Abstract
Contemporary classification of hypertrophic cardiomyopathy (HCM) was mainly based on the site of myocardial hypertrophy and left ventricular outflow tract obstruction. A complementary classification based on left ventricular function could provide a powerful tool to identify individuals with high risk of adverse cardiovascular outcomes and guide individualized managements. Multi-dimensional echocardiographic parameters of left ventricular function derived from conventional echocardiography, tissue Doppler imaging, and speckle tracking echocardiography were obtained in 266 HCM patients and 169 healthy controls (HCs). According to these parameters, HCM subtypes were calculated by principal component analysis and unsupervised cluster analysis. Variables of different groups were compared. The prognosis between HCM subtypes were evaluated. There were two HCM subtypes generated, subtype 1 HCMs (n = 123) and subtype 2 HCMs (n = 143). Compared to HCs, left ventricular diastolic and systolic function were significantly declined to varying degrees in both subtype 1 HCMs and subtype 2 HCMs, especially in subtype 1 HCMs (all P value < 0.001). Subtype 1 HCMs characterized as increased LAVI and E/E′, decreased mean E′ and untwist rate, increased global and segmental longitudinal strains, circumferential strains and radial strains, decreased rotation degree, twist degree, and twist rate, in comparison with subtype 2 HCMs (all P value < 0.001). Notably, subtype 1 HCMs were more susceptible to adverse prognosis of atrial fibrillation (HR: 4.34; 95% CI 1.08–17.53; P value: 0.039). Collectively, we stratified HCM patients into two subtypes with different diastolic and systolic performance and risk of atrial fibrillation. This complementary classification might eventually help to target management of HCM patients who would benefit most.
Similar content being viewed by others
Introduction
Hypertrophic cardiomyopathy (HCM) was the most common myocardial disease, affecting 0.2–0.5% of the population worldwide1. Up to 30% to 40% HCM patients would experience adverse outcomes2. Left ventricular hypertrophy, myocardial hypercontractility, reduced compliance, myofibrillar disarray, and fibrosis could be observed in the hearts of HCM patients3,4. Symptomatic HCM patients often experienced heterogenous phenotypic manifestations, such as shortness of breath, especially with physical exertion, atrial fibrillation, chest pain, syncope, dizziness and sudden cardiac death5.
With the development of clinical and molecular research, especially the promotion of family pedigree screening and the implementation of more sensitive cardiac imaging diagnosis, asymptomatic HCM patients were often disclosed during treatments for other disease and routinely medical examination6,7. As the population of HCM patients gradually expanded, so had their unmet medical needs. The overall principle of HCM treatment was to reduce symptoms, improve cardiac function, and delay disease progression8. As novel pharmacotherapies targeting the molecular underpinnings of HCM emerged, assessment of both asymptomatic and symptomatic HCM patients needed to be updated9,10.
Among the many modalities, echocardiography was widely utilized in clinical practice as the most common initial tests recommended by guidelines for patients with suspected HCM11,12. Multi-dimensional echocardiographic parameters, such as diastolic and systolic velocities of mitral annulus, global longitudinal strain, twist mechanics, and so on, had refined our understanding of mechanisms of left ventricular dysfunction, and emerged as sensitive methods to noninvassively assess left ventricular function13,14. Our study made full use of multi-dimensional echocardiographic parameters in the evaluation of HCM patients in the hope of describing a broad group of HCM patients who were actually characterized by different clinical, pathophysiological, and prognostic characteristics.
Clustering, also known as cluster analysis, was an unsupervised machine learning technique that could explore naturally occurring groups and group data points together based on their similarities15. Since classification was performed by the clustering algorithms, not by humans16. To date, attempts to describe disease heterogeneity in HCM patients by cluster algorithms had been limited to the analysis of clinical variables17. Easy and objective identification of this heterogeneity through multi-dimensional echocardiographic parameters could assist in identifying, within the broad HCM classification, patients with different risk profile.
In this study, we utilized unsupervised cluster analysis to identify and validate complementary classification of HCM by exploring and exploiting multi-dimensional echocardiographic parameters of left ventricular function. We identified echocardiographic markers that enabled a delineation of HCM into complementary subtypes with different degree of left ventricular dysfunction and risk profile. Specially, we evaluated the prognostic value across the identified complementary subtypes of HCM. Our study provided innovative risk stratification strategy and new decision point for therapy.
Materials and methods
Study population
The study included a total of 435 participants consisting of 266 HCM patients and 169 healthy controls (HCs), who were recruited from the inpatient and outpatient services of the People’s Hospital of China Medical University and the First Affiliated Hospital of China Medical University, and the local community at Shenyang, from July 2017 to June 2023. Inclusion criteria were echocardiographic evidence of left ventricular hypertrophy defined as a diastolic maximum wall thickness ≥ 15 mm or ≥ 13 mm in case of a first-degree relative with HCM, in the absence of other cardiac or systemic diseases that could account for the observed hypertrophy18. Exclusion criteria were as follows: (1) poor acoustic windows; (2) history of atrial fibrillation or atrial fibrillation status; (3) history of myocardial infarction or coronary artery disease; (4) history of septal myectomy or alcoholic septal ablation; and (5) impaired renal function, or metallic implants. Age- and sex-matched HCs were included, who had no evidence or no family history of HCM, hypertension, diabetes mellitus, or any other disease. The study was approved by the Institutional Review Board of the People’s Hospital of China Medical University or the First Affiliated Hospital of China Medical University. All participants provided written informed consent after receiving a detailed description of the study and all experiments were performed in accordance with relevant guidelines and regulations.
Clinical variables
The clinical examinations consisted of standardized questionnaires, physical examinations and laboratory examinations. The questionnaire included age, sex, smoking, alcohol consumption, family medication history, and self-reported health status. Smokers were defined as having smoked at least one cigarette per day for more than one year. Drinkers were defined as having consumed at least one alcoholic beverage a day for a minimum period of six months. The physical examinations included measurements of height, weight, body mass index (BMI), body surface area (BSA), systolic blood pressure (SBP), diastolic blood pressure (DBP), and 12-lead electrocardiogram. The laboratory examinations included total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL), low-density lipoprotein cholesterol (LDL), fasting blood glucose (FBG), 2 h blood glucose (2hBG), glycosylated hemoglobin Alc (HbAlc), serum creatinine (Cr), serum urea nitrogen (UN), serum uric acid (UA), serum alanine aminotransferase (ALT), serum aspartate aminotransferase (AST), free triiodothyronine (FT3), free thyroxine (FT4), thyroid-stimulating hormone (TSH), cardiac troponin T (cTNT), and N-terminal pro-brain natriuretic peptide (NT-proBNP).
Echocardiographic parameters
For each subject, conventional and advanced echocardiography were recorded with a Vivid 7 Dimension ultrasound system (GE Healthcare, Waukesha, WI) using the protocol of American Society of Echocardiography19. Conventional echocardiographic parameters included left ventricle end-diastolic dimension (LVEDD), left ventricle end-systolic dimension (LVESD), left ventricular ejection fraction (LVEF), maximum wall thickness (MWT), left ventricular mass index (LVMI), left ventricular outflow tract obstruction (LVOTO), left ventricular outflow tract obstruction peak gradient at rest (LVOTG), left atrial volume (LAV), derived LAV index (LAVI) (LAVI = LAV/BSA), peak early and late diastolic mitral inflow velocities (E and A), and derived E/A ratio. According to the echocardiographic morphology, there were three HCM types, including septal hypertrophy, apical hypertrophy, and mixed hypertrophy. Tissue Doppler imaging parameters included early diastolic velocities (E′), late diastolic velocities (A′), and systolic velocities (S′) of mitral annulus from both posterior septal and lateral sides. Mean E′, mean A′, mean S′ and E/E′ values were calculated. Speckle tracking echocardiographic parameters included left ventricular strains and twist mechanics which were generated from collected echocardiography cine clips after post-processing on professional software provided by GE Healthcare. Strains included global and segmental longitudinal strains, circumferential strains, and radial strains. Twist mechanics included segmental rotations, twist degree, peak twist rate in systolic phase and peak untwist rate in early and late diastolic phase20.
Adverse cardiovascular outcomes
After study enrollment, HCM patients were evaluated every six months. At each visit, adverse cardiovascular outcomes were documented and assessed, which included atrial fibrillation, heart failure, stroke, syncope, and cardiovascular hospitalization. Enrollment date was defined as the first visit to the outpatient clinic. Follow-up surveys were taken up for two and a half years. Follow-up surveys were completed in 113 HCM patients. The missing follow-up HCM patients were due to out of contact and refusal to our follow-up after multiple contacts.
Unsupervised clustering
Eleven variables representing left ventricular function, including LAVI, E/E′, E′, S′, A′, global longitudinal strain, global circumferential strain, global radial strain, twist degree, twist rate, untwist rate were identified for cluster analysis. Generally, K-means clustering and principal component analysis (PCA) were applied to identify potential subtypes of interest21. K-means clustering was one of the simplest and popular unsupervised machine learning algorithms to partition a given data set into a set of K clusters effectively15. The HCM patients with a similar diastolic and systolic function pattern could group into the same cluster. Moreover, PCA was the main linear technique for dimensionality reduction, in order to simplify visual inspection of multivariate data by a linear transformation of data from high dimensional space into a low dimensional space that still retained the meaningful properties of the original data. The clustering workflows were described as below.
First, data normalization: Z-score normalization was used to transform data from multiple features to the same scale. It was calculated by subtracting the mean value for each field from the values of the file and then dividing by the standard deviation of the field. Second, K-means clustering: K-means clusters were specified as k = 2 to ensure that there were a reasonable number of HCM patients within each cluster for interpretability. Meanwhile, the iteration was set as ten. The HCM patients were randomly clustered into the defined clusters until a local minimum was found by using the Euclidean sum of squares as a descriptor. Third, PCA: PCA was used to convert high dimensional data to three-dimensional data (the first three principal components). Then PCA results were presented in an interactive 3D scatterplot. Z-score normalization, K-means clustering and PCA were carried out using Python 3.7.
Statistical analysis
Statistical analysis was performed using SPSS statistics 23.0 (SPSS Inc., Chicago, IL). Categorical variables were expressed as counts (n) and percentages (%) and continuous variables as mean and standard deviation (SD) whenever appropriate. Between-group differences of continuous variables among HCM subtypes and HCs were compared by one-way analysis of variance (ANOVA) followed by least significant difference (LSD) post-hoc test. Categorical variables were compared using the chi-square test (χ2) test. To further evaluate the prognostic and discriminative utility of the HCM subtypes, Kaplan–Meier curves were plotted with the duration from the enrollment to the last follow-up or adverse cardiovascular outcomes and compared with the log-rank test. Cox proportional hazard analysis was performed to evaluate the association between the adverse cardiovascular outcomes and the HCM subtypes, with or without adjusting by basic characteristics (age and sex). A P value less than 0.05 was considered statistically significant.
Results
Identified subtypes
The ensemble cluster analysis identified two subtypes in HCM patients (n = 266) (Fig. 1). Subtype 1 included 123 HCM patients (Subtype 1 HCMs), and Subtype 2 included 143 HCM patients (Subtype 2 HCMs). Clinical variables according to subtypes were shown in Table 1. The levels of cTNT and NT-proBNP were significantly different among Subtype 1 HCMs, Subtype 2 HCMs and HCs (P = 0.049 and P = 0.018, respectively). Compare to HCs, Subtype 1 HCMs showed significant higher levels of cTNT and NT-proBNP (P = 0.015 and P = 0.005, respectively). There was no significant difference among Subtype 1 HCMs, Subtype 2 HCMs and HCs in demographic characteristics, physical variables, blood sugar, blood lipid, liver function, kidney function, and thyroid function (all P value > 0.05).
There were significant differentces among Subtype 1 HCMs, Subtype 2 HCMs and HCs in the conventional parameters of echocardiography, including LVEDD, MWT, LVMI, LVOTO, and E (all P value < 0.001). Compared to HCs, Subtype 1 HCMs and Subtype 2 HCMs showed significant smaller LVEDD, thicker MWT, higher LVMI, and lower E (all P value < 0.001). However, there was no significant difference between Subtype 1 HCMs and Subtype 2 HCMs in the above parameters (all P value > 0.05). In addition, no statistical differences of LVOTO and LVOTG were observed between Subtype 1 HCMs and Subtype 2 HCMs (all P value > 0.05), as well as morphological types of HCM (all P value > 0.05).
Subtype-related diastolic function alterations
There was significant difference in diastolic function among Subtype 1 HCMs, Subtype 2 HCMs and HCs (all P value < 0.001) (Table 2). Subtype 1 HCMs had the most severe diastolic dysfunction, expressed as the highest LAVI value and E/E′ ratio, and the lowest mean E′ and A′ value compared to Subtype 2 HCMs and HCs (all P value < 0.001). Subtype 2 HCMs had moderate diastolic dysfunction as the higher LAVI value and E/E′ ratio, and the lower mean E′ value compared to HCs (all P value < 0.001). The detailed data were illustrated in Table 2.
Subtype-related systolic function alterations
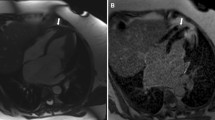
There was significant difference in systolic function among Subtype 1 HCMs, Subtype 2 HCMs and HCs (all P value < 0.001). Subtype 1 HCMs had the most severe systolic dysfunction, characterized as the lowest global and segmental longitudinal strains, circumferential strains, and radial strains, as well as the disturbed twist mechanics, including the lowest segmental rotation degree in the basal, middle, and apical levels, twist degree, peak twist rate and peak untwist rate compared to Subtype 2 HCMs and HCs (all P value < 0.05). Moreover, compared to HCs, Subtype 2 HCMs had moderate systolic dysfunction as lower global and segmental longitudinal strains, circumferential strains, and radial strains, and reduced twist mechanics as lower segmental rotation degree in basal, middle, and apical levels, and lower twist degree (all P value < 0.05) (Figs. 2 and Fig. 3). The detailed data were illustrated in Table 3 and Table S1.
Distinct strain patterns of subtype 1 HCMs, subtype 2 HCMs and HCs. (A) Longitudinal strain pattern of subtype 1 HCMs, subtype 2 HCMs and HCs. (B) Circumferential strain pattern of subtype 1 HCMs, subtype 2 HCMs and HCs. (C) Radial strain pattern of subtype 1 HCMs, subtype 2 HCMs and HCs. This figure represented the distribution of mean strain value in different myocardial segments. The darker the color was, the larger its absolute value was. HCMs, patients with hypertrophic cardiomyopathy; HCs, healthy controls.
Distinct twist mechanics patterns of subtype 1 HCMs, subtype 2 HCMs and HCs. (A) Rotation pattern of subtype 1 HCMs, subtype 2 HCMs and HCs. (B) twist degree pattern, twist rate pattern and untwist rate pattern of subtype 1 HCMs, subtype 2 HCMs and HCs. This figure represented the distribution of mean twist mechanics value in different myocardial segments. The darker the color was, the larger its absolute value was. HCMs, patients with hypertrophic cardiomyopathy; HCs, healthy controls.
Subtype-related adverse cardiovascular outcomes
Follow-up data were available for 113 of the 266 (42.48%) HCM patients included in the cluster analysis (follow-up duration: 30 months, interquartile range: 6–30 months). The composite endpoint occurred in 31 patients (27.43%), including nine atrial fibrillation (7.96%), seven heart failure (6.19%), four stroke (3.54%), four syncope (3.54%), and seven cardiovascular hospitalization (6.19%). As shown in Fig. 4, survival analysis found a trend toward statistical significance in adverse cardiovascular outcomes between Subtype 1 HCMs and Subtype 2 HCMs (log-rank P-value = 0.093) (Table S2). Moreover, it showed that there was significant difference in atrial fibrillation between Subtype 1 HCMs and Subtype 2 HCMs (log-rank P-value = 0.022). Using Cox proportional hazards modeling, Subtype 1 HCMs were more like to suffer from atrial fibrillation compared to Subtype 2 HCMs after adjusting for age and sex (HR: 4.34; 95% CI 1.08–17.53; P-value: 0.039) (Table 4).
Discussion
The widely used clinical classification of HCM was mainly based on hemodynamic characteristics and the site of myocardial hypertrophy3. Periodic risk stratification for HCM related sudden cardiac death was carried out clinically22,23. However, there were still lack of well established protocols for risk assessment of adverse cardiovascular outcomes in HCM patients. There was a pressing need for a HCM classification that could distinguish patients with higher risk of adverse cardiovascular outcomes. To our knowledge, this was the first application of cluster analysis in disclosing classification of HCM patients according to multi-dimensional echocardiographic parameters of left ventricular function other than demographic characteristics and clinical variables. Our study achieved a binary classification of HCM mainly featured with different cardiac diastolic and systolic dysfunction, myocardial mechanic disorder and susceptibility of atrial fibrillation.
In this study, we successfully found two complementary subtypes of HCM based on data-driven cluster analysis, which was quantified by multi-dimensional echocardiographic parameters, from conventional echocardiography, tissue Doppler imaging, and speckle tracking echocardiography. The two subtypes mainly differed in left ventricular diastolic and systolic function featured by E′, E/E′, LAVI, longitudinal strain, circumferential strain, radial strain, rotation and twist parameters. Subtype 1 HCMs demonstrated poorer left ventricular diastolic and systolic function compared to subtype 2 HCMs. However, demographic characteristics, physical variables, blood sugar, blood lipid, liver function, kidney function, and thyroid function showed no significant difference. As conventional echocardiographic parameters could hardly fully represent left ventricular function, multi-dimensional echocardiographic parameters, like E′ and E/E′ in tissue Doppler imaging, longitudinal strain, circumferential strain, radial strain, rotation and twist in speckle tracking echocardiography, were introduced to quantify myocardial reflexation and contraction24. A few researchers showed that E′ and E/E′ were associated with worse prognosis in HCM patients25. Moreover, they also pointed out that there were a close correlation of abnormal regional and global strains, myocardial fibrosis, and myocardial contraction in HCM patients26,27,28.
Our study could well distinguish HCM patients who were susceptive to atrial fibrillation with specific echocardiographic characteristics. Atrial fibrillation was the most common sustained tachyarrhythmia in HCM patients, and had been regarded as a turning point of living status and prognosis when effective atrial fibrillation management strategies were not available. Approximately 20% of HCM patients could develop atrial fibrillation mostly in their fifties. It was well established that age, BMI, height, hypertension, diabetes, obstructive sleep apnea, myocardial infarction, heart failure, and smoking were risk factors for atrial fibrillation development and perpetuation29,30,31. Elevated filling pressure due to left ventricular diastolic dysfunction, myocardial hypertrophy, mitral regurgitation and left ventricular outflow tract obstruction was fully acknowledged determinant of left atrial enlargement in HCM clinical course32,33. In the meantime, myocardial fibrosis also contributed to left atrial enlargement and functional impairment. Previous researcheres had pointed out that increased left atrial volume could lead to increased risk of atrial fibrillation34. This was consistent with our study. In our study, no significant difference was noticed among subtype 1 HCMs, subtype 2 HCMs and HCs in demographic characteristics, physical variables, blood sugar, blood lipid, liver function, kidney function, and thyroid function. It was reasonable to conclude that left atrial size and echocardiographic parameters were better biological markers of atrial fibrillation risk assessment in HCM patients.
For the first time, our study conducted cluster analysis using a large number of noninvasive multi-dimensional echocardiographic parameters of HCM patients. Contemporary risk stratification for HCM patients mainly focused on sudden cardiac death and syncope22,35. Moreover, contemporary stratification strategy of atrial fibrillation in HCM patients exhibited not enough concordance for clinical practice. The findings of our study could help to fill a gap in this area, and to identify HCM patients at risk for atrial fibrillation quantitatively. We also achieved in utilizing an unbiased approach to find out existed, distinct, and mutually independent patient clusters that could be used for individualized HCM management36,37.
There were several limitations in our study. First, deformation parameters were afterload dependent. Follow-up studies should introduce afterload independent parameters, such as myocardial work, to differentiate abnormal parameters resulting from systolic dysfunction and abnormal parameters resulting from abnormal afterload. Second, the relative small sample size, especially of the follow-up HCM patients, was a drawback of our study. Multicenter, longitudinal studies with larger sample size should be conducted in order to reveal the correlations of the strain, rotation, and twisting patterns and morphorlogical types of HCM in Subtype 1 HCMs and Subtyper 2 HCMs. Our cohort enrolled relatively fewer patients with severe LVOT obstruction. For further enhancement of this model, more severe obstructive patients should be recruited in subsequent studies. Meanwhile more detailed follow-up should be pay more attention in the furure. Third, all HCM patients in this study didn’t experience cardiac MRI screening, which forbad us to analyze the cardiac structure with fibrosis in detail. Last, most data of HCM patients were recorded in rest. Further studies should be pay more attention to provocative data, especially in LVOTO and LVOTG.
As far as we know, this was the first complementary classification of HCM patients utilizing multi-dimensional echocardiographic parameters of left ventricular function, not only conventional echocardiographic measurements, tissue Doppler imaging data, but also speckle tracking echocardiographic assessments. This classification was composed of two clinically meaningful subtypes with significant differences in diastolic and systolic dysfunction. Notably, the complementary classification could well distinguish HCM patients with adverse cardiovascular outcome of atrial fibrillation. Our study could lead to new target of HCM managements. Moreover, our study could help in design and execution of clinical trials of HCM patients.
Data availability
The data underlying this article cannot be shared publicly due to the privacy of individuals that participated in the study. The data used and/or analysed during the current study will be available from the corresponding author on reasonable request.
References
Maron, B. J. & Maron, M. S. Hypertrophic cardiomyopathy. Lancet 381, 242–255. https://doi.org/10.1016/S0140-6736(12)60397-3 (2013).
Ommen, S. R. et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: A report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation 142, e558–e631. https://doi.org/10.1161/CIR.0000000000000937 (2020).
Teekakirikul, P., Zhu, W., Huang, H. C. & Fung, E. Hypertrophic cardiomyopathy: An overview of genetics and management. Biomolecules 9, 878. https://doi.org/10.3390/biom9120878 (2019).
Maron, B. J. et al. Diagnosis and evaluation of hypertrophic cardiomyopathy: JACC state-of-the-art review. J. Am. Coll. Cardiol. 79, 372–389. https://doi.org/10.1016/j.jacc.2021.12.002 (2022).
Muresan, I. D. & Agoston-Coldea, L. Phenotypes of hypertrophic cardiomyopathy: Genetics, clinics, and modular imaging. Heart Fail. Rev. 26, 1023–1036. https://doi.org/10.1007/s10741-020-09931-1 (2021).
Melas, M., Beltsios, E. T., Adamou, A., Koumarelas, K. & McBride, K. L. Molecular diagnosis of hypertrophic cardiomyopathy (HCM): In the heart of cardiac disease. J. Clin. Med. 12, 225. https://doi.org/10.3390/jcm12010225 (2022).
Chung, H. & Choi, E. Y. multimodality imaging in patients with hypertrophic cardiomyopathy and atrial fibrillation. Diagnostics 13, 3049. https://doi.org/10.3390/diagnostics13193049 (2023).
Ommen, S. R. & Semsarian, C. Hypertrophic cardiomyopathy: A practical approach to guideline directed management. Lancet 398, 2102–2108. https://doi.org/10.1016/S0140-6736(21)01205-8 (2021).
DeVries, J. H., Irs, A. & Hillege, H. L. The European Medicines Agency assessment of mavacamten as treatment of symptomatic obstructive hypertrophic cardiomyopathy in adult patients. Eur. Heart J. 44, 3492–3494. https://doi.org/10.1093/eurheartj/ehad429 (2023).
Kawana, M., Spudich, J. A. & Ruppel, K. M. Hypertrophic cardiomyopathy: Mutations to mechanisms to therapies. Front. Physiol. 13, 975076. https://doi.org/10.3389/fphys.2022.975076 (2022).
Arbelo, E. et al. 2023 ESC guidelines for the management of cardiomyopathies. Eur. Heart J. 44, 3503–3626. https://doi.org/10.1093/eurheartj/ehad194 (2023).
Kitai, T. et al. Contemporary diagnosis and management of hypertrophic cardiomyopathy: The role of echocardiography and multimodality imaging. J. Cardiovasc. Dev. Dis. https://doi.org/10.3390/jcdd9060169 (2022).
Desai, M. Y. et al. LV global function index provides incremental prognostic value over LGE and LV GLS in HCM. JACC Cardiovasc Imaging 13, 2052–2054. https://doi.org/10.1016/j.jcmg.2020.03.023 (2020).
Finocchiaro, G. et al. Role of Doppler diastolic parameters in differentiating physiological left ventricular hypertrophy from hypertrophic cardiomyopathy. J. Am. Soc. Echocardiogr. 31, 606–613. https://doi.org/10.1016/j.echo.2017.11.022 (2018).
Jaeger, A. & Banks, D. Cluster analysis: A modern statistical review. Wiley Interdiscip. Rev. Comput. Stat. 15, e1597 (2023).
Loftus, T. J. et al. Phenotype clustering in health care: A narrative review for clinicians. Front. Artif. Intell. 5, 842306. https://doi.org/10.3389/frai.2022.842306 (2022).
Hourqueig, M. et al. Hypertrophic cardiomyopathies requiring more monitoring for less atrial fibrillation-related complications: A clustering analysis based on the French registry on hypertrophic cardiomyopathy (REMY). Clin. Res. Cardiol. 111, 163–174. https://doi.org/10.1007/s00392-020-01797-5 (2022).
Lancellotti, P. et al. Cardiovascular imaging practice in Europe: A report from the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 16, 697–702. https://doi.org/10.1093/ehjci/jev116 (2015).
Nagueh, S. F. et al. American society of echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with hypertrophic cardiomyopathy: Endorsed by the American society of nuclear cardiology, society for cardiovascular magnetic resonance, and society of cardiovascular computed tomography. J. Am. Soc. Echocardiogr. 24, 473–498. https://doi.org/10.1016/j.echo.2011.03.006 (2011).
Dorobantu, D. M. et al. The Role of Speckle Tracking Echocardiography in the Evaluation of Common Inherited Cardiomyopathies in Children and Adolescents: A Systematic Review. Diagnostics 11, 635. https://doi.org/10.3390/diagnostics11040635 (2021).
Greenacre, M. et al. Principal component analysis. Nat. Rev. Methods Prim. 2, 100 (2022).
Maron, B. J., Rowin, E. J. & Maron, M. S. Evolution of risk stratification and sudden death prevention in hypertrophic cardiomyopathy: Twenty years with the implantable cardioverter-defibrillator. Heart Rhythm 18, 1012–1023. https://doi.org/10.1016/j.hrthm.2021.01.019 (2021).
Al Samarraie, A., Petzl, A., Cadrin-Tourigny, J. & Tadros, R. Sudden death risk assessment in hypertrophic cardiomyopathy across the lifespan: Reconciling the American and European approaches. Card. Electrophysiol. Clin. 15, 367–378. https://doi.org/10.1016/j.ccep.2023.04.010 (2023).
Modesto, K. & Sengupta, P. P. Myocardial mechanics in cardiomyopathies. Prog. Cardiovasc. Dis. 57, 111–124. https://doi.org/10.1016/j.pcad.2014.03.003 (2014).
Lu, D. Y. et al. E/e′ ratio and outcome prediction in hypertrophic cardiomyopathy: The influence of outflow tract obstruction. Eur. Heart J. Cardiovasc. Imaging 19, 101–107. https://doi.org/10.1093/ehjci/jex134 (2018).
Almaas, V. M. et al. Noninvasive assessment of myocardial fibrosis in patients with obstructive hypertrophic cardiomyopathy. Heart 100, 631–638. https://doi.org/10.1136/heartjnl-2013-304923 (2014).
Yang, Y., Wu, D., Wang, H. & Wang, Y. Prognostic value of global longitudinal strain in hypertrophic cardiomyopathy: A systematic review and meta-analysis. Clin. Cardiol. 45, 1184–1191. https://doi.org/10.1002/clc.23928 (2022).
Saito, M. et al. Clinical significance of global two-dimensional strain as a surrogate parameter of myocardial fibrosis and cardiac events in patients with hypertrophic cardiomyopathy. Eur. Heart J. Cardiovasc. Imaging 13, 617–623. https://doi.org/10.1093/ejechocard/jer318 (2012).
Garg, L. et al. Atrial fibrillation in hypertrophic cardiomyopathy: Prevalence, clinical impact, and management. Heart Fail. Rev. 24, 189–197. https://doi.org/10.1007/s10741-018-9752-6 (2019).
Kramer, C. M. et al. Predictors of major atrial fibrillation endpoints in the national heart, lung, and blood institute HCMR. JACC Clin. Electrophysiol. 7, 1376–1386. https://doi.org/10.1016/j.jacep.2021.04.004 (2021).
Rowin, E. J., Link, M. S., Maron, M. S. & Maron, B. J. Evolving contemporary management of atrial fibrillation in hypertrophic cardiomyopathy. Circulation 148, 1797–1811. https://doi.org/10.1161/CIRCULATIONAHA.123.065037 (2023).
Philipson, D. J., Rader, F. & Siegel, R. J. Risk factors for atrial fibrillation in hypertrophic cardiomyopathy. Eur. J. Prev. Cardiol. 28, 658–665. https://doi.org/10.1177/2047487319828474 (2021).
Veselka, J., Anavekar, N. S. & Charron, P. Hypertrophic obstructive cardiomyopathy. Lancet 389, 1253–1267. https://doi.org/10.1016/S0140-6736(16)31321-6 (2017).
Dragasis, S. et al. Atrial fibrillation in hypertrophic cardiomyopathy—A contemporary mini-review. Hell. J. Cardiol. 67, 66–72. https://doi.org/10.1016/j.hjc.2022.05.002 (2022).
Pu, L. et al. Current perspectives of sudden cardiac death management in hypertrophic cardiomyopathy. Heart Fail. Rev. 29, 395–404. https://doi.org/10.1007/s10741-023-10355-w (2024).
Mehra, N., Veselka, J., Smedira, N. & Desai, M. Y. Invasive therapies for symptomatic obstructive hypertrophic cardiomyopathy. Prog. Cardiovasc. Dis. 80, 46–52. https://doi.org/10.1016/j.pcad.2023.08.003 (2023).
Braunwald, E., Saberi, S., Abraham, T. P., Elliott, P. M. & Olivotto, I. Mavacamten: A first-in-class myosin inhibitor for obstructive hypertrophic cardiomyopathy. Eur. Heart J. 44, 4622–4633. https://doi.org/10.1093/eurheartj/ehad637 (2023).
Acknowledgements
The authors thank all the participants for their cooperation and are grateful for the support of Department of Ultrasound, The People’s Hospital of Liaoning Province and Department of Cardiovascular Ultrasound, The First Affiliated Hospital of China Medical University.
Funding
This study was supported by the National Natural Science Foundation of China (82371982), the Shenyang Middle younger Scientific and Technological Innovation Support Plan (RC220223), the Natural Science Foundation of Liaoning Province (2022-MS-078).
Author information
Authors and Affiliations
Contributions
J.Y., D.S. and C.M. designed and conceptualized the study. D.S., X.F., Y.Z. and Z.Z. collected clinical and echocardiographic data. D.S. and X.F. analyzed data and wrote the manuscript. J.Y. revised the manuscript. All authors contributed to data interpretation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sun, D., Fang, X., Zhang, Y. et al. Complementary classification of hypertrophic cardiomyopathy using unsupervised cluster analysis on left ventricular function. Sci Rep 15, 8362 (2025). https://doi.org/10.1038/s41598-025-93202-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-93202-2