Abstract
In maintenance hemodialysis patients, efficient removal of phosphate during the hemodialysis session is crucial for the control of hyperphosphatemia and other frequent abnormalities of mineral metabolism. A mathematical model that integrates different distribution compartments and forms of phosphate may provide deeper insight and elucidation of observed kinetics of phosphate levels in plasma. Three mathematical models were constructed to describe the kinetics of phosphate during a one-week cycle of three dialysis sessions. The models included the extracellular and intracellular compartments for phosphate ions, plasma and interstitial compartments for phosphate ions bound to protein, and a compartment for fast exchangeable phosphate ions, and differing by the presence or exclusion of the fast or the intracellular compartment. The models included also an intracellular store of phosphate that might be released at an increasing rate during dialysis sessions. The weekly kinetics of total phosphate levels in plasma predicted by the three models were similar and agreed with the clinical data. The inclusion of free phosphate ion and protein bound phosphate separately provided small but significant modifications of the predicted profiles. The time dependent release of phosphate from the intracellular store was critical for the correct description of phosphate kinetics in plasma. The hypothesis that a fast compartment and an intracellular store compartment separately or combined contribute significantly to the kinetics of total phosphate in plasma was shown to be compatible with clinical data.
Similar content being viewed by others
Introduction
Disturbances in mineral metabolism associate with increased mortality and cardiovascular events in end stage renal disease patients on dialysis and can necessitate transfer to renal replacement therapies in patients with pre-dialysis chronic kidney disease1,2. The correct mass balance for phosphate may be maintained by diet, phosphate chelators and by dialysis, but many disorders related to mineral metabolism, including bone loss, adynamic bone disease and smooth muscle and vascular calcification, are frequent among patients on dialysis3,4,5.
The kinetics of phosphate during and between dialysis sessions differs from that of other small solutes such as urea and creatinine; however, the reason for these differences is unclear. Typically, phosphate concentration in plasma decreases during the initial two hours of dialysis, then stabilizes or even increases, especially if the session is longer than four hours; after the end of dialysis, the phosphate concentration in plasma quickly rebounds reaching 80% or more of the pretreatment level in 4 – 12 hours6,7,8,9,10,11,12,13. The standard two compartment model for a single dialysis session cannot describe correctly the phosphate kinetics during and after a dialysis session and therefore some authors proposed a specific role of the intracellular compartment6,7,10,13,14, while others focused on the “fast compartment” being likely the fast exchangeable pool of phosphate and calcium related to bone mass15,16,17,18. The removal of phosphate is also an important issue in peritoneal dialysis19,20.
Another specific feature of phosphate kinetics in hemodialysis patients receiving three weekly dialysis sessions is that the initial plasma phosphate concentration before each session is similar despite sessions being unevenly distributed during a one week cycle of dialysis; this is in contrast to other small solutes such as urea and creatinine11,17. This observation suggests tight control of phosphate level in the extracellular compartment.
The kinetics of phosphate ions during dialysis sessions were analyzed previously in clinical studies and by mathematical modeling using a simplified description for a single dialysis session10,15,21,22. The successful application of the so called pseudo one compartment model for standard hemodialysis was extended for its mathematical theory and new test for hemodialysis with close loop dialysate circulation23,24. Recently, measurements of phosphate throughout a one-week cycle of three dialysis sessions enabled a more accurate description of phosphate removal during dialysis by extending the pseudo-one compartment model for phosphate from a single session to a cycle of one week11,17. However, this modeling does not take explicitly into account the mass balance based on intake, removal, generation and distribution of phosphate that should be included into modeling to be able to predict changes in phosphate kinetics with different modes and schedules of dialysis.
Phosphate has a complicated distribution in the body (85% is stored in bones, 14–15% in cells, and less than 1% in the extracellular fluid) and its turnover and plasma levels are regulated by a complex set of processes that makes modeling and tests of the models difficult to perform. For example, Spalding et al. introduced a model that, beside intracellular and extracellular compartments, included two non-specified compartments that release phosphate into extracellular and intracellular compartments if plasma phosphate concentration drops below predefined thresholds; the model was tested for a single hemodialysis session10. Daugirdas proposed a two compartment model with a distal compartment with large distribution volume, two to three times greater than that for urea, and intercompartment clearance dependent on plasma concentration of phosphate13,25,26,27.
The aims of our study were: 1) to formulate a model of phosphate turnover during and between dialysis sessions for the whole weekly dialysis cycle of three sessions with interdialytic breaks of 2–2–3 days11,17, 2) to formulate and theoretically analyze different assumptions involved in the extracellular phosphate control during and between hemodialysis sessions, 3) to compare the kinetics of phosphate during hemodialysis predicted by three different models that are based on different assumptions on the mechanisms of phosphate replenishment in extracellular compartment: Model F, based on the fast phosphate compartment related to the bone phosphate mass; Model IC, based on the exchange of phosphate between extracellular and intracellular phosphate compartments with increased generation of intracellular phosphate during dialysis from an intracellular phosphate pool14,28; and Model F&IC, with both these phosphate replenishment mechanisms taken into account, 4) to provide a description of different forms of phosphate ions in the extracellular compartment such as free ions and protein bound ions, and 5) to assess the impact of different factors on the predicted kinetics of phosphate.
The proposed models go beyond the previous two pool compartment and pseudo one compartment models for phosphate kinetics and the approaches to phosphate kinetics proposed previously12,22,29, and they attempt to take into account detailed observations that were made recently in clinical and animal studies. Some features of the model were derived partly from previous models that were applied for the analysis of long term hormonal control of phosphate plasma levels30,31,32; those models go however beyond the problems related to the weekly oscillations of these ions induced by dialysis. The model was adjusted to provide the weekly profiles of total phosphate ion (inorganic phosphorus) measured in plasma in patients during dialysis11.
The following issues were addressed in this study: 1) The prediction of the profiles of total phosphate concentration in serum during a one-week cycle of dialysis and comparisons with the average measured clinical profiles of the same duration11. 2) The prediction of the profiles of free phosphate ion, and protein bound phosphate in plasma and interstitial fluid, i.e., profiles that are not typically measured during clinical studies. 3) The analysis of the relative impact of the intracellular phosphate compartment vs. fast phosphate compartment on the phosphate profile during dialysis sessions. 4) The impact of a hypothetical intracellular phosphate generation during dialysis on the plasma phosphate profiles in patients on maintenance hemodialysis, i.e., the adjustment and comparison of three models: Model F, Model IC and Model F&IC. 5) The mass balance of the intake and removal of phosphate in patients on hemodialysis.
Methods
Patients and measurements
The protocol of the study, and descriptions of the enrollment, clinical characteristics, treatment, and measurements in the patients, were described previously11,17,18,33,34. In brief, three standard hemodialysis sessions (duration 239 ± 11 min) were monitored in 25 anuric, prevalent hemodialysis patients (age 62.3 ± 14 years, 16 females, dialysis vintage 13.0 ± 9.3 years, body weight 67.8 ± 15.5 kg, total body water 29.0 ± 5.7 L, extracellular water 13.8 ± 2.6 L). All patients had arteriovenous fistulas and arterial blood samples were collected from the fistula before, at 1, 2, and 3 h, at the end and 45 min after each session, and before the fourth dialysis session. Hemodialysis treatments were performed using high-flux dialyzers in 4 patients or low-flux dialyzers in 21 patients with blood flow in the range of 200–360 mL/min, dialysate flow 500 mL/min and mean ultrafiltration rate 10.6 ± 3.5 mL/min. Plasma total phosphate concentration (i.e., inorganic phosphorous) was measured using Advia 1800 (Siemens, Erlangen, Germany). Phosphate chelators were prescribed to all patients with the dose regulated according to plasma phosphate. The volumes of total body water and extracellular water were measured by a Body Composition Monitor (Fresenius, Bad Homburg, Germany) before, at the end, and 45 min after the end of each dialysis session.
This prospective, observational study has been conducted in accordance with the Declaration of Helsinki and applicable rules. The approval for the study was issued by the Bioethical Committee at the Medical University of Lublin (Poland). Written informed consent was obtained from each patient.
Kinetics of phosphate in hemodialysis: content of the model
Assumptions of the model
The models, F, IC and F&IC, have some common features such as phosphate intake and phosphate removal by dialysis. In the models, it is assumed that phosphate is absorbed from the gastrointestinal tract. The amount of absorbed phosphate may be reduced by phosphate chelators, and, because of the lack of detailed data, it is considered in the model as an adjustable parameter. Furthermore, it is assumed that no residual renal clearance is present, in agreement with the patient data11.
The excretory function of the kidneys is replaced by intermittent dialysis therapy. A standard schedule with three hemodialysis sessions per week and interdialytic breaks of 2–2–3 days is assumed. Excess water and solutes are removed during the treatment, but slowly accumulate in the body between the dialysis sessions. There is no phosphate in fresh dialysis fluid. Whereas small amounts of complexes with phosphate ions and small cations are present in body fluids, the precise concentration and distribution is not known; therefore, this form of phosphate is not taken into account in the model. Another form of phosphate, i.e., phosphate ions bound to protein, is assumed not to be removed by dialysis but is expected to be in dynamic equilibrium with the free ion form. The protein bound fraction of phosphate may slightly increase during dialysis because of the drop in the volume of plasma water leading to hemoconcentration of proteins35. Typically, only the concentration of total phosphate (or phosphorus) in plasma is available from clinical and experimental studies11,13.
Changes in the volume of body fluids are taken into account as the ultrafiltration of water from blood during dialysis and the (assumed continuous) intake of fluid that results in the accumulation of water in the extracellular fluid between dialysis sessions. Plasma volume also changes during dialysis because of the ultrafiltration provided by the dialyzer but because of the refilling of water from the extracellular compartment, the change in plasma volume is much lower, about 20% on average, i.e., about 700 mL, in comparison to the total ultrafiltration volume of 1.5 – 3 L. In our model, these processes are described as the net rate of the plasma volume decrease during dialysis and the net rate of replenishment of plasma volume between dialysis sessions.
The transport of phosphate in the dialyzer is described according to the one-dimensional theory of dialyzer with the parameter of clearance according to the clinical data and transmittance coefficient typical for small solutes and ions36,37,38. Protein bound phosphate is not removed directly by hemodialysis.
The models differ by the assumptions regarding the replenishment of phosphate in the extracellular compartment from other possible phosphate pools in the body.
Model F. The phosphate ions in extracellular fluid are in equilibrium with the “fast” compartment, that is the compartment with phosphate that can be quickly transported to plasma if its concentration in plasma decreases, or absorbed from plasma if its concentration in plasma increases15,16,17,18,30,31,32,39. The fast compartment is attributed to a small part of bone that is also in equilibrium with the bone mass of phosphate. In our approach, we do not take into account this last equilibrium as the exchange between fast and bone compartments is slow and is related to long term changes in bone structure30,31,32.
Model IC. Phosphate ion is present in the intracellular compartment with concentration five – six times higher than phosphate concentration in plasma40. The difference is maintained by active transport of phosphate ions to the intracellular compartment40. The decrease of phosphate concentration in plasma/extracellular compartment results in increased release of phosphate from the intracellular compartment. Our model also takes into account experimental data suggesting intracellular generation of phosphate14.
Model F&IC. In this model, we assume that fast and intracellular compartments are concomitantly available for phosphate exchange during dialysis and in the intradialytic breaks.
Mathematical model
The three models comprise the following compartments: 1) extracellular fluid with volume Ve for phosphate ion (plasma is here considered as a part of the extracellular compartment), 2) plasma compartment with volume Vpl for protein bound phosphate, and 3) interstitial fluid compartment with volume Vif for protein bound phosphate ions (the last two compartments have different protein concentrations and therefore different concentrations of protein bound ions), (Fig. 1). In addition, Model F describes: 4) fast compartment for phosphate ions defined by their mass amount without any specific volume attributed to it, and Model IC and Model F&IC have: 5) intracellular compartment with volume Vi for phosphate ions.
The general kinetic equations for the three models describe the rate of change in the mass of phosphate ion in extracellular compartment, MP_e, mass of phosphate ion in intracellular compartment, MP_i, protein bound phosphate in plasma, MPB_pl, and interstitial fluid, MPB_if, phosphate ion, MP_fast, in fast compartment, volume of extracellular fluid, Ve, and plasma volume, Vpl:
where \(M_{P\_e} = V_{e} \cdot P_{e}\) , \(M_{P\_i} = V_{i} \cdot P_{i}\), \(M_{PB\_pl} = V_{pl} \cdot PB_{pl}\), \(M_{PB\_if} = V_{if} \cdot PB_{if}\), Pe phosphate concentration in extracellular (e) compartment, respectively, Pi is phosphate ion concentration in intracellular (i) compartment, PBpl is protein bound phosphate concentration in plasma, PBif is protein bound phosphate concentration in interstitial fluid, Vi is intracellular compartment volume, \({\text{V}}_{{{\text{if}}}} = V_{e} - V_{pl}\) is interstitial fluid compartment volume, ufr is the rate of ultrafiltration in dialyzer, flintr is the rate of fluid intake, bvd is the rate of depletion of plasma volume, and bvres is the rate of restoration of plasma volume. The inflow of phosphate to the extracellular compartments \(J_{{P\_{\text{int}} ake}}\) is the net result of phosphate ingestion, absorption from the intestinal tract, removal with feces or residual kidney function, impact of phosphate chelators, etc. The flow of phosphate, JP_dial, removed from blood in the dialyzer is described as:
where KP_dial denotes clearance and Trp – transmittance coefficient for phosphate 36. The parameters of the models are described in Tables 1 and 2.
The specification of the model is obtained from the general equations as follows: for Model F: \(K_{P\_ei} = 0\), for Model IC: \(K_{P\_fast} = 0\). The parameters for exchange of phosphate with the fast compartment, \(K_{P\_fast}\), and with the intracellular compartment, \(K_{P\_ei}\), are separately adjusted in Model F&IC, which combines the exchange of extracellular phosphate with the intracellular and fast stores.
Equation. (2) describes the intracellular (inorganic) phosphate mass and its kinetics due to exchange of phosphate between intracellular and extracellular compartments. To describe the internal intracellular generation and clearance of phosphate and their hypothetical modification by hemodialysis discussed in14, a modified version of the model was developed. In this version, called Model IC, Eq. (2) is extended to:
where \(G_{P\_i}\) is the intracellular generation of phosphate and \(K_{P\_i}\) is the intracellular clearance of phosphate. Furthermore, a compartment of intracellular store of phosphate ion is introduced that is the source and sink for intracellular phosphate ions, i.e.:
where \(M_{sPi}\) is the mass of intracellular store of phosphate.
The parameter \(G_{P\_i}\) may increase during dialysis session according to the data and hypothesis presented in14. It was assumed that during dialysis \(G_{P\_i}\) increases in a sigmoidal fashion from its equilibrium value \(G_{P\_i,0}\) to the maximal value \(G_{P\_i,\max }\) in about one hour, \(G_{P\_i} \left( t \right) = G_{P\_i,0} + \left( {G_{P\_i,\max } - G_{P\_i,0} } \right)0.6t^{4} /\left( {1 + 0.6t^{4} } \right)\), and decreases after the end of the session, according to the analogous pattern, to the equilibrium value; the parameters of this function were adjusted by computer simulations and comparison to the clinical data, c.f. Table 2. The application of similar “switching functions” for modeling of mineral metabolism may be found in30,31.
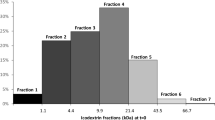
The parameters of the models related to the patient and dialysis treatment (dialyzer clearance and transmittance coefficient of phosphate, ultrafiltration rate, initial compartment volumes, initial total phosphate concentrations) were the average values for the patient population described previously11,17, see Table 2 and Fig. 2. Some physiological parameters were derived from general physiological knowledge4,11,40,41,42, and the parameters related to the compartments that were not accessible for our clinical study, were found using the trial–error method with simulations of each model until obtaining the good comparison to the average data points of the measured variables, see Tables 1 and 2 for details.
Results
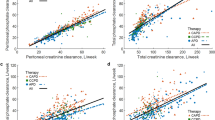
The weekly time course of phosphate concentrations in plasma during a one-week cycle of hemodialysis treatment according to Model F (Table 1) is shown in Fig. 2 for different forms of phosphate. Comparisons of the predictions from Models F, IC and F&IC are presented in Figs. 3 and 4 with the model parameters, which differed between these models, shown in Table 2. The presented results were obtained after preliminary simulations of 20 weeks of dialysis to get the time course repeatable from each week cycle to the next one. The systems described by Models F and IC are well balanced for weekly cycles of concentration and amount of phosphate in all compartments. The initial values and oscillation amplitudes of total phosphate concentration in serum are similar to those observed in clinical studies (Fig. 3)11. The profiles of the ions in plasma predicted by Models IC and F&IC are similar to those obtained by Model F (Fig. 3), with some of the phosphate turnover parameters adjusted (Table 2). The post-dialysis plasma profile of phosphate has a slight overshoot according to Model IC that is not observed for the other models (Fig. 3). The concentration of phosphate in plasma had clear tendency to equilibrate at the end of the four-hour dialysis session for all models (Fig. 3). In contrast, the profiles of phosphate in the intracellular and fast compartments differed among the models (Fig. 4).
Clinical data (mean ± standard deviation, red) and the profiles of total and ion phosphate (P) in plasma during a one-week cycle of three hemodialysis (HD) sessions predicted by Models F, IC and F&IC in a stable patient. Shown are total (panel a) and ion (panel b) phosphate profiles, and close up of total and ion phosphate profiles during the midweek dialysis session (panels c and d, respectively) in plasma predicted by Models F (continuous lines), IC (dotted lines) and F&IC (hatched lines), see Tables 1 and 2 for the model parameters.
The profiles of free intracellular phosphate (P) and phosphate mass in intracellular store as well as the phosphate amount in the fast compartment during a one-week cycle of three hemodialysis (HD) sessions in a stable patient predicted by Models F, IC and F&IC. Shown are ion phosphate concentration (panel a) and mass (panel b) in intracellular space as well as ion phosphate amounts (panel c) in the fast compartments predicted by Models F (continuous lines), IC (dotted lines) and F&IC (hatched lines), see Tables 1 and 2 for the model parameters.
The time course of the variables not measured in clinical studies were qualitatively similar to those measured, but with another level and another amplitude of oscillations between initial and final concentrations during each session (Figs. 2 – 4). A low amplitude of oscillations was numerically predicted for intracellular phosphate, protein bound phosphate in serum, and phosphate amount in the fast compartment (Figs. 2 – 4). The model predicted also a slight decrease in the concentration of protein bound phosphate during dialysis, in spite of the hemoconcentration of proteins, due to the fast equilibration between free and protein bound phosphate (Fig. 2).
An important observation from all the models is that the phosphate concentration between dialysis sessions equilibrated not to the equilibrium phosphate concentration in extracellular fluid, Pe0, according to the assumed dynamics of the exchange between extracellular and fast compartments, Eqs. (1) and (5), but was slighly higher to allow the replenishment of phosphate store in the fast compartment (Models F and F&IC) or/and the intracellular store (Models IC and F&IC) that decreased during the dialysis session. The replenishment was due to the absorption of phosphate from the intestine.
Some modifications of the model were proposed and tested with the aim to check the role of different processes in shaping the profile of phosphate. The omission of the protein binding for phosphate (the concentration of protein bound phosphate was assumed to be 15% of total phophate in plasma in the standard simulation, Fig. 2) decreased the amplitude of the phosphate concentration drop during dialysis (Fig. 5).
The profiles of total phosphate (P) in plasma predicted by Model F and when Model F is modified by neglecting binding of phosphate to proteins during a one-week cycle of three hemodialysis (HD) sessions. Shown are total phosphate in plasma predicted by Model F (continuous line) and Model F modified by neglecting binding of phosphate to proteins (dotted line, parameters from Table 1 with the modified KPBound_pl = KPBound_if = 0 and Pe0 = 1.4 mmol/L).
The shape of the phosphate profile during dialysis depends to some extent on the volume of the central phosphate distribution compartment (which is the extracellular fluid in our model). The simulations presented in Fig. 6 were performed for two different values of the extracellular volume (15 L and 11 L resepectively) with all other parameters being the same. The curve predicted for the lower extracellular volume has slightly faster initial decrease and earlier equilibration phase, i.e., deeper rebound, than the curve for the higher volume. Although the difference is not large, this observation is important because the pseudo-one compartment model underestimates the distribution volume for phosphate compared to the measured or estimated extracellular volume15,39,43.
The profile of total phosphate (P) in plasma during the midweek hemodialysis (HD) session predicted by Model F and when Model F is modified by changing the extracellular fluid volume from 15 to 11 L. Shown are total phosphate predicted by Model F (continuous line) and Model F modified by changing the extracellular volume Ve from 15 to 11 L (dashed line). Other model parameters (Table 1) were the same for both simulations.
The role of the intracellular compartment of phosphate for phosphate removal during dialysis was studied by modifying the clearance parameter KP_ei for the phosphate exchange between extracellular and intracellular compartments in Models IC and F&IC (Fig. 7). The concentration profile of phosphate predicted by Model IC is sensitive to the value of the clearance parameter for the exchange of phosphate between extracellular and intracellular compartments, KP_ei (Fig. 7). The modification of KP_ei by + /- 50% changes the predicted plasma phosphate level between dialysis sessions and the final value of phosphate at the end of dialysis, whereas the kinetics of phosphate in the intracellular store of phosphate is similar for all three values of KP_ei (Fig. 7, panels a and b). In contrast, similar modifications of the value of KP_ei applied in Model F&IC result in only slight change in phosphate profiles in both compartments (Fig. 7, panels c and d).
The profiles of total phosphate (P) in plasma and ion phosphate in intracellular space predicted by Model IC and Model IC&F during the weekly cycle of three hemodialysis (HD) sessions for different clearances between extracellular and intracellular compartments. Shown are total phosphate in plasma (panel a) and ion phosphate in intracellular compartment (panel b) predicted by Model IC for standard set of parameters, Table 2, (continuous line), intercompartment clearance, \(K_{P\_ei}\), reduced by 50% (dotted line) and increased by 50% (hatched line). Panels c and d present the predictions for similar modifications of standard intercompartment clearance, \(K_{P\_ei}\), for Model IC&F. Other model parameters (Table 1) were the same for all the three simulations for each of the models.
Discussion
In this study, we formulated and tested against clinical data on circulating phosphate, a set of models describing phosphate kinetics in hemodialysis. The models have an extended scope as compared to previous models because they consider not only physical components, i.e., phosphate distribution in various body compartments, different forms of extra- and intracellular phosphate such as free phosphate ion, and protein bound phosphate, phosphate intake, and phosphate removal by dialysis, but also temporal aspects, i.e., changes in phosphate kinetics during a one-week cycle of dialysis. We show that the models could accurately describe the time course of changes in phosphate concentrations in plasma during a one-week cycle of three hemodialysis sessions and provide analysis of the impact of different factors such as the intracellular phosphate compartment and the intracellular phosphate generation on the predicted kinetics of phosphate.
Some parameters were taken from clinical data and other models, such as the initial concentration of phosphate (ionic and total) in plasma11 while other parameters were assumed based on the general physiology literature40,44. The net inflow of phosphate to the system (because of dietary intake, gastrointestinal absorption, fecal and urinary removal, and impact of phosphate chelators, etc.) was adjusted according to the principle of equilibration of phosphate inflow to its removal during the weekly cycle of dialysis using computer simulations; its value is similar to that reported recently in13,25,26. The equilibrium reaction constants for binding of phosphate to protein were selected based on the general physiology40, and the rates of these reactions were assumed enough high to obtain fast equilibration when the concentrations of free forms of phosphate change during dialysis. The clearance of phosphate from the extracellular to the fast compartment was similar to the value obtained in the pseudo-one compartment model15,16,17,39. Our Model IC and Model F&IC take into account the specific distribution of phosphate between intracellular and extracellular compartments: at equilibrium the intracellular concentration is five times higher than the extracellular concentration40. In this way, the active transport of phosphate across the cellular membrane is indirectly taken into account using a similar, approximate principle as in modeling of sodium and potassium kinetics during hemodialysis45. In contrast, the previous models of phosphate kinetics in hemodialysis assumed simple diffusion between these two compartments and equilibrated concentrations9,10,13,23,24.
To solve problems with modeling of the phosphate profile, time-dependent phosphate generation during hemodialysis was proposed in 1983; a linear or exponentially saturated increase in the generation rate of intracellular phosphate from the intracellular store with dialysis time was assumed and applied in a one-compartment model of phosphate kinetics28. It was noted in that study that the phosphate level in red blood cells did not drop during dialysis28. In another study, after the observation of a poor fit of the two compartment model of phosphate for hemodialysis kinetics with constant parameters, an increasing influx of phosphate from intracellular to extracellular compartment was adjusted to the data9. Additional phosphate generation from a “third pool” controlled by the intracellular phosphate concentration and from a “fourth pool” inside the intracellular compartment was introduced into the two compartment phosphate model to improve the modeling of the extracellular phosphate concentration10. An increase in the intracellular level of phosphate during acute hemodialysis session in bilaterally nephrectomized pigs was (indirectly) demonstrated14. A similar approach using additional pools of phosphate that were triggered to release phosphate by low phosphate concentration in intra-/extracellular compartment was recently proposed and extensively tested13,25,26. The organic phosphate in ATP or polyphosphates or glycophosphates were mentioned as sources of intracellular inorganic phosphate7,14.
We followed the idea that the intracellular store can release phosphate during dialysis and included such compartment in Models IC and F&IC, and then predicted the extracellular kinetics of phosphate during one week of dialysis in a metabolically stable patient, i.e., phosphate concentration (and mass) in all compartments should be the same after one week as at its beginning. Thus, our objective was to provide a quantitative description of the role of the intracellular phosphate store that can release phosphate in response to changes in circulating phosphate levels induced by dialysis. While our approach is formal, and a more physiological modeling of these intracellular processes should probably provide a better description of the clinical and experimental findings, our results confirm that the intracellular store contributes significantly to the profile of extracellular phosphate concentration during dialysis and provides a good description of the clinical data. The presented Models IC and F&IC should be considered as examples of the consistent description of the increase in intracellular phosphate level in a patient with steady state phosphate turnover including the internal store (the “fourth” compartment) rather than the definite solution of this problem. Further studies on the molecular biology of organic and inorganic phosphate turnover in the cell are needed to provide more information on the kinetics of these processes.
The classic two compartment model, i.e., extracellular/ accessible and intracellular/ fast/ non-accessible compartments for phosphate ion, yielded phosphate concentrations in plasma in disagreement with the measured values6,7,9,10,13. Another approach to modeling phosphate kinetics was to fix the phosphate concentration in the non-accessible compartment, i.e., assuming that phosphate concentration in this compartment does not change if the phosphate exchange between the two compartments occurs15,16,23,24; this approach is sometimes called pseudo one compartment model15,16,17,18. Our models extends pseudo one compartment model by assuming high amount of phosphate in inaccessible compartment (F and F&IC Model) that is only slightly modified by the removal during hemodialysis session but is also sensitive to phosphate replenishment during and between hemodialysis sessions by phosphate intake. Still different and successful extension of the two (and pseudo one) compartment model assumes additional phosphate stores that are controlled by intracellular (or extracellular) phosphate concentrations10. In our models (IC and F&IC Model), we assumed an additional compartment of intracellular store of phosphate ions (suggested by experimental findings14) and the content of all compartments is modified by phosphate loss and gain during hemodialysis and interdialytic breaks, respectively. For this approach to work one needs rather fast exchange of phosphate between extra- and intracellular compartments, especially decreasing the exchange rate parameter (with other parameters constant) yields phosphate profiles in plasma much different from the standard version of the model, whereas an increase of this parameters has negligible impact on the predicted profile (Fig. 7).
The change in the extracellular phosphate was similar in all three models (Fig. 3) while the models differed in transport parameters for phosphate (Table 2). In Model F&IC, to avoid slow depletion of the intracellular store of phosphate in the consecutive weeks of dialysis, the parameter of phosphate transport across the cellular membrane, KP_ei, was decreased and the clearance of phosphate to the fast compartment, KP_fast, was also lower than in Model IC and Model IC&F, respectively (Table 2).
Our study does not provide several important features of the investigated models. Our objective was mostly to include into the models characteristics of phosphate distribution and turnover in the body pools that are well known or were suggested by experimental findings. This is in contrast to more common approach that is focused on formal description of the kinetics of (typically total) phosphate during (typically one) dialysis session, whereas the dialytic removal is mostly by one form of phosphate: free ionic phosphate. Each of the three models separately may be investigated from theoretical point of view by analysis (theoretical or numerical) of its sensitivity to the change of the parameters (some glimpses of such analysis are shown in Figs. 5–7) and identifiability of parameters. Furthermore, the parameters of the model may be estimated by its fitting to the available individual data. However, the physiological basis of our models yields the necessity of using the variables that are not available from clinical data and therefore using more parameters that cannot be estimated for each patient separately from the data. A solution to the problem is “tuning” the parameters that means fixing some parameters and estimating a few other. According to our objective, at this stage of investigations, it is more important to select a hypothesis on the effect of hemodialysis on phosphate turnover and the interpretation of inaccessible compartments. To this end, more clinical (or experimental) investigations should carried out with different dialysis challenges (dialyzer clearance of phosphate, dialysis time and schedules, phosphate intake, etc.) in the same patient, with more details on the phosphate rebound after dialysis session collected. Such studies are challenging to perform, however without more quantitative observations it may be difficult to formulate a model that can correctly describe not only one particular session in fixed condition, but can also correctly predict the phosphate levels in different conditions of dialysis treatments. We consider our study as an initial step towards more realistic (not only formal) description of phosphate removal during dialysis that could be later integrated with a model of hormonal control of mineral metabolism.
Our clinical data include a small group of 4 patients that used high flux dialyzers whereas the other 21 patients used low flux dialyzers. This may add to heterogeneity of the results, however because the group of high flux dialysis was small and we applied the average phosphate profiles and the average values of parameters from clinical study this heterogeneity does not skew our results much. It is worth to notice that data from the application of dialyzers with considerable different phosphate clearances in the same patient would be of interest for selection between the physiological hypotheses behind our three models.
In summary, among conclusions that can be drawn from this investigation of models for phosphate kinetics in hemodialysis, the following may be especially relevant:
1) In our models, a fast compartment and an intracellular store compartment—separately or combined—contribute significantly to the kinetics of total phosphate in plasma and the pattern of changes was kinetically compatible with clinical data after adjusting model parameters.
2) On the other hand, the substantial exchange of phosphate between extracellular and intracellular compartments during dialysis, assumed by some models30,31, is not supported by the clinical profile of the plasma concentration of phosphate, which tends to reach a steady level early during the dialysis session and then rebounds quickly to the pretreatment value after dialysis. In contrast, the model assuming an increased exchange between extra- and intracellular compartments predicts a considerably higher amplitude of dialysis – induced oscillations of phosphate (between initial and final concentrations during each session) in the weekly profile than that observed in clinical studies (Fig. 7).
3) The pre-dialysis concentration of phosphate in plasma is higher than the equilibrium concentration for the exchange between the extracellular and fast compartments. This phenomenon should be expected in patients with equilibrated mineral mass balance because the phosphate lost from the fast compartment during dialysis must be replenished between the treatments and this process needs higher concentration in extracellular fluid than the respective equilibrium concentrations for this exchange. These mechanisms are also valid for the intracellular phosphate store.
These findings underline the complex nature of plasma phosphate kinetics in patients undergoing hemodialysis and underscore the need of further studies to better understand the dynamic changes of phosphate ions and total phosphorous in extra- and intracellular compartments and how these are influenced during hemodialysis by the fast exchangeable pool of phosphate and calcium related to bone mass.
Data availability
The clinical dataset used during the current study is available from the corresponding author on request.
References
Covic, A. et al. Systematic review of the evidence underlying the association between mineral metabolism disturbances and risk of all-cause mortality, cardiovascular mortality and cardiovascular events in chronic kidney disease. Nephrol. Dial. Transplant. 24, 1506–1523 (2009).
Smith, D. H. et al. Outcomes predicted by phosphorous in chronic kidney disease: a retrospective CKD-inception cohort study. Nephrol. Dial. Transplant. 25, 166–174 (2010).
Bover, J., Andres, E., Lloret, M. J., Aguilar, A. & Ballarin, J. Dietary and pharmacological control of calcium and phosphate metabolism in dialysis patients. Blood Purif. 27, 369–386 (2009).
Messa, P., Cerutti, R., Brezzi, B., Alfieri, C. & Cozzolino, M. Calcium and phosphate control by dialysis treatments. Blood Purif. 27, 360–368 (2009).
Kestenbaum, B. & Belozeroff, V. Mineral metabolism disturbances in patients with chronic kidney disease. Eur. J. Clin. Invest. 37, 607–622 (2007).
Pogglitsch, H., Petek, W., Ziak, E., Sterz, F. & Holzer, H. Phosphorus kinetics during haemodialysis and haemofiltration. Proc. Eur. Dial. Transplant. Assoc. Eur. Ren. Assoc. 21, 461–468 (1985).
Sugisaki, H., Onohara, M. & Kunitomo, T. Dynamic behavior of plasma phosphate in chronic dialysis patients. Trans. Am. Soc. Artif. Intern. Organs 28, 302–307 (1982).
Hou, S. H. et al. Calcium and phosphorus fluxes during hemodialysis with low calcium dialysate. Am. J. Kidney Dis. 18, 217–224 (1991).
Maasrani, M., Jaffrin, M. Y., Fischbach, M. & Boudailliez, B. Urea, creatinine and phosphate kinetic modeling during dialysis: application to pediatric hemodialysis. Int. J. Artif. Organs 18, 122–129 (1995).
Spalding, E. M., Chamney, P. W. & Farrington, K. Phosphate kinetics during hemodialysis: Evidence for biphasic regulation. Kidney Int. 61, 655–667 (2002).
Debowska, M., Wojcik-Zaluska, A., Ksiazek, A., Zaluska, W. & Waniewski, J. Phosphate, urea and creatinine clearances: haemodialysis adequacy assessed by weekly monitoring. Nephrol. Dial. Transplant. 30, 129–136 (2015).
Nordio, M. et al. Analysis of phosphate kinetics in hemofiltration and hemodiafiltration: formulation of an efficiency index. Artif. Organs 17, 24–27 (1993).
Daugirdas, J. T. A two-pool kinetic model predicts phosphate concentrations during and shortly following a conventional (three times weekly) hemodialysis session. Nephrol. Dial. Transplant. 33, 76–84 (2018).
Lemoine, S. et al. Intracellular phosphate dynamics in muscle measured by magnetic resonance spectroscopy during hemodialysis. J. Am. Soc. Nephrol. 27, 2062–2068 (2016).
Agar, B. U., Akonur, A., Lo, Y. C., Cheung, A. K. & Leypoldt, J. K. Kinetic model of phosphorus mobilization during and after short and conventional hemodialysis. Clin. J. Am. Soc. Nephrol. 6, 2854–2860 (2011).
Leypoldt, J. K. et al. Determinants of phosphorus mobilization during hemodialysis. Kidney Int. 84, 841–848 (2013).
Debowska, M., Poleszczuk, J., Wojcik-Zaluska, A., Ksiazek, A. & Zaluska, W. Phosphate kinetics during weekly cycle of hemodialysis sessions: Application of mathematical modeling. Artif. Organs 39, 1005–1014 (2015).
Poleszczuk, J., Debowska, M., Wojcik-Zaluska, A., Ksiazek, A. & Zaluska, W. Phosphate kinetics in hemodialysis: Application of delayed pseudo one-compartment model. Blood Purif. 42, 177–185 (2016).
Bernardo, A. P. et al. Peritoneal membrane phosphate transport status: a cornerstone in phosphate handling in peritoneal dialysis. Clin. J. Am. Soc. Nephrol. 6, 591–597 (2011).
Gomez, R., Waniewski, J., Zapata, A., Pietribiasi, M. & Lindholm, B. Phosphate equilibration rate and daily clearance in patients on CAPD, CCPD and APD. Int. J. Artif. Organs 39, 596–602 (2017).
Gotch, F., Kotanko, P., Handelman, G. & Levin, N. A kinetic model of calcium mass balance during dialysis therapy. Blood Purif. 25, 139–149 (2007).
Gotch, F. A. et al. A kinetic model of inorganic phosphorus mass balance in hemodialysis therapy. Blood Purif. 21, 51–57 (2003).
Andersen, M., Bangsgaard, K. O., Heaf, J. G. & Ottesen, J. T. Analytical solution of phosphate kinetics for hemodialysis. J. Math. Biol. 87, 11 (2023).
Bangsgaard, K. O., Andersen, M., Heaf, J. G. & Ottesen, J. T. Bayesian parameter estimation for phosphate dynamics during hemodialysis. Math. Biosci. Eng. 20, 4455–4492 (2023).
Daugirdas, J. T. Comparison of measured vs kinetic-model predicted phosphate removal during hemodialysis and hemodiafiltration. Nephrol. Dial. Transplant. 37, 2522–2527 (2022).
Daugirdas, J. T. Comparison of modeled versus reported phosphate removal and modeled versus postdialysis serum phosphate levels in conventional hemodialysis. Semin. Dial. 36, 337–344 (2023).
Kapoian, T., Khalil, S., O’Mara, N. B., Brink, D. M. & Daugirdas, J. T. Modeled daily ingested, absorbed and bound phosphorus: New measures of mineral balance in hemodialysis patients. Am. J. Nephrol. 49, 368–376 (2019).
Sugisaki, H., Onohara, M. & Kunitomo, T. Phosphate in dialysis patients. Trans. Am. Soc. Artif. Intern. Organs 29, 38–43 (1983).
Gutzwiller, J. P. et al. Estimating phosphate removal in haemodialysis: an additional tool to quantify dialysis dose. Nephrol. Dial. Transplant. 17, 1037–1044 (2002).
Peterson, M. C. & Riggs, M. M. A physiologically based mathematical model of integrated calcium homeostasis and bone remodeling. Bone 46, 49–63 (2010).
Raposo, J. F., Sobrinho, L. G. & Ferreira, H. G. A minimal mathematical model of calcium homeostasis. J. Clin. Endocrinol. Metab. 87, 4330–4340 (2002).
Jaros, G. G., Guyton, A. C. & Coleman, T. G. The role of bone in short-term calcium homeostasis: an analog-digital computer simulation. Ann. Biomed. Eng. 8, 103–141 (1980).
Debowska, M. et al. Association between biomarkers of mineral and bone metabolism and removal of calcium and phosphate in hemodialysis. Blood Purif. 49, 71–78 (2020).
Waniewski, J., Debowska, M., Wojcik-Zaluska, A., Ksiazek, A. & Zaluska, W. Quantification of dialytic removal and extracellular calcium mass balance during a weekly cycle of hemodialysis. PLoS One 11, e0153285 (2016).
Pietribiasi, M., Waniewski, J., Zaluska, A., Zaluska, W. & Lindholm, B. Modelling transcapillary transport of fluid and proteins in hemodialysis patients. PLoS One 11, e0159748 (2016).
Waniewski, J. et al. Theoretical basis and experimental verification of the impact of ultrafiltration on dialyzer clearance. Artif. Organs 15, 70–77 (1991).
Waniewski, J., Lucjanek, P. & Werynski, A. Alternative descriptions of combined diffusive and convective mass transport in hemodialyzer. Artif. Organs 17, 3–7 (1993).
Waniewski, J., Lucjanek, P. & Werynski, A. Impact of ultrafiltration on back-diffusion in hemodialyzer. Artif. Organs 18, 933–936 (1994).
Leypoldt, J. K., Agar, B. U., Akonur, A., Gellens, M. E. & Culleton, B. F. Steady state phosphorus mass balance model during hemodialysis based on a pseudo one-compartment kinetic model. Int. J. Artif. Organs 35, 969–980 (2012).
Guyton, A. C. & Hall, J. E. Textbook of Medical Physiology (Saunders, 2000).
Graff, J., Fugleberg, S., Brahm, J. & Fogh-Andersen, N. The transport of phosphate between the plasma and dialysate compartments in peritoneal dialysis is influenced by an electric potential difference. Clin. Physiol. 16, 291–300 (1996).
Rippe, B., Venturoli, D., Simonsen, O. & de Arteaga, J. Fluid and electrolyte transport across the peritoneal membrane during CAPD according to the three-pore model. Perit. Dial. Int. 24, 10–27 (2004).
Agar, B. U., Akonur, A., Cheung, A. K. & Leypoldt, J. K. A simple method to estimate phosphorus mobilization in hemodialysis using only predialytic and postdialytic blood samples. Hemodial. Int. 15(Suppl 1), S9–S14 (2011).
Ross Morton, A. & Hercz, G. in Nutritional management of renal disease (eds J.D. Kopple & S.G. Massry) 341–369 (Williams & Wilkins, 1997).
Ursino, M. et al. Mathematical modeling of solute kinetics and body fluid changes during profiled hemodialysis. Int. J. Artif. Organs 22, 94–107 (1999).
Funding
This study was supported by the Polish National Science Centre, grant no N N518 289840.
Author information
Authors and Affiliations
Contributions
J.W.: Conceptualization, Formal analysis, Software, Writing—Original Draft, Validation; M.D.: Data Curation, Software, Visualization, Writing—Review & Editing; A.W-Z.: Data Curation, Investigation; W.Z.: Investigation, Supervision, Validation; B.L.: Investigation, Validation, Writing—Review & Editing. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
B.L. was previously employed by Baxter Healthcare Corporation. Baxter Novum is the result of a grant of Baxter Healthcare Corporation to Karolinska Institutet. The other authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Waniewski, J., Debowska, M., Wojcik-Zaluska, A. et al. Mathematical models for phosphate kinetics in patients on maintenance hemodialysis. Sci Rep 15, 9176 (2025). https://doi.org/10.1038/s41598-025-93443-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-93443-1