Abstract
Background: Antibiotic treatment contributes to gut microbiota dysbiosis. Previous studies have shown that fecal microbiota transplantation (FMT), fecal filtrate (FF), and activated charcoal (AC) treatments can prevent gut microbiota disturbances caused by antibiotics or Clostridioides difficile infection. However, these treatments have typically been limited to restoring gut microbiota after dysbiosis, and antibiotics must be discontinued beforehand. Here, we investigated the protective effects of these treatments on gut microbiota to prevent dysbiosis during concurrent systemic ceftriaxone administration. Methods: C57BL/6 mice that received intraperitoneal ceftriaxone for seven consecutive days were concomitantly treated with AC, FMT, FMT + AC, FF, or FF + AC via oral gavage. Gut microbiomes were analyzed using 16 S rRNA gene sequencing, and intestinal mucosal pathology was evaluated through H&E staining. Results: Systemic ceftriaxone administration significantly altered gut microbiota diversity and composition but did not affect intestinal mucosal histology. Alpha and beta diversity analyses showed that microbiota diversity decreased in all ceftriaxone-treated groups, with the ceftriaxone + FF + AC group retaining the highest diversity. The ceftriaxone + AC group had higher Enterococcus but lower Muribaculaceae relative abundances than the control (no ceftriaxone), ceftriaxone only, and ceftriaxone + FF + AC groups. Conclusions: These results show that fecal filtrate transplantation combined with activated charcoal treatment may help balance gut microbiota diversity and reduce the presence of resistant bacteria during ceftriaxone exposure.
Similar content being viewed by others
Introduction
It has recently been established that the gut microbiota is essential for health and disease. The gut microbiota comprises a community of bacteria, fungi, viruses, protozoa, and other microorganisms that colonize the gastrointestinal tract. Additionally, the predominant bacteria in the gut are anaerobes1,2. Dysbiosis refers to a change in the composition and/or diversity of the gut microbial community caused by factors such as the host, diet, genetics, antibiotics, and infections3. Several studies have shown that gut microbiota dysbiosis is associated with many diseases, including colorectal cancer, obesity, and infection4,5,6.
Antibiotic treatment can lead to gut microbiota dysbiosis, characterized by reduced species diversity, altered metabolome, and increased antibiotic resistance7. Broad-spectrum antibiotics used for infections, such as cephalosporins, carbapenems, vancomycin, and colistin, can also disrupt the gut microbiota8,9. Strategies to prevent antibiotic-induced gut dysbiosis include the replacement of lost microbiota (e.g., fecal microbiota transplantation or probiotics), manipulation of the microbiota (e.g., phages or prebiotics), and inactivation of the offending antibiotics (e.g., adsorption by activated charcoal).
Recently, fecal microbiota transplantation (FMT) has emerged as a promising therapy for the treatment of gastrointestinal diseases10,11, type II diabetes12, cancer13,14,15, and recurrent Clostridioides difficile infection16,17. Previous studies have reported that FMT can restore gut microbiota after antibiotic treatment. In a dysbiosis mouse model, BALB/c mice were treated with ceftriaxone for 7 days, followed by FMT for 3 days, which resulted in increased microbial diversity and decreased levels of pro-inflammatory cytokines18. Treatment with vancomycin and colistin for 7 days, followed by FMT for 2 days, restored the composition and diversity of the gut microbiota, protecting mice from Pseudomonas aeruginosa infection19. Previous studies on FMT have focused primarily on restoring gut microbiota after antibiotic-induced dysbiosis has occurred, as FMT was typically administered after such disruptions. Since antibiotics can affect the microbiota during FMT, they are usually discontinued prior to the procedure. However, repeated doses of FMT may help replace killed microbes and maintain microbiota diversity. It remains unclear whether FMT can prevent antibiotic-induced gut dysbiosis when administered concurrently and repeatedly without halting antibiotic treatment.
Fecal filtrate (FF), which is sterilely derived from bacterium-depleted fecal microbiota transplantation (FMT), contains various phages, immunoglobulins, macromolecules, and metabolites. Even without viable bacteria, FF exhibits activity against C. difficile infection20, with its efficacy thought to be associated with bacteriophages21. In contrast to FMT, which is typically administered after antibiotics have been discontinued, FF theoretically should not be affected by concurrent antibiotic treatment since it does not contain live bacteria. Therefore, FF could potentially be administered alongside antibiotics and might help prevent antibiotic-induced gut dysbiosis.
Activated charcoal (AC) is a safe and commonly used treatment for bacterial infections, and it helps protect the gut microbiota during antibiotic treatment. The co-administration of DAV132—a colon-targeted charcoal-based adsorbent—and moxifloxacin has been studied to safeguard the gut microbiota in healthy volunteers22. Moreover, AC could reduce ceftriaxone concentration in fecal samples from patients who received intravenous ceftriaxone23.
In our hospital, ceftriaxone is the most common intravenous antibiotic for the first empirical treatment of various community-acquired infections in a patient who has been newly admitted. With high biliary excretion and broad spectrum, ceftriaxone can cause dysbiosis, leading to colonization and infection with multidrug-resistant bacteria18,24. For non-gastrointestinal infections (e.g., pneumonia, urinary tract infection, meningitis, etc.), the residual ceftriaxone in the gut excreted after parenteral administration can be eliminated safely without interfering with blood ceftriaxone level, since its absorption through the gastrointestinal tract is negligible25.
In this study, we investigated the effects of combining FMT with AC compared to FF with AC on the gut microbiota in a ceftriaxone-induced dysbiosis mouse model. We found that mice treated with the combination of FF and AC exhibited higher gut microbiota diversity and a lower number of resistant bacteria during ceftriaxone exposure.
Materials and methods
Animals and gut microbial dysbiosis model
The study was approved (Approval ID 2491011) by the Institutional Animal Care and Use Committee of the Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand. The animal care and protocol used in this study were based on the National Institutes of Health (NIH), USA. All methods were performed following the ARRIVE guidelines.
Female C57BL/6 mice (aged 6–8 weeks) were purchased from Nomura Siam International, Bangkok, Thailand. The mice were co-housed in standard individually ventilated cages (5 mice per cage) under a 12-h light/dark cycle and given food and water ad libitum. After 14 days of acclimatization, all mice were randomly separated into 7 groups which were Control group (no ceftriaxone), Ceftri group (ceftriaxone treatment only), CeftriAC group (concurrent ceftriaxone and activated charcoal treatment), CeftriFMT group (concurrent ceftriaxone and fecal microbiota transplantation treatment), CeftriFMTAC group (concurrent ceftriaxone and fecal microbiota transplantation plus activated charcoal treatment), CeftriFF group (concurrent ceftriaxone and fecal filtrate transplantation treatment), CeftriFFAC group (concurrent ceftriaxone and fecal filtrate transplantation plus activated charcoal treatment).
To establish the gut microbial dysbiosis model, mice were intraperitoneally injected with 0.2 ml ceftriaxone (50 mg/ml) following a previous publication26 once daily for 7 consecutive days. For microbiota analysis, feces samples were collected from control, ceftriaxone, and other treatments mice at 0 and 7 days after treatments. Each mouse was labeled on its tail differently to keep track of each mouse for all time points throughout the experiment.
During the collection, each mouse was put into a separate box, one mouse per box, waiting for defecated feces, which were then collected freshly in a 1.5 mL microcentrifuge tube and stored at -80 °C until further processing. For histology analysis, the colon was collected at the proximal 2 cm of the cecum from all mice at the endpoint.
At the endpoint, mice were euthanized under isoflurane anesthesia. Animals were removed from all experiments if they reached moribund criteria (lack of purposeful movement or > 20% weight loss) before the end point.
Preparation of fecal sample and treatment
The feces were collected from untreated mice and immediately stored at -80 ◦C. For fecal microbiota transplantation (FMT), pool fresh fecal samples were mixed and diluted with 10 volumes in sterile normal saline. Large particles in the fecal suspension were precipitated by gravity for 5 min at room temperature, and the obtained supernatant was used. For fecal filtrate (FF), the supernatant was centrifuged for 10 min at 3000 g and filtered with a 0.45 μm sterile filter. 200 µl of the FMT and FF were orally gavaged into each mouse for 7 days. In CeftriAC, CeftriFMTAC, and CeftriFFAC, oral-activated charcoal (AC) was given before FMT and FF by oral gavage (50 mg in 200 µl) for 7 days.
DNA extraction and PCR amplification
The feces were collected from all groups on day 0 and 7 and immediately stored at -80 ◦C. Frozen fecal samples were isolated using the QIAamp PowerFecal Pro DNA Kit (Qiagen, Hilden, Germany) according to the manufacturer’s protocols. Briefly, 0.25 g of fecal samples were extracted. The quality of the extracted DNA was determined via the DeNovix QFX Fluorometer. The V3-V4 regions of the 16 S rRNA gene were performed using the Qiagen QIAseq 16 S/ITS Region panel (Qiagen, Hilden, Germany). Cycling conditions followed the targeted PCR: 95 °C for 2 min, and 12 cycles of 95 °C for 30 s, 50 °C for 30 s, and 72 °C for 2 min, followed by 72 °C for 7 min. The 16 S rRNA gene amplicons were purified by QIAseq magnetic beads and labeled with different sequencing adaptors using QIAseq 16 S/ITS Region Panel Sample Index PCR Reaction (Qiagen, Hilden, Germany). Cycling conditions followed the index PCR reaction: 95 °C for 2 min, and 19 cycles of 95 °C for 30 s, 60 °C for 30 s, and 72 °C for 2 min, followed by 72 °C for 7 min. The DNA libraries with different indexes (approximately 630 bp) were purified using QIAseq magnetic beads (Qiagen, Hilden, Germany). The quality and quantity of DNA libraries were evaluated respectively using DeNovix QFX Fluorometer and QIAxcel Advanced (Qiagen, Hilden, Germany). Paired-end sequencing, 2 × 300, was performed using the Illumina Miseq platform following the manufacturer’s protocols (Illumina, San Diego, CA, USA).
Analysis of 16 S rRNA gene sequences
The sequences were processed following DADA2 v1.16.0 pipeline (https://benjjneb.github.io/dada2/). The DADA2 pipeline describes microbial diversity and community structures using unique amplicon sequence variants (ASVs)7. Microbial taxa were classified from Silva version 138 as a reference database8. Alpha diversity index (Chao1 richness, Shannon, and PD whole tree) was computed using DADA2 software. Non-metric multidimensional scaling (NMDS) based on Bray-Curtis dissimilarity and principal coordinate analysis (PCoA) were plotted from Phyloseq data for beta diversity. Linear discriminant analysis effect size (LEfSe) and cladogram plot were performed to identify the bacterial biomarkers.
Histological analysis
The proximal colon tissues were fixed in 10% neutral buffered formalin for 24 h. Five-micron thick sections of paraffin-embedded (FFPE) tissues were stained with hematoxylin and eosin, and a blinded, experienced researcher scored slides. The histological damage score was scored as previously described27.
Statistical analysis
Pairwise comparison of alpha diversity (Observed ASVs, Chao1, Shannon, and PD whole tree) and LEfSe analysis were calculated using the Kruskal-Wallis test. Permutational multivariate analysis of variance (PERMANOVA) was performed to evaluate the significant differences in beta diversity among groups. These bioinformatics analyses were performed with the DADA2 v1.16.0 pipeline (https://benjjneb.github.io/dada2/). Mouse body weight and relative abundance at the genus level were compared using one-way ANOVA Welch’s test analysis using GraphPad Prism software (version 10, San Diego, CA, USA). Data were expressed as the mean ± s.e.m. and p values *p ≤ 0.05 and **p ≤ 0.01 for all experiments were considered statistically significant.
Results
The effect of treatments on gut microbiota
C57BL/6 mice were treated with ceftriaxone for 7 consecutive days. Concomitantly, activated charcoal (AC), fecal microbiota transplantation (FMT), and fecal filtrate (FF) were administered to the ceftriaxone-treated mice via oral gavage. The experimental design is illustrated in Fig. 1A. During ceftriaxone treatment, all mice showed no incidents of diarrhea or signs of distress. On day 7, the average body weight (BW) of the Ceftri group was not significantly different from the Control group. The BW of the CeftriFFAC group was significantly lower than that of the Ceftri group, while BW of the CeftriAC, CeftriFMTAC, CeftriFMT, and CeftriFF groups were not significantly different from the Ceftri group (Supplementary Fig. 1A). The alpha-diversity and beta-diversity analyses were conducted to assess the effects of the treatments. The results showed that the highest alpha diversity, as measured by observed species, Chao1, Shannon, and PD whole tree, was found in the control group and pre-treatment of each group. On day 7, the observed species, Chao1, and PD whole tree of the Ceftri, CeftriAC, CeftriFMT, CeftriFMTAC, CeftriFF, and CeftriFFAC groups were significantly lower than that of the Control group, except Shannon in CeftriFF and CeftriFFAC groups. Notably, the Chao 1 and PD whole tree of the CeftriFFAC group were significantly higher than that of the CeftriAC group (Fig. 1B). Moreover, the principal coordinate analysis (PCoA) using weighted UniFrac and Bray-Curtis dissimilarity demonstrated that the microbial community structures were distinct among the groups (PERMANOVA test; p < 0.001) (Fig. 1C). The pairwise distance testing revealed that all groups were significantly different than that of control group on day 7 (Supplementary Fig. 1B). These findings indicate that while ceftriaxone treatment alters gut microbiota diversity and composition, certain interventions can modulate these effects, with the CeftriFFAC group showing the most promising effects.
The diversity of gut microbiota changes in the dysbiosis mouse model. A The experimental design of dysbiosis model. C57BL/6J mice were treated with ceftriaxone and followed by treatments (AC, FMT, FMT + AC, FF, and FF + AC) for 7 consecutive days. B Alpha diversity (observed species, Chao1, Shannon, and PD whole tree) by 16 S rRNA gene sequencing in the feces from different experimental treatment groups at pre-condition versus day 7 (n = 3–8 per group). C PCoA on weighted UniFrac using the Bray Curtis method on 16 S rRNA gene sequencing of fecal microbiota from different treatment groups at pre-condition versus day 7(n = 3–8 per group). All experimental data were representative of two independent experiments. Statistics were done using the Kruskal-Wallis test (B) and the Permutational multivariate analysis of variance (PERMANOVA) test (C). *p < 0.05, **p < 0.01.
Alterations in the composition of the gut microbiota
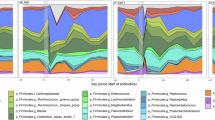
To explore the effect of ceftriaxone on the gut microbiota alteration in the different treatment groups, we performed 16s RNA sequencing on fecal samples from ceftriaxone-treated mice at pre-condition compared to day 7. The relative abundances of various taxa differed among the groups at the genus level (Fig. 2A). The relative abundance of Muribaculaceae was notably high in all groups at pre-condition. On day 7, the CeftriAC group showed a significantly higher relative abundance of Enterococcus than both the Control and Ceftri groups. In contrast, the CeftriFFAC group showed a significantly lower relative abundance of Enterococcus than the CeftriAC group. The CeftriFFAC group still had somewhat higher, though not significantly, Enterococcus relative abundance than the Control group (Fig. 2B). On the other hand, the relative abundance of Muribaculaceae of the CeftriFFAC group was significantly higher than in the CeftriAC group. In contrast, both the Ceftri and CeftriAC groups had significantly lower abundances compared to the control group (Fig. 2C). Additionally, compared to the control group, the Ceftri group showed a significantly higher relative abundance of Lactobacillus, while Clostridia was also higher, though this difference was not significant (Fig. 2D-E). Though not significantly different, the highly abundant Dubosiella and less abundant Ruminococcus, Rikenella, Prevotellaceae, Lachnospiraceae, Lachnoclostridium, and Clostridia_UCG-014 in the Control group almost disappeared from all groups with ceftriaxone administration, no matter what concurrent treatment they had (Fig. 2A). These results indicate that ceftriaxone significantly alters gut microbiota composition, with concurrent treatments modulating specific bacterial populations.
Relative abundance of gut microbiota in different groups at the genus levels. A The relative abundance of the fecal gut microbiota at genus level from different treatment groups at pre-condition versus day 7(n = 3–8 per group). B-E Mean relative abundance of Enterococcus, Muribaculaceae, Lactobacillus, and Clostridia on day 7(n = 3–8 per group). All experimental data were representative of two independent experiments. Statistics were done using one-way ANOVA Welch’s test (B-E). *p < 0.05, **p < 0.01, ***p < 0.001.
The linear discriminant analysis effect size (LEfSe) analysis
The LEfSe analysis was used to assess differences across all classification levels and identify taxonomic variations among the groups. Bacterial taxa with LDA scores greater than 4 are displayed in Fig. 3A.The Bacteroidota, Bacteroidia, Bacteroidales, Muribaculaceae, Lachnospirales, and Lachnospiraceae were significantly dominant in the control group, while the Staphylococcales, Staphylococcaceae, and Staphylococcus were significantly dominant in Ceftri group at day 7. The CeftriAC group was enriched considerably with bacteria, including Enterorhabdus, Lachnoclostridium, and Turicibacter at pre-condition, and with Firmicutes, Bacilli, Lactobacillales, Enterococcaceae, and Enterococcus at day7. The Clostridia and Clostridia_UCG_014 were significantly enriched in the CeftriFMT at pre-condition. The Proteobacteria, Actinobacteria, Coriobacteria, Coriobacteriales, Gammaproteobacteria, Enterobacteriaceae, Atopobiaceae, Coriobacteriaceae_UCG_002, Parasutterella, Bacteroidaceae, Bacteroides, and Muribaculum were significantly enriched in the CeftriFMT at day 7. The CeftriFMTAC group was enriched considerably with bacteria, including Erysipelotrichales, Erysipelotrichaceae, and Dubosiella at pre-condition. The Lactobacillaceae and Lactobacillus were significantly enriched in the CeftriFF group on day 7. Finally, the CeftriFFAC group was enriched considerably with Eggerthellaceae at pre-condition and with Verrucomicrobiota, Verrucomicrobiae, Verrucomicrobiales, Akkermansiaceae, and Akkermansia (Fig. 3A-B). These results highlight distinct microbial shifts across treatments, with specific bacterial taxa enriched in response to different interventions.
The linear discriminant analysis effect size (LEfSe). A The bar plot represented the effect size (LDA) for a significant difference in bacterial relative abundance from experimental treatment groups at pre-condition versus day 7 (n = 3–8 per group). B Cladogram showed the different taxonomic clades among the treatment groups (n = 3–8 per group). All experimental data were representative of two independent experiments. Statistics were done using the Kruskal-Wallis test (A-B).
Systemic administration of ceftriaxone does not affect intestinal mucosal pathology
To assess the intestinal mucosal pathology of ceftriaxone-treated mice following different treatments, proximal colon samples were stained with hematoxylin and eosin (H&E) on day 7, at the end of the treatment (Fig. 4A-B). All groups showed no or little inflammatory cellular infiltration without any significant difference between groups. In addition, loss of mucosal architecture, crypt abscesses, and goblet cell depletion remained unchanged in the Ceftri, CeftriAC, CeftriFMT, CeftriFMTAC, CeftriFF, and CeftriFFAC groups compared to the control group (data did not show). These findings suggest that systemic administration of ceftriaxone in this setting did neither change the intestinal wall structure nor increase cellular infiltration.
Systemic ceftriaxone administration did not affect intestinal mucosal pathology. A Representative picture of H&E stained sections of the proximal colon from different experimental treatment groups on day 7. Magnification, ×200 (scale bar, 50 μm). B Cellular infiltration score of proximal colon sections was blindly graded (n = 3 per group). Data are shown as the mean ± SEM of one experiment.
Discussion
Previous studies have shown that antibiotic treatment contributes to gut microbiota dysbiosis7,8,9. It has been reported that gut microbiota dysbiosis can be associated with many diseases, including colorectal cancer, obesity, and infection4,5,6. In this study, C57BL/6 mice were systematically administered ceftriaxone sodium with concomitant different treatment strategies for 7 days. Fecal bacterial diversity significantly decreased in the ceftriaxone treatment group compared to the control group. Although FMT is a promising therapy for treating recurrent C. difficile infection and antibiotic-induced dysbiosis16,17,28, FMT treatment in our study only showed a non-significant increase in diversity. The Ceftri FF AC group exhibited higher Chao1 and PD whole tree diversities compared to the Ceftri AC group. These results indicate a synergistic effect between FF and AC on the balance of microbial diversity in the mouse intestine during ceftriaxone administration.
Previous studies showed the impact of FMT after the withdrawal of antibiotics18,19. In contrast, this study demonstrated the effect of different treatments during the ceftriaxone administration, resembling real clinical settings where antibiotics cannot be discontinued at will. Theoretically, ceftriaxone administration may induce the production of AmpC beta-lactamase in Enterobacter29, promote horizontal transfer of AMR genes30, and favorably select bacteria with intrinsic resistance to ceftriaxone, such as Pseudomonas aeruginosa, Bacteroides, Lactobacillus, and Enterococcus31. Chakraborty et al. reported that short-term systemic ceftriaxone treatment induced expansion of the Enterococcus and Lactobacillus genera in the mouse intestine24. Consistently, our results showed that, on day 7, the Enterococcus and Lactobacillus genera increased in the gut of ceftriaxone-treated mice. However, Bacteroides and Enterobacter were comparable between groups in this study, while P. aeruginosa—not a normal flora for mice—could not be observed in any groups.
Previous studies have suggested that activated charcoal (AC) can adsorb antibiotics in the gut during treatment, potentially reducing the colonization and proliferation of resistant bacteria. A mouse model treated with cefotaxime and DAV131 (a charcoal-based adsorbent) for 3 days prior to infection with the Klebsiella pneumoniae strain (PUG-2) showed decreased colonization of K. pneumoniae in the fecal samples32. However, in this study, the Ceftri AC group showed a significantly higher abundance of Enterococcus genus compared to the Ceftri group. Although there is no definitive explanation, this may be due to desorption (the release of drugs, e.g., aspirin, from AC after adsorption33) of ceftriaxone from AC. Without AC, the ceftriaxone level in the gut would quickly rise due to biliary excretion and decline rapidly through normal defecation. However, with AC, the rapid increase in ceftriaxone levels in the gut might be blunted by AC adsorption, and the decline may be delayed due to desorption of ceftriaxone from AC and constipation caused by AC. In general, prolonged and low-level antibiotic exposure can promote overgrowth of drug-resistant bacteria more effectively than short, high-level exposure. We observed that mice in the CeftriAC group defecated more slowly than those in other groups, and our records indicated that collecting feces from this group was troublesome due to the relatively small amount produced. Unfortunately, we did not quantitatively record these data, so we cannot strongly confirm our claim. Unlike CeftriAC group, we found that the CeftriFFAC group did not exhibit a higher abundance of Enterococcus and Lactobacillus genera compared to the Ceftri group. FF may counteract the constipation caused by activated charcoal, as we did not encounter any issues with fecal collection in the CeftriFFAC group.
The balance between the residual fecal ceftriaxone and the dosage of AC might play an important role. An excess amount of AC should work as an adsorbent in the presence of a low amount of residual ceftriaxone. On the other hand, an excess amount of ceftriaxone might quickly saturate the adsorption ability of a low amount of AC, and the AC might then act as a reservoir instead. The outcomes could be better if the dosage of AC had been increased or used at the end of antibiotic treatment to adsorb a limited amount of residual antibiotic.
Previous studies have shown that FMT can restore the mucosal barrier functions in mice with ceftriaxone-induced dysbiosis18. However, the CeftriFMT and CeftriFMTAC groups in this study had a higher abundance of enterococci compared to the Ceftri group, although this increase was not statistically significant. FMT likely transferred a low number of enterococci already present in the fecal suspension, which were then selected and expanded by ceftriaxone in the gut. In contrast, FF did not contain any bacteria and could not introduce additional enterococci into the recipients. Ott et al. demonstrated that sterile fecal filtrate transfer restored normal stool habits and eliminated symptoms of C. difficile infection20.
The Muribaculaceae family is the most abundant in the gastrointestinal tract of mice34. Our results showed that the Muribaculaceae family significantly decreased in the Ceftri group compared to the control group. Some mice in the CeftriFFAC group retained comparable abundance to that of the control group. Wang et al. demonstrated that polyphenol rosemary acid treatment increased the abundance of Muribaculaceae and restored mucous secretion in mice with colitis35.
Li et al. reported that short-term oral ceftriaxone administration resulted in distorted tissue architecture, vascular congestion, and inflammatory cell infiltration18. Another study found histological lesions in the intestine following long-term oral ceftriaxone administration36. Unlike oral administration, our model with intraperitoneal administration showed that ceftriaxone-treated mice did not exhibit loss of mucosal architecture, crypt abscesses, or goblet cell depletion, except for a limited amount of inflammatory cell infiltration. Our results are consistent with previous reports indicating that short-term systemic ceftriaxone treatment does not affect the intestinal pathology of mice24. We suggest that the routes and doses of antibiotic administration may contribute to different pathologies in the colon.
Though oral antibiotics may better show the benefits of our treatments, they are impractical in clinical settings. AC can reduce the oral bioavailability of antibiotics, thus contraindicated for the oral route of antibiotics. The complexity of the FMT process and its potential risks (e.g., aspiration, infections from hidden or unknown pathogens) can limit its usage to carefully selected cases, typically inpatients who have prolonged intravenous broad-spectrum antibiotics and suffer recurrent severe infections caused by multidrug-resistant bacteria. On the other hand, relatively mild outpatient cases who can have oral antibiotics may not be worth receiving FMT due to its risks and hassle.
There are some limitations to our study. Only relative abundance was analyzed in this study. While absolute abundance can reflect the growth and decline of taxa directly, the increase or decrease of the relative abundance of any particular taxon may also be due to the decrease or increase of other taxa, respectively. Overall absolute abundance analysis requires bacterial cell count either by culture (colony-forming units) or by flow cytometry37. Multiplying each taxon relative abundance by the overall absolute abundace will give specific absolute abundance of that particular taxon. However, the culture method is limited to only culturable bacteria. For flow cytometry, host cell debris and small food particles may jeopardize the results of bacterial cell count. Real-time PCR or digital droplet PCR, utilizing a primer/probe set specific to a taxon of interest, may be more reliable for quantification of specific taxon absolute abundance.
We could not keep the same total volume of oral gavage for all groups. The CeftriFMTAC and CeftriFFAC groups received twice the volume compared to the other groups. Mixing FMT and AC into a single volume of 200 µl was too thick for oral gavage. Rather than preparing a 400 µl mix of FMT and AC, we decided to feed them sequentially, 200 µl each. Oral gavage with AC was performed first to adsorb intestinal ceftriaxone, keeping the residual antibiotic away from the FMT in the later gavage. However, the difference in volume fed could alter the chance of complications (e.g., aspiration, gut injuries) and the anatomical distribution of FMT components in the recipient’s gut38. Oral gavage with FMT to a mouse with a stomach full of AC suspension from the first gavage might also result in a different distribution of FMT components compared to a mouse with an empty stomach. These could become a confounder, affecting the observed characteristics of gut microbiota after the treatments.
In terms of microbiota diversity and compositions, the pretreatment heterogeneity across all seven groups was quite remarkable (Figs. 1B and 2A, and 3A). Two weeks of acclimation were probably not enough, because the Control group at day 7 was still quite different from the Control group at day 0 (Fig. 1C), meaning that the microbiota was still not stable at the time of rerandomization (day 0). Since we had many groups (7 in total), the rerandomization might not guarantee the balance of the rapidly changed and different microbiota in each mouse, resulting in baseline differences, which could then obscure the treatment effects.
Our experiments presented only a few phenotypic results, and we did not conduct any mechanistic studies. We have not yet explored the interaction mechanisms between the host gut microbiota and activated charcoal during ceftriaxone treatment in combination with fecal filtrate transplantation. This will be the focus of our future research.
Conclusions
This is the first study to demonstrate that fecal filtrate transplantation combined with activated charcoal may help balance gut microbiota diversity and reduce the presence of resistant bacteria in response to ceftriaxone exposure. This combination could serve as an alternative approach during ceftriaxone administration for patients with resistant bacteria.
Data availability
The raw data of 16 S rRNA sequencing that support the results in this study are available in the BioSample database under accession number PRJNA1168919 (https://dataview.ncbi.nlm.nih.gov/object/PRJNA1168919).
Abbreviations
- AC:
-
Activated charcoal
- C. difficile:
-
Clostridioides difficile
- FMT:
-
Fecal microbiota transplantation
- FF:
-
Fecal filtrate
- FFPE:
-
Formalin-fixed paraffin-embedded
- H&E:
-
Hematoxylin and eosin
- K. pneumoniae:
-
Klebsiella pneumoniae
- LEfSe:
-
Linear discriminant analysis effect size
- PCoA:
-
Principal coordinate analysis
- PERMANOVA:
-
Permutational multivariate analysis of variance
References
Maciel-Fiuza, M. F. et al. Role of gut microbiota in infectious and inflammatory diseases. Front. Microbiol. 14 (2023).
Madhogaria, B., Bhowmik, P. & Kundu, A. Correlation between human gut Microbiome and diseases. Infect. Med. 1 (3), 180–191 (2022).
Levy, M., Kolodziejczyk, A. A., Thaiss, C. A. & Elinav, E. Dysbiosis and the immune system. Nat. Rev. Immunol. 17 (4), 219–232 (2017).
Bernard-Raichon, L. et al. Gut Microbiome dysbiosis in antibiotic-treated COVID-19 patients is associated with microbial translocation and bacteremia. Nat. Commun. 13 (1), 5926 (2022).
Hamilton, M. J., Weingarden, A. R., Sadowsky, M. J. & Khoruts, A. Standardized frozen Preparation for transplantation of fecal microbiota for recurrentclostridium difficileinfection. Official J. Am. Coll. Gastroenterol. | ACG. 107 (5), 761–767 (2012).
Wang, J-W. et al. Fecal microbiota transplantation: review and update. J. Formos. Med. Assoc. 118, S23–S31 (2019).
Ramirez, J. et al. Antibiotics as major disruptors of gut microbiota. Front. Cell. Infect. Microbiol. 10, 572912 (2020).
Patangia, D. V., Anthony Ryan, C., Dempsey, E., Paul Ross, R. & Stanton, C. Impact of antibiotics on the human Microbiome and consequences for host health. MicrobiologyOpen 11 (1), e1260 (2022).
Palleja, A. et al. Recovery of gut microbiota of healthy adults following antibiotic exposure. Nat. Microbiol. 3 (11), 1255–1265 (2018).
Benech, N. & Sokol, H. Fecal microbiota transplantation in Gastrointestinal disorders: time for precision medicine. Genome Med. 12 (1), 58 (2020).
Tan, P., Li, X., Shen, J. & Feng, Q. Fecal microbiota transplantation for the treatment of inflammatory bowel disease: An update. Front. Pharmacol. 11, 574533 (2020).
Siew, C. N. et al. Microbiota engraftment after faecal microbiota transplantation in obese subjects with type 2 diabetes: a 24-week, double-blind, randomised controlled trial. Gut 71 (4), 716 (2022).
Baruch, E. N. et al. Fecal microbiota transplant promotes response in immunotherapy-refractory melanoma patients. Science 371 (6529), 602–609 (2021).
Davar, D. et al. Fecal microbiota transplant overcomes resistance to anti-PD-1 therapy in melanoma patients. Science 371 (6529), 595–602 (2021).
Routy, B. et al. Fecal microbiota transplantation plus anti-PD-1 immunotherapy in advanced melanoma: a phase I trial. Nat. Med. 29 (8), 2121–2132 (2023).
Baunwall, S. M. D. et al. Faecal microbiota transplantation for recurrent clostridioides difficile infection: An updated systematic review and meta-analysis. EClinicalMedicine 29–30, 100642 (2020).
Gupta, S., Allen-Vercoe, E. & Petrof, E. O. Fecal microbiota transplantation: in perspective. Therapeutic Adv. Gastroenterol. 9 (2), 229–239 (2016).
Li, M. et al. Fecal microbiota transplantation and bacterial consortium transplantation have comparable effects on the re-establishment of mucosal barrier function in mice with intestinal dysbiosis. Front. Microbiol. 6, 692 (2015).
Dessein, R. et al. Antibiotic-related gut dysbiosis induces lung immunodepression and worsens lung infection in mice. Crit. Care. 24 (1), 611 (2020).
Ott, S. J. et al. Efficacy of sterile fecal filtrate transfer for treating patients with Clostridium difficile infection. Gastroenterology 152 (4), 799–811 (2017). e7.
Zuo, T. et al. Bacteriophage transfer during faecal microbiota transplantation in Clostridium difficile infection is associated with treatment outcome. Gut 67 (4), 634–643 (2018).
de Gunzburg, J. et al. Protection of the human gut Microbiome from antibiotics. J. Infect. Dis. 217 (4), 628–636 (2018).
Torvorapanit, P. et al. The in vitro efficacy of activated charcoal in fecal ceftriaxone adsorption among patients who received intravenous ceftriaxone. Antibiotics (Basel, Switzerland) 12(1) (2023).
Chakraborty, R. et al. Ceftriaxone administration disrupts intestinal homeostasis, mediating noninflammatory proliferation and dissemination of commensal enterococci. Infect. Immun. 86(12) (2018).
Lee, S., Kim, S. K., Lee, D. Y., Chae, S. Y. & Byun, Y. Pharmacokinetics of a new, orally available ceftriaxone formulation in physical complexation with a cationic analogue of bile acid in rats. Antimicrob. Agents Chemother. 50 (5), 1869–1871 (2006).
Bongers, K. S. et al. Antibiotics cause metabolic changes in mice primarily through Microbiome modulation rather than behavioral changes. PLoS One. 17 (3), e0265023 (2022).
Grasa, L. et al. Antibiotic-Induced depletion of murine microbiota induces mild inflammation and changes in Toll-Like receptor patterns and intestinal motility. Microb. Ecol. 70 (3), 835–848 (2015).
Yang, M. et al. Antibiotic-Induced gut microbiota dysbiosis modulates host transcriptome and m6A epitranscriptome via bile acid metabolism. Adv. Sci. 11 (28), 2307981 (2024).
Jacoby, G. A. AmpC beta-lactamases. Clin. Microbiol. Rev. 22 (1), 161–182 (2009). Table of Contents.
Liu, G., Thomsen, L. E. & Olsen, J. E. Antimicrobial-induced horizontal transfer of antimicrobial resistance genes in bacteria: a mini-review. J. Antimicrob. Chemother. 77 (3), 556–567 (2022).
Hollenbeck, B. L. & Rice, L. B. Intrinsic and acquired resistance mechanisms in Enterococcus. Virulence 3 (5), 421–433 (2012).
Grall, N. et al. Oral DAV131, a charcoal-based adsorbent, inhibits intestinal colonization by beta-lactam-resistant Klebsiella pneumoniae in cefotaxime-treated mice. Antimicrob. Agents Chemother. 57 (11), 5423–5425 (2013).
Filippone, G. A., Fish, S. S., Lacouture, P. G., Scavone, J. M. & Lovejoy, F. H. Jr. Reversible adsorption (desorption) of aspirin from activated charcoal. Arch. Intern. Med. 147 (8), 1390–1392 (1987).
Ormerod, K. L. et al. Genomic characterization of the uncultured bacteroidales family S24-7 inhabiting the guts of homeothermic animals. Microbiome 4 (1), 36 (2016).
Wang, Q. et al. Rosmarinic acid restores colonic mucus secretion in colitis mice by regulating gut Microbiota-Derived metabolites and the activation of inflammasomes. J. Agric. Food Chem. 71 (11), 4571–4585 (2023).
Guo, Y. et al. Long-term use of ceftriaxone sodium induced changes in gut microbiota and immune system. Sci. Rep. 7, 43035 (2017).
Guk, J. et al. Modeling the bacterial dynamics in the gut microbiota following an antibiotic-induced perturbation. CPT Pharmacometrics Syst. Pharmacol. 11 (7), 906–918 (2022).
Rodriguez-Palacios, A., Khoretonenko, M. V. & Ilic, S. Institutional protocols for the oral administration (gavage) of chemicals and microscopic microbial communities to mice: analytical consensus. Exp. Biol. Med. (Maywood). 244 (6), 459–470 (2019).
Acknowledgements
We would like to thank all staff of the Excellence Center for Infectious Diseases, King Chulalongkorn Memorial Hospital, Thai Red Cross Society, Bangkok, Thailand, for help and support in the laboratory, and the team of the animal center from the Faculty of Medicine of Chulalongkorn University for their assistance and care of the animals during this study.
Funding
This work was supported by the Thailand Science Research and Innovation Fund Chulalongkorn University (HEA_FF_68_079_3000_013) and Ratchadapiseksompotch Fund, Faculty of Medicine, Chulalongkorn University (RA-MF-52/64). SK was supported by the Ratchadapisek Somphot Fund for Postdoctoral Fellowship, Chulalongkorn University.
Author information
Authors and Affiliations
Contributions
KK and KP performed the experiments; SK performed the experiments, interpreted the data, co-directed the study, and wrote the manuscript.; VN designed the experiments, interpreted the data, directed the studies, and wrote the manuscript. All the authors critically reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kumpunya, S., Kawang, K., Pollapong, K. et al. The effects of repeated fecal transplantation and activated charcoal treatment on gut dysbiosis induced by concurrent ceftriaxone administration in mice. Sci Rep 15, 13908 (2025). https://doi.org/10.1038/s41598-025-96701-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-96701-4