Abstract
Some clinical algorithms incorporate an individual’s race, ethnicity, or both as an input variable or predictor in determining diagnoses, prognoses, treatment plans, or risk assessments. Inappropriate use of race and ethnicity in clinical algorithms at the point of care may exacerbate health disparities and promote harmful practices of race-based medicine. Using database analysis primarily, we identified 42 risk calculators that use race and ethnicity as predictors, five laboratory test results with reference ranges that differed based on race and ethnicity, one therapy recommendation based on race and ethnicity, 15 medications with race- and ethnicity-based initiation and monitoring guidelines, and five medical devices with differential racial and ethnic performances. Information on these clinical algorithms is freely available at https://www.clinical-algorithms-with-race-and-ethnicity.org/. This resource aims to raise awareness about the use of race and ethnicity in clinical algorithms and track progress toward eliminating their inappropriate use. The database is actively updated to include clinical algorithms that were missed and additional characteristics of these algorithms.
Similar content being viewed by others
Introduction
Clinical algorithms are tools that aid decision-making in a variety of medical conditions and procedures. Examples include diagnostic calculators that assess the current presence of a disease or condition, prognostic algorithms that predict the future risk of a disease or health outcome1, treatment guidelines for managing chronic conditions, interpretation recommendations for laboratory test results, and precision directions for medication use2,3. Such algorithms enable standardization of care, increased efficiency, and improved clinical decision-making quality2.
Some clinical algorithms incorporate the individual’s race, ethnicity, or both as an input variable or predictor. In medicine, race and ethnicity are used to describe certain population characteristics that may have implications for health and healthcare. While these terms are often used interchangeably, they each have distinct meanings and refer to separate aspects of human identity and ancestry4. Race is a categorization system that classifies individuals based on visible physical traits such as skin color, facial features, hair texture, and eye shape. Influenced by historical and political factors, race has been used to classify people into broad groups, such as White, Black, or Asian, among several others. In contrast, ethnicity is a categorization system that groups people based on language, religion, traditions, and other aspects of shared cultural heritage passed down through generations. Shaped by ancestry and geographical location, ethnicity has been used to classify people into culturally distinct groups, such as Hispanic, Chinese, or Navajo, among many others. Despite the distinction between race and ethnicity, clinical algorithms sometimes use the term race to refer to both race and ethnicity and, at other times, to refer to only race.
Race and ethnicity are widely used in medicine to study genetic variations, disease prevalence, treatment responses, and disparities in health and healthcare. However, using race and ethnicity as proxies for genetic differences or, more broadly, biological differences may oversimplify complex health issues and have the potential to contribute to disparities when not carefully contextualized. Frequent causes of health disparities include, among others, environmental, socioeconomic, healthcare access, discrimination, and cultural factors. Although clinical algorithms incorporating race and ethnicity are intended to improve healthcare, they can inadvertently exacerbate healthcare disparities in several ways. They may embed racial and ethnic prejudices and stereotypes arising from historical and societal biases and can inadvertently reinforce these stereotypes. Medical students are taught to associate race and ethnicity with diseases such as sickle cell anemia, sarcoidosis, or cystic fibrosis, which reinforces their use as proxies for the biological bases of disease5. Using race and ethnicity as an alternative for genetic variation oversimplifies the complex interactions between genes, environment, and disease6; furthermore, there is more genetic variation within racial and ethnic categories than across them7. Thus, the use of race and ethnicity in clinical algorithms may incorrectly presume genetic and biological differences between such groups and may result in incorrect diagnoses or inadequate treatment in some groups8. Further, the use of race and ethnicity in clinical algorithms raises ethical concerns regarding discrimination, equity, and equality of opportunity9. It may violate the principles of justice and equality if individuals are treated differently based on their race and ethnicity instead of their individual health needs.
Race and ethnicity are now widely accepted as historical and social constructs rather than biological ones, and their use in clinical decision-making has come under increasing scrutiny. Several high-profile articles have identified and deemed problematic such clinical algorithms in a range of clinical specialties, such as nephrology10, urology11, obstetrics12, and cardiology5,13,14. Further, medical organizations such as the American Academy of Pediatrics15, the National Kidney Foundation and the American Society of Nephrology16, and the American College of Obstetricians and Gynecologists17 have recommended the elimination of race and ethnicity from algorithms in current use.
However, it is not clear that the inclusion of race and ethnicity as predictors to inform clinical decision-making will always perpetuate long-standing healthcare disparities18. Until recently, it was assumed that clinical prediction algorithms should include all patient variables, biological or not, with predictive power to produce more accurate predictions. A recent study showed that dropping race and ethnicity from algorithms may unexpectedly propagate healthcare inequities9. Thus, the impact of including race and ethnicity in clinical algorithms can range from occasionally beneficial (when they are included to reduce disparities), neutral (when their inclusion has no effect), and harmful (when historically underserved populations are disadvantaged by race- and ethnicity-based medicine)19,20. Therefore, it is necessary to analyze each algorithm systematically to identify the best way to improve it. The appropriate course of action for a particular algorithm may be to either change the algorithm to exclude race and ethnicity, use a substitute for race and ethnicity, such as a genetic marker or a measure of social determinants of health, or retire the algorithm and replace it with an alternative that promotes equity21. However, several practical obstacles exist to develop and implement changes. These include gathering and utilizing new data for assessing an existing algorithm and developing an alternative22, comprehensively analyzing the impact of an alternative algorithm23, advocating for increased transparency regarding the role of race and ethnicity in an algorithm24, educating clinicians and patients on interpreting results, and ensuring that an updated algorithm is widely used.
Our goal in this study was to create an up-to-date database of clinical algorithms that include race and ethnicity as predictors. It is a resource for raising awareness of the use of race and ethnicity in clinical decision-making and tracking the progress made toward eliminating their inappropriate use. We conducted a systematic search and analysis of databases and published literature to identify clinical algorithms, medications, and medical devices that use race and ethnicity.
Clinical algorithms include risk calculators in diagnostic and prognostic settings, flowcharts, lookup tables, nomograms, and guidelines. A risk calculator uses a mathematical equation or a statistical model to assess the presence of a disease (diagnostic calculator) or predict the risk of future disease onset (prognostic calculator), such as assessing current osteoporosis status and predicting future fracture risk associated with osteoporosis. A flowchart is a branching decision tree, such as a diagnostic flowchart for determining the etiology of chest pain. A lookup table enables quick reference of data, such as a table containing energy and nutritional content of various foodstuffs. A nomogram is a graphical tool used for a specific calculation, such as a nomogram of height and weight measurements used to find the surface area of a person. We focused on identifying and cataloging clinical algorithms such as risk calculators that use race and ethnicity as predictors, laboratory test results with reference ranges that differed based on race and ethnicity, therapy recommendations based on race and ethnicity, medications with race- and ethnicity-based initiation and monitoring guidelines, and medical devices with differential racial and ethnic performances.
While an individual’s race and ethnicity directly influence the results generated by these clinical algorithms, such algorithms typically include other factors such as demographics, comorbidities, and laboratory test findings, which may have a greater impact on the result than race and ethnicity. Furthermore, while an alternative algorithm that does not use race and ethnicity will alter the results for all individuals compared to the original algorithm, clinical decisions based on these results will likely change for only a small subset of individuals25. Thus, a fine-grained examination of each algorithm is necessary to determine the extent of the impact of using race and ethnicity.
Results
We report separately clinical calculators with race and ethnicity (including risk calculators, laboratory tests, and therapy recommendations), medications with guidelines based on race and ethnicity, and devices with differential racial and ethnic performances.
Clinical calculators
We identified 191 internet resources with clinical calculators, of which 37 met the inclusion criteria, and 208 peer-reviewed articles, of which three met the inclusion criteria (Fig. 1). After merging the lists of calculators identified from the internet resources and the three articles, the final list contained 45 calculators. Since the online database was published, the public has contributed three additional calculators, bringing the total to 48. Detailed information for each calculator is provided in the online database.
Selection of clinical calculators with race- and ethnicity-based guidelines. *Exclusion criteria for internet resources, with numbers excluded. Each excluded resource is counted only against the first exclusion criterion that was met: Lacked contact information = 33; Provided no references to peer-reviewed articles = 20; Provided only hyperlinks to external websites = 53; Described only smartphone apps for calculators = 12; Did not implement calculators for online data entry and result output = 36; **Exclusion criteria for articles, with numbers excluded. Each excluded article is counted only against the first exclusion condition that was met: Not peer-reviewed (e.g., preprint) = 16; Did not contain a table or list with more than one clinical calculator with race and ethnicity = 189.
Among the internet resources (see Supplementary Information), MDCalc, UpToDate Medical Calculators, and MDApp are the most comprehensive. MDCalc is widely used globally; in the U.S., over 65% of physicians use it monthly26. UpToDate is a widely used point-of-care database containing a comprehensive calculator resource27. MDApp is a U.K.-based company that implements clinical calculators. The MD Anderson Cancer Center has created several cancer-related calculators to predict survival, clinical outcomes, and treatment response.
Based on intended use, the clinical calculators were categorized into risk calculators, laboratory tests, and therapy recommendations (see Table 1). The calculators were also grouped into medical specialties, country of origin, model type, output type, and target user. The rationale for using race and ethnicity was mainly based on a statistical analysis of epidemiological data that found racial and ethnic differences. Seven of the 48 calculators have been modified to exclude race and ethnicity as predictors (Anemia in pregnancy, ASCVD Risk Calculator, MDRD GFR Equation, Kidney Donor Risk Index (KDRI), Spirometry Reference Value Calculator, Vaginal Birth After Cesarean (VBAC) and UTICalc).
Race and ethnicity are treated as separate predictors in only three calculators (Predict COVID-19 Test Result, Predict Hospitalization Risk for COVID-19 Positive, and Kidney Donor Risk Index); in the majority of the calculators, race and ethnicity are treated as a single predictor or only race is included as a predictor. There were 49 distinct race and ethnicity categories, and common categories included White, Black, other, Asian, Caucasian, East Asian, mixed, and South Asian. The category “other” is commonly used to lump groups with small sample sizes for analysis, and most online calculators do not identify which groups are included in the “other” category.
Medications
From Micromedex, we identified 47 (keyword: ancestry), 108 (keyword: descent), 133 (keyword: ethnicity), 17 (keyword: heritage), and 5 (keyword: peoples) medications with potential race- and ethnicity-based guidelines. After removing duplicates and applying the exclusion criteria, the final list contained 15 medications for which we verified that the U.S Food and Drug Administration (FDA) Drug Product Labeling included guidelines based on race and ethnicity (see Fig. 2). Detailed information for each medication is provided in the online database. Based on how race and ethnicity were used, medications were categorized into those with race- and ethnicity-based indication, race- and ethnicity-based dose adjustment, race- and ethnicity-based monitoring, and race- and ethnicity-based pharmacogenetic screening (see Table 2). The rationale for using race and ethnicity was mainly based on a statistical analysis of epidemiological data that found differences in genetics or pharmacokinetics based on race and ethnicity.
Selection of medications with guidelines based on race and ethnicity. *Exclusion criteria for medications, with numbers excluded. Each excluded medication is counted only against the first exclusion criterion that was met: Was a combination of multiple drugs and one of the constituent drugs was already included as a single medication = 43; Had no FDA Drug Label Information = 16; The FDA Drug Label Information did not contain race and ethnicity-based guidelines = 155.
Medical devices
We identified 83 peer-reviewed articles, of which four met the inclusion criteria (Fig. 3). Detailed information for each medical device is provided in the online database. Devices were divided into categories based on the source of differential performance, which included skin color and scalp hair characteristics (Table 3). Inadequate calibration on sufficiently diverse populations is the most likely source of skin color-related performance differences.
Over the last decade, a great number of medical software have been developed that use artificial intelligence (AI) and machine learning (ML) and are regulated by the FDA as AI/ML-based software as a medical device (SaMD). We excluded these medical devices since almost all of them lack publicly available data that would allow us to determine whether race and ethnicity are used as inputs in the AI/ML model.
Discussion
Clinical algorithms are embedded in electronic health records, clinical guidelines, and decision support tools, and it is feared that the use of race- and ethnicity-based algorithms may lead to disparities in healthcare, especially in minority populations. As our understanding of race and ethnicity in medicine evolves, efforts are being made to investigate their role in clinical tools. Recently, the Agency for Healthcare Research and Quality conducted a stakeholder review of 18 healthcare algorithms based on race and ethnicity13. With the beginning of this new era, it is crucial for the medical community to have an up-to-date catalog of clinical algorithms that use race and ethnicity in order to anticipate and measure progress in evaluating and mitigating the bias in these tools. We conducted an exhaustive search of internet resources and databases, the scientific literature, and the FDA Drug Label Information and identified 42 risk calculators that use race and ethnicity as predictors, five laboratory test results with reference ranges that differed based on race and ethnicity, one therapy recommendation based on race and ethnicity, 15 medications with race- and ethnicity-based initiation and monitoring guidelines, and five medical devices with differential racial and ethnic performances. Information on these clinical algorithms is available in an online database at https://www.clinical-algorithms-with-race-and-ethnicity.org/.
A key issue is the lack of standardization in the racial and ethnic categorization systems currently in use. Typically, an optimal categorization system has consistent definitions for universally applicable categories, and the categories are mutually exclusive. A good system is also complete and capable of absorbing entities that have not yet been identified without requiring system revisions. All of these features are lacking in racial and ethnic categorization systems. There is no universal global racial and ethnic categorization system in use across the world. The Office of Management and Budget in the U.S. defines six racial categories: White, Black or African American, American Indian or Alaskan Native, Asian, Native Hawaiian or Other Pacific Islander, and Middle Eastern or North African, as well as two ethnic categories: Hispanic or Latino and not Hispanic or Latino. In the U.K., the Office of National Statistics defines five high-level ethnic categories: “Asian, Asian British, Asian Welsh,” “Black, Black British, Black Welsh, Caribbean or African,” “Mixed or Multiple,” “White,” and “Other ethnic group.” These systems make racial and ethnic categories difficult to define in practice, and there are no well-defined rules governing what constitutes a racial or ethnic category a person belongs to. For example, Caucasians are often called Whites or Europeans, even though many Caucasians are neither, and Blacks are often called Africans, even though many Blacks are not African. Because racial and ethnic categories are not mutually exclusive, individuals can simultaneously belong to multiple racial and ethnic categories. Finally, the addition of new racial and ethnic categories leads to rearrangements of the system. For example, in 1977, the U.S. Census Bureau established four racial categories, including White, Black, American Indian or Alaskan Native, and Asian or Pacific Islander. Two decades later, the Bureau split the Asian or Pacific Islander category into two, namely Asian and Native Hawaiian and Pacific Islander categories. And, in 2024, the Bureau added the new racial category of Middle Eastern and North African. Further, racial and ethnic categories are used inconsistently in the research literature and data sets. A recent review showed that the U.S. racial categories of White, Black, and Asian mapped to 66, 62, and 49 different racial or ethnic categories, respectively28. This lack of standardization leads to ambiguities in operationalizing race- and ethnicity-based algorithms for clinical use. For example, guidelines are silent on how race adjustment should be applied to a patient with a White mother and a Black father14.
Concerns regarding the inappropriate use of race and ethnicity in clinical algorithms have prompted calls for their elimination as inputs in clinical algorithms both in the academic literature and by organizations such as the Coalition to End Racism in Clinical Algorithms29 and the Kaiser Family Foundation30. According to recent reports from the Council of Medical Specialty Societies (CMSS) and the National Academies of Sciences, Engineering, and Medicine (NASEM), the impact of race and ethnicity in clinical algorithms can be beneficial (if race and ethnicity are included in an intentional, well-considered effort to reduce inequities), neutral (have no impact), or harmful (if the algorithm perpetuates clinical decisions that harm historically marginalized populations). As a result, each algorithm must be reviewed individually to determine whether race and ethnicity should be retained, removed, or replaced with an alternative such as a socioeconomic determinants of health measure. Several national efforts are in progress. The Doris Duke Foundation has funded several organizations, including the American Academy of Pediatrics, the American Heart Association, the American Society of Hematology, the Coalition to End Racism in Clinical Algorithms, the CMSS, and the NASEM to reexamine clinical algorithms and validate them through rigorous research. The CMSS launched the Encoding Equity Alliance in 2024 to identify inappropriate use of race and ethnicity in algorithms and guidelines and help redesign more accurate and equitable decision tools.
We found that seven clinical algorithms have been revised in the context of the impact of race and ethnicity. In 2021, the American College of Obstetricians and Gynecologists eliminated cutoffs for hematocrit levels based on race for screening for iron deficiency anemia in pregnancy31, data from the Cesarean Registry of the Maternal-Fetal Medicine Units Network was reanalyzed to develop a new Vaginal Birth After Cesarean (VBAC) calculator without race and ethnicity32, and a Task Force established by the National Kidney Foundation and the American Society of Nephrology recommended the use of an updated estimated glomerular filtration rate (eGFR) equation without race16. In 2022, the original UTICalc calculator was replaced by a race-free calculator with comparable predictive performance33. In 2023, race was removed from the Spirometry Reference Value Calculator34. In 2024, the American Heart Association adopted the Predicting Risk of cardiovascular disease EVENTs (PREVENT)22 as a race-free version of the Atherosclerotic Cardiovascular Disease (ASCVD) Risk Calculator35, and the American Society of Transplantation adopted an updated race- and ethnicity-free Kidney Donor Risk Index (KDRI)36.
Thus, it is critical to thoroughly investigate the impact of race and ethnicity on clinical decision-making and health disparities. While replacing race and ethnicity in clinical decision-making with an individual’s unique genetic makeup, environmental factors, and other relevant factors is preferable, including race and ethnicity in understanding health and healthcare disparities may still be prudent37. Race and ethnicity are often correlated with health disparities due to various factors such as socioeconomic status, access to healthcare, environmental conditions, and historical systemic racism. Removing race and ethnicity from algorithms without addressing these underlying disparities may overlook important risk factors and perpetuate health inequities. And completely ignoring race and ethnicity could lead to an incomplete understanding of health outcomes for marginalized communities. Some diseases and genetic variations are known to have higher prevalence rates among specific racial or ethnic populations. For instance, sickle cell anemia is more common in individuals of African or Mediterranean descent, and genetic mutations causing G6PD deficiency are more common in persons of African, Asian, and Mediterranean descent. In such instances, using race for screening may be acceptable in the interim until a better biological substitute is developed. The predictive models underlying clinical algorithms are frequently derived from datasets that were assembled from processes of clinical care. These datasets may contain racial and ethnic biases due to historical disparities in healthcare access and diagnosis. Simply removing race and ethnicity without addressing the underlying biases might perpetuate or amplify existing inaccuracies, leading to misdiagnoses and inappropriate treatment decisions.
Clinical algorithms, particularly risk scores, are currently exempt from FDA oversight due to their transparency, clinician-driven nature, and perceived low risk of direct injury. However, regulatory approaches continue to evolve, and the FDA has indicated that some algorithms, such as the Epic Sepsis Model38, may be regulated in the future under certain scenarios. In such cases, the FDA should add guidelines for evaluating the impact of race and ethnicity in these algorithms.
Five medications have race- and ethnicity-based pharmacogenetic screening recommendations (see Table 2), including testing for glucose-6-phosphate dehydrogenase (G6PD) deficiency in pegloticase and rasburicase, testing for the HLA-B*1502 variant in carbamazepine and oxcarbazepine, and testing for the HLA-B*5801 variant in allopurinol. Pharmacogenetic screening focuses on determining who should undergo specific pharmacogenetic testing so that testing is pursued only for those who are most likely to require it. However, the use of broad racial and ethnic categories complicates the application of these guidelines in practice. For instance, while the HLA-B*1502 variant is present in over 10% of individuals from Indonesia, Hong Kong, and Vietnam, it is present in less than 1.5% of individuals from Japan and Korea. Therefore, the broad racial category of Asians is inadequate for identifying which patients are at the greatest risk and would most likely benefit from genetic testing39. Hence, pharmacogenetic screening recommendations based on race and ethnicity may result in disparities in healthcare, though other clinical factors such as demographics and comorbidities may reduce the likelihood of adverse clinical outcomes. With rapid progress in precision medicine, replacing race and ethnicity, where possible with suitable blood and genetic tests is preferable. And as genetic tests, including multigene panels and whole genome sequencing, become more affordable, race- and ethnicity-based pharmacogenetic screening will become obsolete.
In recent years, the U.S. Congress has established requirements for drug manufacturers to submit a diversity action plan to the FDA that details their plans to enroll a diverse population in clinical trials based on sex, age, race, and ethnicity40. The FDA should go a step further and reexamine medications with race- and ethnicity-based guidelines and, if necessary, request that manufacturers reevaluate them on diverse populations.
In the catalog for medical devices, we chose to include those devices that have been in use for several decades and have published research demonstrating racial and ethnic performance differences. Though the use of these devices may result in disparities in healthcare, other clinical factors such as demographics and comorbidities may decrease the chance of adverse clinical outcomes. As mentioned in the “Results” Section, we excluded AI/ML-based SaMD products due to inadequate publicly available information. Recently, the U.S. Congress required device manufacturers, including those of SaMD, to submit a diversity action plan to the FDA outlining their plans to enroll a diverse population in the evaluation40. To ensure transparency, the FDA should require SaMD manufacturers to disclose the input variables used by the AI/ML software. This will allow the scientific community to characterize the medical AI/ML algorithms based on race and ethnicity.
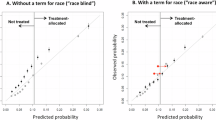
There are limitations to our approach. We concentrated on a narrow subset of the extensive clinical usage of race and ethnicity. Beyond risk calculators, differential reference ranges for laboratory test results, guidelines for medications, and differential performances of medical devices , race and ethnicity are often used to distinguish among variations in physiological processes, genetics, behavior, and cultural characteristics41. In the future, we intend to add uses of race and ethnicity outside of calculators, medication guidelines, and medical devices. We did not include the original online implementations of calculators that were subsequently modified to exclude race and ethncity as predictors because the original implementations were not available. The future inclusion of race- and ethnicity-based implementations of these algorithms will be useful for historical reasons as well as to evaluate if the revised formulations are indeed less biased. We did not include information on the potential harm or equity concerns related to the use of race and ethnicity because it is currently unclear if their inclusiondoes propagate disparities in all such algorithms. Some authors have pointed out that under certain frameworks of social utility and fairness, all individuals are served better when clinical decisions are guided by all predictors, including race and ethnicity. Further, the particular use of an algorithm may inform if race and ethnicity should be included or not. For example, a recent simulation study showed that removing race from diagnostic algorithms could make healthcare inequities worse while excluding race in prognostic algorithms that help decide how to allocate resources can mitigate inequities9.
The database will be actively updated to include additional clinical algorithms with race and ethnicity. In the future expansion of the database, we plan to offer additional details of algorithms, such as mathematical equations and statistical models, and include descriptions of the datasets from which the algorithms were derived and, if possible, provide access to the datasets themselves. Furthermore, we plan to review the literature and summarize the impact of each algorithm, as well as invite the public to offer evidence, positive, neutral, or negative, on racial and ethnic disparities. We intend to add additional useful information to the online database and expand its utility in collaboration with the Encoding Equity Alliance.
Methods
Data sources and search strategy
We conducted an exploratory search of databases, internet resources, and peer-reviewed scientific literature to identify clinical calculators, medications, and medical devices that were likely to use race- and ethnicity-based guidelines. We examined several sets of search terms and selected one that maximized sensitivity while maintaining good precision.
We conducted a Google search for internet resources with clinical calculators and designed the query to maximize sensitivity while aiming for reasonable precision. We ran the query in May 2023 (query: (medical OR clinical) AND (calculator OR equation OR score OR guideline) AND (race OR ethnicity)). We excluded internet resources if they lacked contact information, provided no references to peer-reviewed articles, provided only hyperlinks to external websites, described only smartphone apps for calculators, or did not implement calculators for online data entry and result output. From the included resources, we created a list of calculators with race and ethnicity.
We also conducted a PubMed search to find peer-reviewed articles that included a list of clinical calculators with race and ethnicity. We created the search query to maximize sensitivity while aiming for reasonable precision and ran the query in June 2023 (query: (medical OR clinical) AND (calculator OR equation OR score OR guideline) AND (race OR ethnicity) AND (bias or fairness)). We excluded articles that were not peer-reviewed (e.g., preprints) or did not contain a table or list with more than one clinical calculator with race and ethnicity. From the articles included, we compiled a list of clinical calculators with race and ethnicity. After merging the list obtained from internet resources with the list obtained from peer-reviewed articles, we removed duplicates to create a final list.
We used Micromedex, one of the largest pharmacological knowledge bases, to identify medications with race- and ethnicity-based initiation and monitoring guidelines. We queried Micromedex in May 2023 and generated independent lists for each of the following keywords: ancestry, descent, ethnicity, heritage, and peoples. After merging the lists and removing duplicates, we excluded medications that were combinations of multiple drugs since one of the constituent drugs was already included as a single medication, had no FDA Drug Label Information, or the Drug Label Information did not contain race and ethnicity-based guidelines.
We also used a PubMed search to find peer-reviewed articles about medical devices with different racial and ethnic performances (query: (medical OR clinical) AND device AND (race OR ethnicity) AND (bias or fairness)) and excluded articles that did not describe a medical device with differential racial and ethnic performances.
Data extraction
We reviewed the internet source and the PubMed reference for each included calculator and extracted pertinent information. The information included the name of the calculator, its purpose, a description of its use of race and ethnicity and rationale for their use, the predictors, a PubMed reference, and, if available, a description of modifications made to eliminate race and ethnicity after its introduction. In addition, we categorized each calculator based on its intended use and identified its primary clinical specialty.
We reviewed the FDA Drug Label Information for each included medication and extracted pertinent information. The information included the name of the medication, a description of the medication, a description of the use of race and ethnicity and rationale for their use, a reference to the FDA Drug Label Information, and the section(s) that contained guidelines based on race and ethnicity. In addition, we categorized each medication according to the racial and ethnic context of its use and identified its primary clinical specialty.
We reviewed the article for each included device and extracted pertinent information. The information included the name of the device, its purpose, a description of its use, a description of racial and ethnic differences in the performance of the device, and a PubMed reference.
Online database
After identification, data extraction, and validation, we created an online database that provides free access to the results. We plan to regularly update this open-access database as new calculators, medications, and other clinical uses of race and ethnicity are identified. We added a submission feature to the database, allowing the public to submit new calculators, medications, and medical devices that our search missed. Before being added to the database, all public submissions will be verified and cross-checked.
Data availability
All data generated during this study are included in this published article [and its supplementary information files]. Results of this study are available online at https://clinical-algorithms-with-race-and-ethnicity.org/.
References
Collins, G. S., Reitsma, J. B., Altman, D. G. & Moons, K. G. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD statement. Ann. Intern. Med. 162(1), 55–63 (2015).
Dziadzko, M. A., Gajic, O., Pickering, B. W. & Herasevich, V. Clinical calculators in hospital medicine: Availability, classification, and needs. Comput. Methods Programs Biomed. 133, 1–6 (2016).
Green, T. A., Whitt, S., Belden, J. L., Erdelez, S. & Shyu, C. R. Medical calculators: Prevalence, and barriers to use. Comput. Methods Programs Biomed. 179, 105002 (2019).
Lu, C., Ahmed, R., Lamri, A. & Anand, S. S. Use of race, ethnicity, and ancestry data in health research. PLOS Glob. Public Health 2(9), e0001060 (2022).
Cerdeña, J. P., Plaisime, M. V. & Tsai, J. From race-based to race-conscious medicine: How anti-racist uprisings call Us to act. Lancet 396(10257), 1125–1128 (2020).
Sirugo, G., Tishkoff, S. A. & Williams, S. M. The quagmire of race, genetic ancestry, and health disparities. J. Clin. Invest. 131(11) (2021).
Rebbeck, T. R., Mahal, B., Maxwell, K. N., Garraway, I. P. & Yamoah, K. The distinct impacts of race and genetic ancestry on health. Nat. Med. 28(5), 890–893 (2022).
Eneanya, N. D. et al. Health inequities and the inappropriate use of race in nephrology. Nat. Rev. Nephrol. 18(2), 84–94 (2022).
Basu, A. Use of race in clinical algorithms. Sci. Adv. 9(21), eadd2704 (2023).
Schmidt, I. M. & Waikar, S. S. Separate and unequal: Race-based algorithms and implications for nephrology. J. Am. Soc. Nephrol. 32(3), 529–533 (2021).
Kessler, L., Watts, K. & Abraham, N. Should we correct the use of race in urological risk calculators? J. Urol. 209(1), 17–20 (2023).
O’Brien, J. & Clare, C. A. Race-based versus race-conscious medicine in obstetrics and gynecology. Clin. Obstet. Gynecol. 66(1), 95–106 (2023).
Jain, A. et al. Awareness of Racial and ethnic bias and potential solutions to address bias with use of health care algorithms. JAMA Health Forum 4(6), e231197 (2023).
Vyas, D. A., Eisenstein, L. G. & Jones, D. S. Hidden in plain sight—reconsidering the use of race correction in clinical algorithms. N. Engl. J. Med. 383(9), 874–882 (2020).
Wright, J. L. et al. Eliminating race-based medicine. Pediatrics 150(1) (2022).
Delgado, C. et al. A unifying approach for GFR estimation: Recommendations of the NFK-ASN task force on reassessing the inclusion of race in diagnosing kidney disease. J. Am. Soc. Nephrol. 32(12), 2994–3015 (2021).
ACOG Practice Bulletin No. 205: Vaginal birth after cesarean delivery. Obstet. Gynecol. 133(2), e110–e127 (2019).
Manski, C. F. Patient-centered appraisal of race-free clinical risk assessment. Health Econ. (2022).
National Academies of Sciences, Engineering, and Medicine. Rethinking race and ethnicity in biomedical research (2024).
Council of Medical Specialty Societies. Reconsidering race in clinical algorithms: Driving equity through new models in research and implementation (2023). Available from: https://cmss.org/programs-and-resources/encoding-equity/.
Siddique, S. M. et al. The impact of health care algorithms on Racial and ethnic disparities: A systematic review. Ann. Intern. Med. 177(4), 484–496 (2024).
Khan, S. S. et al. Development and validation of the American heart association’s PREVENT equations. Circulation 149(6), 430–449 (2024).
Diao, J. A. et al. Implications of race adjustment in Lung-Function equations. N. Engl. J. Med. 390(22), 2083–2097 (2024).
Chin, M. H. et al. Guiding principles to address the impact of algorithm bias on Racial and ethnic disparities in health and health care. JAMA Netw. Open 6(12), e2345050 (2023).
Coots, M., Saghafian, S., Kent, D. M. & Goel, S. A framework for considering the value of race and ethnicity in estimating disease risk. Ann. Intern. Med. 178(1), 98–107 (2025).
Elovic, A. & Pourmand, A. MDCalc medical calculator app review. J. Digit. Imaging 32(5), 682–684 (2019).
McKinney, A. UpToDate: Evidence-based medicine database. J. Electron. Resour. Med. Libr. 9(1), 56–64 (2012).
Zhang, F. & Finkelstein, J. Inconsistency in race and ethnic classification in pharmacogenetics studies and its potential clinical implications. Pharmgenomics Pers. Med. 12, 107–123 (2019).
Khazanchi, R., Soled, D. R. & Yearby, R. Racism-conscious praxis: A framework to materialize anti-oppression in medicine, public health, and health policy. Am. J. Bioeth. 23(4), 31–34 (2023).
Schor, E. L. The Henry J. Kaiser family foundation. Acad. Med. 65(1), 26–27 (1990).
Anemia in Pregnancy. ACOG practice bulletin, number 233. Obstet. Gynecol. 138(2), e55–e64 (2021).
Grobman, W. A. et al. Prediction of vaginal birth after Cesarean delivery in term gestations: A calculator without race and ethnicity. Am. J. Obstet. Gynecol. 225(6), 664 (2021).
Shaikh, N. et al. Reassessment of the role of race in calculating the risk for urinary tract infection: A systematic review and meta-analysis. JAMA Pediatr. 176(6), 569–575 (2022).
Bowerman, C. et al. A Race-neutral approach to the interpretation of lung function measurements. Am. J. Respir. Crit. Care Med. 207(6), 768–774 (2023).
Goff, D. C. Jr. et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American college of cardiology/american heart association task force on practice guidelines. Circulation 129(25 Suppl 2), S49–73 (2014).
Miller, J., Lyden, G. R., McKinney, W. T., Snyder, J. J. & Israni, A. K. Impacts of removing race from the calculation of the kidney donor profile index. Am. J. Transpl. 23(5), 636–641 (2023).
Choy, K. W. From race-based to race-conscious medicine: Proceed with care. Intern. Med. J. 51(2), 309 (2021).
Lyons, P. G. et al. Factors associated with variability in the performance of a proprietary sepsis prediction model across 9 networked hospitals in the US. JAMA Intern. Med. 183(6), 611–612 (2023).
Goodman, C. W. & Brett, A. S. Race and pharmacogenomics-personalized medicine or misguided practice? Jama 325(7), 625–626 (2021).
Varma, T., Bierer, B. E. & Hantel, A. The promise and perils of diversity action plans for clinical trials. Jama 332(21), 1787–1788 (2024).
Cerdeña, J. P., Asabor, E. N., Plaisime, M. V. & Hardeman, R. R. Race-based medicine in the point-of-care clinical resource uptodate: A systematic content analysis. EClinicalMedicine 52, 101581 (2022).
Acknowledgements
This study was funded in part by the National Center for Advancing Translational Sciences of the National Institutes of Health under award numbers UL1 TR001857 and U24 TR004111.
Author information
Authors and Affiliations
Contributions
S.V. led all aspects of the review: conceptualization, supervision, search strategy, screening, validation, creation of database, and writing (original draft, review, and editing); M.J.S. was involved in search strategy, screening, validation, and writing (review and editing); E.M.S., M.M.M., and A.R.V. were involved in validating entries for accuracy and reviewing the final manuscript. All authors had full access to the data and accepted responsibility for submitting for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Visweswaran, S., Sadhu, E.M., Morris, M.M. et al. Online database of clinical algorithms with race and ethnicity. Sci Rep 15, 10913 (2025). https://doi.org/10.1038/s41598-025-94152-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-94152-5