Abstract
Diabetic retinopathy (DR) is a common complication of type II diabetes mellitus (T2DM) and a leading cause of blindness in the working population. Apolipoprotein levels have been reported to be associated with the risk of DR. This study aimed to develop a predictive model for DR based on apolipoproteins (apoA and apoB) and menopausal status in Chinese Han women with T2DM and to evaluate the model’s effectiveness. Data from 2339 T2DM women were collected between January 2018 and June 2022. Multilevel regression was used to explore the independent effect of apolipoproteins and interaction between apolipoproteins and menopausal status on DR and proliferative diabetic retinopathy (PDR). Receiver operating characteristic (ROC) analysis was performed to compare the fitting degree and predictive efficiency of different models. Results showed that both apoA and apoB were independent influencing factors for DR and PDR and interacted significantly with menopausal status. The interaction between apoA and menopausal status had a protective effect on DR [OR (95% CI) = 0.925 (0.858–0.996), P = 0.040] and PDR [OR (95% CI) = 0.937 (0.895–0.981), P = 0.006]. In contrast, the interaction between apoB and menopausal status was a risk factor for DR [OR (95% CI) = 1.684 (1.141–2.379), P = 0.008)] and PDR [OR (95% CI) = 3.377 (1.148–9.937), P = 0.027]. ROC analysis demonstrated that the interaction model outperformed models without interaction terms (P < 0.01). The area under the curve for the interaction model was 0.879 (95% CI 0.864–0.893) for DR and 0.930 (95% CI 0.915–0.945) for PDR. These findings suggest that the interaction model is highly efficient in predicting DR, particularly PDR, in Chinese Han women with T2DM.
Similar content being viewed by others
Background
Diabetic retinopathy (DR) is one of the most prevalent complications of type II diabetes mellitus (T2DM) and represents the leading cause of blindness among the adult working population1,2. Beyond its detrimental effects on vision, DR significantly increases the risk of cardiovascular diseases. By 2025, the global prevalence of DR is projected to rise to 5.4%3. According to the International Diabetes Federation (2021), there are 300 million women worldwide with diabetes mellitus (DM), representing a prevalence rate of 10.2%4. In China, the prevalence of DR in women with DM is notably higher at 29.8%5. DR has thus become a critical public health challenge globally6. Its onset is often insidious, and delayed diagnosis can lead to vision-threatening complications. Furthermore, the endocrinology departments, where most T2DM patients first seek care, are often insufficiently equipped to diagnose DR early. This underscores the urgent need for sensitive biomarkers to facilitate timely detection of DR.
T2DM is a systemic metabolic disorder frequently accompanied by dyslipidemia7,8. Dyslipidemia accelerates pathological processes such as non-enzymatic glycosylation and polyol pathway activation, which contribute to microvascular basement membrane thickening, endothelial dysfunction, microcirculatory disturbances, retinal barrier damage, and other DR-related pathological changes9,10. Compared to DM patients without dyslipidemia, those with dyslipidemia exhibit a higher prevalence of DR11,12,13. Lipoprotein, apolipoproteins, low-density lipoprotein (LDL), high-density lipoprotein (HDL), and total cholesterol (TC) are strongly associated with the incidence and severity of DR12,14. Apolipoproteins, which mediate cholesterol transport from blood to the liver, play a pivotal role in lipid metabolism and are linked to an elevated risk of coronary heart disease, stroke, and DR12,15,16.
Additionally, menopause has been shown to influence apolipoprotein levels and DR prevalence17,18. The rapid decline in estrogen levels among postmenopausal women contributes to dyslipidemia and diminishes the protective effects on retinal ganglion cells (RGCs)18,19. Despite these findings, no prior studies have explored whether the interaction between apolipoproteins and menopausal status affects DR.
This cross-sectional study aims to investigate the relationship between apolipoproteins and menopausal status in relation to DR in women with T2DM. Furthermore, an interaction model was developed to evaluate the combined effects of apolipoproteins and menopausal status on DR. Receiver operator characteristic (ROC) analysis was conducted to assess the model’s fitting degree and prediction efficiency.
Materials and methods
Participants
This cross-sectional study included female patients with T2DM who were hospitalized in the Endocrinology Departments of Henan Provincial People’s Hospital, Guangshan County People’s Hospital, and Xincai County People’s Hospital between January 2018 and December 2021.
Inclusion criteria Female patients aged ≥ 18 years with T2DM diagnosed according to the 2018 standards of the American Diabetes Association, which include fasting plasma glucose ≥ 7.0 mmol/L, oral glucose tolerance test two-hour plasma glucose ≥ 11.1 mmol/L, HbA1c ≥ 6.5%, or self-reported T2DM. Participants were required to provide informed consent and agree to participate in the study.
Exclusion criteria Patients were excluded if they had other retinal diseases that could be confused with DR, such as hypertensive retinal disease, retinal vasculitis, or retinal vein occlusion. Exclusion also applied to patients lacking key data, including age, menopausal status, or blood lipid measurements, as well as those with unclear fundus photos due to small pupils, cataracts, or vitreous opacity.
This study adhered to the principles outlined in the Declaration of Helsinki and was approved by the Ethics Committee of Henan Provincial People’s Hospital [ethical approval code: HNEECKY-2022(22)]. All participants were fully informed about the purpose and details of the study and provided written informed consent.
The sample size was calculated using PASS 11.0 software, based on formulas for cross-sectional studies (formula a) and diagnostic tests (formula b)20. The significance level (α) was set at 0.05, statistical power at 0.90, and allowable error (δ) at 0.08. In formula (a), k represented the ratio of patients without DR to those with DR, with k = 1 in this study. In formula (b), p represented the sensitivity or specificity of the diagnostic method. Pre-survey results indicated that the mean apoA levels in T2DM patients with and without DR were 1.16 ± 0.37 g/L and 1.07 ± 0.43 g/L, respectively, and the mean apoB levels were 0.96 ± 0.38 g/L and 0.89 ± 0.41 g/L, respectively. The sensitivity and specificity of the diagnostic method were 80.3% and 78.6%, respectively. Based on these parameters, the required sample size was 418 for both the DR and non-DR groups. To account for potential invalid samples, a 20% margin was added, resulting in a minimum required sample size of 502 for each group.
Data collection
At the beginning of the study, a self-designed questionnaire was used to collect information from participants, including demographic characteristics, menopausal status, age at the onset of menopause, medical history, and family history. Fundus examinations were conducted by an experienced ophthalmologist using a Zeiss non-mydriatic fundus camera (VISUCAM 224, Germany). Images were captured from five fields of each eye: macula-centered, temporal, nasal, upper quadrant, and lower quadrant of the retina. Additionally, optical coherence tomography angiography (OCTA) was performed to evaluate retinal microvascular changes in the T2DM patients.
Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured after 10 min of seated rest. Measurements were taken three times by the same staff using a calibrated M7 digital sphygmomanometer (Omron M7, Hoofddorp, The Netherlands), and the average of the three readings was recorded.
Blood samples were collected from fasting veins in the morning, and serum samples were separated to measure levels of lipoprotein (a) (Lpa), apolipoprotein A (apoA), apolipoprotein B (apoB), HDL, LDL, triglyceride (TG), TC, and hemoglobin A1c (HbA1c). Clinical data and biochemical indicator values were retrieved from the hospital information system and independently checked by two authors to ensure accuracy.
Definitions and diagnostic criteria
The diagnosis of DR was determined by an ophthalmologist with more than five years of clinical experience based on the International Clinical Diabetic Retinopathy (ICDR) criteria21. DR was classified into three categories: (1) Absence of DR (NDR): no visible signs of retinopathy or abnormalities; (2) Non-proliferative diabetic retinopathy (NPDR): the early stage of DR characterized by leaking blood vessels or fluid within the retina without the formation of new blood vessels; and (3) Proliferative diabetic retinopathy (PDR): an advanced stage of DR involving the growth of abnormal and fragile new blood vessels triggered by retinal signals (neovascularization). “Any DR” includes both NPDR and PDR. In cases where grading results from two clinicians were inconsistent, a panel of four retina specialists adjudicated to establish the reference standard. Patients with DR in both eyes were treated as a single case, and the severity of DR was graded according to the more severely affected eye. Menopause was defined as meeting any of the following criteria: (a) amenorrhea for ≥ 12 months; (b) age ≥ 60 years; or (c) a history of bilateral ovariectomy in T2DM patients22.
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics 25.0 (IBM, Chicago, IL) and R software (version 4.2.0). Quantitative data were described as mean ± standard deviation (SD) for normal distribution data and median (inter-quartile range, IQR) for skewed data. Quantitative data were compared by t-test (normal distribution data) or nonparametric test (skewed data). Qualitative data were described by frequency and were compared by chi-square test. Multilevel regression analysis was employed to evaluate the relationships between apolipoproteins, menopausal status, and DR. Interaction models were constructed to examine the combined effects of apolipoproteins and menopausal status on DR. Forest plots of the multilevel regression results were generated using R software (version 4.2.0). The importance ranking of variables and Shapley Additive Explanations (SHAP) dependency plots were generated based on a random forest model, using the “randomForest,” “shapviz,” and “randomForestExplainer” packages in R software (version 4.2.0). ROC analysis was performed to evaluate the model’s fitting degree and predictive efficiency for DR and PDR. ROC curves were generated using IBM SPSS Statistics 25.0 (IBM, Chicago, IL). The DeLong test was applied to compare the area under the curve (AUC) between ROC curves. All statistical tests were two-sided, with a significance level of α = 0.05.
Results
Participant characteristics
According to the inclusion criteria, a total of 2463 female T2DM patients were screened. Their personal information and clinical data were collected, and 124 patients were excluded because of incomplete information or unclear fundus photos. Therefore, 2339 patients aged 18–92 (58.17 ± 13.87) were analyzed. Among them, 1621 patients (69.3%) were postmenopausal, and 718 (30.7%) were premenopausal. The duration of T2DM was 9.69 ± 7.48 years. There were 925 (including 635 NPDR and 290 PDR) DR patients and 1414 (60.5%) non-diabetic retinopathy (NDR) patients. The general characteristics and biochemical indicators of the two groups are shown in Table 1.
Association between apolipoprotein and DR in premenopausal and postmenopausal women with T2DM
Our preliminary analysis indicated that the relationships between apoA, apoB, and the prevalence of DR were non-linear. Compared to analyzing these variables as continuous numerical data, converting apoA and apoB into categorical variables based on quartiles allowed us to more accurately capture their associations with DR. Consequently, all patients were divided into four groups according to the quartile of apoA (apoAP1: apoA ≤ 1.07 g/L, apoAP2: 1.08 g/L ≤ apoA ≤ 1.19 g/L, apoAP3: 1.20 g/L ≤ apoA ≤ 1.36 g/L, apoAP4: apoA ≥ 1.37 g/L) and apoB (apoBP1: apoB ≤ 0.78 g/L, apoBP2: 0.79 g/L ≤ apoB ≤ 0.98 g/L, apoBP3: 0.99 g/L ≤ apoB ≤ 1.22 g/L, apoBP4: apoB ≥ 1.23 g/L). The prevalence of DR and PDR was analyzed across these groups (Fig. 1A, B).
In premenopausal women, the prevalence of both DR and PDR was significantly higher in the highest apoA quartile (apoAP4) compared to the second and third quartiles (apoAP2 and apoAP3) [(any DR: apoAP2 vs. apoAP4: 25.0% vs. 44.4%, P = 0.001; apoAP3 vs. apoAP4: 27.5% vs. 44.4%, P = 0.002), (PDR: apoAP2 vs. apoAP4: 12.5% vs. 25.9%, P = 0.005; apoAP3 vs. apoAP4: 9.2% vs. 25.9%, P < 0.001)]. Similarly, the prevalence was higher in the lowest apoB quartile (apoBP1) compared to the third and fourth quartiles (apoBP3 and apoBP4) [(any DR: apoBP1 vs. apoBP3: 43.8% vs. 33.0%, P = 0.036; apoBP1 vs. apoBP4: 43.8% vs. 25.0%, P < 0.001), (PDR: apoBP1 vs. apoBP3: 22.5% vs.11.4%, P = 0.005; apoBP1 vs. apoBP4: 22.5% vs. 14.1%, P = 0.040)].
In postmenopausal women, different patterns were observed. The prevalence of DR and PDR was lower in the lowest (apoAP1) and highest (apoAP4) apoA quartiles compared to the second (apoAP2) and third (apoAP3) quartiles [(any DR: apoAP1 vs. apoAP2: 37.6% vs. 51.5%, P < 0.001; apoAP1 vs. apoAP3: 37.6% vs. 47.4%, P = 0.006; apoAP2 vs. apoAP4: 51.5% vs. 37.8%, P < 0.001; apoAP3 vs. apoAP4: 47.4% vs. 37.8%, P = 0.005), (PDR: apoAP1 vs. apoAP2: 7.4% vs. 14.6%, P = 0.001; apoAP1 vs. apoAP3: 7.4% vs. 15.1%, P = 0.001; apoAP2 vs. apoAP4: 14.6% vs. 8.7%, P = 0.006; apoAP3 vs. apoAP4: 15.1% vs. 8.7%, P = 0.004)]. Conversely, the prevalence was lower in the first (apoBP1) and second (apoBP2) apoB quartiles compared to the fourth quartile (apoBP4) [(any DR: apoBP1 vs. apoBP4: 31.5% vs. 49.7%, P < 0.001; apoBP2 vs. apoBP4: 40.9% vs. 49.7%, P = 0.015), (PDR: apoBP1 vs. apoBP4: 8.8% vs. 18.5%, P < 0.001; apoBP2 vs. apoBP4: 10.0% vs. 18.5%, P = 0.001)].
These results suggest that the effects of apoA and apoB on DR and PDR differ between premenopausal and postmenopausal women with T2DM. Specifically, in premenopausal women, the relationship between apoA and DR/PDR prevalence exhibited a U-shaped pattern, while apoB showed an L-shaped pattern. In postmenopausal women, apoA and DR/PDR prevalence demonstrated an inverted U-shaped pattern, whereas apoB followed a J-shaped pattern.
The correlation between apoA and apoB
Spearman correlation analysis was performed to evaluate the relationship between apoA and apoB levels. The Spearman correlation coefficients (rs) are summarized in Table 2. The analysis revealed no significant linear correlation between apoA and apoB in premenopausal women with T2DM (rs = − 0.043, P = 0.254). However, a weak but statistically significant correlation was observed in the overall study population (rs = 0.041, P = 0.045) and in postmenopausal women with T2DM (rs = 0.077, P = 0.002). When stratified by DR status, the correlation between apoA and apoB was stronger in patients with DR compared to those without DR (NDR), with the highest correlation observed in PDR patients. These findings suggest that the relationship between apoA and apoB is influenced by both menopausal status and the presence or severity of DR.
Apolipoprotein and menopausal status as significant factors for DR in women with T2DM
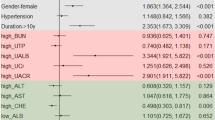
To investigate the influence of apolipoproteins and menopausal status on DR, we constructed five multilevel regression models using DR and PDR as dependent variables. The independent variables and covariates included in these models are detailed in Table 3. In Models 2, 4, and 5, menopausal status was treated as a within-subject variable. Forest plots illustrating the multilevel regression results are presented in Fig. 2A, B. When apoA and apoB were analyzed independently (Models 1 and 3), their effects on DR were relatively small. However, after incorporating menopausal status and its interaction with these apolipoproteins, their influence on DR increased significantly (Models 2 and 4). This indicates that apoA and apoB not only directly affect DR prevalence but also indirectly influence it through their interaction with menopausal status. In the comprehensive Model 5, which included apoA, apoB, menopausal status, and interaction terms, the results showed that apoA levels of ≥ 1.20 g/L were associated with an increased risk of DR (1.20 g/L ≤ apoA ≤ 1.36 g/L: OR (95% CI) = 1.900 (1.047–3.448), P = 0.035; apoA ≥ 1.37 g/L: OR (95% CI) = 3.881 (1.988–7.579), P < 0.001) and PDR (1.20 g/L ≤ apoA ≤ 1.36 g/L: OR (95% CI) = 2.394 (1.248–4.593), P = 0.009; apoA ≥ 1.37 g/L: OR (95% CI) = 7.798 (3.061–19.867), P < 0.001). The interaction between apoA and menopausal status demonstrated a weak protective effect on DR [OR (95% CI) = 0.925 (0.858–0.996), P = 0.040] and PDR [OR (95% CI) = 0.937(0.895–0.981), P = 0.006]. Similarly, higher apoB levels (≥ 1.23 g/L) were associated with an increased prevalence of DR [OR (95% CI) = 1.594 (1.135–2.240), P = 0.007] and PDR [OR (95% CI) = 1.747 (1.051–2.905), P = 0.031]. The interaction between apoB and menopausal status had an adverse effect on DR [OR (95% CI) = 1.648 (1.141–2.379), P = 0.008] and PDR [OR (95% CI) = 3.377 (1.148–9.937), P = 0.027]. Postmenopausal women were at a higher risk of DR [OR (95% CI) = 1.843 (1.517–2.239), P < 0.001] and PDR [OR (95% CI) = 1.078 (1.008–1.154), P = 0.027] compared to premenopausal women. Additionally, the interaction between apoA and age showed adverse effects on DR [OR (95% CI) = 1.034 (1.028–1.041), P < 0.001] and PDR [OR (95% CI) = 1.108 (1.037–1.183), P = 0.003].
A random forest model was also utilized to determine the importance of independent variables for DR and PDR. The ranking of feature importance based on accuracy is depicted in Fig. 3A (DR) and Fig. 3B (PDR). These results highlighted apoA, apoB, and menopausal status as critical factors, with apoA having a greater impact than apoB. Based on the random forest model, SHAP values were computed to visualize the effects of these variables, and the dependence plots are shown in Fig. 3C–F. The results indicated a non-linear relationship between apoA and DR, with interactions between lower and higher apoA levels and menopausal status exhibiting contrasting effects. Specifically, low and high apoA levels combined with non-menopausal status had a positive effect on DR, while the same levels combined with menopausal status had a negative effect (Fig. 3C, D). Conversely, apoB displayed an approximately linear relationship with DR, and higher apoB levels combined with menopausal status amplified DR risk (Fig. 3E, F). These findings, consistent with the multilevel regression analysis, suggest that apoA, apoB, menopausal status, and their interactions are significant factors influencing DR and PDR in women with T2DM.
The importance and SHAP value of apoA and apoB based on random forest model. A The importance of apoA, apoB, and other independent variables on the dependent variable (DR) in the random forest model; B The importance of apoA, apoB, and other independent variables on the dependent variable (PDR) in the random forest model; C SHAP dependency plot of apoA on DR based on random forest model, purple represents premenopausal individuals, while yellow represents postmenopausal individuals; D SHAP dependent plot of the interaction effect between apoA and menopause on DR; E SHAP dependency plot of apoB on DR based on random forest model, purple represents premenopausal individuals, while yellow represents postmenopausal individuals; F SHAP dependent plot of the interaction effect between apoB and menopause on DR
The fitting degree and prediction efficiency of the five models in women with T2DM
To evaluate the fitting degree and prediction efficiency of the five models, we used DR and PDR as state variables and the prediction probabilities of the models as test variables to construct ROC curves (Fig. 4A, B). The ROC analysis revealed that models incorporating menopausal status and interaction effects had a significantly better fit compared to models without these variables. Specifically, the comparison between models 1 and 2 showed an improvement in the AUC (0.671 vs. 0.727, Z = 3.600, P < 0.001). Similarly, the AUC for model 4, which included interaction effects, was significantly higher than that of model 3 (0.703 vs. 0.661, Z = 2.700, P = 0.007). Model 5, which included both apoA and apoB along with menopausal status and their interactions, demonstrated the best fitting degree among all models. The AUC of model 5 was significantly higher compared to model 2 (0.879 vs. 0.727, Z = 11.658, P < 0.001) and model 4 (0.879 vs. 0.703, Z = 13.499, P < 0.001), for both any DR and PDR. Additionally, model 5 showed superior predictive efficiency for PDR compared to any DR, with an AUC of 0.930 for PDR versus 0.879 for any DR (Z = 4.798, P < 0.001). The results of the five model in predicting DR and PDR are shown in Table 4. These findings suggest that incorporating the interaction between apolipoproteins and menopausal status significantly enhances the model’s ability to explain variations in DR and PDR, providing a more robust predictive model.
Discussion
Apolipoproteins, primarily synthesized in the liver, combine with lipids to form lipoproteins, which are crucial for lipid metabolism and transportation. These processes play a significant role in regulating blood lipid levels23,24. Apolipoproteins have been shown to be closely associated with the occurrence and progression of DR12. This study provides evidence that in female patients with T2DM, the effects of apoA and apoB on DR and PDR differ between premenopausal and postmenopausal women. Specifically, the interaction between apolipoproteins and menopausal status significantly influences the prevalence of both any DR and PDR. Our findings demonstrate that incorporating the interaction between apoA, apoB, and menopausal status into regression models significantly improves the explanation of variations in DR and PDR. The models that included interaction terms outperformed those without interactions in terms of fitting degree and predictive efficiency. Notably, the prediction efficiency for PDR in the interaction model was superior to that for any DR. These results highlight the importance of considering both apolipoproteins and menopausal status, along with their interactions, when studying the risk factors for DR and PDR in women with T2DM. This approach provides a more nuanced understanding of the mechanisms underlying these conditions and could contribute to more targeted screening and intervention strategies.
This study investigated the influence of apolipoproteins and menopausal status on the prevalence of DR and PDR in female patients with T2DM using statistical descriptions and multilevel regression analyses, incorporating interaction effects. The findings revealed that the relationship between apolipoproteins and DR varied significantly between premenopausal and postmenopausal patients and that apolipoproteins exerted distinct effects on DR at different levels. In premenopausal women, those with apoA levels ≥ 1.37 g/L had a higher risk of DR compared to those with apoA levels < 1.37 g/L, while those with apoB levels ≤ 0.78 g/L exhibited a higher risk of DR than those with apoB levels > 0.78 g/L. In contrast, in postmenopausal women, those with apoA levels > 1.07 g/L but < 1.37 g/L faced a higher risk of DR compared to those with apoA levels ≤ 1.07 g/L or ≥ 1.37 g/L. Similarly, postmenopausal women with apoB levels ≤ 0.98 g/L had a lower risk of DR than those with levels > 0.98 g/L. These findings underscore the importance of routine monitoring of apolipoprotein levels in T2DM women. For premenopausal women, fundus examinations should be performed when apoA levels are ≥ 1.37 g/L and apoB levels are ≤ 0.78 g/L. For postmenopausal women, fundus function should be evaluated when apoA levels exceed 1.07 g/L or apoB levels exceed 0.98 g/L to detect and address potential DR early.
Multilevel regression analyses showed that, without considering menopausal status, apoA and apoB had relatively small effects on DR prevalence. However, when menopausal status and its interaction with apolipoproteins were included, the impact of both apoA and apoB on DR increased significantly. The comprehensive Model 5 demonstrated that apoA, apoB, menopausal status, and their interactions all significantly influenced DR prevalence. While menopause and the interaction between apoB and menopausal status were identified as risk factors for DR and PDR, the interaction between apoA and menopausal status acted as a protective factor for both conditions. The predictive performance of the five models was also evaluated, with Model 5 achieving the highest AUC values of 0.879 for any DR and 0.930 for PDR. The accuracy of Model 5 was 83.0% for DR and 86.3% for PDR. These findings suggest that the interaction model is a valuable tool for predicting DR in women, particularly for identifying those at risk for PDR.
DR is a common microvascular complication of T2DM. Patients with T2DM and DR face an elevated risk of cardiovascular complications, including stroke and coronary heart disease25,26,27,28. Given these serious health implications, identifying reliable biomarkers for DR holds significant clinical importance. This study demonstrated that dyslipidemia, specifically abnormal levels of apoA and apoB, is statistically associated with DR prevalence. Moreover, the relationship between apolipoproteins and DR varied based on menopausal status, suggesting a complex interplay between lipid profiles and hormonal factors in DR pathogenesis.
Comparisons with previous studies underscore the novelty of these findings. A cross-sectional study by Ankit et al. conducted in India reported that HDL and apoAI levels were inversely related to DR severity, while apoB levels were positively correlated with DR severity in a cohort of 117 DR patients29. Consistent with these observations, our study confirmed associations between apolipoproteins and DR but highlighted differences between premenopausal and postmenopausal women, revealing unique patterns that were not explored in earlier research. Similarly, a retrospective cohort study of 1023 diabetes patients found that baseline serum apoAI levels ≥ 7.4 µmol/L were associated with a reduced risk of DR, while elevated levels of apoCIII (≥ 6.3 µmol/L), apoE (≥ 1.1 µmol/L), and ratios such as apoCIII/apoAI (≥ 0.9) and apoE/apoAI (≥ 0.2) were linked to an increased risk of DR30. Additionally, a case-control study by Moosaie et al. demonstrated a negative correlation between serum apoA and DR risk in T2DM patients12. While these studies support the role of apolipoproteins in DR, our findings provide deeper insights by stratifying results based on menopausal status, emphasizing the influence of hormonal changes on apolipoprotein effects. These distinctions advance the understanding of apolipoprotein-related dyslipidemia as a potential biomarker for DR, particularly in the context of menopausal transitions in women with T2DM.
Previous studies have suggested that elevated levels of apoA and its subtypes may act as protective factors against DR, while apoB has been positively correlated with DR severity. However, our findings diverge from these patterns. In premenopausal women with T2DM, apoA levels ≥ 1.37 g/L were identified as a risk factor for DR, while lower apoB levels emerged as a risk factor. In postmenopausal women, lower apoB levels became a protective factor. Several factors may explain these differences. First, the outcome in our study focused on the prevalence of DR, whereas studies by Ankit et al. and Moosaie et al. examined DR severity. This distinction in study endpoints likely contributes to the observed discrepancies. Second, the influence of estrogen on the pathophysiology of DR provides a compelling explanation. In hyperglycemic environments, estrogen, specifically 17β-estradiol, stabilizes the mitochondrial membrane potential in RGCs, reduces intracellular reactive oxygen species (ROS) levels, upregulates anti-apoptotic protein Bcl-2, and inhibits pro-apoptotic protein Bax. These processes collectively protect retinal ganglia and reduce cell apoptosis. Before menopause, the presence of estrogen may antagonize the adverse effects of apolipoproteins on DR. This protective effect diminishes after menopause due to the rapid decline in estrogen levels, potentially explaining the increased prevalence of DR in postmenopausal women18. In contrast, prior studies did not account for the modulatory role of estrogen, highlighting a critical gap that our findings address. These results underscore the importance of considering hormonal influences when evaluating the relationship between apolipoproteins and DR, particularly in the context of menopausal transitions. Such insights can inform more targeted approaches to the prevention and treatment of DR in women with T2DM.
Most previous studies examining the relationship between cholesterol or apolipoprotein levels and DR prevalence did not consider the potential impact of menopausal status. In contrast, our study separately analyzed the associations between apolipoproteins and DR in premenopausal and postmenopausal women. Additionally, we assessed the interaction between apolipoproteins and menopausal status using multilevel regression models. The results of our ROC analysis demonstrated that regression models incorporating interaction terms outperformed those without interactions, underscoring the importance of accounting for the interplay between apolipoproteins and menopausal status. Furthermore, the combined action model of apoA and apoB exhibited superior predictive performance compared to models evaluating apoA or apoB independently. This finding suggests that apolipoproteins influence DR not only independently but also indirectly through their interactions with sex hormones.
Moreover, DR patients often first visit endocrinology departments, where the use of fundus cameras and OCTA may not be routine. Consequently, DR is frequently underdiagnosed in its early stages. The measurement of apoA and apoB, however, is a standard part of biochemical testing in endocrinology clinics. This routine assessment does not increase patients’ medical expenses and could serve as an auxiliary diagnostic tool for identifying patients at higher risk for DR. Our findings highlight the practical significance of integrating apolipoprotein levels into DR screening protocols, especially in endocrinology settings. This approach could improve the timely diagnosis and management of DR, particularly in women with T2DM.
However, this study has several limitations that should be acknowledged. First, while apolipoproteins were the primary focus of this analysis, other factors influencing the prevalence of DR, such as comorbid conditions, glycemic and lipid control, lipid management practices, self-compensation levels, and lifestyle variables, were not included. The omission of these variables may have introduced bias into the results. Second, menopausal status in this study was defined based on age, amenorrheic duration, and a history of bilateral ovariectomy. This definition did not account for hormonal markers such as follicle-stimulating hormone and estradiol levels, which could provide a more precise classification of menopausal status. Lastly, the cross-sectional design of this study limits its ability to establish causal relationships between apolipoprotein levels and DR prevalence. It remains unclear whether elevated apolipoprotein levels increase the risk of DR or whether DR itself leads to changes in apolipoprotein levels. To address these limitations, future research should include prospective studies with larger sample populations. Such studies should incorporate additional confounding variables, utilize more precise definitions of menopausal status based on hormonal levels, and explore the causal pathways between apolipoprotein levels and DR development.
Conclusion
Apolipoprotein levels and menopausal status are significant factors influencing the prevalence of DR in women with T2DM. Apolipoproteins independently affect DR, while their interaction with menopausal status also plays a critical role. Regression models that include these interaction effects demonstrate superior fit and predictive efficiency compared to models without interactions, particularly in predicting PDR. These findings underscore the importance of incorporating apolipoproteins and menopausal status into risk assessment models for DR. They provide valuable insights for early diagnosis and timely intervention, potentially improving outcomes for women with T2DM.
Data availability
All relevant data are included in the papers. Contact to corresponding author for additional information regarding data access.
Abbreviations
- apoA:
-
Apolipoprotein A
- apoB:
-
Apolipoprotein B
- AUC:
-
Area under the receiver operating characteristic curve
- CI:
-
Confidence interval
- DBP:
-
Diastolic blood pressure
- DM:
-
Diabetes mellitus
- DR:
-
Diabetic retinopathy
- HDL:
-
High-density lipoprotein
- HbA1c:
-
Hemoglobin A1c
- ICDR:
-
International clinical diabetic retinopathy
- IQR:
-
Inter-quartile range
- LDL:
-
Low-density lipoprotein
- Lpa:
-
Lipoprotein (a)
- NDR:
-
Non-diabetic retinopathy
- OCTA:
-
Optical coherence tomography angiography
- OR:
-
Odds ratio
- RGCs:
-
Retinal ganglion cells
- ROC:
-
Receiver operator characteristic
- ROS:
-
Reactive oxygen species
- SBP:
-
Systolic blood pressure
- SD:
-
Standard deviation
- T2DM:
-
Type II diabetes mellitus
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
References
Zhuang, X. et al. Association of diabetic retinopathy and diabetic macular oedema with renal function in Southern Chinese patients with type 2 diabetes mellitus: a single-centre observational study. BMJ Open. 9, e031194. https://doi.org/10.1136/bmjopen-2019-031194 (2019).
Pei, X. et al. Efficacy of artificial intelligence-based screening for diabetic retinopathy in type 2 diabetes mellitus patients. Diabetes Res. Clin. Pract. 184, 109190. https://doi.org/10.1016/j.diabres.2022.109190 (2022).
Zhou, Y., Wang, C., Shi, K. & Yin, X. Relationship between dyslipidemia and diabetic retinopathy: a systematic review and meta-analysis. Medicine 97, e12283. https://doi.org/10.1097/md.0000000000012283 (2018).
International diabetes federation diabetes atlas. 10th Edition [Internet]. Accessed on 13 October 2020. (2021). http://www.diabetesatlas.org/
Yin, L., Zhang, D., Ren, Q., Su, X. & Sun, Z. Prevalence and risk factors of diabetic retinopathy in diabetic patients: A community based cross-sectional study. Medicine 99, e19236. https://doi.org/10.1097/md.0000000000019236 (2020).
Yao, X. et al. Distribution of diabetic retinopathy in diabetes mellitus patients and its association rules with other eye diseases. Sci. Rep. 11, 16993. https://doi.org/10.1038/s41598-021-96438-w (2021).
Jaiswal, M., Schinske, A. & Pop-Busui, R. Lipids and lipid management in diabetes. Best Pract. Res. Clin. Endocrinol. Metab. 28, 325–338. https://doi.org/10.1016/j.beem.2013.12.001 (2014).
Yao, X. et al. Relationship between renal and liver function with diabetic retinopathy in patients with type 2 diabetes mellitus: a study based on cross-sectional data. Sci. Rep. 12, 9363. https://doi.org/10.1038/s41598-022-13164-7 (2022).
Toth, P. P. et al. The impact of serum lipids on risk for microangiopathy in patients with type 2 diabetes mellitus. Cardiovasc. Diabetol. 11, 109. https://doi.org/10.1186/1475-2840-11-109 (2012).
Morton, J. et al. Low HDL cholesterol and the risk of diabetic nephropathy and retinopathy: results of the Advavce study. Diabetes Care. 35, 2201–2206. https://doi.org/10.2337/dc12-0306 (2012).
Jeng, C. J. et al. Diabetic retinopathy in patients with dyslipidemia: development and progression. Ophthalmol. Retina. 2, 38–45. https://doi.org/10.1016/j.oret.2017.05.010 (2018).
Moosaie, F. et al. Lipoprotein(a) and apolipoproteins as predictors for diabetic retinopathy and its severity in adults with type 2 diabetes: a case-cohort study. Can. J. Diabetes. 44, 414–421. https://doi.org/10.1016/j.jcjd.2020.01.007 (2020).
Hammer, S. S. & Busik, J. V. The role of dyslipidemia in diabetic retinopathy. Vis. Res. 139, 228–236. https://doi.org/10.1016/j.visres.2017.04.010 (2017).
Li, H. L., Hao, S. F. & Pei, P. P. Correlation between dyslipidemia and diabetic retinopathy in diabetic patients aged 80 years and over. Chin. J. Geriatr. 37, 1376–1378. https://doi.org/10.3760/cma.j.issn.0254-9026.2018.12.020 (2018).
Liu, Y. J., Wang, J. M., Zeng, D. Y. & Yan, P. H. Clinical significance of serum lipids, lipoproteins and apolipoproteins in the patients with coronary heart disease. Chin. J. Hemorheol.. 15, 662–664. https://doi.org/10.3969/j.issn.1009-881X.2005.04.064 (2005).
Marais, A. D. Apolipoprotein E in lipoprotein metabolism, health and cardiovascular disease. Pathology 51, 165–176. https://doi.org/10.1016/j.pathol.2018.11.002 (2019).
Ko, S. H. & Kim, H. S. Menopause-associated lipid metabolic disorders and foods beneficial for postmenopausal women. Nutrients 12, 202. https://doi.org/10.3390/nu12010202 (2020).
Hao, M. et al. Estrogen prevents high-glucose-induced damage of retinal ganglion cells via mitochondrial pathway. Graefe’s Archive Clin. Experimental Ophthalmol. = Albrecht Von Graefes Archiv fur Klinische Und Experimentelle Ophthalmologie. 253, 83–90. https://doi.org/10.1007/s00417-014-2771-7 (2015).
Anagnostis, P. et al. Menopause symptom management in women with dyslipidemias: an EMAS clinical guide. Maturitas 135, 82–88. https://doi.org/10.1016/j.maturitas.2020.03.007 (2020).
Hajian-Tilaki, K. Sample size Estimation in diagnostic test studies of biomedical informatics. J. Biomed. Inform. 48, 193–204. https://doi.org/10.1016/j.jbi.2014.02.013 (2014).
Wilkinson, C. P. et al. Proposed international clinical diabetic retinopathy and diabetic macular edema disease severity scales. Ophthalmology 110, 1677–1682. https://doi.org/10.1016/s0161-6420(03)00475-5 (2003).
National Comprehensive Cancer Network: Clinical Practice Guidelines in Oncology (NCCN guidelines). https://www2.tri-kobe.org/nccn/guideline/breast/english/breast.pdf
Mahley, R. W., Innerarity, T. L., Rall, S. C. Jr. & Weisgraber, K. H. Plasma lipoproteins: apolipoprotein structure and function. J. Lipid Res. 25, 1277–1294 (1984).
Gursky, O. Apolipoprotein structure and dynamics. Curr. Opin. Lipidol. 16, 287–294. https://doi.org/10.1097/01.mol.0000169348.61191.ac (2005).
Cheung, N., Mitchell, P. & Wong, T. Y. Diabetic retinopathy. Lancet (London England). 376, 124–136. https://doi.org/10.1016/s0140-6736(09)62124-3 (2010).
Heng, L. Z. et al. Diabetic retinopathy: pathogenesis, clinical grading, management and future developments. Diabet. Med. J. Br. Diabet. Assoc.. 30, 640–650. https://doi.org/10.1111/dme.12089 (2013).
Xie, J. et al. Association of diabetic macular edema and proliferative diabetic retinopathy with cardiovascular disease: a systematic review and meta-analysis. JAMA Ophthalmol. 135, 586–593. https://doi.org/10.1001/jamaophthalmol.2017.0988 (2017).
Cheung, N. et al. Diabetic retinopathy and the risk of coronary heart disease: the atherosclerosis risk in communities study. Diabetes Care. 30, 1742–1746. https://doi.org/10.2337/dc07-0264 (2007).
Ankit, B. S., Mathur, G., Agrawal, R. P. & Mathur, K. C. Stronger relationship of serum Apolipoprotein A-1 and B with diabetic retinopathy than traditional lipids. Indian J. Endocrinol. Metabol. 21, 102–105. https://doi.org/10.4103/2230-8210.196030 (2017).
Zhang, Q. et al. Relationship between serum apolipoproteins levels and retinopathy risk in subjects with type 2 diabetes mellitus. Acta Diabetol. 55, 681–689. https://doi.org/10.1007/s00592-018-1136-9 (2018).
Acknowledgements
We thank all the members of our study team for their whole-hearted cooperation and the study participants for their contribution to the research.
Funding
This work was supported by the Ministry of Science and Technology of the Peoples Republic of China [grant number 2018YFC0114500]; Henan Provincial Medical Science and Technology Research Joint Co-construction Project [grant number LHGJ20220085]; the Basic Science Project of Henan Eye Institute/Henan Eye Hospital [grant number 22JCQN004 and 21JCZD001]; and National Natural Science Foundation of China [grant number 81470603].
Author information
Authors and Affiliations
Contributions
ZL and XP contributed to the conception of the study. XP and XY contributed to the data interpretation, data analysis, and manuscript writing. DQ, YY and SF contributed to the data collection. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study followed the Declaration of Helsinki and was approved by the Ethics Committee of Henan Provincial People’s Hospital [ethical approval code: HNEECKY-2022(22)]. All patients were informed of the purpose and content of this study, and each one provided informed consent before being included in the study.
Consent for publication
All authors have consent for publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pei, X., Yao, X., Qi, D. et al. Apolipoprotein and menopausal status are significant influencing factors for diabetic retinopathy in type II diabetes mellitus women. Sci Rep 15, 8868 (2025). https://doi.org/10.1038/s41598-025-93161-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-93161-8