Atheroscler Thromb. 16(6), 878–887 (2009).
Seners, P. et al. Incidence, causes and predictors of neurological deterioration occurring within 24 h following acute ischaemic stroke: a systematic review with pathophysiological implications. J. Neurol. Neurosurg. Psychiatry. 86(1), 87–94 (2015).
Zhao, W. et al. Effects of Tirofiban on neurological deterioration in patients with acute ischemic stroke: A randomized clinical trial. JAMA Neurol. e240868 (2024).
Zhou, K. et al. High on-treatment platelet reactivity is associated with poor outcomes after ischemic stroke: A meta-analysis. Acta Neurol. Scand. 146(3), 205–224 (2022).
Wiśniewski, A. et al. A combination of aspirin and clopidogrel predict more favorable dynamics of platelet reactivity versus clopidogrel alone in the acute phase of minor stroke. Healthcare (Basel) 9(6), 628 (2021).
Fidan, E. B., Bali, E. B. & Apaydin, F. G. Comparative study of nickel oxide and nickel oxide nanoparticles on oxidative damage, apoptosis and histopathological alterations in rat lung tissues. J. Trace Elem. Med. Biol. 83, 127379 (2023).
Zwicker, J. I. et al. Tissue factor-bearing microparticles and thrombus formation. Arterioscler. Thromb. Vasc Biol. 31(4), 728–733 (2011).
Wolf, P. The nature and significance of platelet products in human plasma. Br. J. Haematol. 13(3), 269–288 (1967).
Custodio-Chablé, S. J., Lezama, R. A. & Reyes-Maldonado, E. Platelet activation as a trigger factor for inflammation and atherosclerosis. Cir. Cir. 88(2), 233–243 (2020).
Li, X. & Wang, Q. Platelet-derived microparticles and autoimmune diseases. Int. J. Mol. Sci. 24(12), 10275 (2023).
El-Gamal, H. et al. Circulating microparticles as biomarkers of stroke: A focus on the value of endothelial- and platelet-derived microparticles. J. Cell. Physiol. 234(10), 16739–16754 (2019).
Mezouar, S. et al. Involvement of platelet-derived microparticles in tumor progression and thrombosis. Semin. Oncol. 41(3), 346–358 (2014).
Signorelli, S. S. et al. Platelet-derived microparticles (MPs) and thrombin generation velocity in deep vein thrombosis (DVT): Results of a case-control study. Vasc. Health Risk Manag. 16, 489–495 (2020).
Indana, H. A. et al. Association of acute hyperglycemia and diabetes mellitus with platelet-derived microparticle (PDMP) levels during acute myocardial infarction. J. ASEAN Fed. Endocr. Soc. 38(2), 35–40 (2023).
Chiva-Blanch, G. et al. Platelet-, monocyte-derived and tissue factor-carrying circulating microparticles are related to acute myocardial infarction severity. PLoS One. 12(2), e0172558 (2017).
Geng, X. Y. et al. Platelet microparticles: A tool to predict infarction area in rats. J. Invest. Surg. 34(1), 64–69 (2021).
Hayon, Y. et al. Platelet microparticles induce angiogenesis and neurogenesis after cerebral ischemia. Curr. Neurovasc Res. 9(3), 185–192 (2012).
Bivard, A. et al. Platelet microparticles: A biomarker for recanalization in rtPA-treated ischemic stroke patients. Ann. Clin. Transl Neurol. 4(3), 175–179 (2017).
Awelczyk, M., Kaczorowska, B. & Baj, Z. The impact of hyperglycemia and hyperlipidemia on plasma P-selectin and platelet markers after ischemic stroke. Arch. Med. Sci. 13(5), 1049–1056 (2017).
Zhang, L. et al. Prognostic values serum Cav-1 and NGB levels in early neurological deterioration after intravenous thrombolysis in patients with acute ischemic stroke. Clin. Appl. Thromb. Hemost. 29, 10760296231219707 (2023).
de Liyis, B. G. et al. High C-Reactive protein/ albumin ratio predicts mortality and hemorrhage in stroke patients undergoing mechanical thrombectomy: A systematic review and meta-analysis. World Neurosurg. 188, 211–219e1 (2024).
Pawelczyk, M., Kaczorowska, B. & Baj, Z. Fibrinogen concentrations in ischaemic stroke patients with metabolic disorders. Neurol. Neurochir. Pol. 54 (3), 259–264 (2020).
Qu, M. et al. Platelet-derived microparticles enhance megakaryocyte differentiation and platelet generation via miR-1915-3p. Nat. Commun. 11(1), 4964 (2020).
Lazar, S. & Goldfinger, L. E. Platelet microparticles and MiRNA transfer in cancer progression: many targets, modes of action, and effects across cancer stages. Front. Cardiovasc. Med. 5, 13 (2018).
Flaumenhaft, R. et al. Megakaryocyte-derived microparticles: Direct visualization and distinction from platelet-derived microparticles. Blood 113(5), 1112–1121 (2009).
Acknowledgements
We gratefully thank all study participants, their relatives, and the staffs at the recruitment centers for their invaluable contributions.
Funding
The authors received financial support for the research from science and technology plan project of Wenzhou city in Zhejiang province (Y2020066).
Author information
Authors and Affiliations
Contributions
S.-S.H., X.-D.H. and X.-L.M.: Conceptualization, Methodology, Writing—Reviewing and Editing. S.-Z.Z. and Q.-Q.Z.: Data curation, Writing—Original draft preparation. X.-X.C.: Visualization, Investigation. H.-D.W.: Supervision, Sofware, Validation. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
He, SS., Huang, XD., Zhang, SZ. et al. A prospective cohort study on prognostic implications of serum platelet derived microparticles levels in acute cerebral infarction. Sci Rep 15, 14197 (2025). https://doi.org/10.1038/s41598-025-92732-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-92732-z