Abstract
This study examined the different effects of high-fat and capsicum diets on the digestive organs of guinea pigs. Hartley guinea pigs (n = 24) were divided into the high-fat diet (HFD), capsicum diet (CD), and control (C) groups. Guinea pigs in the C, HFD, and CD groups received maintenance feed, high-fat, and capsicum diets, respectively. After 12 weeks of modelling, serum samples were collected for biochemical analysis. Enzyme-linked immunosorbent assay was used to quantify interleukin-1β, interleukin-6, and tumour necrosis factor-α, while haematoxylin-eosin staining was used to observe morphological changes. Blood lipid levels and inflammatory markers in the serum of guinea pigs in HFD and CD groups were significantly elevated than those in the serum of guinea pigs in the C group (P < 0.01). Inflammation and blood lipid disorders were more severe among guinea pigs in the HFD group than among those in the CD and C groups (P < 0.001). Pathological examinations revealed that high-fat and capsicum diets induce damage to the liver, stomach, gallbladder, and colon. Specifically, high-fat diets exhibited more significant effects. High-fat or capsicum diet consumption can damage the digestive organs, causing abnormal lipid metabolism; however, high-fat diets exhibit more significant effects on the digestive organs.
Similar content being viewed by others
Introduction
The prevalence of human diseases is intricately linked to various factors, including dietary habits1,2, climatic conditions3,4, daily routines5, infectious agents6, and emergency situations7,8. Suboptimal dietary practices are significant contributors to the prevalence of digestive system diseases. The maintenance of healthy eating habits correlates with positive outcomes for physiological functions, while poor dietary choices can adversely affect these functions, particularly those of the digestive system. Lipids and capsicum, common components of various diets, are essential in sustaining the energy requirements of the body when included in a balanced diet. However, extensive literature documents the adverse effects associated with prolonged high-fat diets and increased capsicum consumption. Despite ongoing debates within the field, studies on the long-term ramifications of high-fat and capsicum diets on multiple digestive organs, including the liver, stomach, gallbladder, and colon, are relatively new. We conducted a comprehensive study aimed at clarifying the effects of two distinct dietary patterns, a high-fat diet and a chilli-rich diet, on the digestive organs. Through a systematic comparison of the impacts of these dietary patterns on blood lipid profiles, inflammatory markers, and the morphological characteristics of vital digestive tissues (specifically, the liver, stomach, gallbladder, and colon), we have initiated the investigation of the physiological implications associated with each dietary regimen. This study aimed to inform and advocate for the implementation of healthy dietary practices based on empirical evidence.
Results
Effects of High-Fat diet and Capsicum diets on lipid indices in Guinea pigs
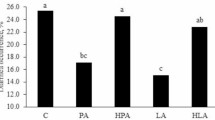
The average triglycerides (TG) levels among guinea pigs in groups HFD, CD, and C were 3.91 mmol/L (P < 0.0001 versus control), 1.61 mmol/L (P < 0.01 versus control), and 0.78 mmol/L. The average TG level among guinea pigs in the CD group was significantly lower than that among those in the HFD group (P < 0.0001). The average TC levels among guinea pigs in groups HFD, CD, and C were 8.41 mmol/L (P < 0.0001 versus control), 3.78 mmol/L (P < 0.0001 versus control), and 1.24 mmol/L. The average TC level among guinea pigs in the CD group was significantly lower than that among those in the HFD group (P < 0.0001). The average HDL-C levels among guinea pigs in the HFD, CD, and C groups were 2.19 mmol/L (P < 0.0001 versus control), 1.20 mmol/L (P < 0.05 versus control), and 0.81 mmol/L. The average HDL-C level among guinea pigs in the CD group was significantly lower than that among those in the HFD group (P < 0.0001). The average LDL-C levels among guinea pigs in the HFD, CD, and C groups were 4.92 mmol/L (P < 0.0001 versus control), 3.11 mmol/L (P < 0.01 versus control), and 1.99 mmol/L. The average LDL-C level among guinea pigs in the CD group was significantly lower than that among those in the HFD group (P < 0.0001). (Fig. 1. A-D)
(A-D) diagrams show the results of lipid profile testing, including TG, TC, HDL-C, and LDL-C (n = 8). The C group is the control group, the HFD group is the high-fat diet group, and the CD group is the Capsicum Diet. The values in the figure are presented as mean ± SD. * P < 0.05, ** P < 0.01, *** P < 0.001, ****P < 0.0001 compared to the C group. # P < 0.05, ## P < 0.01, ### P < 0.001, ####P < 0.0001 compared to the HFD group.
Effects of a high-fat diet and a capsicum diet on the inflammatory markers in serum of guinea pigs
The average TNF-α levels among guinea pigs in groups HFD, CD, and C were 644.62 pg/mL (P < 0.0001 versus control), 468.42 pg/mL (P < 0.01 versus control), and 145.18 pg/mL. The average TNF-α level among guinea pigs in the CD group was significantly lower than that among those in the HFD group (P < 0.01). The average IL-1β levels among guinea pigs in groups HFD, CD, and C were 67.19 pg/mL (P < 0.0001 versus control), 46.68 pg/mL (P < 0.0001 versus control), and 16.44 pg/mL. The average IL-1β level among guinea pigs in the CD group exhibited no significant difference from that of those in the HFD group (P > 0.05). The average IL-6 levels for groups HFD, CD, and C were 126.17 pg/mL (P < 0.0001 versus control), 95.16 pg/mL (P < 0.0001 versus control), and 39.99 pg/mL. The average TC level among guinea pigs in the CD group was significantly lower than that among those in the HFD group (P < 0.001). (Fig. 2. A-C)
(A-C) diagrams show the results of serum inflammation marker tests, including TNF-α, IL-1β, and IL-6 (n = 8). The C group is the control group, the HFD group is the high-fat diet group, and the CD group is the Capsicum Diet. The values in the figure are presented as mean ± SD. * P < 0.05, ** P < 0.01, *** P < 0.001, ****P < 0.0001 compared to the C group. # P < 0.05, ## P < 0.01, ### P < 0.001, ####P < 0.0001 compared to the HFD group.
Effects of high-fat diet and capsicum diet on the morphological changes of liver, stomach, gallbladder, and colon tissues of guinea pig
HE staining method was used to stain the liver, stomach, gallbladder, and colon tissues from the guinea pigs. The experimental findings revealed that the liver tissues of guinea pigs in the HFD group exhibited widespread hepatic steatosis compared to those of guinea pigs in group C. The cytoplasm contained round vacuoles of different sizes (black arrows), mild oval-shaped cell proliferation (yellow arrows), mild fibrosis (blue arrows), and localised inflammatory cell infiltration (red arrows). Significant hepatic steatosis was observed among the liver tissues of guinea pigs in the CD group, with mild fibrosis surrounding the portal regions (blue arrows) and tiny round vacuoles in the cytoplasm (black arrows). However, no obvious infiltration of inflammatory cells was observed. According to the research previously mentioned, eating excessive fat substantially aggravates hepatic steatosis and causes inflammation in the liver. Although eating capsicum diets can cause hepatic steatosis, the inflammatory response is minimal, and the liver damage is less severe than it would be with a high-fat diet. (Fig. 3.)
Shows the HE staining results of liver, stomach, gallbladder, and colon tissues from each group of guinea pigs (magnification ×100). The C group is the control group, the HFD group is the high-fat diet group, and the CD group is the Capsicum Diet. In the liver tissue, the black arrow indicates round vacuoles, the yellow arrow indicates oval-shaped cell proliferation, the red arrow indicates inflammatory cell infiltration, and the blue arrow indicates fibrosis changes. In the stomach tissue, brown indicates irregular changes in gastric glandular tissue, dark blue indicates inflammatory cell infiltration, orange indicates fragmentation of cells within the stomach tissue, green indicates capillary congestion, and purple indicates cystic dilation of the stomach. In the gallbladder tissue, magenta indicates a change in the mucosal epithelial cells from tall columnar epithelium to short columnar epithelium. In the colon tissue, dark gray indicates thinning of the intestinal wall and a reduction in goblet cells, burgundy indicates an increase in submucosal adipocytes, cyan indicates lymphoid tissue proliferation, and dark green indicates inflammatory cell infiltration.
Guinea pigs in the HFD group exhibited focal necrosis and gastric gland cell shedding with irregular gastric gland morphology in the gastric mucosal layer compared to those in C group. In addition to mucosal layer ulcers, atrophy, and necrosis of the gastric glands, cell debris (orange arrows) was obvious in the gastric gland lumen. Proliferated connective tissue replaced the structure, and there is an obvious infiltration of inflammatory cells (dark blue arrows), capillary congestion in the stroma (green arrows), and irregular residual gastric glands (brown arrows). The submucosal layer exhibited localised oedema. Localised ulcers and a loss of mucosal epithelial structure were observed among the stomach tissues of guinea pigs in the CD group. An obvious gastric gland atrophy and necrosis were observed in the lamina propria, where structures have been replaced by proliferating connective tissue. The remaining stomach glands exhibited inflammatory cell infiltration (dark blue arrows), cystic dilatation (purple arrows), and irregular shape (brown arrows). Around the ulcerative lesions, there was atrophy of the stomach glands, a small area of oedema in the lamina propria, and sporadic infiltration of inflammatory cells. These results imply that a high-fat diet and capsicum diet intake considerably exacerbate the inflammatory response, gastric gland atrophy and necrosis, and gastric mucosal ulceration. (Fig. 3.)
While the lamina propria exhibited no significant abnormalities or overt inflammatory cell infiltration, the gallbladder tissue of guinea pigs in the HFD group displayed mucosal layer atrophy and thinning compared to those in the C group, with many mucosal epithelial cells changing from tall columnar epithelial cells to short columnar epithelial cells (magenta arrows). While the lamina propria showed no significant anomalies or overt inflammatory cell infiltration, the gallbladder tissues of guinea pigs in the CD group displayed mild mucosal layer atrophy and thinning, with a few mucosal epithelial cells changing from tall columnar epithelial cells to short columnar epithelial cells (magenta arrows). (Fig. 3.)
Guinea pigs in the HFD group exhibited intestinal wall thinning in colon tissue, fewer goblet cells (dark gray arrow), sporadic inflammatory cell infiltration in the lamina propria (dark green arrow), and an obvious increase in fat cells in the submucosa (burgundy arrow) compared to those in the C group. Colon tissue of guinea pigs in the CD group exhibited a significant increase in fat cells in the submucosa (burgundy arrow), a decrease in goblet cells (dark gray arrow), lymphoid hyperplasia in the lamina propria and submucosa (cyan arrow), and a thinning of the intestinal wall. (Fig. 3.)
Discussion
Dietary behaviours of individuals substantially influence overall health outcomes. Maintaining a balanced and nutritious diet is essential for promoting physiological well-being. The prevalence of unhealthy eating habits has created considerable challenges for public health, resulting in various conditions, including gastrointestinal and cardiovascular diseases. Numerous studies have emphasised the risk associated with high-fat diets, which endanger the health of digestive organs and other organ systems. Chronic consumption of such diets has been associated with health complications, including indigestion, fatty liver disease, atherosclerosis, and cerebrovascular incidents, including strokes. Despite the established risks associated with high-fat dietary patterns, the literature on the health effects of chilli consumption has predominantly focused on its potential role in disease prevention and therapeutic uses. capsicums and their bioactive constituents are frequently cited for their potential benefits, including weight control, analgesic effects, and antibacterial properties. An increasing discourse indicates that chilli may exert beneficial and detrimental effects on human health. This investigation was initiated by an inquiry into the disparate effects of different dietary habits on the health of digestive system organs.
Our research indicates that prolonged consumption of high-fat and chilli-based diets can significantly disrupt blood lipid metabolism. This disruption is marked by abnormal increases in TG, total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterol (LDL-C). A previous study demonstrated that long-term high-fat diets are significant causes of blood lipid metabolism disorders9.TG, TC, HDL-C, and LDL-C are essential markers of lipid metabolism. Triglycerides are essential for energy storage and safeguarding of internal organs; however, elevated TG levels may signify the onset of metabolic diseases, including hyperlipidaemia, diabetes, and cardiovascular conditions10. TC represents the overall level of cholesterol present in all lipoproteins in the bloodstream. Abnormal increases in TC levels are closely associated with hyperlipidaemia, atherosclerosis, coronary heart disease, stroke, and other cardiovascular diseases11. HDL-C is primarily synthesised in the liver and is essential in transporting phospholipids and cholesterol. HDL-C exerts anti-atherosclerotic and cardiovascular benefits through various mechanisms, including facilitating cholesterol reverse transport, antioxidation, and anti-inflammation. Numerous studies have demonstrated a negative correlation between HDL-C levels and the incidence of coronary heart disease. However, a previous study demonstrated that conditions including chronic hepatitis and fatty liver can cause elevated HDL-C levels12. Conversely, hyperlipoproteinemia, acute myocardial infarction, coronary heart disease, and diabetes are closely associated with abnormal increases in LDL-C levels. Studies have demonstrated a significant positive correlation between LDL-C concentrations and the risk of coronary heart disease. Herein, the high-fat diet group exhibited abnormal increases in serum TG, TC, HDL-C, and LDL-C, confirming that long-term high-fat diets can impair lipid metabolism. Additionally, numerous studies demonstrated that capsicum diets or capsaicin intake may help improve lipid metabolic disorders13,14. However, there is a lack of studies on the impact of a high capsicum intake on blood lipids. Our study demonstrates that a long-term chilli-based diet can lead to abnormal increases in serum TG, TC, HDL-C, and LDL-C. This effect is probably associated with pathological liver damage and inflammatory changes in the intestines induced by the chilli diet, which disrupt cholesterol metabolism15,16,17,18,19. Furthermore, numerous studies have demonstrated that cholesterol is secreted from the liver into the intestines via bile, a process closely associated with bile acids and intestinal microbiota20,21,22,23. However, the specific mechanism by which prolonged chilli intake disrupts serum cholesterol metabolism, and whether this is mediated by bile acid metabolism or gut microbiota, requires further comprehensive investigation.
Our investigation demonstrated that the long-term high-fat and chilli-based diet intake can elicit inflammatory responses in the serum, characterised by significant elevations in pro-inflammatory cytokines, specifically TNF-α, IL-1β, and IL-6. These cytokines are essential in the inflammatory process, and substantial evidence from existing literature indicates that prolonged high-fat diet intake fosters inflammatory responses within the serum. Tan’s research highlights that an increased intake of dietary fats leads to excessive accumulation of free fatty acids in the bloodstream, which subsequently incites oxidative stress, thereby promoting systemic inflammation24. Furthermore, Binayi et al. reported that high-fat diets induce endoplasmic reticulum stress, which impairs lipid metabolism and subsequently triggers inflammatory pathways25. Malesza et al. reported that extended high-fat diet intake can lead to dysbiosis of gut microbiota and impairments in intestinal barrier function, facilitating the translocation of metabolic byproducts from harmful bacteria into the circulatory system, exacerbating systemic inflammation26. Our findings are consistent with those of previous studies, reinforcing that long-term high-fat diet intake is associated with increased inflammatory responses. Conversely, although it is a common belief that diets enriched with capsicum provide health benefits, primarily through the activation of the transient receptor potential vanilloid 1 (TRPV1) receptor signalling pathway, which is believed to attenuate inflammation and alleviate pain, literature documenting the potential inflammatory effects of prolonged capsicum intake is scarce27. Xiang et al. reported that high doses of capsaicin may induce intestinal inflammation, potentially attributable to alterations in gut microbiota composition28. Our research extends these findings by demonstrating that a prolonged diet high in capsicum diets induces inflammatory responses in the serum and adversely affects the digestive organs, substantiating the adverse consequences of sustained capsicum intake on gastrointestinal health.
Studies demonstrated that prolonged consumption of high-fat foods and capsicum diets can significantly damage gastric tissue. This damage is primarily characterised by injury to the gastric mucosa, inflammatory responses, and the ensuing development of ulcers. In comparing the effects of high-fat diets to those resulting from long-term exposure to capsicum diets, the gastric mucosa exposed to long-term capsicum diets exhibit more severe manifestations, including increased ulceration, atrophy, and necrosis. The stomach is essential to the digestive system; it is responsible for food storage and mechanical and chemical digestion processes, which are facilitated by gastric motility, acid secretion, and pepsin activity. Numerous academic studies have suggested a direct correlation between high-fat diets and the onset of gastritis, although the precise mechanisms underlying this association are inadequately clarified. Some researchers suggest that this association may arise from lipotoxicity, which compromises the stability of gastric mucosal organelles and gastric tissue integrity, thereby inducing gastritis and precancerous transformations in gastric tissue29. Additionally, obesity, frequently associated with high-fat consumption, has been associated with pathological alterations in gastric tissue. An increase in the quantity of ghrelin-expressing cells in the stomach is posited to correlate closely with obesity mechanisms induced by high-fat diets30,31,32. Our research has confirmed the deleterious effects of high-fat diets on gastric tissue; however, the extent to which this impact is due to lipid toxicity, as opposed to other contributing factors, requires further investigation. The current literature indicates a duality in the effects of capsicum diets. Many scholars assert that capsicum diets and their derivatives exhibit anticancer and antioxidant properties and therapeutic potential for gastric cancer treatment. This functionality may be significantly associated with the activation of the TRPV1 receptor signalling pathway33,34. However, some researchers have empirically demonstrated a correlation between elevated capsicum diets and specific gastric conditions, including gastric bleeding35. Increasing evidence indicates that a higher intake of capsicum diets or capsaicin can markedly elevate the risk of developing gastric cancer36,37,38. Our research has concluded that long-term capsicum consumption adversely affects gastric tissue. The underlying mechanisms contributing to this impact are closely associated with inflammatory processes and immune responses; however, the specific pathways involved require further investigation.
Studies demonstrate that prolonged high-fat food intake causes substantial damage to liver tissue. This damage is predominantly characterised by liver steatosis, fibrosis, and the onset of inflammatory processes. However, prolonged intake of capsaicin leads to liver steatosis and mild fibrosis, although without significant inflammatory alterations compared to prolonged high-fat diet intake. The liver is the primary metabolic and digestive organ. It is essential in glucose and lipid metabolism and bile production and secretion. Extensive studies have demonstrated the deleterious effects of high-fat diets on liver health, confirming that long-term adherence to such dietary patterns results in fat accumulation, fibrosis, and progression of conditions including fatty liver39,40,41, chronic hepatitis42, and cirrhosis43,44. Our findings confirm the consensus that prolonged high-fat dietary intake precipitates fatty liver and hepatitis, thereby enhancing the understanding of its detrimental effects on liver function. Conversely, there is a widespread belief regarding the health benefits of capsicum diet consumption. Research indicates that capsaicin, a bioactive compound found in capsicum diets, may possess therapeutic potential in alleviating cholestatic liver fibrosis and preventing hepatotoxic injury45,46. A previous study has demonstrated that capsaicin can inhibit hepatic fat accumulation in murine models of non-alcoholic fatty liver disease induced by a high-fat diet47. Xie et al. reported that capsaicin suppresses the stemness of liver progenitor cells and inhibits liver cancer development through the SIRT1/SOX2 signalling pathway48. These findings indicate that dietary capsaicin may confer protective effects against liver fibrosis, diminish hepatic fat accumulation, and impede the onset of liver malignancies. However, the investigation into the potential adverse effects of chronic dietary capsaicin on liver health is limited. Our research indicates that long-term intake of capsicum diets may negatively impact liver function, indicating that dietary capsaicin possesses a dualistic nature regarding human health, with potential long-term adverse effects outweighing its benefits, possibly associated with inflammatory responses.
Our investigation revealed the detrimental effects of a high-fat and chilli-based diet on the gallbladder mucosa, specifically resulting in its atrophy. The gallbladder is essential for the storage, concentration, and secretion of bile, a substance vital to cholesterol metabolism. Research indicates that a moderate intake of dietary fats can stimulate normal gallbladder contraction, facilitating the timely release of bile and decreasing bile stagnation, thereby reducing the risk of gallstone formation and exacerbation of cholecystitis. Numerous studies confirm that prolonged high-fat intake may impair gallbladder contractility49,50although the underlying mechanisms are unclear. Furthermore, extensive research has demonstrated that high-fat diets significantly increase the prevalence of cholesterol gallstone formation51,52. Our findings indicate that prolonged high-fat dietary patterns correlate with atrophy of the gallbladder mucosa, frequently serving as the primary pathological basis for conditions including chronic cholecystitis and gallstone disease. Many studies have demonstrated that prolonged consumption of chilli-based diets can adversely affect gallbladder health. Studies have specifically identified excessive intake of red capsicums as a risk factor for long-term gallstone formation and gallbladder cancer, especially among Chilean women53,54. Our investigation indicates that prolonged consumption of capsicums correlates with damage to the gallbladder mucosa, suggesting a significant role of persistent capsicum intake in the pathogenesis of chronic cholecystitis and other gallbladder-related disorders.
This study demonstrated significant implications of long-term dietary patterns involving high-fat and capsicum diets on colon health. Specifically, we observed that a prolonged high-fat diet can result in colon tissue atrophy and stimulate inflammatory responses, and significant accumulation of adipocytes beneath the mucosal layer of the colon. The colon is essential to the digestive system, serving in essential nutrient absorption, including vitamins, water, and minerals, and in faeces formation. Furthermore, the symbiotic bacteria and microorganisms residing within the colon are essential in maintaining metabolic homeostasis in the digestive system. Existing literature has demonstrated that high-fat diets induce oxidative stress within the colonic mucosa, leading to enhanced permeability of the epithelial barrier and the subsequent onset of colonic mucosal inflammation55. Our findings confirm the detrimental effects of prolonged high-fat diets on colon tissue, which seem to be associated with oxidative stress-related inflammatory processes within the colonic environment. However, further investigation into the specific underlying mechanisms is required. A dichotomy of perspectives exists regarding the effect of long-term capsicum consumption on colon health. Some scholars posit that dietary capsicums may adversely affect the colon. Engel et al. (2012) demonstrated that capsaicin, the active compound in capsicums, activates the TRPV1 receptor, resulting in an increased release of calcitonin gene-related peptide and substance P, potentially contributing to the pathogenesis of colitis56. However, other researchers support the possible protective effects of capsicums and capsaicin against colonic diseases, including colitis. Kihara et al. reported that capsaicin could ameliorate dextran sulphate sodium-induced colitis through TRPV1 receptor activation57. Additionally, Mi et al. reported a significant correlation between the frequency of chilli consumption and the incidence of colitis58. This study supports the previous perspective, indicating that prolonged capsicum intake may jeopardise colon health. The underlying mechanisms for these observations may be attributed to factors including oxidative stress and inflammation; however, a more comprehensive analysis is essential to clarify the precise processes involved.
The limitations of this study are primarily focused on its analysis of the effects of high-fat and chilli diets on the morphological alterations in digestive organ tissues. The research notably failed to investigate the underlying mechanisms that may correlate inflammation, lipid metabolism, and the resultant damage to digestive organs. Future investigations should consider integrating lipidomics, proteomics, molecular biology, and other multi-omics methodologies. These comprehensive methodologies would facilitate a multi-dimensional analysis, yielding deeper insights into the key pathological mechanisms involved.
This study demonstrated that prolonged high-fat and chilli-based diet intake may adversely affect digestive organs, including the liver, stomach, gallbladder, and colon. The underlying mechanism seems to be closely associated with inflammatory responses, which cause damage to these organs and subsequently impair cholesterol metabolism. This impairment may further exacerbate lipid metabolic disorders. Although inflammation is a crucial factor in various pathological processes, the specific mechanisms require additional investigation. This research highlights the detrimental effects of prolonged chilli consumption on digestive health to inform dietary recommendations for optimal human health.
Methods
Materials
Animals and feed
This study included 24 specific pathogen-free-grade Hartley strain guinea pigs (male; 200–220 g) acquired from Beijing Vital River Laboratory Animal Technology Co. Inc. (Permit No.: SCXK (Beijing) 2021-0011). The guinea pigs were housed for 1 week in experimental animal rooms maintained at 20–24 °C and humidity levels of 45–55% for 1 week for acclimatisation. The rooms featured a 12-hour light and dark cycle. All the animal experimental procedures were conducted in accordance with the guidelines for the care and use of laboratory animals and were approved by the Inner Mongolia Medical University Animal Ethics Committee (ethics approval number: YKD202302058). The feed and high-fat feed were acquired from Beijing Xiaoshu Youtai Company (License No. SCXK (Beijing) 2018-0006), while the Capsicum annuum var. conoides were procured from Sichuan Honglin Food Co. Ltd (License No. SC1035 SC10351018201640)). The Capsicum feed was produced by Beijing Xiaoshu Youtai Company. (Table 1.)
Reagents
The biochemistry test kit was obtained from Wuhan Colorful Gene Biological Technology Co., China it included the following: triglyceride (TG, catalogue number. 230213201), TC (catalogue number. 230629102), HDL-c (catalogue number. 230308201), LDL-c (catalogue number. 230811201). The enzyme-linked immunosorbent assay test kit was obtained from Wuhan Colourful Gene Biological Technology Co., China. It comprised the following: tumour necrosis factor-α (TNF-α, catalogue number. JYM0025Gu), interleukin-1β (IL-1β, catalogue number. JYM0001Gu), and interleukin-6 (IL-6, catalogue number. JYM0017Gu). Pathological morphology examination reagents were obtained from Shanghai YuanYe Bio-Technology Co., China. The key reagents included 4% paraformaldehyde, ethanol, xylene, and haematoxylin staining solutions.
Methods
Model preparation
The 24 guinea pigs were randomly divided into a high-fat diet (HFD group; n = 8), capsicum diet (CD group; n = 8), and control (C group; n = 8) using a random grouping method based on body weight. The specific model construction techniques included: (a) The maintenance feed was given to the C group guinea pigs. (b) The high-fat feed was given to the HFD group guinea pigs. (c) The capsicum annuum var. conoides content feed was given to the CD group guinea pigs. The model cycle lasted for 90 days.
Sample collection
On day 91, the guinea pigs were anaesthetised through intraperitoneal injection of 45 mg/kg sodium pentobarbital. After anaesthesia, the guinea pig was placed on a surgical table and subjected to an abdominal incision, and 5 mL of blood was extracted from the abdominal aorta for biochemical and enzyme-linked immunosorbent assays. The blood was centrifuged at 3000 rpm, and the supernatant obtained was stored in a freezer at −80 °C. The liver and gallbladder were excised and immersed in a 4% paraformaldehyde solution for stabilisation after the blood vessels and ligaments were severed. Subsequently, the stomach of the guinea pig was incised with dissecting scissors along a wider arc after the clamping of the gastric cardia. The contents of the stomach were cleansed with saline, and the stomach tissue was stabilised with a 4% paraformaldehyde solution. Subsequently, 5 cm of the distal segment of the colon was incised, and the intestinal contents were cleaned with saline, and the colon tissue was preserved in a 4% paraformaldehyde solution.
Serum biochemical analysis
This study used biochemical assays to assess the serum lipid indices in guinea pigs. These markers included TC, HDL cholesterol, LDL cholesterol, and triglycerides. The biochemical assay protocols and procedures were carefully followed during testing, and all tests were performed according to the manufacturer’s instructions.
Enzyme-linked immunosorbent assay
The collected blood samples were centrifuged for 20 min at 3000 rpm. Standard and samples were prepared as follows: We added 100 µL of a standard solution with varying concentrations to the standard wells, followed by 40 µL of the sample diluent. Subsequently, we added 10 µL of the serum sample to the wells. We ensured that no sample or enzyme reagent was added to the control wells. We filled each standard and sample well with 50 µL of the enzyme reagent, excluding the empty wells. The reaction wells were covered with a sealing membrane and incubated at 7 °C for 30 min. After incubation, the liquid was carefully removed, and the wells were gently pat dried. The washing solution was added to each well and subsequently drained. Subsequently, we added 50 µL of the enzyme reagent into each standard and sample well. We covered the reaction wells with a sealing membrane and allowed them to sit at 7 °C for 30 min. After the liquid had been removed and gently dried, the washing solution was added to each well. After 30 s, we drained the liquid and repeated the process five times, ensuring that the wells were gently dried after each wash. Subsequently, 50 µL of dye A and 50 µL of dye B were added to each well. The contents were thoroughly mixed and incubated in the dark at 37 °C for 10 min to develop the desired colour you want. We added 50 µL of the stop solution to each well to stop the reaction. After calibrating the empty wells to zero, the absorbance (OD) of each well was measured at 450 nm within 15 min.
Histopathology
Tissue samples from the liver, stomach, gallbladder, and colon were fixed in 10% formaldehyde and subsequently wrapped in 75% ethanol overnight. The tissues were dehydrated in 95% ethanol and cleared using xylene. Cleared tissue samples were embedded in paraffin molds, soaked for 3 h, and sectioned into 5-mm-thick slices. The sections were stained with HE, examined under a microscope, and photographed.
Statistical analysis
Statistical Package for the Social Sciences software (version 28.0) was utilised for data analysis. A t-test or rank-sum test was used for comparisons between the two groups. The data are presented as mean ± standard deviation/standard error of the mean. Student’s t-tests were used to compare the effects of the two groups. GraphPad software (version 9.5) was used to create statistical graphs.
Data availability
We declare that the data supporting the results of this study can be found within this article, and the data atlas has been submitted as supplementary material to the providing system.
References
Głąbska, D., Guzek, D., Groele, B. & Gutkowska, K. Fruit and vegetable intake and mental health in adults. Syst. Rev. Nutrients. 12 (1), 115. https://doi.org/10.3390/nu12010115 (2020).
Iłowiecka, K. et al. Lifestyle, eating habits, and health behaviors among dietary supplement users in three European countries. Front. Public. Health. 10, 892233. https://doi.org/10.3389/fpubh.2022.892233 (2022).
Stewart, S., Keates, A. K., Redfern, A. & McMurray, J. J. V. Seasonal variations in cardiovascular disease. Nat. Rev. Cardiol. 14 (11), 654–664. https://doi.org/10.1038/nrcardio.2017.76 (2017).
McMichael, A. J. & Lindgren, E. Climate change: present and future risks to health, and necessary responses. J. Intern. Med. 270 (5), 401–413. https://doi.org/10.1111/j.1365-2796.2011.02415.x (2011).
Fujiwara, H. et al. Life habits and mental health: behavioural addiction, health benefits of daily habits, and the reward system. Front. Psychiatry. 13, 813507. https://doi.org/10.3389/fpsyt.2022.813507 (2022).
IHME Pathogen Core Group. Global burden associated with 85 pathogens in 2019: a systematic analysis for the global burden of disease study 2019. Lancet Infect. Dis. 24 (8), 868–895. https://doi.org/10.1016/S1473-3099(24)00158-0 (2024).
Mollica, R. F. et al. Mental health in complex emergencies. Lancet (London England). 364 (9450), 2058–2067. https://doi.org/10.1016/S0140-6736(04)17519-3 (2004).
Garry, S. & Checchi, F. Armed conflict and public health: into the 21st century. J. Public Health. 42 (3), e287–e298. https://doi.org/10.1093/pubmed/fdz095 (2020).
Keles, U., Kalem-Yapar, N. E., Hultén, H., Zhao, L. N. & Kaldis, P. Impact of Short-Term lipid overload on Whole-Body physiology. Mol. Cell. Biol., 1–12. (2024). Advance online publication.
Laufs, U., Parhofer, K. G., Ginsberg, H. N. & Hegele, R. A. Clinical review on triglycerides. Eur. Heart J. 41 (1), 99–109c. https://doi.org/10.1093/eurheartj/ehz785 (2020).
Nussbaumerova, B. & Rosolova, H. Obesity and dyslipidemia. Curr. Atheroscler. Rep. 25 (12), 947–955. https://doi.org/10.1007/s11883-023-01167-2 (2023).
Feingold, K. R. The effect of diet on cardiovascular disease and lipid and lipoprotein levels. In (ed Feingold, K. R.) et. Al., Endotext. MDText.com, Inc. (2024).
Joo, H. K. et al. Protective role of dietary Capsanthin in a mouse model of nonalcoholic fatty liver disease. J. Med. Food. 24 (6), 635–644. https://doi.org/10.1089/jmf.2020.4866 (2021).
Chen, Z. et al. Dietary supplementation with capsaicinoids alleviates obesity in mice fed a high-fat-high-fructose diet. Food Funct. 15 (16), 8572–8585. https://doi.org/10.1039/d4fo02102a (2024).
Tchernof, A. & Després, J. P. Pathophysiology of human visceral obesity: an update. Physiol. Rev. 93 (1), 359–404. https://doi.org/10.1152/physrev.00033.2011 (2013).
Musso, G., Gambino, R. & Cassader, M. Cholesterol metabolism and the pathogenesis of non-alcoholic steatohepatitis. Prog. Lipid Res. 52 (1), 175–191. https://doi.org/10.1016/j.plipres.2012.11.002 (2013).
Larabi, A., Barnich, N. & Nguyen, H. T. T. New insights into the interplay between autophagy, gut microbiota and inflammatory responses in IBD. Autophagy 16 (1), 38–51. https://doi.org/10.1080/15548627.2019.1635384 (2020).
Herbert, K. E. & Erridge, C. Regulation of low-density lipoprotein cholesterol by intestinal inflammation and the acute phase response. Cardiovascular. Res. 114 (2), 226–232. https://doi.org/10.1093/cvr/cvx237 (2018).
Zeng, H., Umar, S., Rust, B., Lazarova, D. & Bordonaro, M. Secondary bile acids and short chain fatty acids in the colon: A focus on colonic microbiome, cell proliferation, inflammation, and Cancer. Int. J. Mol. Sci. 20 (5), 1214. https://doi.org/10.3390/ijms20051214 (2019).
Cai, J., Rimal, B., Jiang, C., Chiang, J. Y. L. & Patterson, A. D. Bile acid metabolism and signaling, the microbiota, and metabolic disease. Pharmacol. Ther. 237, 108238. https://doi.org/10.1016/j.pharmthera.2022.108238 (2022).
de Vallim, A., Tarling, T. Q., Edwards, P. A. & E. J., & Pleiotropic roles of bile acids in metabolism. Cell Metabol. 17 (5), 657–669. https://doi.org/10.1016/j.cmet.2013.03.013 (2013).
Winston, J. A. & Theriot, C. M. Diversification of host bile acids by members of the gut microbiota. Gut Microbes. 11 (2), 158–171. https://doi.org/10.1080/19490976.2019.1674124 (2020).
Brown, E. M., Clardy, J. & Xavier, R. J. Gut Microbiome lipid metabolism and its impact on host physiology. Cell. Host Microbe. 31 (2), 173–186. https://doi.org/10.1016/j.chom.2023.01.009 (2023).
Tan, B. L. & Norhaizan, M. E. Effect of High-Fat diets on oxidative stress, cellular inflammatory response and cognitive function. Nutrients 11 (11), 2579. https://doi.org/10.3390/nu11112579 (2019).
Binayi, F., Moslemi, M., Khodagholi, F., Hedayati, M. & Zardooz, H. Long-term high-fat diet disrupts lipid metabolism and causes inflammation in adult male rats: possible intervention of Endoplasmic reticulum stress. Arch. Physiol. Biochem. 129 (1), 204–212. https://doi.org/10.1080/13813455.2020.1808997 (2023).
Malesza, I. J. et al. High-Fat, Western-Style diet, systemic inflammation, and gut microbiota. Narrative Rev. Cells. 10 (11), 3164. https://doi.org/10.3390/cells10113164 (2021).
Bal, S. et al. Biomedical and antioxidant potentialities in Chilli: perspectives and way forward. Molecules (Basel Switzerland). 27 (19), 6380. https://doi.org/10.3390/molecules27196380 (2022).
Xiang, Q. et al. Capsaicin, the spicy ingredient of Chili peppers: effects on Gastrointestinal tract and composition of gut microbiota at various dosages. Foods (Basel Switzerland). 11 (5), 686. https://doi.org/10.3390/foods11050686 (2022).
Arita, S., Kinoshita, Y., Ushida, K., Enomoto, A. & Inagaki-Ohara, K. High-fat diet feeding promotes stemness and precancerous changes in murine gastric mucosa mediated by leptin receptor signaling pathway. Arch. Biochem. Biophys. 610, 16–24. https://doi.org/10.1016/j.abb.2016.09.015 (2016).
François, M. et al. High-fat diet increases ghrelin-expressing cells in stomach, contributing to obesity. Nutrition 32 (6), 709–715. https://doi.org/10.1016/j.nut.2015.12.034 (2016).
Sato, T. et al. Physiological roles of Ghrelin on obesity. Obes. Res. Clin. Pract. 8 (5), E405–E413. https://doi.org/10.1016/j.orcp.2013.10.002 (2014).
van Loenen, M. R., Geenen, B., Arnoldussen, I. A. C. & Kiliaan, A. J. Ghrelin as a prominent endocrine factor in stress-induced obesity. Nutr. Neurosci. 25 (7), 1413–1424. https://doi.org/10.1080/1028415x.2020.1863740 (2022).
Merritt, J. C. et al. Anti-cancer activity of sustained release capsaicin formulations. Pharmacol. Ther. 238, 108177. https://doi.org/10.1016/j.pharmthera.2022.108177 (2022).
Wang, F. et al. Extraction, purification, bioactivity and Pharmacological effects of capsaicin: a review. Crit. Rev. Food Sci. Nutr. 62 (19), 5322–5348. https://doi.org/10.1080/10408398.2021.1884840 (2022).
Myers, B. M., Smith, J. L. & Graham, D. Y. Effect of red pepper and black pepper on the stomach. Am. J. Gastroenterol. 82 (3), 211–214 (1987).
Luo, L., Yan, J., Wang, X. & Sun, Z. The correlation between Chili pepper consumption and gastric cancer risk: A meta-analysis. Asia Pac. J. Clin. Nutr. 30 (1), 130–139. https://doi.org/10.6133/apjcn.202103_30(1).0016 (2021).
Bley, K., Boorman, G., Mohammad, B., McKenzie, D. & Babbar, S. A comprehensive review of the carcinogenic and anticarcinogenic potential of capsaicin. Toxicol. Pathol. 40 (6), 847–873. https://doi.org/10.1177/0192623312444471 (2012).
López-Carrillo, L., Hernández Avila, M. & Dubrow, R. Chili pepper consumption and gastric cancer in Mexico: a case-control study. Am. J. Epidemiol. 139 (3), 263–271. https://doi.org/10.1093/oxfordjournals.aje.a116993 (1994).
Ravichandra, A. (ed F. Schwabe, R.) Mouse models of liver fibrosis. Methods Mol. Biology (Clifton N J) 2299 339–356 https://doi.org/10.1007/978-1-0716-1382-5_23 (2021).
Lian, C. Y., Zhai, Z. Z., Li, Z. F. & Wang, L. High fat diet-triggered non-alcoholic fatty liver disease: A review of proposed mechanisms. Chemico-Biol. Interact. 330, 109199. https://doi.org/10.1016/j.cbi.2020.109199 (2020).
Li, X. et al. Establishment of a non-alcoholic fatty liver disease model by high fat diet in adult zebrafish. Anim. Models Experimental Med. 7 (6), 904–913. https://doi.org/10.1002/ame2.12309 (2024).
42.Li, H. et al. Hepatocyte adenosine kinase promotes excessive fat deposition and liver inflammation. Gastroenterology 164 (1), 134–146. https://doi.org/10.1053/j.gastro.2022.09.027 (2023).
Tsuchida, T. et al. A simple diet- and chemical-induced murine NASH model with rapid progression of steatohepatitis, fibrosis and liver cancer. J. Hepatol. 69 (2), 385–395. https://doi.org/10.1016/j.jhep.2018.03.011 (2018).
Chaikoff, I. L., Eichorn, K. B., Connor, C. L. & Entenman, C. The production of cirrhosis in the liver of the normal dog by prolonged feeding of a High-Fat diet. Am. J. Pathol. 19 (1), 9–21 (1943).
Karimi-Sales, E., Mohaddes, G. & Alipour, M. R. Hepatoprotection of capsaicin in alcoholic and non-alcoholic fatty liver diseases. Arch. Physiol. Biochem. 130 (1), 38–48. https://doi.org/10.1080/13813455.2021.1962913 (2024).
Sheng, J. P., Zhang, B. H., Chen, Y. F. & Yu, F. X. Capsaicin attenuates liver fibrosis by targeting Notch signaling to inhibit TNF-α secretion from M1 macrophages. Immunopharmacol. Immunotoxicol. 42 (6), 556–563. https://doi.org/10.1080/08923973.2020.1811308 (2020).
Shin, M. K., Yang, S. M. & Han, I. S. Capsaicin suppresses liver fat accumulation in high-fat diet-induced NAFLD mice. Anim. Cells Syst. 24 (4), 214–219. https://doi.org/10.1080/19768354.2020.1810771 (2020).
Xie, Z. Q. et al. Capsaicin suppresses hepatocarcinogenesis by inhibiting the stemness of hepatic progenitor cells via SIRT1/SOX2 signaling pathway. Cancer Med. 11 (22), 4283–4296. https://doi.org/10.1002/cam4.4777 (2022).
Kim, M. S. et al. Causal effect of adiposity on the risk of 19 Gastrointestinal diseases: a Mendelian randomization study. Obesity 31 (5), 1436–1444. https://doi.org/10.1002/oby.23722 (2023).
Mathur, A. et al. Steatocholecystitis: the influence of obesity and dietary carbohydrates. J. Surg. Res. 147 (2), 290–297. https://doi.org/10.1016/j.jss.2007.04.042 (2008).
Di Ciaula, A. et al. The role of diet in the pathogenesis of cholesterol gallstones. Curr. Med. Chem. 26 (19), 3620–3638. https://doi.org/10.2174/0929867324666170530080636 (2019).
Parra-Landazury, N. M., Cordova-Gallardo, J. & Méndez-Sánchez, N. Obesity and gallstones. Visc. Med. 37 (5), 394–402. https://doi.org/10.1159/000515545 (2021).
Báez, S. et al. Genetic variants involved in gallstone formation and capsaicin metabolism, and the risk of gallbladder cancer in Chilean women. World J. Gastroenterol. 16 (3), 372–378. https://doi.org/10.3748/wjg.v16.i3.372 (2010).
Tsuchiya, Y. et al. Mutagenicity and mutagens of the red Chili pepper as gallbladder Cancer risk factor in Chilean women. Asian Pac. J. Cancer Prev. 12 (2), 471–476 (2011). Retrieved from < Go to ISI>://WOS:000293172800025
Li, X. et al. High-fat diet promotes experimental colitis by inducing oxidative stress in the colon. Am. J. Physiology-Gastrointestinal Liver Physiol. 317 (4), G453–G462. https://doi.org/10.1152/ajpgi.00103.2019 (2019).
Engel, M. A. et al. The proximodistal aggravation of colitis depends on substance P released from TRPV1-expressing sensory neurons. J. Gastroenterol. 47 (3), 256–265. https://doi.org/10.1007/s00535-011-0495-6 (2012).
Kihara, N. et al. Vanilloid receptor-1 containing primary sensory neurones mediate dextran sulphate sodium induced colitis in rats. Gut 52 (5), 713–719. https://doi.org/10.1136/gut.52.5.713 (2003).
Mi, L. et al. Dietary risk factors for inflammatory bowel disease in Shanghai: A case-control study. Asia Pac. J. Clin. Nutr. 31 (3), 405–414 (2022). doi:ARTN 95439610.6133/apjcn.202209_31(3).0008.
Acknowledgements
This research was supported by several projects, including the Inner Mongolia Autonomous Region Science and Technology Project(Investigations into Mongolian medicinal practices have focused on the creation and application of bear bile substitutes, particularly their anti-diabetic and pancreatic regeneration properties). Inner Mongolian Medical University’s Mongolian Pharmaceutical “First Class Program” Project (MYX2022-K01), the Inner Mongolian Medical University’s Mongolian Pharmaceutical “First Class Program” Graduate Research Capacity Enhancement Program (MYX2022-R08), the Inner Mongolian Medical University’s Mongolian medicine “First Class Program” Graduate Research Innovation Program (2022 MYYLXKYC009), and the Inner Mongolian Coordinating Innovation’s Mongolian Medical Research Center’s Graduate Research Capacity Enhancement Program (MYXXTBS202309), and the Education Department of Inner Mongolia Autonomous Region Project (Biological Basis of Atherosclerotic Heat and Cold Classification-B20231119Z).
Author information
Authors and Affiliations
Contributions
Wen-Xiang Guan wrote the paper. Wen-Xiang Guan, Zhuo-Lan, and Jing-Xian Gao contributed equally to this article. Wen-Xiang Guan is the first author, while Zhuo-Lan and Jing-Xian Gao are co-first authors. Wen-Xiang Guan and Xiao-Jun Luo primarily conducted the experimental procedures, and Zhuo Lan prepared Figs. 1, 2 and 3. Jing-Xian Gao and Chang-xi Bai supervised the experimental operations and manuscript writing, and all authors reviewed the manuscript. Chang-Xi Bai as the corresponding author and Xiao-Jun Luo as the co-corresponding author.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical statement
All the animal experimental procedures were conducted in accordance with the guidelines for the care and use of laboratory animals and were approved by the Inner Mongolia Medical University Animal Ethics Committee (ethics approval number: YKD202302058). This study is reported based on the ARRIVE guidelines.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Guan, WX., Zhuo-Lan, Luo, XJ. et al. Comparative study on the effects of high fat diet and capsicum diet on the digestive organs of guinea pigs. Sci Rep 15, 17886 (2025). https://doi.org/10.1038/s41598-025-93583-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-93583-4