Abstract
This study aims to investigate the efficacy of glueless simple oral mucosal transplantation to prevent the development of the limbal stem cell deficiency in rabbit model. Rabbit limbal stem cell deficiency (LSCD) models were constructed with alcohol and mechanical scraping. The oral mucosa and limbal tissue were harvested and cut into small pieces. Microincisions were made on the corneal limbus and the precut pieces were inserted in. Animals were divided to three groups: glueless simple oral mucosal epithelium transplantation (GSOMT), glueless simple limbal epithelium transplantation (GSLET) and LSCD group. Corneal epithelium defects, opacity and neovascularization were observed after surgery by slit-lamp microscopy. Neovascularization and epithelialization were scored. HE staining and immunohistochemistry of CK12, CK13, p63 were performed after observation. In the LSCD group, corneal neovascularization and opacification were present and epithelial defects were still observed by 4 months. In the GSOMT group, the cornea was clear and epithelialization was complete by 15 days; the fluorescein staining scores and neovascularization were significantly lower in GSOMT group comparing with LSCD group. There were no significant differences between GSOMT group and GSLET group. Histological study showed that the transplanted oral mucosal graft blend into the recipient corneal tissue well after surgery and the morphology or phenotype of the corneal epithelium surrounding the graft were similar to that of normal corneal epithelium. The glueless simple oral mucosal transplantation successfully prevented the development of the limbal stem cell deficiency in rabbit model. This method avoids the limited graft sources and the allogeneic rejection problem especially in binocular LSCDs. GSOMT could become a new surgery method for treating LSCD and this basic research lays a foundation for next clinical promotion and application.
Similar content being viewed by others
Introduction
The corneal epithelium forms a natural functional barrier to pathogenic bacterial infection, tear penetration into the corneal stroma, water evaporation and other factors, and forms a smooth and moist refractive surface, which is one of the important refractive media of the eyeball. The corneal epithelium relies on limbal stem cells, whether it is the apoptosis renewal of physiological states or the repair of wounds in pathological situations. Limbal stem cells are localized in the basal layer of epithelium within the limbal tissue1,2. Various physical and chemical factors, Steven-Joson syndrome, ocular pemphigoid and other eye diseases, and iatrogenic trauma such as ocular surface tumor resection and cryosurgery can damage the limbal tissue. The limbal is damaged to some extent, the function of limbal stem cells is difficult to maintain, the peripheral conjunctival epithelium invades the cornea to form vascularized conjunctival scar tissue wrapping the corneal surface, the smooth and transparent corneal epithelium is replaced by conjunctival tissue, the corneal transparency is reduced, and vision is impaired. This pathological change in the ocular surface is called limbal stem cell deficiency ocular surface (LSCD)3.
At present, the repair for limbal stem cell deficiency ocular surface mainly relies on limbal tissue transplantation4,5,6. In vitro construction of autologous limbal epithelial cell membranes is difficult to be widely implemented in clinical practice. In recent years, autologous (glueless) simple limbal epithelial transplantation (SLET or GSLET)7,8 has been successfully used for monocular the limbal stem cell deficiency ocular surface repair. GSLET realizes simple and easy operation, which is convenient for clinical development widely9,10,11,12. “Glueless” avoids glue-induced inflammation or graft displacement risks. However, the autologous limbal tissue materials required for transplantation are limited, especially the deficiency of limbal stem cells in both eyes, which cannot provide the autologous limbal tissue required for transplantation. On the other hand, the limbal is rich in blood vessels and lymphoid tissues, which is a site prone to immune reaction, and the rejection after allogeneic transplantation is serious, resulting in the failure of ocular surface repair13. Therefore, there is an urgent need to explore other tissue sources that can replace autologous limbal tissues to repair the limbal stem cell deficiency ocular surface in both eyes.
For a long time, many scientific research teams have been actively exploring other autologous tissue cells that can replace limbal stem cells as seed cells to repair the limbal stem cell deficiency ocular surface14. Oral mucosal epithelial cells, conjunctival epithelial cells, mesenchymal stem cells, hair follicle stem cells and embryonic stem cells are all research objects15,16,17,18. Previous studies have found that the oral mucosal epithelial cell membrane constructed with amniotic membrane in vitro as a carrier could repaired the rabbit limbal stem cell deficiency ocular surface19. However, the technology of tissue engineering cell membranes construction in vitro is complicated and requires not only laboratory hardware but also scientific researchers who have mastered tissue engineering technology. On the other hand, transformation this technology into clinical application requires a complex procedure with a long process. So, it restricts the extensive application of oral mucosal epithelial cell.
Drawing on the previous technical scheme of GSLET and based on the repair function of oral mucosal epithelial cell membrane, in this study, we plan to conduct a feasibility study on the repair of limbal stem cell deficiency ocular surface in a rabbit model by autologous glueless simple oral mucosal transplantation (GSOMT) as a novel alternative for treating bilateral limbal stem cell deficiency (binocular LSCD), hoping to avoid the limitations of cell culture and tissue engineering technology required for in vitro construction of cell membranes, and lay a foundation for the next clinical promotion and application.
Methods
Animals and grouping
Fifteen female New Zealand white rabbits aged 12 to 14 weeks and weighing 2.0–2.5 kg (Xilingjiao Experimental Animal Breeding Center, Jinan, Shandong Province, China) were selected and randomly divided into three groups: a glueless simple oral mucosal epithelium transplantation (GSOMT) group (n = 5), a glueless simple limbal epithelium transplantation (GSLET) group (n = 5) or limbal stem cell deficiency with no tissue transplantation (LSCD) group (n = 5). For details, the animals’ right eyes of the three groups were made into LSCD model; and in the GSOMT group, the right eyes received mucosal epithelium transplantation; and in the GSLET group, the right eyes received limbal stem cell transplantation collected from their left eyes. General anesthesia was induced by intravenously injection of 3% pentobarbital sodium (40–50 mg/kg). Evaluation was performed at 3 days, 7 days, 15 days, 2 months, and 4 months after surgery, and ocular specimens were excised at 4 months postoperatively after the rabbits were sacrificed by an intravenous overdose of pentobarbital sodium (1% solution, 150 mg/kg body weight, 2 mL/min). All animals were treatment in accordance to the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research. All animal experiments were approved by the Institutional Review Board of Shandong Second Provincial General Hospital (approval number XYK20210117).
The modeling of rabbit total limbal stem cell deficiency
The LSCD animal model was made according to previous literature20. Briefly, after being treated with antibiotic eyedrops three times a day for three days, the rabbits were anesthetized intravenously with 3% pentobarbital sodium (40–50 mg/kg) and topically with oxybuprocaine hydrochloride three times in half an hour, and the right eyes were disinfected and sterile draped (Fig. 1A). The whole ocular surface is soaked in an alcohol solution for 60 s followed by rinsing of the conjunctival sac thoroughly with balanced salt solution (Fig. 1B). The epithelium was removed completely after Alcohol soaking (Fig. 1C). The limbal area was further destroyed with additional mechanical scraping by a tunnel knife (Fig. 1D).
The process of modeling rabbit limbal stem cell deficiency (A–D) and key surgical steps of un-suturing autologous small oral mucosal or limbal tissue transplantation (E–I). (A) Normal rabbit ocular surface. (B, C) The epithelium was removed completely with Alcohol soaking. (D) The limbal area was further destroyed with additional mechanical scraping. (E, F) Oral mucosal was harvested, thinned, and split into small pieces. (G) 12 symmetrical incisions on the corneal limbus were made. (H) Short slightly oblique or horizontal tunnels were formed. (I, J) The precut pieces were inserted into the tunnels with forceps, and its ends exposed on the ocular surface (arrow and magnification). The harvest of limbal graft was not showed. The process of small limbal graft transplantation was similar with small oral mucosal graft.
Harvesting of oral mucosa epithelium
The rabbits were anesthetized intravenously with 3% pentobarbital sodium (40–50 mg/kg). After the oral cavity was disinfected with povidone iodine, oral mucosa of the lips was grasped with hooked forceps and a 3 × 4 mm piece of mucosal tissue was excised with spring scissors (Fig. 1E). The oral mucosa was then gently held with Lim’s forceps and cut into twelve to fifteen small pieces with scissors or surgical blade in a sterile Petri dish (Fig. 1F).
Harvesting of limbal tissue epithelium
The limbal tissue was harvested according to previous article7. After anesthesia the rabbit left eyes were disinfected and sterile draped. Then a 2*2 mm area was marked centered on the superior limbus, the conjunctiva was incised, and a sub-conjunctival dissection was carried out until the limbus was reached. A shallow dissection was then carried out 1 mm into the clear cornea, and the limbal tissue was excised and placed in balanced salt solution. The limbal tissue was then cut into small pieces.
Transplantation of small epithelial tissue pieces (oral mucosal or limbal tissue)
At 1–12 o’clock positions, 12 symmetrical radial 1.0-mm wide superficial incisions (20–50 µm in depth) on the corneal periphery adjacent and parallel to the limbus were made using 15° knife (Fig. 1G). Short slightly oblique or horizontal tunnels were formed using tunnel knife, which extended from the floor of every vertical incision with the length not exceeding 1.0 mm (Fig. 1H). The precut pieces (limbal or oral mucosal) were inserted into the tunnels with forceps and its ends exposed on the ocular surface (Fig. 1I, J). The precut pieces (limbal or oral mucosal) were transplanted immediately after remove the limbal stem cells from the right eye. Postoperatively, ofloxacin eye drops were applied three times a day for one week.
Clinical observations and evaluations
Corneal epithelium defects, opacity and corneal neo-vascularization were examined under white light and cobalt blue light using fluorescein staining by slit-lamp microscopy at 3 days, 7 days, 15 days, 2 months and 4 months respectively after transplantation.
The neo-vascularization was evaluated and graded according to previously reported21,22. Grade 0, no neovascularization of the cornea (score = 0); Grade 1, neovascularization within limbal ≤ 2 mm (score = 1); Grade 2, neovascularization around cornea ≤ 1/2 (score = 2); Grade 3, neovascularization around cornea > 1/2 (score = 3); Grade 4, neovascularization whole cornea (score = 4).
Corneal epithelial fluorescein sodium staining was used to record the area of epithelial defect. Image J software was used to circle the staining area and the ratio of defect area/ whole corneal area was recorded. Epithelialization was scored as follows: Grade 0, no fluorescein staining of the cornea (score = 0); Grade 1, staining ≤ 1/4 (score = 1); Grade 2, staining from 1/4 to 1/2 (score = 2); Grade 3, staining from 1/2 to 3/4 (score = 3); Grade 4, staining > 3/4 (score = 4)22.
Histological study
Oral mucosa and operated rabbit eyes were fixed in 4% paraformaldehyde for at least 24 h, paraffin-embedded, cut into 5-mm slices, and deparaffinized. HE staining were performed by a standard protocol. Immunohistochemical (IHC) studies were performed following standard protocol using anti-CK12 (× 300; Abcam, Cambridge, MA), anti-CK13 (× 200; Santa Cruz, Dallas, Texas), and anti-p63 (× 50: Abcam, Cambridge, MA). After primary incubation, slices were washed and incubated with the appropriate secondary antibody and stained with 3, 3-diaminobenzidine.
Statistics
SPSS 17.0 was used for data analysis. The T test was used to examine differences between the two groups. Comparisons among three or more groups were made using one-way ANOVA test. P < 0.05 was considered to be statistically significant.
Results
The morphology and histology of donor oral mucosa
The small oral mucosal graft was about 1.0 mm*1.0 mm size and composed of mucosal epithelium and subepithelial tissue (Fig. 2A). The surface of epithelium was smooth and the subepithelial tissue was relatively rough. The epithelium consisted of stratified squamous epithelium. The basal layer presented finger-like protrusions or wavy lines in the submucosal tissue to harbor a high density of high nucleus/plasma ratio cells. And no goblet cells were observed in the oral mucosal graft. Immunohistochemistry showed that the oral mucosal epithelial cells are diffusely stained by CK13 (Fig. 2B) and all layers are negative for CK12 (Fig. 2C). Some basal cells show nuclear p63 (stem cell markers) positivity in the lowest basal cell layer (Fig. 2D).
Clinical observation
Representative anterior segment photographs in LSCD, GSOMT and GSLET groups were shown in Fig. 3. In the LSCD group (Fig. 3A, B) epithelium was almost complete defect at 3 and 7 days after surgery and the fluorescein dyeing of the corneal was completely staining. On 15 days the corneal epithelium was still rough and partial fluorescein staining of the corneal is observed. Epithelial defects were still could be observed by 2 and 4 months. Corneal neovascularization and opacification were present in by 2 and 4 months. In the GSOMT (Fig. 3C, D) and GSLET (Fig. 3E, F) experimental groups, fluorescein staining demonstrated widespread positivity throughout the corneal epithelium at postoperative day 3, with a marked transition to focal staining observed by day 7, which indicating the graft promoting epithelial wound healing. Most of the rabbit corneal epithelium was completely repaired by 15 days. The cornea was clear, and only a few neovascularization may be seen within the superficial stroma. In the GSLET group, the left eye was used to collect limbal stem cells. The cornea of the left eye remained clear, and the epithelium was smooth and intact and no LSCD or neovascularization was developed during the observation period.
Clinical slit-lamp microscope and fluorescein staining observations after surgery at different time points. (A, B) In the LSCD group, epithelium defect was severe and exist though observation. Corneal neovascularization and opacification were present in by 2 and 4 months. (C, D) In the GSOMT group and GSLET group (E, F), epithelium was expanding over the corneal surface toward the center and no fluorescein staining of the cornea was observed at 15 days. The cornea was clear, and only a few neovascularization could be seen.
Table 1 shows the fluorescein staining scores in different groups. Table 2 shows the mean corneal epithelial defect/whole corneal area ratio in different groups. These results demonstrated lower scores in both GSOMT and GSLET groups compared to LSCD at all post-operative timepoints (P < 0.05), means that the epithelial repair speed was faster in the GSOMT group and GSLET group. No statistically significant difference was observed between GSOMT and GSLET (P > 0.05).
Table 3 shows the neovascularization scores of each rabbit obtained after surgery. At 4 months after surgery, the average score was 0.8 ± 0.45, 0.6 ± 0.55, 2.8 ± 0.45 separately in the GSOMT, GSLET and LSCD groups. The neovascularization scores were significantly lower in the GSOMT group and GSLET group compared with the LSCD group at both 2 months (P < 0.05) and 4 months (P < 0.01). There was no significant difference in GSOMT group and GSLET group (P > 0.05).
Histological study after surgery
HE staining shows that, in GSOMT group (Fig. 4A1, A2), the transplanted oral mucosal graft blend into the recipient corneal tissue well 4 months after surgery. The graft was located in the limbal of the cornea (Fig. 4A1, blue arrow), where corneal epithelium are visible on the right (Fig. 4A1, ※) and conjunctival epithelium on the left (Fig. 4A1, #). The graft was a round mound shape with a thick center and a flattened perimeter, bulging from the corneal surface. The structure at the transplant site resembled the normal oral mucosal and was composed of multiple layers of cells, consists of stratified squamous epithelium and basal cells with a large nucleus/plasma ratio. The neovascularization lumen is located within the superficial stroma of the cornea (Fig. 4A2, arrow). The neovascularization emanates from the graft and extends to the center of the cornea. In GSLET group (Fig. 4B1, B2), the limbal graft also blend into the recipient corneal tissue well. However, in LSCD group (Fig. 4C1, C2), the epithelial layer covering on the corneal surface was very thin and goblet cells were observed, indicating the existence of conjunctival epithelium.
HE staining after 4 months surgery in different groups. (A) In GSOMT group the transplanted oral mucosal graft blend into the recipient corneal tissue well. The graft was located in the limbal of the cornea (blue arrow), where corneal epithelium was visible on the right (※) and conjunctival epithelium on the left (#). The neovascularization lumen is located within the superficial stroma of the cornea (black arrow). (B) In GSLET group, the limbal graft (blue arrow) also blend into the recipient corneal tissue well. (C) In LSCD group the epithelial layer covering on the corneal surface was very thin and goblet cells were observed. Scale bar = 100 μm.
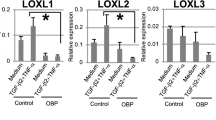
Immunohistochemistry results
Immunohistochemistry showed that in GSOMT group (Fig. 5A–C), CK12 are negative in all layers of the transplanted oral mucosal graft, while CK13 shows cytoplasmic positivity and p63 shows nuclear positivity in the basal cells, consistent with the phenotype of oral mucosal epithelium. In the epithelium surrounding the graft, CK12 is positive in the cytoplasm of cells in the all layers of the epithelium, while CK13 are negative, consistent with the phenotype of normal corneal epithelium.
Immunohistochemistry after 4 months surgery in different groups. (A–C) In GSOMT group, CK12 is negative while CK13 and p63 positivity in the oral mucosa graft consistent with the phenotype of oral mucosal epithelium. In the epithelium surrounding the graft, CK12 is positive while CK13 is negative, consistent with the phenotype of normal l corneal epithelium. (D–F) In the GSLET group, CK12 and p63 are positive, while CK13 is negative in the limbal tissue graft and the epithelium surrounding the graft, consistent with the phenotype of normal corneal epithelium. (G-I) In the LSCD group, CK13 and p63 are positive, while CK12 is negative, consistent with the conjunctival epithelium. (J-L). In normal central cornea, CK12 is positive in the cytoplasm of cells in the all layers of the epithelium and p63 nuclear positive in the basal cells while CK13 is negative. Scale bar = 100 μm.
In the GSLET group (Fig. 5D–F), CK12 is cytoplasm positive in the epithelial cells and p63 nuclear positive in the basal cells, while CK13 are negative in all layers. Same as the graft, in the epithelium surrounding the graft, CK12 and p63 are positive, while CK13 is negative.
In the LSCD group (Fig. 5G–I), CK13 is positive in the cytoplasm of cells in the all layers of the epithelium and p63 in the basal cells, while CK12 are negative in all layers, at the same time goblet cells were observed, consistent with the conjunctival epithelium, confirming the occurrences of LSCD.
In normal central cornea (Fig. 5J–L), CK12 is positive in the cytoplasm of cells in the all layers of the epithelium and p63 nuclear positive in the basal cells, while CK13 negative in all layers.
Discussion
This study preliminarily confirmed the effectiveness of GSOMT to prevent the development of limbal stem cell deficiency in a rabbit model. Half a month after GSOMT, slit lamp microscopy and fluorescein staining confirmed that the corneal surface of the operated eye was covered with a complete epithelial layer. The transplanted oral mucosal tissue was in place well, and the morphology gradually changed with the prolongation of time. 4 months after surgery, it is a round mound shape with a thick center and a flattened perimeter. As part of the smooth ocular surface, it blends into the recipient corneal tissue. HE sections showed that the epithelium at the transplant site resembled the normal oral mucosal epithelium and was composed of multiple layers of cells, with a large nucleus/plasma ratio in the basal layer expressing the stem cell marker p63. Neovascularization may be seen within the superficial stroma. The morphological structure of the epithelium on the surface of the corneal stroma outside the graft site is consistent with that of normal corneal epithelium and the corneal epithelial cell-specific marker CK12 is expressed. However, in the LSCD group, 7 days after modeling, the epithelial surface of the cornea was widely defected and the epithelium healed slowly. With the prolongation of time, the fibrovascular tissue membrane gradually grew, and after 4 months, the corneal surface was covered with a dense fibrovascular tissue membrane. The corneal surface was coated with conjunctival epithelium, the transparency was poor, and the pupil was faintly visible, showing typical clinical features of the limbal stem cell deficiency ocular surface. There were statistically significant differences in corneal neovascularization and transparency scores between the GSOMT and the LSCD group. HE staining and immunohistochemistry confirmed that the epithelium of LSCD group coated on the corneal surface was conjunctival epithelium (CK13 positive), which further confirmed the limbal stem cell deficiency ocular surface. The corneal epithelium of rabbits in the GSOMT group was smooth and transparent, and the scores of neovascularization and transparency were not significantly different from those in the GSLET group. These results showed the effectiveness of GSOMT to prevent the development of limbal stem cell deficiency in a rabbit model, and it was similar to GSLET that have been used clinically.
For the treatment of unilateral total LSCD, transplantation of autologous limbal epithelial stem cells cultured on HAM without the use of nonhuman animal cells or products has been demonstrated a safe and effective method23. However, the repair of bilateral limbal stem cell deficiency ocular surface is a clinical topic that needs to be solved urgently24. Allogeneic limbal stem cell transplantation is currently the main treatment, but the success rate of surgery is low25. The limbus is rich in blood vessels and lymphoid tissue, and is prone to rejection. In order to alleviate immune rejection and improve the success rate of surgery, local and systemic anti-rejection drugs are required for long-term use after surgery, which aggravates the economic burden of patients and has obvious drug toxicity and side effects13. Previous studies have shown that tissue engineering oral mucosal epithelial cell membrane transplantation in vitro can repair limbal stem cell deficiency ocular surface15,16. Autologous oral mucosal epithelial cell membrane transplantation avoids the risk of rejection associated with allogeneic limbal stem cell transplantation. However, the animal serum required for the construction of epithelial cell membrane maybe contain prions, and there is a risk that the recipients will be infected after transplantation of the epithelial cell membrane. In addition, the construction of cell membrane is expensive, and so far, the preparation of tissue-engineered corneal epithelial cell membrane can only be completed in laboratories with construction capabilities, and it is difficult to apply them to individual patients, which is difficult to realize the large-scale promotion and application of industrialization to clinical practice26. In this study, the autologous fresh oral mucosa was cut into small pieces and transplanted by glueless technology to successfully prevent the development of limbal stem cell deficiency. This study preliminary indicated the effectiveness of GSOMT to prevent the development of LSCD in a rabbit model. This protocol is simple to carry out and is expected to become an effective solution to prevent the development of limbal stem cell deficiency in both eyes. It has good prospect of clinical transformation. However, in clinical practice, stem cell transplantation can only be performed after the ocular surface inflammation is stabilized in the eye of LSCD, so the therapeutic effect of GSOMT on the LSCD needs to be further confirmed by our future experiments. In addition, we will expand the number of experimental animals and observation indicators to obtain more detailed data.
In this study, it was found that the small oral mucosal tissue pieces transplanted in the GSOMT group survived well on the limbal surface of the recipient and maintained its own biological characteristics. However, the morphology changes gradually to coincide with the curvature of the ocular surface. During the transplantation process, a superficial stromal pocket is first prepared at the position of 12 h at the limbus of the recipient, and then small oral mucosal tissue piece is stuffed into the pocket, and the moderately sized pocket accommodates and fixes the tissue piece to avoid the tissue piece falling off due to mechanical factors such as eyelid opening and closing. This method of transplantation eliminates the cost of sutures or bioglue and the risk of sutures stimulating inflammation, inducing neovascularization into the clear cornea, and increasing infection. Both in vivo and in vitro studies have shown that the maintenance of the biological characteristics of epithelial stem cells is inseparable from serum components27. In vivo, the oral mucosa and limbal epithelial layer contains stem cells, which are located in areas rich in blood vessels, in contrast, the avascular clear cornea, whose epithelial layer does not contain stem cells28. Animal transplantation experiments confirmed that the transplanted epithelial stem cells were located in the limbus containing blood vessels, while on the surface of the transparent cornea, epithelial stem cells were missing29. In this study, the tissue pieces were transplanted to the recipient limbus at the position of 12 h, and the limbus was rich in blood vessels, which was convenient for the survival of the transplanted tissue pieces, and the new blood vessels in the superficial matrix under the tissue pieces gradually grew in, providing energy for the self-renewal, proliferation and differentiation of basal stem cells. The close adhesion between the eyelid and the ocular surface and the shear force formed by the sliding of the eyelid on the ocular surface cause the morphology of the tissue pieces to gradually change, from the lump shape at the beginning of transplantation to a flat shape until it becomes a part of the smooth ocular surface.
In this study, it was found that the surface of corneal surface was covered by conjunctival epithelium which indicated the occurs of LSCD in the LSCD group. While in the GSOMT and GSLET group, corneal surface was normal corneal epithelium, indicating the development of LSCD was prevented. The specific mechanism by which the transplanted small oral mucosal tissue in this study prevents the occurrence of LSCD was not clear. Previous studies have shown that the local limbal stromal microenvironment for limbal epithelial stem cells may be improved by transplanted limbal substrates30. In our study, there were clear demarcation and different phenotype between the transplanted oral mucosal epithelium and the surrounding regenerated epithelium. This indicates that the regenerated epithelium surrounding the graft does not come from the transplanted oral mucosa, but from the stimulation of oral mucosa to residual limbal cells to promote their regeneration. The specific mechanism was not clear. Previous studies have confirmed that a variety of growth factors, cytokines, and other soluble molecules, such as epidermal growth factor (EGF), basic fibroblast growth factor (bFGF) and nerve growth factor (NGF), β‐catenin, interleukin-13 (IL13) ,WNT16B, Neuregulin 1 (NRG1) have regulatory effects on the proliferation, differentiation and apoptosis of limbal stem cells31,32,33,34. In the future experiments, we will study the relevant factors at the protein and gene levels, hoping to reveal the specific mechanism that the development of LSCD was prevented in this study.
Conclusion
This study confirmed that autologous simple oral mucosal tissue transplantation can prevent the development of LSCD and avoid the limited graft sources or the allogeneic rejection problem especially in binocular LSCDs. It provides a new strategy to prevent the development of LSCD and lays a foundation for the next clinical promotion and application.
Data availability
Data supporting the results of this study are available from the corresponding author Lin Shen upon reasonable request.
References
Ramos, T., Scott, D. & Ahmad, S. An update on ocular surface epithelial stem cells: cornea and conjunctiva. Stem Cells Int. 2015, 601731. https://doi.org/10.1155/2015/601731 (2015).
Ordonez, P. & Di Girolamo, N. Limbal epithelial stem cells: role of the niche microenvironment. Stem Cells 30, 100–107. https://doi.org/10.1002/stem.794 (2012).
Le, Q., Xu, J. & Deng, S. X. The diagnosis of limbal stem cell deficiency. Ocul. Surf. 16, 58–69. https://doi.org/10.1016/j.jtos.2017.11.002 (2018).
Kenyon, K. R. & Tseng, S. C. Limbal autograft transplantation for ocular surface disorders. Ophthalmology 96, 709–722. https://doi.org/10.1016/s0161-6420(89)32833-8 (1989) (discussion 722–703).
Tsai, R. J. & Tseng, S. C. Human allograft limbal transplantation for corneal surface reconstruction. Cornea 13, 389–400. https://doi.org/10.1097/00003226-199409000-00003 (1994).
Tsubota, K. et al. Treatment of severe ocular-surface disorders with corneal epithelial stem-cell transplantation. N. Engl. J. Med. 340, 1697–1703. https://doi.org/10.1056/NEJM199906033402201 (1999).
Sangwan, V. S., Basu, S., MacNeil, S. & Balasubramanian, D. Simple limbal epithelial transplantation (SLET): a novel surgical technique for the treatment of unilateral limbal stem cell deficiency. Br. J. Ophthalmol. 96, 931–934. https://doi.org/10.1136/bjophthalmol-2011-301164 (2012).
Malyugin, B. E., Gerasimov, M. Y. & Borzenok, S. A. Glueless simple limbal epithelial transplantation: The report of the first 2 cases. Cornea 39, 1588–1591. https://doi.org/10.1097/ICO.0000000000002467 (2020).
Thokala, P. et al. Economic, clinical and social impact of simple limbal epithelial transplantation for limbal stem cell deficiency. Br. J. Ophthalmol. 106, 923–928. https://doi.org/10.1136/bjophthalmol-2020-318642 (2022).
Basu, S. et al. Simple limbal epithelial transplantation: Long-term clinical outcomes in 125 cases of unilateral chronic ocular surface burns. Ophthalmology 123, 1000–1010. https://doi.org/10.1016/j.ophtha.2015.12.042 (2016).
Malyugin, B. E., Kalinnikova, S. Y., Knyazer, B. & Gerasimov, M. Y. Midterm outcomes of autologous glueless simple limbal epithelial transplantation for unilateral limbal stem cell deficiency. Cornea 43, 45–51. https://doi.org/10.1097/ICO.0000000000003279 (2024).
Malyugin, B. et al. Femtosecond laser-assisted autologous glueless simple limbal epithelial transplantation in unilateral limbal stem cell deficiency: 12-month outcome of the first clinical cases. Cornea https://doi.org/10.1097/ICO.0000000000003688 (2024).
Qi, X., Xie, L., Cheng, J., Zhai, H. & Zhou, Q. Characteristics of immune rejection after allogeneic cultivated limbal epithelial transplantation. Ophthalmology 120, 931–936. https://doi.org/10.1016/j.ophtha.2012.11.001 (2013).
Utheim, T. P. Limbal epithelial cell therapy: Past, present, and future. Methods Mol. Biol. 1014, 3–43. https://doi.org/10.1007/978-1-62703-432-6_1 (2013).
Rovere, M. R. et al. Preserving basement membranes during detachment of cultivated oral mucosal epithelial cell sheets for the treatment of total bilateral limbal stem cell deficiency. Cell Transplant. 27, 264–274. https://doi.org/10.1177/0963689717741140 (2018).
Oliva, J., Bardag-Gorce, F. & Niihara, Y. Clinical trials of limbal stem cell deficiency treated with oral mucosal epithelial cells. Int. J. Mol. Sci. 21, 411. https://doi.org/10.3390/ijms21020411 (2020).
Galindo, S. et al. Subconjunctival injection of mesenchymal stem cells for corneal failure due to limbal stem cell deficiency: State of the art. Stem Cell Res. Ther. 12, 60. https://doi.org/10.1186/s13287-020-02129-0 (2021).
Hassan, N. T. & AbdelAziz, N. A. Oral mucosal stem cells, human immature dental pulp stem cells and hair follicle bulge stem cells as adult stem cells able to correct limbal stem cell deficiency. Curr. Stem Cell Res. Ther. 13, 356–361. https://doi.org/10.2174/1574888X13666180223124936 (2018).
Le, Q. & Deng, S. X. The application of human amniotic membrane in the surgical management of limbal stem cell deficiency. Ocul Surf. 17, 221–229. https://doi.org/10.1016/j.jtos.2019.01.003 (2019).
Atalay, E. et al. Animal models for limbal stem cell deficiency: A critical narrative literature review. Ophthalmol. Ther. 13, 671–696. https://doi.org/10.1007/s40123-023-00880-0 (2024).
Faraj, L. A., Said, D. G., Al-Aqaba, M., Otri, A. M. & Dua, H. S. Clinical evaluation and characterisation of corneal vascularisation. Br. J. Ophthalmol. 100, 315–322. https://doi.org/10.1136/bjophthalmol-2015-306686 (2016).
Zhu, J. et al. Reconstruction of functional ocular surface by acellular porcine cornea matrix scaffold and limbal stem cells derived from human embryonic stem cells. Tissue Eng. Part A 19, 2412–2425. https://doi.org/10.1089/ten.TEA.2013.0097 (2013).
Kolli, S., Ahmad, S., Lako, M. & Figueiredo, F. Successful clinical implementation of corneal epithelial stem cell therapy for treatment of unilateral limbal stem cell deficiency. Stem Cells 28, 597–610. https://doi.org/10.1002/stem.276 (2010).
Vazirani, J. et al. Surgical management of bilateral limbal stem cell deficiency. Ocul Surf. 14, 350–364. https://doi.org/10.1016/j.jtos.2016.02.006 (2016).
Cheung, A. Y. et al. Allogeneic ocular surface stem cell transplantation outcomes with decreased or no systemic immunosuppression in the elderly. Cornea 42, 1482–1487. https://doi.org/10.1097/ICO.0000000000003233 (2023).
Cabral, J. V., Jackson, C. J., Utheim, T. P. & Jirsova, K. Ex vivo cultivated oral mucosal epithelial cell transplantation for limbal stem cell deficiency: A review. Stem Cell Res. Ther. 11, 301. https://doi.org/10.1186/s13287-020-01783-8 (2020).
Shen, Y. & Le, Q. The progress in techniques for culturing human limbal epithelial stem cells. Hum. Cell 36, 1–14. https://doi.org/10.1007/s13577-022-00794-2 (2023).
Robertson, S. Y. T., Roberts, J. S. & Deng, S. X. Regulation of limbal epithelial stem cells: Importance of the niche. Int. J. Mol. Sci. 22, 11975. https://doi.org/10.3390/ijms222111975 (2021).
Jurkunas, U., Johns, L. & Armant, M. Cultivated autologous limbal epithelial cell transplantation: New frontier in the treatment of limbal stem cell deficiency. Am. J. Ophthalmol. 239, 244–268. https://doi.org/10.1016/j.ajo.2022.03.015 (2022).
Huang, M. et al. Using acellular porcine limbal stroma for rabbit limbal stem cell microenvironment reconstruction. Biomaterials 32, 7812–7821. https://doi.org/10.1016/j.biomaterials.2011.07.012 (2011).
Trosan, P., Cabral, J. V., Smeringaiova, I., Studeny, P. & Jirsova, K. Interleukin-13 increases the stemness of limbal epithelial stem cells cultures. PLoS ONE 17, e0272081. https://doi.org/10.1371/journal.pone.0272081 (2022).
Zhao, S., Wan, X., Dai, Y., Gong, L. & Le, Q. WNT16B enhances the proliferation and self-renewal of limbal epithelial cells via CXCR4/MEK/ERK signaling. Stem Cell Rep. 17, 864–878. https://doi.org/10.1016/j.stemcr.2022.03.001 (2022).
Wan, X. et al. WNT16b promotes the proliferation and self-renewal of human limbal epithelial stem/progenitor cells via activating the calcium/calcineurin A/NFATC2 pathway. Cell Prolif. 56, e13460. https://doi.org/10.1111/cpr.13460 (2023).
Wang, B. et al. NRG1 regulates proliferation, migration and differentiation of human limbal epithelial stem cells. Curr. Issues Mol. Biol. 45, 10121–10130. https://doi.org/10.3390/cimb45120632 (2023).
Acknowledgements
Thanks to everyone who participated in the experiment.
Funding
This work was supported by grants from the medical health science and technology development plan project of Shandong Province (202007021534), the National Natural Science Foundation of China (number 82401220), the National Natural Science Foundation of China (number 82070925).
Author information
Authors and Affiliations
Contributions
K. Z. and L.S. conceived, designed the study and wrote the manuscript; K. Z., W.L., X. R. and Y. Y. acquired, analyzed, or interpreted data; W. C., F. C. and J.Z. performed statistical analysis; L. S. supervised the study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This research was approved by the Institutional Review Board of Shandong Second Provincial General Hospital. The number of the approved animal study by the Review board was XYK20210117. Treatment is in accordance to the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research. The study is in accordance with ARRIVE guidelines.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, K., Liu, W., Ren, X. et al. Autologous glueless simple oral mucosal transplantation for the repair of limbal stem cell deficiency ocular surface in a rabbit model. Sci Rep 15, 10855 (2025). https://doi.org/10.1038/s41598-025-96088-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-96088-2